Abstract
Rationale: Cystic fibrosis is a progressive disease requiring a complex, time-consuming treatment regimen. Nonadherence may contribute to an acceleration of the disease process. Spirituality influences some parental healthcare behaviors and medical decision-making.
Objectives: We hypothesized that parents of children with cystic fibrosis, when classified into groups based on adherence rates, would share certain psychosocial and religious and/or spiritual variables distinguishing them from other adherence groups.
Methods: We conducted a multisite, prospective, observational study focused on parents of children younger than 13 years old at two cystic fibrosis center sites (Site 1, n = 83; Site 2, n = 59). Religious and/or spiritual constructs, depression, and marital adjustment were measured by using previously validated questionnaires. Determinants of adherence included parental attitude toward treatment, perceived behavioral norms, motivation, and self-efficacy. Adherence patterns were measured with the Daily Phone Diary, a validated instrument used to collect adherence data. Cluster analysis identified discrete adherence patterns, including parents’ completion of more treatments than prescribed.
Measurements and Main Results: For airway clearance therapy, four adherence groups were identified: median adherence rates of 23%, 52%, 77%, and 120%. These four groups differed significantly for parental depression, sanctification of their child’s body, and self-efficacy. Three adherence groups were identified for nebulized medications: median adherence rates of 35%, 82%, and 130%. These three groups differed significantly for sanctification of their child’s body and self-efficacy.
Conclusions: Our results indicated that parents in each group shared psychosocial and religious and/or spiritual factors that differentiated them. Therefore, conversations about adherence likely should be tailored to baseline adherence patterns. Development of efficacious religious and/or spiritual interventions that promote adherence by caregivers of children with cystic fibrosis may be useful.
Keywords: cystic fibrosis, parents, psychosocial, spirituality, treatment adherence
Children with chronic medical conditions often experience health declines secondary to poor adherence to prescribed therapies, which are often the parents’ responsibility. Parental cystic fibrosis (CF) treatment adherence is variable, which is partly due to the complex and time-consuming daily treatment regimen (1, 2). For most patients, the current accepted CF treatment regimen consists of a minimum of airway clearance therapy (ACT), chronic use of oral and nebulized medications (NMs), and pancreatic enzyme replacement with intermittent need for additional oral, nebulized, and occasional intravenous medications during acute illness. Patients with CF are at significant risk over time for developing comorbidities, adding additional complexity. Poor adherence leads to increased exacerbations and disease progression, resulting in greater stress and financial burden, time away from school, academic and social deficits, and decreased quality of life (3).
Previous studies of patients with CF have shown poor adherence when objective measures are used. Reported adherence rates are 27–46% for pancreatic enzymes and 51% for frequency of airway clearance (4). Past studies have also shown that patients can be classified into groups based on adherence patterns (5). Psychosocial factors are known to affect adherence, including depression (6) and family cohesiveness and conflict (7). Poorer marital functioning has long been identified with lower adherence to a child’s medical treatment for CF (8). An underappreciated influence on adherence is religious beliefs and spirituality (R/S). Definitions of R/S are numerous because of significant overlap between the constructs and their multidimensional nature. Following Hill and colleagues, spirituality is defined herein as, “feelings, thoughts, experiences, and behaviors which arise from a search for the sacred,” and religion is distinguished by its communal nature by adding to the definition “the means and methods (e.g., rituals or prescribed behaviors) of the search receive validation and support from within an identifiable group of people” (9). R/S has been related to treatment adherence in other populations (10–13), and parents of children with CF have described a relationship between their spiritual beliefs and treatment adherence (14).
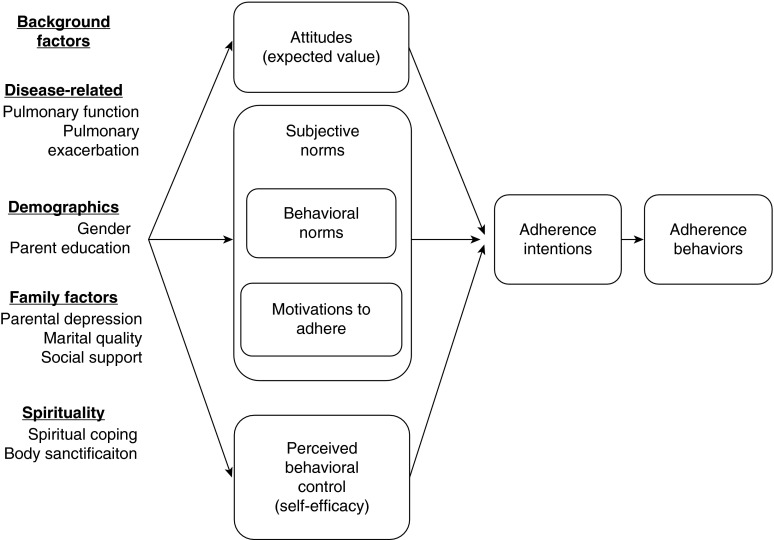
In prior work, we presented preliminary evidence of the relationship between R/S and parental adherence to CF treatments using the theory of reasoned action (15) as a conceptual model (16). This theoretical model (see Figure 1) posits that adherence behavior can be reasonably well anticipated by parents’ intentions to adhere to their child’s treatments, which are predicted by three “determinants”: attitude toward the value of the treatment (its utility), perceived behavioral norms (interactions between their motivation to follow the regimen and the expectations they perceive others have for them to adhere), and self-efficacy for completing the treatment regimen. The determinants are influenced by “background factors” that include demographics, disease-related variables, and psychosocial and spiritual factors. On the basis of our prior work and that of others (17), R/S was operationalized using two constructs: religious coping and sanctification of the body. Religious coping, defined as “a search for significance in times of stress, in ways related to the sacred” (18), has both positive and negative dimensions, each reflecting its association with health outcomes rather than the nature of the coping itself. Sanctification is defined as imbuing one’s child’s body with spiritual significance, reflecting the idea that parents see their child’s body as a “gift” or “miracle” or that their child’s body is “created in the image of God.” It is a two-dimensional construct, with both monotheistic (manifesting God) and spiritual (having sacred significance) dimensions (17).
