Abstract
Traumatic amputations remain one of the most emotionally disturbing wounds of conflict, as demonstrated by their frequent use in films to illustrate the horrors of war. Unfortunately, they remain common injuries, particularly following explosions, and, in addition, many survivors require primary amputation for unsalvageable injuries or to save their life. A third group, late amputations, is being increasingly recognised, often as a result of the sequelae of complex foot injuries. This article will look at the epidemiology of these injuries and their acute management, complications and outcome.
Keywords: Acute pain, chronic pain, musculoskeletal pain, neuralgia, pain
Key points
Traumatic amputation remains very common following combat or terrorist wounding.
With the significant advances in resuscitation, proximal and multiple amputations are being increasingly seen in survivors.
As a result of the effects of the explosion, considerable tissue trauma occurs.
Nerve injury is common and, with time, the functional level of the amputee will fall.
These injuries remain a significant problem to health services following wars.
Introduction
Traumatic amputations remain one of the most emotionally disturbing wounds of conflict, as demonstrated by their frequent use in films to illustrate the horrors of war. Unfortunately, they remain common injuries, particularly following explosions, and, in addition, many survivors require primary amputation for unsalvageable injuries or to save their life. A third group, late amputations, is being increasingly recognised, often as a result of the sequelae of complex foot injuries. This article will look at the epidemiology of these injuries and their acute management, complications and outcome.
Epidemiology
In both Iraq and Afghanistan, improvised explosive devices (IEDs) became the insurgents’ weapon of choice, and were the most common cause of military deaths between 2008 and 2011.1 The recent conflicts have also been associated with an improvement in the survival rate following severe injury to unprecedented levels,2 as well as a change in wounding patterns from those previously documented.3 This has resulted in survivors with traumatic, and often multiple, amputations. The majority of these are due to explosions – when gases under high pressure are produced rapidly from a chemical material such as gunpowder or nitroglycerine. This high-pressure gas moves rapidly away from the site of the explosions in all directions. Although the exact mechanism of the traumatic amputation is uncertain, it is likely that the blast wind avulses the limb, possibly after the initial shock wave causes a fracture.4
These are common injuries, but were usually seen in fatalities rather than survivors. Mellor and Cooper reported 52 in 828 servicemen killed or injured by explosion in Northern Ireland, with an incidence of 20% in fatalities, but only 1.5% in survivors,5 and Hadden et al. reported a 1% incidence in 1532 consecutive survivors seen at the Royal Victoria Hospital in Belfast following terrorist bombings.6 These reports from Northern Ireland are also consistent with injuries following terrorist incidents elsewhere. Frykberg and Tepas reviewed 3357 casualties of 220 incidents from around the world and documented a 1.2% incidence of traumatic amputation,7 and Almogy et al., in a report from Israel, documented 153 deaths and 798 injured in 15 suicide bombings.8 Traumatic amputations occurred in 41% of those who died but only 1.3% of those who survived, with an odds ratio of 50.1.8 Similar figures have also been reported following the Spanish train bombings.9
These findings lead to the assumption that significant blast loading was required, and that this would cause such severe pulmonary damage that survival was unlikely. However, recent UK experience has demonstrated that haemorrhage, rather than lung injury, was the leading cause of death. As such, with the significant advances in haemorrhage control and resuscitation that have been made, survival is not only possible, but common.
As well as large explosions, such as terrorist bombings, traumatic amputations can be caused by smaller devices such as antipersonnel land mines. Antipersonnel mines may be buried and operated by stepping on them, or placed above ground, when they are commonly operated by (trip) wires. These are usually associated with a smaller explosive charge, and may also produce multiple fragments. Unlike the explosions described above, the majority of casualties will survive the injuries, even if evacuation and medical treatment are delayed.
Johnson et al., in a longitudinal study of 251 war casualties admitted to the Royal Thai Army Hospital Bangkok, documented that 120 were due to land mines.10 Of the 251 casualties, 99 sustained lower limb injuries, of which 79% were traumatic amputations. Of the 46 upper limb injuries, only 7% were traumatic amputations.
