Abstract
Pain related to cardiac disease has been recognised for centuries. However, the precise mechanisms of angina pectoris remain bafflingly obscure. Conventional cardiological angina management concentrates on methods to improve oxygen delivery to cardiac myocytes as our understanding of cardiac muscle cells’ response to hypoxia increases. In common with other chronic visceral pain syndromes, little is understood about how pain signals are generated and propagated by visceral nerves. Improved imaging and other physiological assessments have demonstrated important central nervous system (CNS) responses to myocardial ischaemia, including activation of CNS areas known to be ‘key players’ in chronic pain syndromes. Patients with stable angina usually have an excellent prognosis, especially if left ventricular function is preserved. Educating patients about their condition, teaching simple techniques known to help chronic pain patients and introducing targeted pain treatments specific to angina can be extremely helpful adjuncts to conventional cardiological treatments and will often bring about significant improvements in quality of life.
Keywords: Chest pain, chronic pain, intractable pain, pain, visceral pain
“There is a disorder of the breast marked with strong and peculiar symptoms, considerable for the kind of danger belonging to it, and not extremely rare, which deserves to be mentioned more at length. The seat of it, and sense of strangling, and anxiety with which it is attended, may make it not improperly be called angina pectoris”.
Thus wrote William Heberden, in a document to the Royal College of Physicians in 1768.1 It is clear that Heberden was a keen observer – all the cardinal features of angina pectoris are well described in a text that can still be used today as an exemplar of medico-literary clarity – even though he must have been perplexed by the variety in the manner of presentations of the condition.
There is an assumption prevalent today that angina pectoris is synonymous with ischaemic heart disease; atheromatous narrowings in the coronary arteries are certainly associated with the expression of symptoms that would be familiar to Heberden. By the 19th century angina was established as being related to the heart. However, the disease processes that provoke the symptoms of angina are wide ranging. In 1900 the two most common causes of angina pectoris were rheumatic valve disease and syphilitic aortitis (both causing reduced coronary perfusion, but with differing mechanisms).
Around the turn of the 20th century, it was thought that the symptom of angina might be due to distension of the ventricular wall, the so-called mechanical hypothesis;2 however, in the 1930s it was proposed that angina was actually caused by the release of chemical mediators within the myocardium and that this might be related to reduced blood flow.3 It is since the 1950s, with the introduction of more accurate and invasive investigations, that the association between coronary atheroma and angina has become so strongly established that many specialists (incorrectly) use the terms ‘angina’ and ‘ischaemia’ interchangeably.
Significant advances in lifestyle modification, medication and treatment of other conditions known to be associated with ischaemic heart disease have had a dramatic and beneficial impact on survival rates,4 yet a diagnosis of angina is commonly associated with (at least in the patient’s mind) a gloomy and uncertain outlook. In this article, we attempt to dispel some of the myths surrounding angina pectoris, to explain current theories of the mechanism and neurobiology of angina and to show how a multidisciplinary approach to angina management can have a significant impact on the patient’s quality of life.
Ischaemic heart disease
It is estimated that about 1.5 million UK citizens have atheromatous coronary disease, and about 100,000 people are newly diagnosed with angina each year.5 Television and film dramas often depict the acute presentation of cardiac disease as a life-threatening situation. This may create a false impression of the level of risk associated with the diagnosis of angina in the mind of the lay person. Healthcare professionals frequently contribute to this false impression with well-meaning but inaccurate admonitions:
Take things easy – you’ve got a time-bomb in your chest.
Use your GTN spray – it will open your arteries.
It’s important to take an aspirin every day – it will help keep your blood thin.
Taking regular exercise is good for you, but don’t overdo things or you may get into trouble.