Figure 1.
The theory of reasoned action.
In this study, we sought to describe the link between R/S and adherence in parents of children with CF for ACT and NM. We hypothesized that parents classified into groups based on rates of adherence would share certain psychosocial and R/S variables that would distinguish them from other adherence groups. Identification of important psychosocial or R/S constructs could then be targeted for intervention in subsequent research.
Methods
This multisite, cross-sectional study was performed at two academic pediatric hospitals with accredited CF centers: Cincinnati Children’s Hospital Medical Center (Site 1) and University of Alabama at Birmingham/Children’s Hospital of Alabama (Site 2). Parents of children with CF ages 13 years and younger were eligible for the study (n = 160 at Site 1; n = 175 at Site 2). The study was approved by the institutional review boards at both sites (IRB 2010-1041). Parents were informed by a letter from their child’s pulmonologist of their eligibility for this study and were approached at their child’s next clinic appointment with the opportunity to ask questions, decline to participate, or complete an informed consent form.
When informed consent was obtained from parents, they were given an internet link enabling them to log into the REDCap Survey site (19) to complete a series of questionnaires at their convenience. Appointments were also made for parents to complete three Daily Phone Diary (DPD) calls (20).
Measures
Background factors
Multiple questionnaires were completed to assess a series of background factors. Surveys included the following scales: sanctification of the body, religious coping styles, religiosity, depression, and marital adjustment. Additional details about these scales, including measures of reliability, score ranges, and examples of questions, can be found in Table 1.
Table 1.
Measurements of spiritual, religious, and psychosocial background factors
| Scale/Subscale | Cronbach’s α (Previous Studies) | Score Range | What the Scale Measures | Examples |
|---|---|---|---|---|
| Sanctification of the body | 0.98 (0.74–0.98)* | 12–84 (Likert) | Belief that the sacred is manifest in their child’s body | “My child’s body is created in God’s image.” |
| Manifestation of God | ||||
| Sacred qualities | 0.98 (0.74–0.98) | 10–70 (Likert) | The extent to which respondents perceive their child’s body as having sacred qualities | “My child’s body is miraculous.” |
| Religious coping styles (RCOPE) | 0.86 (0.85–0.93)† | 0–21 (Likert) | How often positive religious coping is used | “Looked for a stronger connection with God” |
| Positive religious coping | ||||
| Negative religious coping | 0.86 (0.85–0.93) | 0–21 (Likert) | How often negative religious coping is used | “Wondered what I did for God to punish me” |
| Problem solving | 0.86 (0.85–0.93) | Item level | How often religious coping is used for problem solving or control of a stressor | “Tried to deal with the situation on my own without God’s help.” |
| Religiosity (Duke) | 0.84 (0.75)‡ | 5–27 | Three dimensions of religiosity: organizational, nonorganizational, and intrinsic | “How often do you attend church or other religious meetings?” |
| Faith, peace, and meaning (FACIT) | 0.88 (0.84)§ | 0–48 (Likert) | Three spiritual domains in persons dealing with chronic illnesses | “I find comfort in my spiritual beliefs.” |
| Depression (CES-D) | 0.93 (0.63–0.93)‖ | 0–60 (Likert) | How often the child experienced symptoms | “I talked less than usual.” |
| Marital adjustment (dyadic) | 0.92 (0.96)¶ | 0–151 | Quality of relationship in married or cohabitating couples | “Do you and your mate engage in outside interests together?” |
Definition of abbreviations: CES-D = Center for Epidemiologic Studies Depression Scale; FACIT = Functional Assessment of Chronic Illness Therapy–Spiritual Well-being Scale; RCOPE = Religious Coping Scale.
Mahoney and colleagues (17).
Pargament and colleagues (41).
Koenig and colleagues (42).
Canada and colleagues (43).
Radloff (27).
Spanier (44).
Adherence determinants
Various adherence determinants were measured with standardized questionnaires, including parental attitude toward treatment, perceived behavioral norms, motivation, self-efficacy, and adherence intentions. Additional details about these scales, including score ranges and examples of questions, can be found in Table 2.
Table 2.
Measurements of parental adherence determinants
| Adherence Determinant | Scale Used | Score Range | Examples |
|---|---|---|---|
| Treatment attitude | Adherence Determinants Questionnaire–Perceived Utility Subscale* | 8–40 (Likert) | “I believe that my child’s treatment plan will prevent an exacerbation.” |
| Motivation | Theory of reasoned action (one item)† | 1–7 (Likert) | “When it comes to my child’s health, I want to do/don’t want to do what my child’s pulmonologist thinks I should do.” |
| Perceived behavioral norms | Theory of reasoned action† | 3–21 (Likert) | “Most people who are important to me think I should/should not make sure my child’s airway clearance gets done the number of times recommended by our doctor each day.” |
| Self-efficacy | Created from Bandura’s guidelines‡ | 0–1,100 | “Please rate how certain you are that you can make sure that your child does his/her treatment the number of times recommended by your doctor each day.” |
| Adherence intentions | Theory of reasoned action (three items)† | 3–21 | “I intend to have my child do airway clearance the number of times recommended by our doctor each day over the next month.” |
Adherence rates
Parental treatment behavior was measured using the DPD to obtain the number of ACT and NM treatments completed (4, 20). This semistructured telephone interview uses a cued recall system in which participants recount all events of at least 5 minutes’ duration during the past 24 hours and gives the event, duration, number and relationship(s) of other people present, mood, and classification of the event as recreational or instrumental. Inquiry into all events of each day theoretically “blinds” participants to the behaviors of interest and decreases the likelihood of giving a false response that is socially acceptable. The DPD is commonly used to study CF treatment adherence, and it has established psychometric properties, including test–retest reliability (20), interrater reliability greater than 90% (21), and convergent validity when compared with electronic monitoring (22). Adherence is calculated as the ratio of treatments completed per DPD to treatment prescribed at the clinic appointment at which enrollment occurred. Participants were scheduled to complete three DPDs at their convenience during the 3 weeks immediately following questionnaire completion. Because treatment adherence can vary between weekdays and weekends (23), DPDs were planned to take place on one weekend day and two weekdays. Two coauthors (D.H.G. and S.D.) were trained to use the DPD by its developer (A.L.Q.).
