Abstract
This article provides a simple overview of acute trigeminal pain for the non dentist.
This article does not cover oral mucosal diseases (vesiculobullous disorders) that may cause acute pain.
Dental pain is the most common in this group and it can present in several different ways.
Of particular interest for is that dental pain can mimic both trigeminal neuralgia and other chronic trigeminal pain disorders.
It is crucial to exclude these disorders whilst managing patients with chronic trigeminal pain.
Introduction
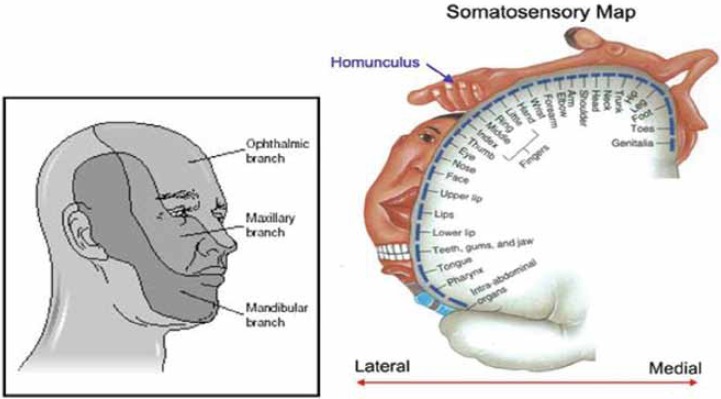
Orofacial pain is pain within the trigeminal system. The trigeminal nerve supplies general sensory supply to face, scalp, and mouth (Figure 1). A vast proportion of the sensory cortex represents the trigeminal input (over 40%).
Figure 1.
The trigeminal nerve sensory distribution and its representation in the sensory cortex
The trigeminal sensory region is very complex, incorporating the cranium, ears, eyes, sinuses, nose, pharynx, infratemporal fossa, jaw joint, teeth, jaws, salivary glands, oral mucosa, and skin. As many medical students are rarely exposed to ear, nose, and throat (ENT), otolaryngology, and dentistry, this region remains an enigma to most, with their singular experience of trigeminal pain being based on trigeminal neuralgia in relation to neurosurgical procedures.
Aetiology of acute orofacial pain
Orofacial pain can be associated with pathological conditions or disorders related to somatic and neurological structures. There are a wide range of causes of acute orofacial pain conditions, the most common being dental pain (toothache). Dental disease of the hard tissues (caries of enamel, dentine, and cementum), and soft tissues and supporting bone (gingivitis/periodontitis) are recognized as the most common diseases to afflict the general population. These conditions are largely diagnosed by dental practitioners by history, dental clinical examination, and radiographs. By far the most common forms of oral pain are the acute form of pains that tend to last for short periods of time. These include toothache (dental pulpitis), gum pain (pericoronitis in 80% of the population), periapical periodontitis (owing to apical infection or postendodontic therapy of high occlusal contact). Dentine sensitivity affects 40% of the adult population; dry socket is an intense postsurgical pain that affects 10% of patients after extraction of their teeth. Other orofacial acute pain conditions include trauma or infection of the orofacial tissues.
Odontogenic pain
Odontogenic pain refers to pain initiating from the teeth or their supporting structures, the mucosa, gingivae, maxilla, mandible or periodontal membrane.
‘A toothache, or a violent passion, is not necessarily diminished by our knowledge of its causes, its character, its importance or insignificance.’ TS Eliot
Toothache is caused by inflammation of the dental pulp (Figure 2), most commonly as a result of dental caries (tooth decay), the most common human infective disease worldwide, affecting 60–90% of school children worldwide.
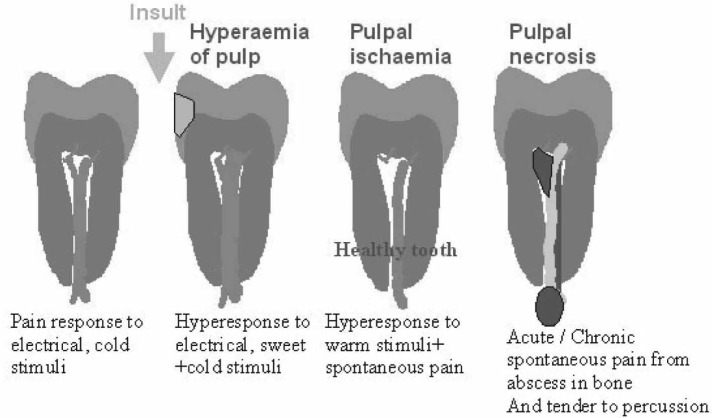
Figure 2.