In distinction to most other muscular beds, the oxygen extraction from the coronary circulation by the myocardium is nearly maximal, even at rest, with around 70% of oxygen being extracted, compared with around 30% elsewhere.6 Consequently, in order to supply the four- to fivefold increase in oxygen delivery that the myocardium requires under conditions of exercise or stress, blood flow must increase by a similar amount. Normally this is achieved by a beautifully coordinated vascular response involving neural, chemical and physical factors such as shear stress acting on several different regions of the coronary circulation.7 Normally adjustments in the size of the epicardial coronary arteries make only a small contribution to this process; however, when the flow of blood is limited by stenosis in the epicardial coronary artery, a mismatch between myocardial oxygen demand and supply inevitably occurs. This rapidly results in a decrease in the adenosine triphosphate (ATP) to adenosine diphosphate (ADP) ratio and generation of adenosine,8 which in turn leads to further dilatation of the coronary pre-arterioles. Normally this would increase coronary blood flow and restore homeostasis, but when the epicardial artery is significantly stenosed, no further blood supply is available and the adenosine levels rise significantly. These high levels activate sympathetic cardiac afferent neurones,9 probably through the use of the A1 subtype of the adenosine receptor.10 The resulting neural outflow appears to be responsible for the resulting sensation of visceral pain or discomfort, which manifests clinically as angina pectoris.
Other changes are induced in the myocardium following exposure to sub-optimal oxygen supply. Within a few minutes of exposure, changes occur in the myocytes’ handling of oxygen, which enable them to tolerate lower oxygen levels and avoid hypoxic injury (ischaemic pre-conditioning).11 In the longer term, release of angiogenic factors encourages the development of networks of collateral blood vessels, which are often clearly visible on coronary angiography. Collateral vessels can maintain adequate myocardial perfusion even when the native coronary arteries are completely occluded by plaque. Myocardial infarction occurs following sudden coronary artery occlusion, usually due to plaque rupture, platelet activation and intra-arterial clot production in territories of the myocardium which have not yet developed adequate protection.
Neurobiology of visceral pain
What is visceral pain for?
There is little evidence for the existence of visceral nociceptors. When considering the ‘rules’ that bind somatic pain, of which we have a more extensive understanding, it becomes clear that the phenomenon we call ‘visceral pain’ does not necessarily adhere to the same criteria.
In the case of somatic pain, following peripheral tissue damage sufficient to mount a pain response, there are predictable sequelae. First, the site of injury is accurately reported to the perceptual centres so it may be precisely located. Almost immediately a local inflammatory response is raised, which changes tissue bed haemodynamics, simultaneously creating an environment hostile to any invading organisms (raise the local temperature, flush out unwanted debris and introduce phagocytes) and making extra raw materials available for tissue repair. This local response is accompanied by changes elsewhere in the nervous system that adjust the wounded individual’s behaviour to protect the injured part while healing occurs. Inhibitory and excitatory interneurones are activated at various points in the ascending central nervous system (CNS), which tend to exaggerate the ‘pain state’ and act as a constant reminder that injury has occurred and that activity with the injured body part should be curtailed until healing is complete before a return to normal function is permitted. This includes activation of brain areas that process memory and emotion. The analytical and abstract thoughts that characterise human behaviour allow the prediction of situations that might exacerbate injury and thus worsen the pain. It is natural that such processing will normally arouse negative emotions and promote avoidance behaviour.
There is clear survival benefit to the individual and the species to have evolved such a sophisticated injury detection system. The way it fits together is elegantly described by the universally agreed definition of pain,12 originally proposed by the Intractable Pain Society (IPS) nearly a half century ago. However, there are some features of visceral pain that sit rather uneasily within the constraints of the IPS’s definition.
Positron emission tomographic (PET) studies of patients with angina clearly demonstrate activation of brain centres connected to the periphery by the lateral spinothalamic tracts, and when angina pain is induced, the brain areas that appear to be activated correspond to the same somatic territories in which the pain is perceived.13 These include the areas that deal with emotional and contemplative functions (hypothalamus, periaqueductal grey, thalami, prefrontal cortex and left inferior anterocaudal cingulate cortex). As, at least from the dorsal horn of the spinal cord onwards, afferent transmission from autonomic sources uses the same route to perception as somatic/nociceptive input, it is no surprise that many (although not all) patients describe such phenomena as painful. However, the very fact that angina may be perceived in many body territories structurally and functionally distant from the heart suggests that somatic and visceral pain are not the same.