Analytic Approach
Family-level variables were created to account for situations where two parents reported outcomes for the same child. Each family-level variable was calculated as the average of the two parents’ reported adherence measures by DPD. For each family unit, the average numbers and duration of ACT and NM administered over the 3 days were calculated. Each of these average values was then divided by the corresponding prescribed treatment frequency or duration, which was obtained by chart review. Differences between parental answers for each variable were assessed using the Wilcoxon signed-rank test. Descriptive analyses were performed with calculation of mean (M), standard deviation (SD), median, and interquartile range (IQR) for each continuous variable. Each categorical variable was summarized with frequency and percentage data. K-means clustering was performed to determine the number of distinct adherence groups (clusters) for each type of adherence measure. Post hoc assessment of clustering solutions for each type of adherence measure suggested that underlying subpopulations were not normally distributed.
To avoid making distribution assumptions necessary for calculating traditional information criteria, the optimal number of adherence groups within a treatment modality was obtained by assessing the sum of squared errors (SSE) and proportion of variance explained for each analysis (24, 25). The K-means cluster analyses were implemented using RStudio Version 3.0.2 software (R Project for Statistical Computing, Vienna, Austria). All other analyses were conducted using SAS 9.3 software (SAS Institute, Cary, NC).
Results
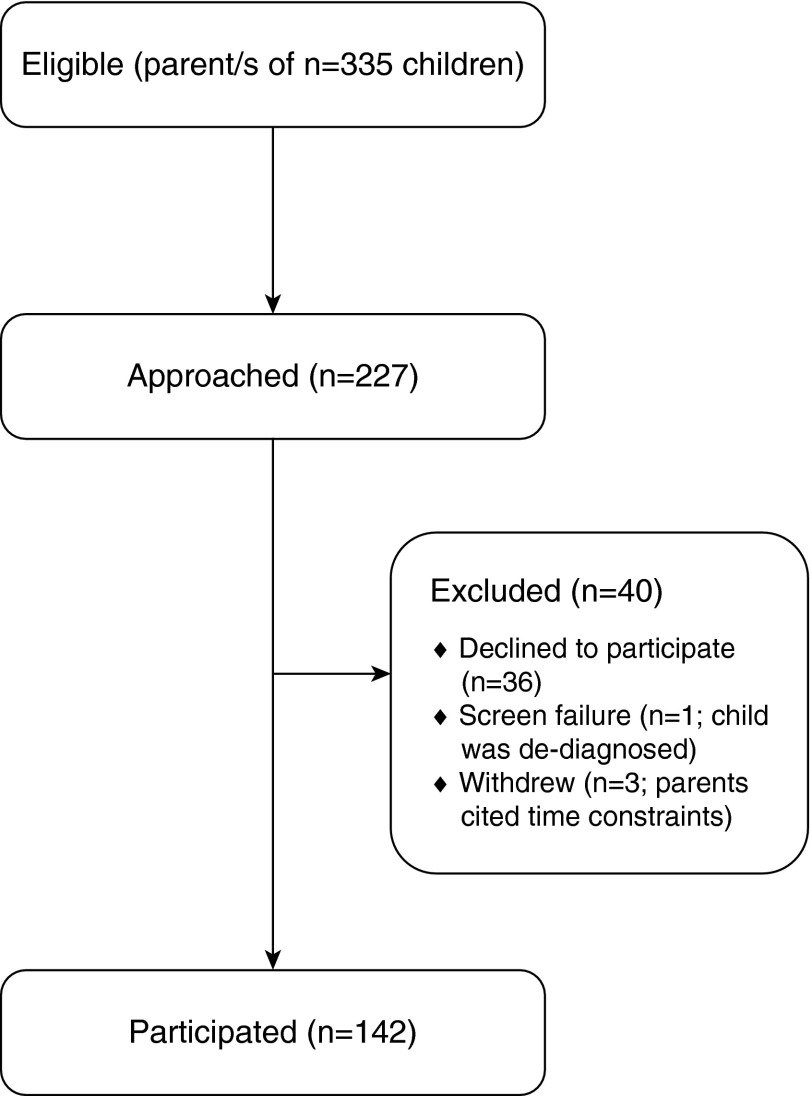
A total of 142 parents—83 from Site 1 (58%) and 59 from Site 2 (42%)—completed the study (see Figure 2). Demographic information and clinical data for their children are presented in Table 3. Compared with the U.S. population as a whole, evangelical and mainline Protestants were overrepresented (34% and 30%, respectively, compared with 26% and 18% in the U.S. general population), whereas Roman Catholics were underrepresented (18% compared with 24% in the U.S. general population) (26). Measures of background factors and adherence determinants with aggregate value and range of scores on psychosocial, R/S, and adherence determinant questionnaires are provided in Table E1 in the online supplement. Graphical assessments of the SSE for various cluster solutions identified different clusters for the two treatment modalities (ACT and NM; see Figures 3 and 4). The psychosocial and R/S variables that were associated with the two treatment modalities were different. The prevalence of depressive symptoms (participants scoring above the usual cutoff value of 16 for clinically significant symptoms) was 47% (27). The overall mean score on the Center for Epidemiologic Studies Depression Scale was 16.2 (SD = 11.5). Participants at Site 1 had a significantly higher level of depressive symptoms (M = 17.9; SD = 12.0) than those at Site 2 (M = 13.5; SD = 10.4) (P = 0.04). Mothers reported significantly more symptoms (M = 17.6; SD = 11.9) than did fathers (M = 12.4; SD = 9.9) (P = 0.03). There were 31 parent dyads in the sample. Dyads had similar responses for all variables except positive religious coping (P = 0.045). Men had slightly lower scores than women.
Figure 2.
Participant enrollment diagram.
Table 3.