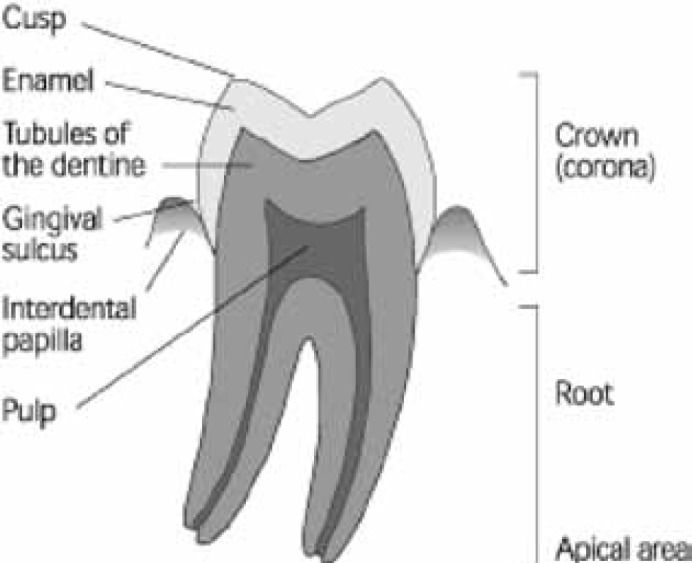
Diagram of a lower molar tooth
Periodontal disease (gum disease) is the second most common infection, and similar to chronic mycobacteria infections, for example Leprosy, is painless. The two bacteria appear to be particularly likely to cause aggressive periodontal disease. Both P gingivalis and A. actinomycetemcomitans, along with multiple deep pockets in the gum, are associated with resistance to standard treatments for gum disease. Other risk factors include smoking and there is very likely a genetic predisposition to developing this silent painless disease, which is the leading cause of tooth loss, and is found in 5–400% of middle-aged adults1. The diagnosis and management of this condition remain outwith this article's remit.
The role of all medical personnel in improving oral health in children is being recognised2. Caries is preventable using fluoride toothpaste and simple dietary advice such as reducing the frequency of sugar intake. Despite this, the numbers of children undergoing general anaesthetic for dental extractions due to caries continues to increase3,4.
Prevalence
The prevalence of dental pain and its characteristics were recorded using standard measures of pain (WHO criteria). In a study of 1,052 individuals the prevalence of reported toothache in schoolchildren in the last six months was 33.6% (31.1–36.8, 95% CI). Multiple logistic and ordinal polytomous regression analysis showed a significant association of both the prevalence and severity of dental pain with lower social class, later birth order, failure at school and attendance at the dentist only when in trouble. The major predictor of the prevalence and severity of pain was the pattern of dental attendance (p<0.001)5.
Dental pulpitis (‘toothache’)
In health, teeth only perceive pain due to dentine sensitivity to cold, sweet or physical stimulus. Dental pulpitis may be due to infection from dental caries close to the pulp (Figure 2, Figure 3), or by inflammation from chemical or thermal insult subsequent to dental treatment. It may be reversible or non-reversible. Intermittent sharp, shooting pains are also symptomatic of trigeminal neuralgia, so care must be taken not to mistakenly label toothache as neuralgia.
Figure 3.