Upper limb traumatic amputations are commonly caused by handling small explosive devices. A retrospective analysis from the International Committee of the Red Cross (ICRC), of 757 victims of antipersonnel mines, has identified three patterns of injuries amongst survivors.11 Pattern 1 injuries occur when a buried mine is stepped on. Severe limb injuries, including traumatic amputations of the lower limbs, are common, as well as genital injuries. With pattern 2 injuries, the device explodes near the victim; this may be due to a buried mine activated by another individual or a pull-action mine that is placed above ground level and is activated by pulling on a wire connected to the device. Lower limb injuries occur, but are less severe than in pattern 1, with traumatic amputations less likely. Injuries to the head, chest and abdomen are common. Pattern 3 injuries occur when the device explodes whilst the victim is handling it. Severe facial and upper limb injuries are common in this group.
Civilian injuries
Although hospitals in Israel, and previously in Northern Ireland, frequently see victims of explosions, most civilian hospitals see traumatic amputations in victims of traffic accidents or work-related incidents.
Livingston, in a retrospective review of 42 patients with traumatic amputations, documented the mechanism of injury and site, as presented in Table 1.12
Table 1.
Incidence and site of traumatic amputation.
| Mechanism | % |
|---|---|
| Motor vehicle accident | 42.9 |
| Industrial | 26.2 |
| Motorcycle accident | 21.4 |
| Other | 9.5 |
| Site of amputation | |
| Above elbow | 10.6 |
| Below elbow | 19.2 |
| Above knee | 17.0 |
| Below knee | 53.2 |
Source: Livingston et al. (1994)12.
Maclean described 41 casualties with traumatic amputations following subway accidents, with a 95% survival rate.13 This is not surprising, as the casualties were usually stable on arrival at hospital and the most common site was an isolated below-knee amputation.
Unfortunately, traumatic amputations also occur in children. Loder reported 256 amputations in 235 children in the upper Midwestern United States over 20 years.14 Of the 256, 193 were major amputations, occurring above the ankle or wrist. The mechanism of injury and site are presented in Table 2.
Table 2.
Mechanism and site of traumatic amputation in children.
| Mechanism | Number |
|---|---|
| Lawnmower | 69 |
| Farm machinery | 57 |
| Motor vehicle accident | 38 |
| Train | 20 |
| Bomb/firework | 10 |
| Gunshot | 7 |
| Site of amputation | |
| Above elbow | 7 |
| Elbow disarticulation | 1 |
| Below elbow | 29 |
| Above knee | 31 |
| Knee disarticulation | 5 |
| Below knee | 89 |
Source: Loder (2004)14.
Management
The principles in the management of casualties with traumatic amputations are, in general, no different from those for other trauma patients. The primary survey of Airway, Breathing and Circulation take priority. In the military, in recognition that a combat-related casualty is far more likely to die of haemorrhage than airway problems, the priorities are changed. C<>ABC is practised with the initial priority being to stop life-threatening (Catastrophic) haemorrhage first.15
Surgical treatment of a traumatic amputation is the same as any military wounds. Debridement is carried out to excise all necrotic and foreign material and the wound should not be closed primarily. The techniques and specifics of the initial management are described elsewhere;16 however, one of the most significant differences between civilian injuries and blast-induced amputation is the level of soft-tissue disruption associated with the avulsed limb segment.
An explosion is a complex physical process that interacts with the musculoskeletal system to cause extensive injury through a combination of the blast wave, penetrating fragments and rapid bodily displacement. The resultant injuries affect all tissues, leading to significant soft-tissue loss. In a review of traumatic amputations following blast, Hull et al.17 reported that the levels of soft-tissue injury were commonly several levels proximal to the level of bone injury (one level was considered to be one-third of a limb segment). Our own recent experience is that the zone of soft tissue associated with traumatic amputations in casualties from Afghanistan was even greater than that reported in previous conflicts. This is probably related to the extensive use of IEDs in the most recent conflicts (Figure 1).
Figure 1.