Demographic data of sample and clinical data of children
| Variable | Aggregate Value | Site 1 | Site 2 | |
|---|---|---|---|---|
| Percent female (parent)* |
72% | 75% | 67% | |
| Religious affiliation | ||||
| Nondenominational Christian | 47 (34) | 26 (19) | 19 (14) | |
| Roman Catholic | 25 (18) | 18 (13) | 4 (7) | |
| Protestant | 42 (30) | 28 (20) | 14 (10) | |
| Orthodox Christian | 3 (2) | 1 (1) | 2 (4) | |
| Jewish | 1 (1) | 1 (1) | 0 (0) | |
| Mormon | 1 (1) | 1 (1) | 0 (0) | |
| None | 24 (17) | 20 (14) | 4 (3) | |
| Child sex (female)* |
66 (47) | 33 (44) | 25 (46) | |
| Child age (yr)† |
5.70 (4.09) | 5.69 (4.44) | 5.44 (3.57) | |
| Number of exacerbations in past 12 mo† | 0.93 (1.39)‡ | 0.57 (1.1) | 1.42 (1.6) | |
Values are n (%). Total sample = 142.
Values are mean (SD).
Between-sites means significant at P < 0.001.
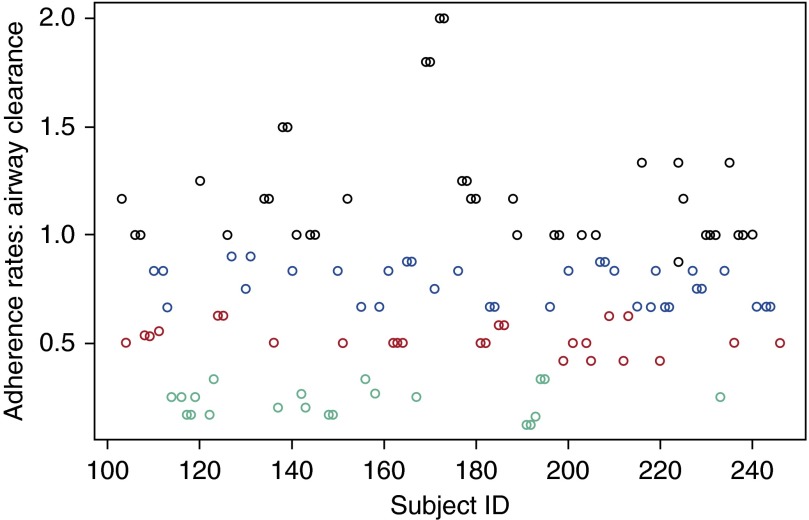
Figure 3.
Four-cluster model of parents’ adherence to their child’s prescribed daily frequency of airway clearance treatments.
Figure 4.
Three-cluster model of parents’ adherence to their child’s prescribed daily frequency of nebulized medication treatments.
Airway Clearance
A four-cluster model provided the best fit for ACT. The four adherence groups (characterized by mean adherence rates) were low-adherent (23%), medium-adherent (52%), high-adherent (77%), and superadherent (120%) parents. The mean adherence rate for each cluster and significant differences in predictors between clusters are shown in Table 4. Complete questionnaire data are given in Table E2. Superadherent parents were significantly less likely to imbue their child’s body with sacred significance (as a manifestation of God) than were high-adherent parents. Medium-adherent parents had significantly lower levels of depressive symptoms than low-adherent, high-adherent, or superadherent parents. Low-adherent parents were less influenced by their perceptions of the expectations of other parents of children with CF regarding ACT than were high-adherent parents. Low-adherent parents reported significantly lower self-efficacy for completing their child’s ACT treatments than did medium-adherent, high-adherent, and superadherent parents.
Table 4.
Predictor variables for airway clearance adherence clusters
| Group 1 (Low Adherence) | Group 2 (Medium Adherence) | Group 3 (High Adherence) | Group 4 (Superadherence) | |||
|---|---|---|---|---|---|---|
| Continuous | |
|||||
| Depressive symptoms (CES-D) |
15.0 (10.5–24.3) | 9.0* (4.0–22.0) | 19.5 (9.75–28.0) | 16.0 (7.5–21.0) | ||
| Sanctification of the body (manifestation of God in child’s body) |
60.0 (48.8–71.0) | 70.0 (56.5–77.0) | 72.0 (59.0–77.0) | 58.0† (49.0–77.0) | ||
| Perceived behavioral norms (other parents of children with CF) |
14.5‡ (12.3–15.0) | 15.0 (13.5–15.0) | 15.0 (15.0–15.0) | 15.0 (13.5–15.0) | ||
| Perceived behavioral norms (airway clearance) |
18.0‡ (16.0–18.0) | 18.0 (18.0–18.0) | 18.0 (18.0–18.0) | 18.0 (17.0–18.0) | ||
| Self-efficacy for completing airway clearance treatment |
856.0§ (801.8–958.5) | 1,077.0 (1,044.0–1,095.8) | 1,080.5‡ (1,027.5–1,097.3) | 1,085.0‖ (974.0–1,098.5) | ||
| Child age |
2.5 (1.6–10.5) | 6.4* (4.0–9.3) | 2.8 (1.7–5.1) | 5.3 (2.5–7.6) | ||
| Categorical | |
|||||
| Parent age‡, yr | 18–25 | 4 (19%) | 1 (4%) | 2 (6%) | 3 (8%) | |
| 26–30 | 2 (10%) | 5 (20%) | 7 (21%) | 8 (22%) | ||
| 31–35 | 5 (24%) | 8 (32%) | 18 (53%) | 10 (27%) | ||
| 36–40 | 7 (33%) | 4 (16%) | 2 (6%) | 11 (30%) | ||
| 41–45 | 1 (5%) | 4 (16%) | 4 (12%) | 4 (11%) | ||
| 46 and older | 2 (10%) | 3 (12%) | 1 (3%) | 1 (3%) | ||
| Parent education level§ | Some high school | 3 (15%) | 0 (0%) | 3 (9%) | 0 (0%) | |
| High school graduate | 5 (25%) | 3 (12%) | 6 (18%) | 8 (22%) | ||
| Some college | 7 (35%) | 4 (16%) | 13 (38%) | 12 (32%) | ||
| College graduate | 4 (20%) | 14 (56%) | 9 (26%) | 15 (41%) | ||
| Graduate school | 1 (5%) | 4 (16%) | 3 (9%) | 2 (5%) | ||
| Collaborative religious coping‖ | Not at all | 5 (25%) | 5 (20%) | 6 (18%) | 4 (11%) | |
| Somewhat | 8 (40%) | 7 (28%) | 11 (32%) | 14 (38%) | ||
| Quite a bit | 1 (5%) | 6 (24%) | 7 (21%) | 13 (35%) | ||
| A great deal | 6 (30%) | 7 (28%) | 10 (29%) | 6 (16%) | ||
| Number of exacerbations in prior years‡,§,‖ | 0 | 16 (76%) | 11 (44%) | 20 (59%) | 17 (46%) | |
| 1 | 2 (10%) | 7 (28%) | 6 (18%) | 8 (22%) | ||
| 2 | 0 (0%) | 4 (16%) | 7 (21%) | 9 (24%) | ||
| 3 | 0 (0%) | 1 (4%) | 0 (0%) | 1 (3%) | ||
| 4 | 1 (5%) | 0 (0%) | 0 (0%) | 2 (5%) | ||
| 5 | 2 (10%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| 6 | 0 (0%) | 1 (4%) | 1 (3%) | 0 (0%) | ||
| 7 | 0 (0%) | 1 (4%) | 0 (0%) | 0 (0%) | ||
Definition of abbreviation: CES-D = Center for Epidemiologic Studies Depression Scale; CF = cystic fibrosis.