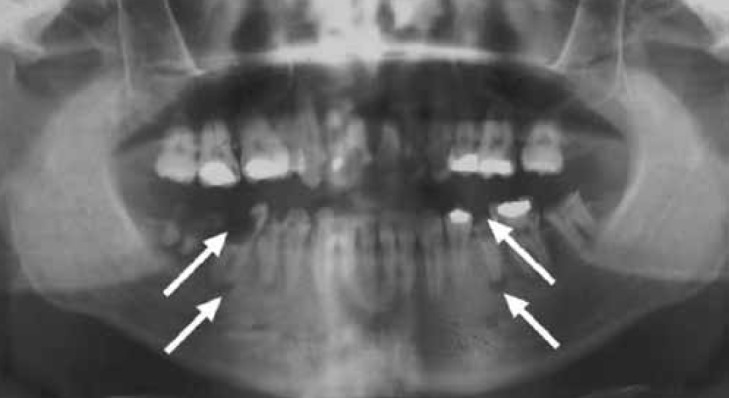
Dentalpantomograph (DPG) showing extensive dental caries (radiolucent areas in the tooth crowns and roots) affecting the crowns of several teeth, and periapical abscess formation (radiolucent areas at the end of the root). Arrows indicate caries and abscess formation on two mandibular teeth.
Insult of the tooth due to caries (causing bacterial products to infiltrate the pulp via the dentine tubules) or iatrogenic insult (dental restoration close to the dental pulp or trauma) will cause pulpal inflammation. This results in extreme sensitivity to cold and sweet flavours with short sharp ‘neuralgic’ pain. Protection of the pulp to bacterial infection and chemical irritation by dietary and salivary content must be undertaken promptly to minimise the risk of acute pulpitis evolving into chronic irreversible pulpitis. This treatment will involve a filling or restoration.
If the insult persists the pulpitis will become irreversible. The increased pulpal vascularity results in a rise in intra pulpal pressure, which induces ischaemia and sensitivity, with prolonged pain to heat. Once necrosis of the dental pulp has occurred, the infection spreads through the apex of the tooth into the surrounding bone and periodontal membrane, initiating periodontal inflammation and eventually a dental abscess causing spontaneous long lasting pain and pain on biting on the tooth. Typically the pain associated with an abscess is described as spontaneous aching or throbbing lasting hours sometime days. Associated swelling in the jaw, trismus or lymphadenopathy may be indicative of an acute spreading infection. Thus different stages of infection have different clinical presentations (Figure 4).
Figure 4.
The stages and characteristics of dental pulpal pain.
Management
Management for dental pulpitis is excavation of the tooth decay with restoration (filling). If the pulpitis becomes irreversible then pulpectomy (pulp removal) and root canal treatment will be required. Acute spreading infection may require additional drainage intra or extraorally via drainage of involved tissue tissue spaces.
Apical pain can be caused by infection spreading through the apical foramen of the tooth into the apical periodontal region causing inflammation (apical periodontitis) and ultimately a dental abscess if left untreated (Figure 4). This is treated by either root canal treatment of the tooth or extraction of the tooth with or without concomitant courses of antibiotics7. Iatrogenic apical pain may result after dental treatment including premature contact if a restoration is left high in occlusion. This is characterized by an initial sharp pain which becomes duller after a period. The pain is due to a recent tooth restoration that is ‘high’ compared with the normal occlusion when biting together and
Postendodontic surgery pain
This is severe aching pain following endodontic treatment such as root canal therapy or apicectomy. While the majority of patients improve over time (weeks), a few will develop a chronic neuropathic pain state (see section on persistent post surgical trigeminal pain). There is considerable variation in the pain reported by patients, but it commonly starts as a sharp stabbing pain that becomes progressively dull and throbbing. At first the pain may be caused by a stimulus, but it then becomes spontaneous and remains for a considerable time after removal of the stimulus. The pain may radiate and be referred to other areas of the mouth. This type of pain tends to cause the patient to have difficulty sleeping and may be exacerbated by lying down. Heat may make the pain worse whereas cold may alleviate it. The pain may be intermittent with no regular pattern and may have occurred over months or years. If there is periapical infection present, patients may no longer complain of pain in response to a thermal stimulus, but rather of sensitivity on biting.
Exposed cementum or dentine
There is tooth sensitivity from cold fluids and/or air, a reflection of a healthy pulp. With gingival recession, recent scaling, or tooth wear due to a high acid diet or gastric reflux, there may be generalised dentine sensitivity. However, with caries, fractured fillings and cracked cusps, the pain tends to be localised to the affected tooth. The tooth root surface comprises of a thin layer of cementum overlaying dentine, may be exposed from excessive and/or incorrect tooth brushing. Dentine underlying the enamel crown is constituted of tiny tubules which are fluid filled and connect directly to the nerve ending in the dental pulp. The current hypotheses for dental pain includes the osmolality theory, whereby the dentine fluids elicit an action potential within the A delta and C fibres in the pulp when stimulated by mechanical stimulation.