Not all visceral pain is related to tissue injury. Cardiac syndrome X, a poorly understood pain condition in which angina pectoris is described in the absence of coronary artery disease (thereby carrying almost no risk of myocardial infarction) is neurologically indistinguishable from angina associated with ischaemic heart disease. It has long been recognised that there is no connection between stimulus intensity (in the case of angina pectoris this is assumed to be myocardial ischaemia) and perceptual intensity. Mild myocardial ischaemia may generate severe and prolonged episodes of angina pain, and yet the phenomenon of ‘silent’ (painless) ischaemia and even infarction is well known. The explanation offered by many specialists that autonomic neuropathy is responsible for this disconnect is both inaccurate and illogical, and has little basis when evidence for this view is sought. It may well be the case that in a subset of patients, particularly those with diabetes mellitus, autonomic neuropathy may form part of the explanation for an increased incidence of painless ischaemia,14 but even in those with diabetes the evidence is somewhat inconsistent.15 The high prevalence of silent ischaemia in those without neuropathy and the fact that the same degree of ischaemia may be painless one minute and painful the next in the same individual is inconsistent with autonomic neuropathy being responsible. Taken together, this evidence suggests that the signalling of cardiac pain may be induced by more than one mechanism, and, furthermore, that the oft-quoted admonition that ‘angina is nature’s warning not to overdo things’ is simply incorrect.
In answer to the question posed by the subtitle, we do not know the purpose, if any, of visceral pain. It is not always related to tissue damage, although it may be expressed in such terms. There is not necessarily an induced inflammatory response following an event that triggers visceral pain. If it has evolved as a natural warning system whose purpose is to modify potentially harmful behaviour (as with somatic pain), then significant anomalies exist which are difficult to explain alongside our current understanding of evolution theory. For example, there is overwhelming evidence that regular exercise in the patient with ischaemic heart disease reduces the risk not only of sudden death but also of the incidence and severity of angina episodes,16 and yet patients often find this difficult to achieve due to the induction of angina by the very exercise they have been advised to take. There is little evolutionary advantage to the perception of angina in this case.
Elucidating the nature and purpose of visceral pain is challenging. Studying visceral pain is difficult. There are only a few established animal models of visceral pain. It is clear that studying the laboratory animal’s responses to induced visceral stress is invasive and may not be representative of what goes on in the human nervous system when visceral pain is perceived.
The only aspect of visceral pain about which there is no disagreement is that it is generally considered ‘an unpleasant sensory and emotional experience’, and it is this component that allows us to characterise certain afferent autonomic neural transmissions as truly painful.
Neurology of angina
Visceral pain is mediated by the autonomic nervous system. As mentioned above, studying autonomic function in humans is challenging, and often invasive, which has limited our understanding.
There is extensive autonomic innervation of the heart; the effects of efferent stimulation are well recognised. Vagal stimulation reduces heart rate and has a negative inotropic effect, whereas sympathetic stimulation does the opposite.
In the case of cardiac pain it seems that afferent sympathetic nerve activity, principally activated by adenosine, as discussed above, is responsible for the bulk of pain signalling from the heart to the spinal cord and brain. The vagus nerve appears to have a minor role in afferent pain transmission.