Data are presented as median (interquartile range) or number (%).
Represents significant difference (P ≤ 0.05) between Group 2 and Group 3.
Represents significant difference (P ≤ 0.05) between Group 3 and Group 4.
Represents significant difference (P ≤ 0.05) between Group 1 and Group 3.
Represents significant difference (P ≤ 0.05) between Group 1 and Group 2.
Represents significant difference (P ≤ 0.05) between Group 1 and Group 4.
Nebulized Medication
A three-cluster model provided the best fit to the NM data, with clusters of low-adherent (35%), high-adherent (82%), and superadherent (130%) parents (see Figure 3). The mean adherence rate for each cluster and significant differences in predictors between clusters are shown in Table 5. Complete questionnaire data are shown in Table E3. There were significant between-cluster differences in the mean values of several predictors of adherence. Low-adherent parents reported increased use of negative religious coping compared with high-adherent parents. Unexpectedly, superadherent parents reported significantly higher use of negative religious coping styles than high-adherent parents did. High-adherent parents imbued their child’s body with sacred significance significantly higher than low-adherent parents did, seeing their child’s body as a manifestation of God as well as attributing sacred qualities to their child’s body. High-adherent parents reported higher feelings of self-efficacy than did low-adherent parents. High-adherent parents had higher intentions to complete their child’s NM than did superadherent parents.
Table 5.
Predictor variables for nebulized medication adherence clusters
| Group 1 (Low Adherence) | Group 2 (High Adherence) | Group 3 (Superadherence) | ||
|---|---|---|---|---|
| Continuous | ||||
| Negative religious coping (Brief RCOPE) | 4.5* (1.3–8.8) | 1.0† (0.0–3.0) | 0.0‡ (0.0–1.3) | |
| Sanctification of the body (manifestation of God in child’s body) | 60.0* (45.8–69.5) | 77.0 (61.0–77.0) | 59.0 (53.3–77.0) | |
| Sanctification of the body (sacred qualities of child’s body) | 55.5* (35.8–68.8) | 68.0 (53.5–76.3) | 62.0 (53.0–77.0) | |
| Self-efficacy for completing nebulized medication | 1,080.0* (1,003.0–1,097.0) | 1,093.0 (1,070.0–1,100.0) | 1,096.0 (1,068.5–1,100.0) | |
| Intentions to complete nebulized medication | 21.0 (21.0–21.0) | 21.0† (21.0–21.0) | 21.0 (18.0–21.0) | |
| Categorical | ||||
| Self-directed religious coping*,‡ | ||||
| 0 | 8 (25%) | 17 (52%) | 14 (67%) | |
| 1 | 16 (50%) | 14 (42%) | 4 (19%) | |
| 2 | 5 (16%) | 0 (0%) | 1 (5%) | |
| 3 | 3 (9%) | 2 (6%) | 2 (10%) | |
| Number of pulmonary exacerbations in prior year† | ||||
| 0 | 16 (50%) | 20 (59%) | 10 (48%) | |
| 1 | 5 (16%) | 8 (24%) | 2 (10%) | |
| 2 | 5 (16%) | 3 (9%) | 8 (38%) | |
| 3 | 1 (3%) | 1 (3%) | 0 (0%) | |
| 4 | 1 (3%) | 2 (6%) | 0 (0%) | |
| 5 | 2 (6%) | 0 (0%) | 0 (0%) | |
| 6 | 1 (3%) | 0 (0%) | 1 (5%) | |
| 7 | 1 (3%) | 0 (0%) | 0 (0%) |
Definition of abbreviation: RCOPE = Religious Coping Scale.
Data are presented as median (interquartile range) or number (%).
Represents significant difference (P ≤ 0.05) between Group 1 and Group 2.
Represents significant difference (P ≤ 0.05) between Group 2 and Group 3.
Represents significant difference (P ≤ 0.05) between Group 1 and Group 3.
Furthermore, among those parents with children who were both performing ACT and taking NM, the type of cluster membership for one treatment modality did not correspond to the same type of cluster membership in another modality (e.g., parents who were superadherent to performing ACT were not necessarily superadherent to taking NM). This is evidenced by the difference in the optimal number of clusters for the two treatment modalities.
Discussion
Discrete clusters of parental rates of adherence to their child’s ACT and NM treatments were identified, together with significant differences in psychosocial and R/S variables between clusters. Parental depression was more prevalent than anticipated. The results suggested that treatment adherence is nuanced. Clinical conversations about adherence may need to be tailored to the person’s adherence patterns. For example, providing adherence-promoting guidance to someone with a baseline adherence of 20% requires a very different conversation from that with a parent who is adhering to 60% of the prescribed treatment plan.