Management
For root sensitivity the use of a desensitising toothpaste and a reduction in acid in the diet will help resolve the symptoms. Modification of harmful tooth brushing habits that contribute to tooth abrasion is recommended. The use of a fluoride mouth-rinse may also help. In the case of caries, a lost filling or fractured tooth, coverage of the exposed dentine with a temporary restoration will usually relieve the symptoms.
Fractured tooth
If the crown of a tooth is fractured by trauma and the broken fragment is available, it should be stored in a physiological medium (milk) until a dentist can assess the patient. Coverage of exposed dentine on the fractured crown with a temporary restoration is desirable to protect the underlying pulp tissue6.
Placement of temporary restorations
Although it is unlikely that many general medical practitioners will have temporary filling materials available in their surgeries, dentine that has been exposed by caries, a lost filling or tooth fracture can be covered relatively easily with glass ionomer cement (GIC) or zinc oxide eugenol (ZOE) materials. Most GIC materials are dispensed in capsules but a hand-mixed material is available, consisting of a powder, liquid and conditioner. The surface of the cavity is painted with the conditioner, then rinsed and dried, before placement of the filling. Zinc oxide eugenol materials consist of a powder and liquid (oil of cloves) that are mixed to a putty-like consistency before placement in the tooth.
Pericoronitis
Pain commonly arises from the supporting gingivae and mucosa when infection arises from an erupting tooth (teething or pericoronitis). This is the most common cause for the removal of third molar teeth (wisdom teeth). The pain may be constant or intermittent, but is often evoked when biting down with opposing maxillary teeth. This elicits pain in the inflamed mucosa and gingivae surrounding the partially erupted tooth. If the infection is acute and spreading then antibiotics must be prescribed. Reccurrent pericoronitis is the main indication for removal of wisdom teeth8. Chronic periodontitis with gradual bone loss, rarely causes pain and patients may be unaware of the disorder until tooth mobility is evident. There is quite often bleeding from the gums and sometimes an unpleasant taste. Food impaction in these areas can cause localised gingival pain. Poor contact between adjacent teeth and the presence of an occluding cusp forcing food into this gap can also cause a build-up of food debris and result in gingival inflammation. This is usually a generalised condition, however, deep pocketing with extreme bone loss can occur around isolated teeth. Acute pericoronitis involves bacterial infection around an erupting orr partially erupted tooth and usually affects the lower third molar (wisdom tooth). The condition is often aggravated by the upper molar impacting on the swollen flap of soft tissue covering the unerupted tooth. There may be associated trismus due to the fact that the lower 8 site is close to the mandibular insertion of the temporalis muscle.
Management
Advise the use of an analgesic to relieve symptoms (ibuprofen), or if ibuprofen is contraindicated or unsuitable, paracetamol is recommended first-line. Paracetamol and ibuprofen can be taken together if pain relief with either alone is insufficient. For adults, if paracetamol and ibuprofen together does not provide enough pain relief, consider adding codeine phosphate or switching to an alternative nonsteroidal anti-inflammatory drug (NSAID). For women who are pregnant or breastfeeding, paracetamol is preferred. A short course of codeine may be added if paracetamol alone is insufficient. Antibiotics are generally not indicated for otherwise healthy individuals when there are no signs of spreading infection. Only prescribe an antibiotic for people who are systemically unwell or if there are signs of severe infection (e.g. fever, lymphadenopathy, cellulitis, diffuse swelling).
Dental management for dental abscess is either root canal procedure with removal of the necrotic pulp or tooth extraction. Periapical inflammation can lead to a cellulitis of the face characterised by a rapid spread of bacteria and their breakdown products into the surrounding tissues causing extensive oedema and pain. If systemic signs of infection are present, for example, fever and malaise, as well as swelling and possibly trismus (limitation of mouth opening), antibiotic treatment alone is not recommended as this is a surgical emergency. If pus is present, it needs to be drained, the cause eliminated, and host defences augmented with antibiotics. The microbial spectrum is mainly gram positive including anaerobes. Appropriate antibiotics would include a penicillin or a ‘first generation’ cephalosporin, combined with metronidazole in more severe cases.