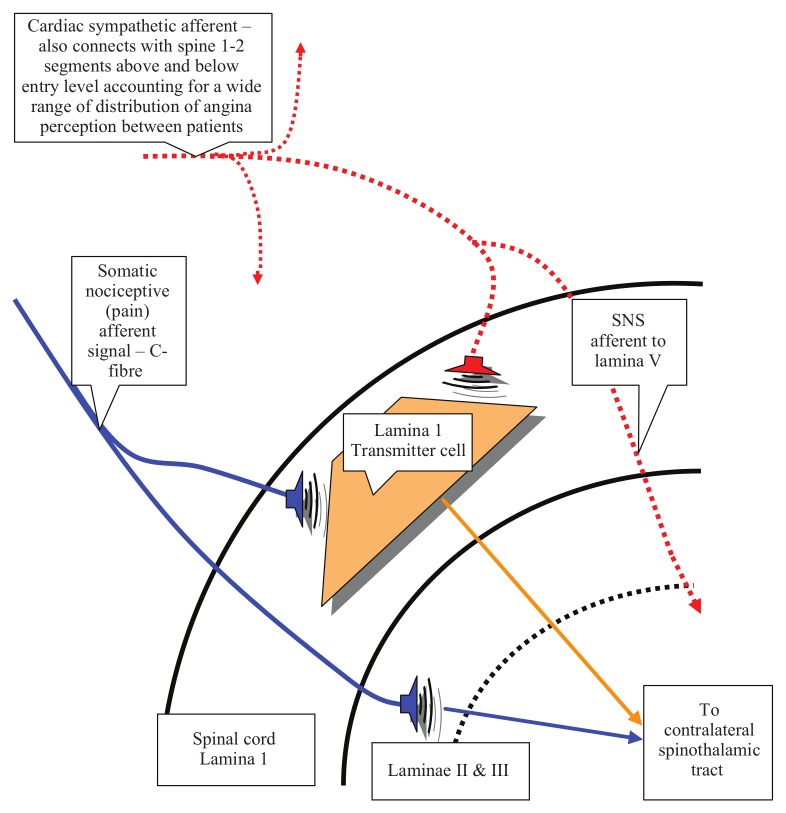
Afferent sympathetic neurones pass from the myocardium to either the superior or inferior cardiac plexus, from which they pass without synapsing through the sympathetic ganglion chain to the dorsal horn of the spinal cord (Figure 1). Here they connect predominantly to neurones in lamina I, although additional connections are made to lamina V. Incoming somatic nociceptive fibres are known to synapse with the same lamina I neurones (in addition to their laminae II and III connections), and it is possible that this is the point at which ‘crosstalk’ occurs between somatic and visceral afferent pathways, giving rise to the referred pain which characterises angina pectoris. Because of the extensive connections between cardiac sympathetic plexi, sympathetic ganglion chain and spinal cord (from the upper cervical ganglion to as far down as the sixth or seventh thoracic segment), it is easy to understand how angina may be expressed over such a large potential proportion of the upper body.
Figure 1.
Angina: suggested nerve connections in the spinal cord dorsal horn. SNS: sympathetic nervous system.
There are extensive afferent neuronal connections from the tracheo-bronchial tree, the lungs, the oesophagus and stomach that connect to the spinal cord at the same segmental levels as cardiac afferent fibres.
In lamina I of the dorsal root entry zone the afferent autonomic neurones may send connecting branches one or two segmental levels rostrally and caudally. These branches may synapse onto a ‘transmitter’ cell, which also receives synapses from incoming sensory nociceptive neurones, the principal synaptic connections of which are in laminae II and III (substantia gelatinosa). It seems likely that incoming ‘angina’ information gains access to the recognised rostral pathways that conduct pain information by this common connection in lamina I. However, there are also opportunities for information transfer with the lamina I transmitter cell’s own connections with the spinothalamic tract, and also the possibility of crosstalk between deeper pain connections in lamina V and the afferent sympathetic neurones that also connect with other neurones in lamina V. Currently all these potential explanations for the distribution of the perception of angina remain speculative.
Adjustments in the expression of inhibitory and/or excitatory neurotransmitters at the dorsal root entry zone (DREZ) may explain the notable finding of altered cutaneous sensitivity in the ‘angina territory’ described by the patient.