A superadherent cluster was identified in this study; positive deviations represent parents who reported doing more treatments, on average, than were prescribed. Qualitative findings supporting such behavior have previously been reported (28). These parents have found ways to create and maintain a highly productive system of completing treatments. A great deal could be learned from these parents about the development and maintenance of treatment routines.
Self-efficacy was the only theoretical adherence determinant that differed significantly between adherence clusters. The between-cluster differences likely represent clinically meaningful differences, making self-efficacy a candidate for future interventions. Motivational interviewing and problem-solving skills training (29) have demonstrated effectiveness and could be used to explore ways interested parents might learn and try new means of increasing their sense of mastery of their child’s treatments.
Depression is a known significant comorbidity among parents of children with CF (30, 31). Though the survey used in the present study is meant to be a screening tool for depression, we found that almost half of the parents in this study were above the clinical cutoff for depressive symptoms. Only medium-adherent parents had low levels of depressive symptoms (not near or above the cutoff value). Depression may contribute to the challenge of adherence for some parents. There is currently an international guidelines group working on implementation of annual screening of these symptoms in both patients with CF and parent caregivers of children with CF (32). Screening parents for depressive symptoms, with referral to a psychologist for assessment, could potentially decrease this comorbidity.
The between-cluster differences in negative religious coping are clinically meaningful. Negative religious coping has been associated with poorer health outcomes in other studies (33–35). In our present study, we also found that religious coping styles that were more negative were associated with worse adherence (33–35). However, what was unexpected was that superadherent parents reported using negative religious coping more frequently than high-adherent parents did. Perhaps negative religious coping styles create increased parental anxiety or a perception that their child’s health is up to them (without divine or congregational support), and this motivates these parents’ superadherent behaviors. R/S beliefs have been shown to be modifiable and have been associated with improved health outcomes (36–38). On the basis of these findings, when parental adherence is suspected to be poor, we recommend, as part of a complete evaluation, referral to a clinically trained, board-certified chaplain for assessment and clarification of whether negative or passive deferring styles of religious coping may contribute to poor adherence. Perceiving one’s body with R/S-related qualities has been connected to positive health behaviors (17). Our findings extend this to the perception of R/S-related qualities in the child’s body. Body sanctification offers a potentially useful construct to frame some adherence interventions.
Religious demographic data are not systematically collected by the Cystic Fibrosis Foundation Registry. The samples used in this study had a larger percentage of Protestant participants than that represented in the U.S. general population. Future studies should include more diverse samples. It may be that different spiritually or religiously based proadherence interventions are needed to properly address the religious diversity within the CF population. As with any intervention, R/S-based interventions should demonstrate cultural competence, taking into account the particular assets and needs of those for whom it is intended. Similar to responding differently based on which cluster of adherence behaviors a parent belongs to, more than a one-size-fits-all approach to R/S-based intervention is needed. This underscores the importance of collecting religious demographic data from this population in the future.
This study has limitations. The cross-sectional design allowed for associations between variables, but not causality, to be determined. In general, adherence measures are a surrogate representation of actual adherence behaviors and inherently may not be completely accurate, albeit there is no “perfect” measure of adherence behavior. The DPD, though a validated measure, provides parent-reported data and is subject to reporting bias. As stated previously, the DPD is one of the best and most feasible approaches to assessing adherence to treatment behaviors (such as airway clearance rates). The two-center sample may not be representative of parents at CF centers as a whole. Nonresponder data were unavailable, and the degree to which our sample is representative of the whole population at these sites could not be calculated. As previously noted, a limitation of the study is the predominately Christian religious demographic of the sample and the lack of population-level data for comparison, making it difficult to judge the extent to which our sample is similar to the CF population. Cluster analysis is an exploratory approach and therefore has limitations. A validation study would be necessary to determine the reproducibility of adherence clusters found in this cohort.
Nevertheless, important conclusions can be drawn. We have shown that parental self-efficacy and certain forms of R/S and coping styles, as well as parental depression, are associated with treatment adherence. Further, adherence rates were not normally distributed, but fell into discrete clusters. Future studies should include multivariate clustering of adherence to different treatment modalities and longitudinal designs exploring causality, as well as potential interactions between spiritual constructs and the disease course over time. Acceptability and feasibility of interventions targeted to the needs of parents at different levels of adherence and including the between-cluster differences may also be beneficial. Intervention studies have demonstrated that R/S components are modifiable and show positive outcomes 38–40). Adherence-promoting interventions using the findings of this study for parents of children with CF are currently underway.
Acknowledgments
Acknowledgments
The authors gratefully acknowledge the contributions by a medical writer, J. Denise Wetzel, in her critical review of the manuscript; Dan Li for assistance with statistical analyses; Nichole Dalessandro, Cody Hanson, and Sarah Lohbeck for assistance with data entry; Stephanie Gamble for assistance with recruitment and data collection; and especially the parents who participated in this study.
Footnotes
Partially supported by the following Eunice Kennedy Shriver National Institute of Child Health and Human Development Grant K23 HD062642 and National Center for Research Resources Grant UL1 RR026314.
Author Contributions: D.H.G., R.D.S., and M.S. were involved in the conception, hypotheses delineation and study design. D.H.G., R.D.S., L.L.B., A.L.Q., B.A.C., S.M.D., and M.S. were involved in data analysis and interpretation. D.H.G., R.D.S., L.L.B., A.L.Q., B.A.C., S.M.D., and C.M.S. were involved in writing the manuscript.