Alveolar osteitis
After extraction, the most common complication is a ‘dry socket’ which is a condition whereby the clot formation within the socket fails at 3—5 days. Healing fails, resulting in an empty socket which traps food and debris. The resultant pain is caused by necrotic foodstuff aggravating bony nerve endings. Interestingly this condition is devoid of the usual acute inflammatory markers (absence of lymphadenopathy, local inflammation and swelling). A dull throbbing pain develops two to four days after a mandibular tooth extraction. It rarely occurs in the maxilla. Smoking is a major predisposing factor as it reduces the blood supply. The tissue around the socket is very tender and white necrotic bone is exposed in the socket. Halitosis is very common. The incidence of this condition is between 1–9%. Patients undergoing mandibular surgical tooth removal should be routinely warned of a possible incidence of 5%.
Management
Irrigation of the socket using saline or chlorhexidine and then an obtundant dressing usually soaked in bacteriorstatic solution (alvogyl paste, BIPP (bismuth iodoform paraffin paste), cotton wool or gauze soaked in iodoform). Immediate pain relief is usually attained and patients rarely re-present for additional treatment. Patients should be shown how to irrigate the area and told to do this regularly. Analgesics are indicated as pain may persist for several days. Although opinion is divided as to whether or not dry socket is an infective condition, we do not recommend the use of antibiotics. If the patient returns with ongoing pain then osteomyelitis should be excluded and localised bony sequestrate should be excluded.
Maxillary sinusitis ‘mimicking’ toothache
Recurrent maxillary sinusitis may cause widespread pain in the maxillary teeth. The pain tends to be increased on lying down or bending over. There is often a feeling of ‘fullness’ on the affected side. The pain is usually unilateral, dull, throbbing and continuous. Quite often the patient feels unwell generally and feverish. It can mimic the maxillary sinusitis-like symptoms in temporomandibular disorders (TMD)9 or neuropathic pain. These dental conditions rarely present as chronic pain unless misdiagnosed.
Management
Inflammation of the maxillary sinuses is best treated using local and systemic decongestants and, if persistent, antibiotics may be prescribed10. Pain originating from the sinus arises mainly from pressure. Decongestants can help sinus drainage. Antibiotics probably have only a minor role in mild cases. Referral to an otorhinolaryngologist for endoscopic sinus surgery may be indicated in chronic cases11.
Acute necrotising ulcerative gingivitis is a rapidly progressive infection of the gingival tissues that causes ulceration of the interdental gingival papillae. It can lead to extensive destruction. Usually young to middle-aged people with reduced resistance to infection are affected (diabetes, HIV infection, chemotherapy). Males are more likely to be affected than females, with stress, smoking and poor oral hygiene being predisposing factors. Halitosis, spontaneous gingival bleeding, and a ‘punched-out’ appearance of the interdental papillae are all important signs. The patients quite often complain of severe gingival tenderness with pain on eating and tooth brushing. The pain is dull, deep-seated and constant. The gums can bleed spontaneously and there is also an unpleasant taste in the mouth and obvious halitosis.
Management
As there is an acute infection with mainly anaerobic bacteria, treatment follows surgical principles and includes superficial debridement, use of chlorhexidine mouthwashes and a course of metronidazole tablets. Treating the contributing factors should prevent a recurrence.
Which tests can assist in diagnosis?
There are several simple tests that may assist in diagnosis of dental pain.
Pulp sensitivity test. Dry ice on a cotton bud, or an ordinary ice stick (made in a plastic or glass tube), is placed on the cervical third (neck region) of the tooth crown. A response (pain is the only sensory response from the dental pulp) to the stimulus indicates that the pulpal tissue is capable of transmitting nerve impulses and is vital. No response may indicate pulp necrosis.
Percussion test. Using an instrument handle, the tooth is tapped in the longitudinal axis. A painful response suggests possible periapical inflammation due to inflammatory sensitivity of the mechanosensory receptors in the periodontal membrane surrounding the tooth.
Probing. Placing a fine, blunt probe gently into the gingival sulcus surrounding the tooth enables the health of the gingival tissues to be assessed. Bleeding and/or sulcus depths greater than 3–4 mm indicate gum disease due to inflammation.