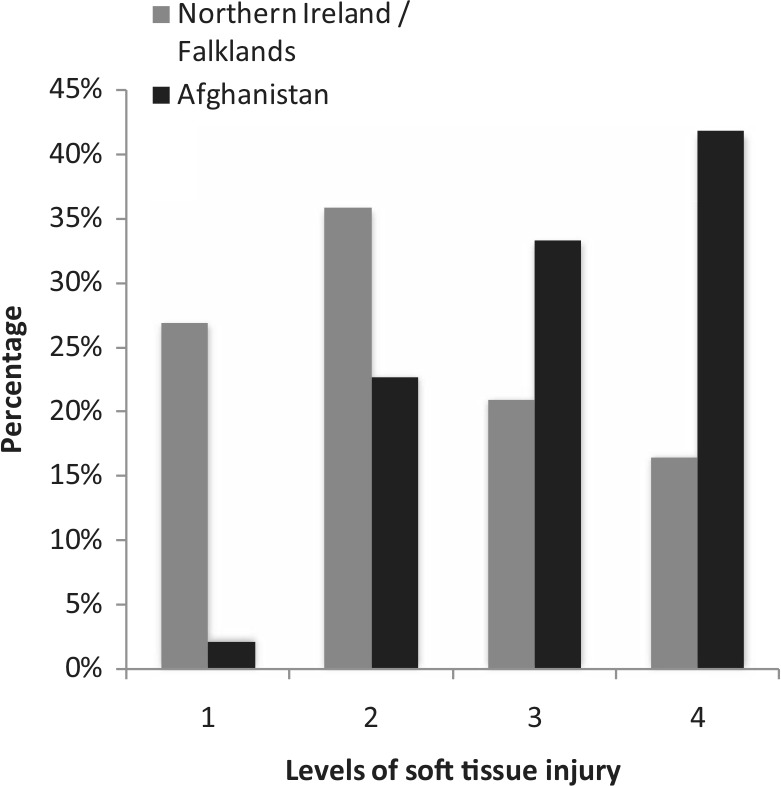
Comparison of soft-tissue injury levels between conflicts.
If the victim is situated close to the seat of the explosion, the effects of the blast wave and detonation products occurs almost instantaneously. This effect is classically noted following the detonation of an anti-personnel mine, but more recently witnessed in victim-operated IED explosions involving dismounted troops. Upon detonation, the blast wave is transmitted directly into the limb, resulting in a brisance effect on bone. One or two milliseconds after detonation, the detonation products and casing/environmental fragments contact the limb causing destruction of traumatised soft tissue and applying maximal stresses on bone previously damaged by the blast wave.18 The net result is either a total or subtotal amputation of the limb, with the zone of soft-tissue injury (including significant amounts of foreign debris and fragments) extending more proximally than the damaged bone.
Based on histological studies of combat casualties during the Soviet occupation of Afghanistan and animal models, Nechaev et al.19 described three major zones of injury following a mine blast as illustrated in Figure 2.20
Figure 2.
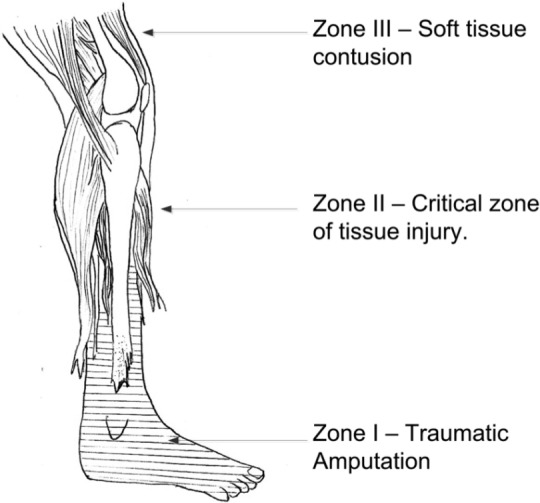
The zones of injury following a mine explosion.
Source: Ramasamy et al. (2013)20.
Zone I represents the area closest to the seat of the explosion.19,20 It is characterised by traumatic amputation of the limb, with widespread damage and anatomical destruction at different levels of the skin, tendons, muscles, bones and neurovascular structures. In all cases, the soft-tissue injuries within this zone are associated with significant contamination from soil and energised explosive fragments. A particular feature of these injuries includes disruption of tissues along fascial sheaths with the high-pressure detonation gases driving soil proximal to the level of bone traumatic amputation. Based on the level of local soft-tissue injury, surgical amputations performed through zone I were considered non-viable.