This article has a data supplement, which is accessible from this issue’s table of contents online at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Quittner AL, Zhang J, Marynchenko M, Chopra PA, Signorovitch J, Yushkina Y, Riekert KA. Pulmonary medication adherence and health-care use in cystic fibrosis. Chest. 2014;146:142–151. doi: 10.1378/chest.13-1926. [DOI] [PubMed] [Google Scholar]
- 2.Sawicki GS, Tiddens H. Managing treatment complexity in cystic fibrosis: challenges and opportunities. Pediatr Pulmonol. 2012;47:523–533. doi: 10.1002/ppul.22546. [DOI] [PubMed] [Google Scholar]
- 3.Berg JS, Dischler J, Wagner DJ, Raia JJ, Palmer-Shevlin N. Medication compliance: a healthcare problem. Ann Pharmacother. 1993;27(9 Suppl):S1–S24. [PubMed] [Google Scholar]
- 4.Modi AC, Lim CS, Yu N, Geller D, Wagner MH, Quittner AL. A multi-method assessment of treatment adherence for children with cystic fibrosis. J Cyst Fibros. 2006;5:177–185. doi: 10.1016/j.jcf.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Modi AC, Cassedy AE, Quittner AL, Accurso F, Sontag M, Koenig JM, Ittenbach RF. Trajectories of adherence to airway clearance therapy for patients with cystic fibrosis. J Pediatr Psychol. 2010;35:1028–1037. doi: 10.1093/jpepsy/jsq015. [DOI] [PubMed] [Google Scholar]
- 6.Smith BA, Modi AC, Quittner AL, Wood BL. Depressive symptoms in children with cystic fibrosis and parents and its effects on adherence to airway clearance. Pediatr Pulmonol. 2010;45:756–763. doi: 10.1002/ppul.21238. [DOI] [PubMed] [Google Scholar]
- 7.DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23:207–218. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- 8.Quittner AL, Tolbert VE, Regoli MJ, Orenstein DM, Hollingsworth JL, Eigen H. Development of the role-play inventory of situations and coping strategies for parents of children with cystic fibrosis. J Pediatr Psychol. 1996;21:209–235. doi: 10.1093/jpepsy/21.2.209. [DOI] [PubMed] [Google Scholar]
- 9.Hill PC, Pargament KI, Hood RW, Jr, McCullough ME, Swyers JP, Larson DB, Zinnbauer BJ. Conceptualizing religion and spirituality: points of commonality, points of departure. J Theory Soc Behav. 2000;30:51–77. [Google Scholar]
- 10.Konkle-Parker DJ, Erlen JA, Dubbert PM. Barriers and facilitators to medication adherence in a southern minority population with HIV disease. J Assoc Nurses AIDS Care. 2008;19:98–104. doi: 10.1016/j.jana.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kemppainen J, Kim-Godwin YS, Reynolds NR, Spencer VS. Beliefs about HIV disease and medication adherence in persons living with HIV/AIDS in rural southeastern North Carolina. J Assoc Nurses AIDS Care. 2008;19:127–136. doi: 10.1016/j.jana.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 12.Parsons SK, Cruise PL, Davenport WM, Jones V. Religious beliefs, practices and treatment adherence among individuals with HIV in the southern United States. AIDS Patient Care STDS. 2006;20:97–111. doi: 10.1089/apc.2006.20.97. [DOI] [PubMed] [Google Scholar]
- 13.Thomas CM. The influence of self-concept on adherence to recommended health regimens in adults with heart failure. J Cardiovasc Nurs. 2007;22:405–416. doi: 10.1097/01.JCN.0000287037.85067.3d. [DOI] [PubMed] [Google Scholar]
- 14.Grossoehme DH, Ragsdale J, Wooldridge JL, Cotton S, Seid M. We can handle this: parents’ use of religion in the first year following their child’s diagnosis with cystic fibrosis. J Health Care Chaplain. 2010;16:95–108. doi: 10.1080/08854726.2010.480833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fishbein M, Ajzen I. New York: Psychology Press; 2010. Predicting and changing behavior: the reasoned action approach. [Google Scholar]
- 16.Grossoehme DH, Opipari-Arrigan L, VanDyke R, Thurmond S, Seid M. Relationship of adherence determinants and parental spirituality in cystic fibrosis. Pediatr Pulmonol. 2012;47:558–566. doi: 10.1002/ppul.21614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahoney A, Carels RA, Pargament KI, Wachholtz A, Leeper LE, Kaplar M, Frutchey R. The sanctification of the body and behavioral health patterns of college students. Int J Psychol Relig. 2005;15:221–238. [Google Scholar]
- 18.Pendleton SM, Cavalli KS, Pargament KI, Nasr SZ. Religious/spiritual coping in childhood cystic fibrosis: a qualitative study. Pediatrics. 2002;109:E8. doi: 10.1542/peds.109.1.e8. [DOI] [PubMed] [Google Scholar]
- 19.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Quittner AL, Opipari LC. Differential treatment of siblings: interview and diary analyses comparing two family contexts. Child Dev. 1994;65:800–814. doi: 10.1111/j.1467-8624.1994.tb00784.x. [DOI] [PubMed] [Google Scholar]
- 21.Quittner AL, Opipari LC, Espelage DL, Carter B, Eid N, Eigen H. Role strain in couples with and without a child with a chronic illness: associations with marital satisfaction, intimacy, and daily mood. Health Psychol. 1998;17:112–124. doi: 10.1037//0278-6133.17.2.112. [DOI] [PubMed] [Google Scholar]
- 22.Quittner AL, Modi AC, Lemanek KL, Ievers-Landis CE, Rapoff MA. Evidence-based assessment of adherence to medical treatments in pediatric psychology. J Pediatr Psychol. 2008;33:916–938. doi: 10.1093/jpepsy/jsm064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ball R, Southern KW, McCormack P, Duff AJA, Brownlee KG, McNamara PS. Adherence to nebulised therapies in adolescents with cystic fibrosis is best on week-days during school term-time. J Cyst Fibros. 2013;12:440–444. doi: 10.1016/j.jcf.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 24.Hartigan JA, Wong MA. Algorithm AS 136: A K-means clustering algorithm. Appl Stat. 1979;28:100–108. [Google Scholar]