Following stimulation of neurones in the lateral spinothalamic tract, there will be activity in the brain areas identified as ‘key players’ in pain processing (peri-aqueductal grey matter, nucleus raphe magnus, insula, thalamus, amygdalo-hippocampal apparatus, sensory cortex and frontal cortex) and the conscious perception of pain will ensue.
However, there are features of angina, in common with other visceral pain syndromes, that distinguish it from somatic pain.
The poor localisation of the pain is most likely due to the diffuse nature of the convergence of visceral autonomic inputs onto common ‘transmitter’ cells used by both visceral and somatic afferents and the subsequent failure of the sensory cortex to project the incoming information accurately onto the ‘body map’, sometimes visualised as the ‘sensorimotor homunculus’. In addition, the inability of these common spinal routes to classify the incoming autonomic information as nociceptive leads to wide individual variations in character and intensity of perception, as well as location. Many patients refuse to describe their angina as painful, preferring instead to use such terms as ‘discomfort’, ‘pressure’ or ‘heaviness’.
Traditional functional classification of brain areas may not help our understanding. There is growing evidence of the role played by the motor cortex in maintaining chronic pain states. There is a long established, though often overlooked, association between angina pectoris and myalgic pain, especially in the trapezius, periscapular and shoulder muscles.17
Little is known about the processing of angina signals in the higher brain centres. However, Farmer et al18 have studied the autonomic responses to evoked oesophageal pain which accesses the spinal cord at the same level as cardiac autonomic fibres and which has several parallels to the observed autonomic changes in some patients with angina. Interestingly, in the case of oesophageal pain, there seems to be a range of responses which depend on the degree of neuroticism. Subjects scoring highly in neuroticism indices following Eysenck personality testing show excessive efferent vagal activity in response to painful oesophageal distension, resulting in bradycardia, reduced cardiac output and obtunded heart rate variability.19 As cardiac patients frequently report similar symptoms during episodes of angina pectoris, it is reasonable to presume a similar neurological mechanism. Conversely, patients with predominantly painless ischaemia show low scores for nervousness and excitability on personality testing and a reduced tendency to complain.20 However, our understanding of the neurobiology of angina, and visceral pain in general, remains fragmented and this is an area of study which has much potential for development.
Psychology of angina
The American College of Cardiology states that ‘the presentation of ischemic heart disease is often dramatic’, making reference to the fact that some patients’ first experience of their problem is a myocardial infarction, i.e. a potentially life-threatening event. Many supporting charitable organisations use this approach to raise public awareness of the condition, and the advice given to patients reflects the potential danger in overlooking or misinterpreting symptoms.
However, this ignores the fact that ischaemic heart disease is a dynamic condition, and applying the rules and restrictions that were appropriate half a century ago may be less relevant nowadays. Changes in our understanding of atheromatous vascular disease, in treatment for myocardial infarction, in better medication and adjustments in diet and other aspects of lifestyle have considerably reduced the death rate from coronary heart disease in the developed world since the 1950s, and these improvements in survival continue to this day.21,22
While ischaemic heart disease remains a common cause of death, the number of people with ischaemic heart disease who survive has increased, and in fact patients with stable angina have an excellent prognosis.23
However, the public perception of ischaemic heart disease as a dangerous and unstable condition remains, and because the symptoms experienced during an episode of angina may be similar to those occurring during myocardial infarction the advice dispensed to patients has changed little in the last 50 years.
Most patients who have been diagnosed with stable angina are still advised to attend hospital if angina pain persists beyond 15 minutes and has failed to respond to two doses of sublingual glyceryl trinitrate (GTN). Patients who follow this advice assiduously will spend a considerable amount of their lives in hospital accident and emergency (A&E) departments and may become ‘labelled’ as frequent attenders. Well-meaning but unhelpful remarks from A&E staff, such as ‘Oh, it’s you again’ or ‘We’ve kept your trolley warm for you’, especially when accompanied by such clumsy remarks as ‘Well, I can’t see your pain’ from an emergency doctor peering down at yet another electrocardiogram which shows no sign of ischaemic change, often create the false impression in the patient’s mind that his or her symptoms are not being taken seriously or, even worse, that the A&E staff think they are being exaggerated or fabricated.