Within zone II of the injured limb, there are focal areas of micro-laceration of the muscle fascicles with associated lacerations of small and large blood vessels, giving rise to focal areas of haemorrhage. From arteriograms performed in animal studies, it was determined that there remained a persistent impairment of blood flow in this zone, with segmental vasospasm and dilatation of arterioles and venules a consistent feature. In addition, endoneural and epineural haemorrhage was witnessed within the peripheral nerves with associated oedema of the nerve. The level of injury diminished with increasing distance from the zone I boundary with areas of tissue completely undamaged. Of note, the focal areas of injuries appeared to be localised near the neurovascular bundles and the osteofascial planes, suggestive of transmission of the blast wave through these structures.
The main features of injuries in zone III are avulsion of small arterioles from main vessels, impaired venous return and reactive changes in the axons of peripheral nerves. In a review of 19 casualties who underwent serial biopsies following surgical amputation in zone III and made an uncomplicated recovery from their injuries, it was noted that, in the first 5 days, there remained extensive tissue oedema with pronounced marginal necrosis of the muscle boundary. This was associated with demyelination of the peripheral nerves. From days 6 to 14, it was noted that vessels in the amputation stump showed signs of panvasculitis with further necrosis of muscle fibres. In addition, biopsy of the peripheral nerves revealed hyperplasia of the Schwann cells and the formation of traumatic neuromas and neurofibromas.
Based on these findings, Nechaev recommended that the optimal level for surgical amputation should be at the border of zone II and III. Clinically, this manifests as the ability for muscle fibres to contract and minimal soft-tissue oedema.
Primary amputations
Despite all the advances made in medicine, amputation remains a commonly required procedure in the management of military limb trauma. The presence of a vascular injury that required repair in a physiologically unstable patient were the main factors in patients who required an amputation in one study.21 This is unsurprising when considering the prolonged time needed for revascularisation, which will not be tolerated in a patient who is critically unwell.
Given the advances that have been made in limb salvage techniques, anatomical indications for amputation, such as ‘unreconstructable’, should not be used, unless the case has been discussed with a specialist centre. In addition, no limb should be amputated on the basis that the patient would be better off without it, unless it has been fully discussed with the patient. In practice, this is rarely possible at the first operation, and so limb salvage should normally be attempted if possible. The presence of a numb sole of foot has, traditionally, been quoted as an indication for amputation. However, recovery of protective sensation has been reported in 50% of civilian trauma patients,22 and has also been noted in 90% of UK military patients. As will be discussed below, severe hindfoot injuries, although salvageable, are associated with a poor outcome. However, in most cases salvage should be attempted initially and an early discussion on prognosis carried out with the patient.
Scoring systems
Several scoring systems have been developed to help guide the decision to amputate after severe lower limb trauma, and are believed to be accurate. Unfortunately, this accuracy may be helpful as a retrospective governance tool, but the relatively low sensitivity or specificity of these tools, makes them unreliable as decision-making instruments. This is particularly well illustrated in the prospective study of the Lower Extremity Assessment Project in the United States, which documented relatively low sensitivities and some inconsistencies when five of the more commonly used scoring systems were applied to 556 lower limb injuries and it was felt that clinical utility was not provided.23 In addition, they are not predictive of the shorter or longer term functional outcome.
Late amputation
One of the features of the current conflicts has been the high incidence of late amputation following injury. Improvements in limb salvage techniques, as well as improvements in resuscitative techniques, have resulted in casualties who are more able to tolerate complex reconstructive attempts following injury. In a review of 348 US combat casualties who underwent amputation, it was reported that 15.2% were performed as a late procedure24 (defined as being more than 12 weeks after injury). The authors postulated that the high incidence of late amputation may be related to the earlier functional recovery of amputees than of limb salvage patients. It is also important to recognise that service personnel, who are likely to place significant physical demands on their salvaged limbs, are less able to tolerate injuries to the foot and ankle complex. Ramasamy et al.25 reported that, of the 30 UK casualties who suffered a fractured calcaneus after a vehicle explosion, only two were able to return to full military duty 3 years after injury, and the amputation rate was 45%.