- 25.MacQueen J. Some methods for classification and analysis of multivariate observations. In: Le Cam LM, Neyman J, editors. Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability. Vol. 1: Statistics. Berkeley, CA: University of California Press; 1967. pp. 281–297. [Google Scholar]
- 26.Pew Forum on Religion & Public LifeU.S. religious landscape survey. Religious affiliation: diverse and dynamic. Washington, DC: Pew Forum on Religion & Public Life; February 2008 [accessed 2015 Apr 3]. Available from: http://religions.pewforum.org/pdf/report-religious-landscape-study-full.pdf
- 27.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 28.Grossoehme DH, Cotton S, Ragsdale J, Quittner AL, McPhail G, Seid M. “I honestly believe God keeps me healthy so I can take care of my child”: parental use of faith related to treatment adherence. J Health Care Chaplain. 2013;19:66–78. doi: 10.1080/08854726.2013.779540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duff AJA, Latchford GJ. Motivational interviewing for adherence problems in cystic fibrosis. Pediatr Pulmonol. 2010;45:211–220. doi: 10.1002/ppul.21103. [DOI] [PubMed] [Google Scholar]
- 30.Quittner AL, Barker DH, Geller D, Butt S, Gondor M. Effects of maternal depression on electronically monitored enzyme adherence and changes in weight for children with CF [abstract 319] J Cyst Fibros. 2007;6(Suppl 1):S78. [Google Scholar]
- 31.Quittner AL, Goldbeck L, Abbott J, Duff A, Lambrecht P, Solé A, Tibosch MM, Bergsten Brucefors A, Yüksel H, Catastini P, et al. Prevalence of depression and anxiety in patients with cystic fibrosis and parent caregivers: results of The International Depression Epidemiological Study across nine countries. Thorax. 2014;69:1090–1097. doi: 10.1136/thoraxjnl-2014-205983. [DOI] [PubMed] [Google Scholar]
- 32.Smyth AR, Bell SC, Bojcin S, Bryon M, Duff A, Flume P, Kashirskaya N, Munck A, Ratjen F, Schwarzenberg SJ, et al. European Cystic Fibrosis Society Standards of Care: Best Practice guidelines. J Cyst Fibros. 2014;13(Suppl 1):S23–S42. doi: 10.1016/j.jcf.2014.03.010. [DOI] [PubMed] [Google Scholar]
- 33.Thuné-Boyle ICV, Stygall J, Keshtgar MRS, Davidson TI, Newman SP. Religious/spiritual coping resources and their relationship with adjustment in patients newly diagnosed with breast cancer in the UK. Psychooncology. 2013;22:646–658. doi: 10.1002/pon.3048. [DOI] [PubMed] [Google Scholar]
- 34.Webb M, Charbonneau AM, McCann RA, Gayle KR. Struggling and enduring with God, religious support, and recovery from severe mental illness. J Clin Psychol. 2011;67:1161–1176. doi: 10.1002/jclp.20838. [DOI] [PubMed] [Google Scholar]
- 35.Tarakeshwar N, Pargament KI. Religious coping in families of children with autism. Focus Autism Other Dev Disabl. 2001;16:247–260. [Google Scholar]
- 36.Oemig Dworsky CK, Pargament KI, Reist Gibbel M, Krumrei EJ, Faigin CA, Gear Haugen MR, Desai KM, Lauricella SK, Quinten L, Warner HL. Winding road: preliminary support for a spiritually integrated intervention addressing college students’ spiritual struggles. In: Piedmont RL, Village A, editors. Research in the Social Scientific Study of Religion. Vol. 24. Leiden, The Netherlands: Brill; 2013. pp. 309–339. [Google Scholar]
- 37.Cole B, Pargament K. Re-creating your life: a spiritual/psychotherapeutic intervention for people diagnosed with cancer. Psychooncology. 1999;8:395–407. doi: 10.1002/(sici)1099-1611(199909/10)8:5<395::aid-pon408>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 38.Murray-Swank NA, Pargament KI. God, where are you? Evaluating a spiritually-integrated intervention for sexual abuse. Ment Health Relig Cult. 2005;8:191–203. [Google Scholar]
- 39.Pargament KI, McCarthy S, Shah P, Ano G, Tarakeshwar N, Wachholtz A, Sirrine N, Vasconcelles E, Murray-Swank N, Locher A, et al. Religion and HIV: a review of the literature and clinical implications. South Med J. 2004;97:1201–1209. doi: 10.1097/01.SMJ.0000146508.14898.E2. [DOI] [PubMed] [Google Scholar]
- 40.Margolin A, Beitel M, Schuman-Olivier Z, Avants SK. A controlled study of a spirituality-focused intervention for increasing motivation for HIV prevention among drug users. AIDS Educ Prev. 2006;18:311–322. doi: 10.1521/aeap.2006.18.4.311. [DOI] [PubMed] [Google Scholar]
- 41.Pargament KI, Koenig HG, Perez LM. The many methods of religious coping: development and initial validation of the RCOPE. J Clin Psychol. 2000;56:519–543. doi: 10.1002/(sici)1097-4679(200004)56:4<519::aid-jclp6>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 42.Koenig H, Parkerson GR, Jr, Meador KG. Religion index for psychiatric research. Am J Psychiatry. 1997;154:885–886. doi: 10.1176/ajp.154.6.885b. [DOI] [PubMed] [Google Scholar]
- 43.Canada AL, Murphy PE, Fitchett G, Peterman AH, Schover LR. A 3-factor model for the FACIT-Sp. Psychooncology. 2008;17:908–916. doi: 10.1002/pon.1307. [DOI] [PubMed] [Google Scholar]
- 44.Spanier GB. Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. J Marriage Fam. 1976;38:15–28. [Google Scholar]
- 45.DiMatteo MR, Hays RD, Gritz ER, Bastani R, Crane L, Elashoff R, Ganz P, Heber D, McCarthy W, Marcus A. Patient adherence to cancer control regimens: scale development and initial validation. Psychol Assess. 1993;5:102–112. [Google Scholar]
- 46.Bandura A. Guide for constructing self-efficacy scales. In: Pajares F, Urdan T, editors. Self-efficacy beliefs of adolescents. Greenwich, CT: Information Age Publishing; 2006. pp. 307–337. [Google Scholar]