Thus there is the potential for confusion and conflict to be created in the mind of the patient with angina, which may take the form of anxiety or frustration. Whichever turns out to be the prominent emotion, the likely result is a stress response, part of which will entail the release of catecholamines. This has the undesirable result of tachycardia and hypertension, which will increase myocardial demand and reduce supply of oxygen, which, in turn, is likely to worsen the perception of angina.
The psychic influence of catecholamine release cannot be overlooked. The effect is to enhance whatever is the prevailing ‘mood’ of the brain: if this is anxiety, the episode of angina will become very frightening; if it is frustration then the emotion will become anger or even rage. Neither of these emotional responses is likely to help reverse the supply–demand mismatch in the myocardium, and exhortations by healthcare professionals to remain calm may be perceived as baffling and impossible to achieve. Keeping a cool head during what the patient believes is a near-death experience is hard to do, no matter how many times it may have happened before.
Our understanding of the relationship between conscious and subconscious brain function, coupled with our observations of patients with stable angina, suggest that in many cases the brain’s ‘decision’ to release catecholamines (or indeed in the case of the ‘neurotic’ patient, to cause excessive vagal stimulation) in response to the arrival of the angina signal is made even before the conscious brain is aware of the angina pain. Patients often describe a prodromal experience that routinely happens before pain is felt. The Earl of Clarendon recognised this phenomenon and described it as angor animi – an ‘anguish of the spirit’, or mortal dread, which may accompany or precede the pain itself.24 When coupled with eyewitness confirmation of physiological change this clearly suggests that catecholamine release (sweating, pallor) or vagal stimulation (nausea, faintness) is a reflex response to changes in myocardial oxygen delivery that has been ‘learned’ by exposure to multiple repeated episodes.
The American College of Cardiology25 goes on to state that:
because of impressive recent technological advances healthcare providers tend to focus on diagnostic and therapeutic interventions, often overlooking critically important aspects of high quality care. Chief among these neglected areas is the education of patients.
This sentiment is reiterated in the guidelines for stable angina management published in 201126 by the National Institute for Health and Clinical Excellence (NICE):
Stable angina is a chronic medical condition. Medical management…includes a combination of pharmacological and revascularisation strategies and lifestyle interventions.
Notably, NICE stresses the paucity of evidence in support of the prognostic gains associated with revascularisation and questions not only the relevance of that scanty evidence but also the cost-effectiveness of non-prognostic revascularisation as part of the modern management of ischaemic heart disease.26
Modern management of stable angina
Despite the relatively small number of patients presenting acutely with a suspected heart attack, there is a uniformity of approach to the management of what has become a complex and many-faceted long-term medical condition.
We shall exclude situations in which the diagnosis is in doubt; clearly, in such a scenario, myocardial infarction must be excluded as a priority. However, until recently patients presenting with chest pain have ended up being exclusively managed by cardiologists, who have, to an extent, become ‘medical ischaemologists’.
In our unit in Liverpool, once an assessment of infarction risk has been completed, we have found a collaborative approach using both cardiological and pain management expertise, delivered in a setting much more akin to a pain clinic than a standard cardiology outpatient unit, has paid dividends in all aspects of the care of patients with stable angina. Not only are there fewer emergency hospital admissions, once patients have been educated about angina and ischaemic heart disease they become more confident in dealing with painful episodes, but they also experience less frequent and less severe pain, take lower doses of fewer drugs and show a reduction in the rate of myocardial infarction.27
If symptom load remains excessive following a simple education programme there is a range of low-cost, low-risk interventions (transcutaneous electrical nerve stimulation, upper thoracic sympathetic nerve block and low-dose strong opioids) which can be tried prior to consideration of more invasive techniques such as spinal cord stimulation or further revascularisation.