Nerve injury
Given that nerves can be injured by both the concussive aspects of the blast wave, as well as by direct injury from energised fragments, the incidence of nerve injury in victims of explosions is relatively high compared with civilian trauma (8.1% vs. 0.5%).26 In a review of 100 consecutive UK combat casualties who presented to the War Nerve Injury clinic at Headley Court, Epsom, 36 casualties suffered neuropathic pain secondary to the nerve injury, with post-traumatic neuralgia the most common mechanism of neuropathic pain.27 In all cases, revision operations were undertaken, with 30 patients experiencing relief of symptoms. At operation, the cause of persisting pain included displaced bone fragments, heterotrophic ossification and, most commonly, scar tissue that enveloped and constricted the nerve. In the initial post-injury phase, these casualties are often too sick to tolerate complex, prolonged plastic surgery procedures. As such, exchange of skin-grafted tissue with fasciocutaneous flaps can only be performed many months after injury. Despite the significant improvement of symptoms following nerve repair, neurolysis and revision skin cover, two casualties had intractable pain that resulted in amputation.
Outcome of combat-related amputation
The increasing number of amputees from Afghanistan, particularly those with high bilateral amputations, is a concern as there are few outcome data available to indicate their long-term prognosis. Only the Vietnam War offers comparable experience, and much of the published literature is by Dougherty28 and relates to the review of casualties managed at the Valley Forge General Hospital, which, he states, was established in 1969 to ‘consolidate the efforts of therapists, nurses, prosthetists, and surgeons to provide more consistent and structured care’ (p. 383). It can be presumed that this is comparable to the current service provided by the Defence Medical Rehabilitation Unit at Headley Court.
Dougherty28 reviewed the records of 484 amputees approximately 28 years after injury, and was able to contact many of the veterans. Given the retrospective nature, and for some injuries a relatively low sampling rate, bias will be present; however, from a review of three published papers, it is possible to make some observations of outcomes based on the level of amputation.
It would appear that an isolated transtibial amputation was associated with a ‘normal’ life, and any reduction in mental or physical health was related to other injuries sustained at the time. Of the 72 patients he contacted, 96% had married, 83% had children and 99% were employed. On average, they wore their prosthetic for 15.9 hours a day. Those who had sustained other injuries were significantly more likely to have received psychological help.
Dougherty29 also reviewed 46 unilateral transfemoral amputees. Again, the vast majority were married and had children, fewer were working, with 90% employed for an average of 20 years, and, when assessed using the Short Form 36, the physical health aspects were significantly reduced compared with a control group. From this it can be surmised that, while the casualties can integrate back into society and lead a relatively functional life, there is a significant physical disability associated with a unilateral transfemoral amputation. In addition, unlike the transtibial amputees, other major injuries are not related to this disability, which seems to be a result of the amputation.
Mobility was even further reduced when Dougherty30 reviewed 23 bilateral transfemoral amputees. Of the 484 case notes reviewed by Dougherty, 30 (6.2%) were in this group, of whom 27 were still alive, at an average of 27.5 years after injury. This is a similar mortality to the unilateral transtibial patients, suggesting a comparable life expectancy, although the patients were still only 45–54 years old at the time of review.
Dougherty found that 91% had married, and 87% had children but only 70% had been employed. Only 22% still wore a prosthesis as their main mobility method for an average 7.7 hours a day; an additional 43% had walked for an average of 12.9 years. From this it can be inferred that there were significant mobility issues in this group, and many were unable to work following their injuries. However, there was no deterioration in their mental health and they were able to reintegrate into society.
A separate study, which is likely to have included some of Dougherty’s cohort, looked specifically at when veterans abandoned prosthetics.31 There were a number of reasons why prosthetics were abandoned, including pain (25%) and residual limb too short (33.3%), ‘too heavy’ (16.7%) and ‘too much fuss’ (16.7%). The prosthetics were abandoned at an average of 6.7 years.