Mobility test. Holding a tooth firmly on the buccal (cheek) and lingual sides between the fingers enables mobility to be assessed. All teeth have a small amount of mobility (<0.5 mm), but visible movement suggests loss of bone support around the root of the tooth.
Palpation. Careful palpation around the area of concern may reveal tenderness and the type and extent of swelling.
Sinus formation. Chronic dental abscesses tend to drain buccally through the mucosa causing mucosal sinuses. Rarely lower mandibular teeth with chronic abscesses may drain buccally (below the buccinator muscle attachment) or inferiorly below the mylohyoid muscle resulting in dermal sinuses that are often mistaken for skin lesions remaining resistant to routine dermatological remedies.
Radiographic examination. If it is possible to obtain a screening radiograph, such as an orthopantomograph (Figure 2), this may assist in the diagnosis and localisation of the cause of the pain. The radiograph should show clearly the apical and periapical structures of teeth and associated tissues. The relationship of the maxillary molars and premolars to the floor of the maxillary sinus can be examined, and radiographs may reveal recurrent caries or periapical radiolucencies associated with an established infection (Figure 3).
Non-odontogenic facial pain
Non-odontogenic facial pain can be caused by inflammation due to tumour, infection, or trauma. Topographical classification is often applied to this complex region. Regions often presenting as orofacial pain complaints include the sinuses, salivary gland, ears, eyes, throat, mandibular, and maxillary bone pathology. Often in patients with chronic orofacial pain there will be multiple causes of discomfort including inflammatory odontogenic pain alongside a neuropathic, neurovascular or idiopathic cause. Thus dental knowledge is crucial in order to exclude common and easily treated odontogenic causes of pain.
References
- 1.World Health Organization World oral health report 2003. WHO, Geneva: Available from: http://www.who.int/oral_health/media/en/orh_report03_en.pdf [Accessed 17.01.2011] [Google Scholar]
- 2.Krol DM. Children's oral health and the role of the pediatrician Current Opinion in Pediatrics., 2010. Sep 30. [Epub ahead of print] PMID: 20885329 [DOI] [PubMed]
- 3.Ashley PF, Parry J, Parekh S, Al-Chihabi M, Ryan D. Sedation for dental treatment of children in the primary care sector (UK) British Dental Journal 2010; 208 (11) E21, 522–523 [DOI] [PubMed] [Google Scholar]
- 4.Albadri SS, Lee S, Lee GT, Llewelyn R, Blinkhorn AS, Mackie IC. The use of general anaesthesia for the extraction of children's teeth. Results from two UK dental hospitals European Archives of Paediatric Dentistry 2006; 7 (2) 110–115 [PubMed] [Google Scholar]
- 5.Goes PSA, Watt RG Hardy R, Sheiham A. The prevalence and severity of dental pain in 14–15 year old Brazilian schoolchildren Community Dental Health 2007; 24 (4) 217–224 [PubMed] [Google Scholar]
- 6.Auld DN, Wright GB. The initial management of dento-alveolar trauma in general dental practice Dental Update 2010; 37 (5) 286–288, 291–294 [DOI] [PubMed] [Google Scholar]
- 7.Abbott PV. Selective and intelligent use of antibiotics in endodontics. Australian Endodontic Journal 2000; 26 (1) 30–39 [DOI] [PubMed] [Google Scholar]
- 8.NICE. Guidance on the extraction of wisdom teeth. NICE, London: 2000. Available from: http://www.nice.org.uk/nicemedia/live/11385/31993/31993.pdf [Accessed 17.01.2011] [Google Scholar]
- 9.Durham J. Recent Advancements in Temporomandibular disorders (TMD). Reviews in Pain. 2011; 5 (1) 18–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arias-Irimia O, Barona-Dorado C, Santos-Marino J A, et al. Meta-analysis of the etiology of odontogenic maxillary sinusitis. Medicina Oral Patologia Oral y Cirugia Bucal 2010; 15 (1) 70–3 [DOI] [PubMed] [Google Scholar]
- 11.Wormald PJ. Treating acute sinusitis Australian Prescriber 2000; (23) 39–42 [Google Scholar]