In conclusion
Angina has been around for centuries, and yet it remains a mysterious condition that affects individuals in different ways. It is clearly a visceral pain syndrome, yet many physicians perversely continue to apply to it the rules that govern somatic pain. There does not seem to be a physiological advantage to the sensing of angina, and many patients without coronary artery disease suffer from identical symptoms as those who do have coronary atheroma.
We are beginning to understand in more detail about how autonomic and somatic activity may converge in the spinal cord, but we know little about how this translates to brain activity, in particular in the neocortex.
If the human visceral nervous system has evolved from the remnants of the segmented invertebrate nervous system, then it seems plausible that the ‘new’ neural tube-derived vertebrate CNS has needed to develop ways of understanding and interpreting afferent visceral activity. At present it seems that visceral pain may be the result of misunderstanding and misinterpretation between the ‘new kid on the block’ (the CNS) and the more ancient aversive system that evolved much earlier, in the simpler multicellular and segmented invertebrate organisms developing on the young earth.
Maybe one reason why a CBT-style approach can be effective in managing human visceral pain is that, in some way, the cerebral cortex is ‘taught’ how to make sense of the clamour of noise that escapes, via the dorsal horn, from a busy autonomic network that is doing its best to control a highly complex interactive system, but which cannot help a few rogue notes from escaping into a consciousness which then jumps to the wrong conclusions when it fails to understand what is going on.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
References
- 1. Heberden W. Some account of a disorder of the breast. Medical Transactions 1772; 2, 59–67. [Google Scholar]
- 2. Colbeck EH. Angina pectoris: a criticism and a hypothesis. Lancet 1903; 1: 793–795. [Google Scholar]
- 3. Lewis T. Pain in muscular ischemia: its relation to anginal pain. Arch Intern Med 1932; 49: 713–727. [Google Scholar]
- 4. Critchley J, Capewell S. Explaining the decline in coronary heart disease mortality in England and Wales between 1981 and 2000. Circulation 2004; 109: 1101–1107. [DOI] [PubMed] [Google Scholar]
- 5.British Heart Foundation. Incidence. Available at: http://www.bhf.org.uk/research/statistics/morbidity/incidence.aspx (accessed 31 January 2013).
- 6. van de Hoef TP, et al. Coronary pressure-flow relations as basis for the understanding of coronary physiology. J Mol Cell Cardiol 2012; 52: 786–793. [DOI] [PubMed] [Google Scholar]
- 7. Patel B, Fisher M. Therapeutic advances in myocardial microvascular resistance: unravelling the enigma. Pharmacol Ther 2010; 127: 131–147. [DOI] [PubMed] [Google Scholar]
- 8. Schrader J, Gerlach E. Compartmentation of cardiac adenine nucleotides and formation of adenosine. Pflugers Arch 1976; 367: 129–135. [DOI] [PubMed] [Google Scholar]
- 9. Montano N, Lombardi F, Ruscone TC, Conti M, Guazzi M, Malliani A. The excitatory effect of adenosine on the discharge activity of the afferent cardiac sympathetic fibers. Cardiologia 1992; 36: 953–959. [PubMed] [Google Scholar]
- 10. Bertolet BD, Belardinelli L, Franco EA, Nicholos WW, Kerenski RA, Hill JA. Selective attenuation by N-0861 (N6-endonorboran-2-yl-9-methyladenine) of cardiac A1 adenosine receptor-mediated effects in humans. Circulation 1996; 93: 1871–1876. [DOI] [PubMed] [Google Scholar]
- 11. Murry C, Jennings R, Reimer K. Pre-conditioning with ischemia. A delay of lethal cell injury in ischemic myocardium. Circulation 1986; 74: 1124–1136. [DOI] [PubMed] [Google Scholar]
- 12.International Association for the Study of Pain. Available at: http://www.iasp-pain.org/AM/Template.cfm?Section=Pain_Definitions#Pain (accessed 31 January 2013).