Deterioration in health can also be inferred from a comparison of veterans of Vietnam and Iraq/Afghanistan.32 Self-reported health status was rated as good to excellent in 40% of his Vietnam group and 80% in the Iraq/Afghanistan group (p = 0.04). Quality of life was rated as good to excellent in 54.6% of the Vietnam group and 70% of the casualties from Iraq/Afghanistan; this is not statistically different, but it may be influenced by other issues such as marriage/ employment as well as mobility.
Conclusion
Despite many advances, traumatic amputation and surgical amputation remain very common following combat or terrorist wounding, and the injury pattern is different from anything experienced from civilian trauma. Owing to the effects of the explosion, considerable tissue trauma occurs to many structures and, with advances in resuscitation, high and multiple amputations are being increasingly seen in survivors. Nerve injury is common and, with time, the functional level of the amputee will fall. These injuries remain a significant problem to health services following wars.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Conflict of interest: The author declares that there is no conflict of interest.
References
- 1. iCasualties. Traumatic amputation. Available at: http://icasualties.org/OEF/index.aspx (2013, accessed 9 January 2013).
- 2. Mazurek T, Ficke JR. The scope of wounds encountered in casualties from the Global War on Terrorism: from the battlefield to the tertiary treatment facility. J Am Acad Orthop Surg 2006; 14: S18–S23. [DOI] [PubMed] [Google Scholar]
- 3. Owens BD, Kragh JF Jr, Wenke JC, et al. Combat wounds in operation Iraqi Freedom and operation Enduring Freedom. J Trauma 2008; 64: 295–299. [DOI] [PubMed] [Google Scholar]
- 4. Hull JB. Traumatic amputation by explosive blast: pattern of injury in survivors. Br J Surg 1992; 79: 1303–1306. [DOI] [PubMed] [Google Scholar]
- 5. Mellor SG, Cooper GJ. Analysis of 828 servicemen killed or injured by explosion in Northern Ireland 1970–84: the Hostile Action Casualty System. Br J Surg 1989; 76: 1006–1010. [DOI] [PubMed] [Google Scholar]
- 6. Hadden WA, Rutherford WH, Merrett JD. The injuries of terrorist bombing: a study of 1532 consecutive patients. Br J Surg 1978; 65: 525–531. [DOI] [PubMed] [Google Scholar]
- 7. Frykberg ER, Tepas JJ., III Terrorist bombings. Lessons learned from Belfast to Beirut. Ann Surg 1988; 208: 569–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Almogy G, Luria T, Richter E, et al. Can external signs of trauma guide management? Lessons learned from suicide bombing attacks in Israel. Arch Surg 2005; 140: 390–393. [DOI] [PubMed] [Google Scholar]
- 9. Turégano-Fuentes F, Caba-Doussoux P, Jover-Navalón JM, et al. Injury patterns from major urban terrorist bombings in trains: the Madrid experience. World J Surg 2008; 32: 1168–1175. [DOI] [PubMed] [Google Scholar]
- 10. Johnson DE, Fleming A, Wongrukmitr B, et al. Combat casualties in Northern Thailand: emphasis on land mine injuries and levels of amputation. Mil Med 1981; 146: 682–685. [PubMed] [Google Scholar]
- 11. Coupland RM, Korver A. Injuries from antipersonnel mines: the experience of the International Committee of the Red Cross. BMJ 1991; 303: 1509–1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Livingston DH, Keenan D, Kim D, et al. Extent of disability following traumatic extremity amputation. J Trauma 1994; 37: 495–499. [DOI] [PubMed] [Google Scholar]
- 13. Maclean AA, O’Neill AM, Pachter HL, et al. Devastating consequences of subway accidents: traumatic amputations. Am Surg 2006; 72: 74–76. [PubMed] [Google Scholar]