- 13. Rosen S, Camici P. The brain–heart axis in the perception of cardiac pain: the elusive link between ischaemia and pain. Ann Med 2000; 32: 350–364. [DOI] [PubMed] [Google Scholar]
- 14. Niakan E, Harati Y, Rolak L, Comstock J, Rokey R. Silent myocardial infarction and diabetic cardiovascular autonomic neuropathy. Arch Intern Med 1986; 146: 2222–2230. [PubMed] [Google Scholar]
- 15. Caracciolo EA, Chaitman BR, Forman SA, et al. Diabetics with coronary artery disease have a prevalence of asymptomatic ischemia during exercise treadmill testing and ambulatory ischemia monitoring similar to that of nondiabetic patients: an ACIP database study. Circulation 1996; 93: 2097–2105. [DOI] [PubMed] [Google Scholar]
- 16. Lavie C, Milani R. Effects of cardiac rehabilitation, exercise training and weight reduction on exercise capacity, coronary risk factors, behavioural characteristics and quality of life in obese coronary patients. Am J Cardiol 1997; 79: 397–401. [DOI] [PubMed] [Google Scholar]
- 17. Procacci P. Ch 29 Cardiac Pain. In: Melzack R, Wall P. (eds) Textbook of pain, 3rd ed. 1994, Edinburgh: Churchill Livingstone; pp. 546 [Google Scholar]
- 18. Farmer A, Aziz Q, Tack J, Van Oudenhove L. The future of neuroscientific research in functional gastrointestinal disorders: integration towards multidimensional (visceral) pain endophenotypes? J Psychosom Res 2010; 68: 475–481. [DOI] [PubMed] [Google Scholar]
- 19. Coen SJ, Kano M, Farmer A, et al. Neuroticism influences brain activity during the experience of visceral pain. Gastroenterology 2011; 141: 909–917. [DOI] [PubMed] [Google Scholar]
- 20. Droste C, Roskamm H. Experimental pain measurements in patients with asymptomatic myocardial ischemia. J Am Coll Cardiol 1983; 1: 940–945. [DOI] [PubMed] [Google Scholar]
- 21. Unal B, Critchley J, Capewell S. Explaining the decline in coronary heart disease mortality in England and Wales between 1981 and 2000. Circulation 2004; 109: 1101–1107. [DOI] [PubMed] [Google Scholar]
- 22. Gerward S, Persson K, Midlov P, Ekesbo R, Gullberg B, Hedblad B. Trends in out-of-hospital ischaemic heart disease deaths 1992–2003 in southern Sweden. Scand J Public Health 2012; 40: 340–347. [DOI] [PubMed] [Google Scholar]
- 23. Parker JD, Parker JO. Stable angina pectoris: the medical management of symptomatic myocardial ischemia. Can J Cardiol 2012; 28(Suppl): s70–80. [DOI] [PubMed] [Google Scholar]
- 24. The Earl of Clarendon, Life of Edward, Earl of Clarendon, 1759 in R.H. Major, Classic Descriptions of Disease, 3rd Edn, 1945. Springfield: Thomas, pp. 416–18. [Google Scholar]
- 25. Gibbons RJ, Chatterjee K, Daley J, et al. ACC/AHA/ACP guidelines for the management of chronic stable angina: a report of the American College of Cardiology/American Heart Association/American College of Physicians Task Force on Practice Guidleines. J Am Coll Cardiol 1999; 33: 2093–2197 [DOI] [PubMed] [Google Scholar]
- 26.National Clinical Guidelines Centre. Stable angina: methods, evidence & guidance. London: Royal College of Physicians, 2011. [PubMed] [Google Scholar]
- 27. Moore R, Groves D, Bateson S, et al. Health-related quality of life of patients with refractory angina before and one year after enrolment onto a refractory angina program. Eur J Pain 2005; 9: 305–310. [DOI] [PubMed] [Google Scholar]