- 14. Loder RT. Demographics of traumatic amputations in children. Implications for prevention strategies. J Bone Joint Surg [Am] 2004; 86-A: 923–928. [DOI] [PubMed] [Google Scholar]
- 15. Hodgetts TJ, Mahoney PF, Russell MQ, et al. ABC to <C>ABC: redefining the military trauma paradigm. Emerg Med J 2006; 23: 745–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Clasper JC. Amputations of the lower limb; a multidisciplinary consensus. J R Army Med Corps 2007; 153: 172–174. [DOI] [PubMed] [Google Scholar]
- 17. Hull JB, Bowyer GW, Cooper GJ, et al. Pattern of injury in those dying from traumatic amputation caused by bomb blast. Br J Surg 1994; 81: 1132–1135. [DOI] [PubMed] [Google Scholar]
- 18. Trimble K, Clasper J. Anti-personnel mine injury; mechanism and medical management. J R Army Med Corps 2001; 147: 73–79. [DOI] [PubMed] [Google Scholar]
- 19. Nechaev EA, Gritsanov AI, Fomin NF, et al. Mine Blast Trauma. St Petersburg: Russian Ministry of Public Health and Medical Industry, 1984. [Google Scholar]
- 20. Ramasamy A, Hughes A, Carter N, et al. The effect of blast on the musculoskeletal system. Trauma 2013; in press. [Google Scholar]
- 21. Brown KV, Ramasamy A, McLeod J, et al. Predicting the need for early amputation in ballistic mangled extremity injuries. J Trauma 2009; 66: S93–S97. [DOI] [PubMed] [Google Scholar]
- 22. Bosse MJ, McCarthy ML, Jones AL, et al. The insensate foot following severe lower extremity trauma: an indication for amputation? J Bone Joint Surg 2005; 87-A: 2601–2608. [DOI] [PubMed] [Google Scholar]
- 23. Bosse MJ, MacKenzie EJ, Kellam JF, et al. A prospective evaluation of the clinical utility of the lower-extremity injury-severity scores. J Bone Joint Surg [Am] 2001; 83-A: 3–14. [DOI] [PubMed] [Google Scholar]
- 24. Stinner DJ, Burns TC, Kirk KL, et al. Prevalence of late amputations during the current conflicts in Afghanistan and Iraq. Late Amputation Study Team. Mil Med 2010; 175: 1027–1029. [DOI] [PubMed] [Google Scholar]
- 25. Ramasamy A, Hill AM, Phillip R, et al. The modern ‘deck-slap’ injury – calcaneal blast fractures from vehicle explosions. J Trauma 2011; 71: 1694–1698. [DOI] [PubMed] [Google Scholar]
- 26. Birch R, Misra P, Stewart MP, et al. Nerve injuries sustained during warfare: part I – Epidemiology. J Bone Joint Surg [Br] 2012; 94-B: 523–528. [DOI] [PubMed] [Google Scholar]
- 27. Birch R, Misra P, Stewart MP, et al. Nerve injuries sustained during warfare: part II – Outcomes. J Bone Joint Surg [Br] 2012; 94-B: 529–535. [DOI] [PubMed] [Google Scholar]
- 28. Dougherty PJ. Transtibial amputees from the Vietnam War. Twenty-eight-year follow-up. J Bone Joint Surg [Am] 2001; 83-A: 383–389. [DOI] [PubMed] [Google Scholar]
- 29. Dougherty PJ. Long-term follow-up of unilateral transfemoral amputees from the Vietnam war. J Trauma 2003; 54: 718–723. [DOI] [PubMed] [Google Scholar]
- 30. Dougherty PJ. Long-term follow-up study of bilateral above-the-knee amputees from the Vietnam War. J Bone Joint Surg [Am] 1999; 81-A: 1384–1390. [DOI] [PubMed] [Google Scholar]
- 31. Laferrier JZ, McFarland LV, Boninger ML, et al. Wheeled mobility: Factors influencing mobility and assistive technology in veterans and service members with major traumatic limb loss from Vietnam war and OIF/OEF conflicts. J Rehabil Res Dev 2010; 47: 349–360. [DOI] [PubMed] [Google Scholar]
- 32. Dougherty PJ, McFarland LV, Smith DG, et al. Combat-incurred bilateral transfemoral limb loss: a comparison of the Vietnam War to the wars in Afghanistan and Iraq. J Trauma Acute Care Surg 2012; 73: 1588–1593. [DOI] [PubMed] [Google Scholar]


