Abstract
Background:
To investigate the prevalence of antibiotic usage in children aged <5 years with acute respiratory tract illness (ARTI) in Iran.
Materials and Methods:
Data were collected from a national health survey conducted in 2010 (Iran's Multiple Indicator Demographic and Health Survey). Participants of this cross-sectional study were selected by multistage stratified cluster-random sampling from 31 provinces of Iran. Parents of children with <5 years of age responded to questions about the occurrence of any cough during the previous 2 weeks, referral to private/governmental/other health care systems, and utilization of any oral/injection form of antibiotics. Data were analyzed using SPSS software18. The chi-square test was used to determine antibiotic consumption in various gender and residency groups and also a place of residence with the referral health care system.
Results:
Of the 9345 children under 5 years who participated in the study, 1506 cases (16.2%) had ARTI during 2 weeks prior to the interview, in whom 1143 (75.9%) were referred to urban or rural health care centers (43.4 vs. 30.4%; P < 0.001). Antibiotics were utilized by 715 (62.6%) of affected children. Injection formulations were used for 150 (13.1%) patients. The frequency of receiving antibiotics was higher in urban than in rural inhabitants (66.0% vs. 57.7% P < 0.05).
Conclusion:
The prevalence of total and injection antibiotics usage in children <5 years with ARTI is alarmingly high in Iran. Therefore, interventions to reduce antibiotic use are urgently needed.
Keywords: Anti-bacterial agents, child, Iran, respiratory tract diseases, utilization
INTRODUCTION
Antibacterial agents are among the most used medications in children especially in the community setting.[1] They are usually obtained by advisement of physicians and health care workers. In some countries, they can be provided directly from pharmacies and drugstores without the need for a prescription.[2] The majority of consumed antibiotics are used for the treatment of viral upper acute respiratory tract illness (ARTI) that do not benefit from their use.[3,4]
Inappropriate overuse of antibiotics arises from incorrect differentiation of bacterial from nonbacterial illnesses or misinterpretation of their effects by patients, physicians, and health care workers.[5] This excessive utilization is a major health problem worldwide, and it has been well documented in the region.[6] It increases potential adverse reactions and cost of the diseases both for the patients and the community, moreover, it's most important disadvantageous the generation and spread of resistant bacteria.[7,8] Infections induced by these resistant microorganisms can increase the mortality, morbidity, and a hospital stay of patients.[9]
Experience reveals that the problem of the resistant bacteria could not be solved by the creation of more effective antibiotics. Other interventions are required to reduce the excessive consumption of antibiotics. This is true especially in outpatient settings because more than 90% of antibiotics are used in such settings.[4]
A thorough evaluation of utilization rate of antibiotics in common illnesses is the first step in planning programs to improve consumption of antibacterials in the population. There is no published study of the rate of antibiotic use in ARTI in Iran. Therefore, in this study we used the data from a nationwide household survey to investigate the antibiotic consumption rate in Iranian children aged under 5 years with ARTI.
MATERIALS AND METHODS
Data were collected from a national health survey conducted in 2010 by the Ministry of Health and Medical Education (MoHME) and National Institute of Health Research, Iran's Multiple Indicator Demographic and Health Survey. Detailed methodology is explained,[10] and herein we describe it in brief.
Design
In summary, the survey was a cross-sectional multistage stratified cluster-random study, which was performed through face to face household interviews in 31 provinces of Iran. The samples were selected proportional to inhabitants of each province and each district within the province. In order to draw meaningful inferences about each province, the minimum sample size for each province was increased to 40 clusters. In addition, the samples were weighted to reflect the population size of rural and urban areas in each district. The clusters in each district were selected randomly from the list of the last national population and housing census of Iran. Finally, 3096 clusters (2187 urban and 909 rural) were included. Each cluster consisted of 10 consecutive households. Provincial samples ranged from 400 to 6400 households per province.[10]
Data collection
In summary, a total of 240 trained teams were collected the predesigned data. Each team consisted of two interviewers, one field editor and one driver. Furthermore, 181 supervisors were involved to ensure the consistency and quality of the collected data.[9]
Ethical considerations
The Ethics Committee of the Tehran University of Medical Sciences, the information office of the MoHME, the review board of the Statistics Center of Iran and the Policy Council and the Board of Deputies of the MoHME approved the study.
Pamphlets about the importance of the survey, its confidentiality, and freeness of the eligible family to participate or refuse the study were presented to selected households at least 1-day before the interview. At the beginning of the interview, verbal assent and written consent were obtained from the eligible individuals and their parents, respectively.
The protection of privacy of interviewee information was assured by categorization and storing of all completed questionnaires in a separate room and saving the data in the web-based information system anonymously. These data were accessible only to specified members of the research team.[10]
Interviews
After checking the age of the children from their birth certificate or its copy, the parents were asked to respond to following questions:
If their under 5 years child had any cough during last 2 weeks prior to interview? (Rate of ARTI).
If yes, if the child taken to physician, pharmacy, or health system personnel? (Rate of referral to heath care system).
If yes, the child taken to a private or governmental clinic? (Rate of referral to private/governmental/both/other health care systems).
Then parents were asked to bring the prescription paper and consumed drugs, trained interviewers checked the presence of prescribed oral and injected antibiotics (antibiotic consumption rate, injection antibiotic consumption rate).
Finally, the data were entered into the predesigned forms.
Data entry
Specialized software was based on the CSPro data-entry software (provided by the UNICEF) was modified to the questionnaires of the study and was used. The data was uploaded daily through a protected web-based system from all provincial teams in a central computer.[10]
Statistical analysis
Data were analyzed using SPSS-PC version 18.0 (SPSS Inc., Chicago, IL, USA). The chi-square test was used to identify the association of gender and place of residence with antibiotic consumption and also a place of residence with the referral health care system in studied children. P < 0.05 was considered as statistically significant.
RESULTS
A total of 29,609 families from 31,350 predesigned families participated in the study (94.5% participation rate). From 9,345 children under 5 years in participant families, 9,298 (99.5%) enrolled in the survey. The mean age of enrolled children was 2.43 ± 1.23 years. Overall, 1506 cases (16.2%) had ARTI in the 2 weeks prior to interview, in whom 1143 (75.9%) were referred to physician, pharmacy or other health care centers.
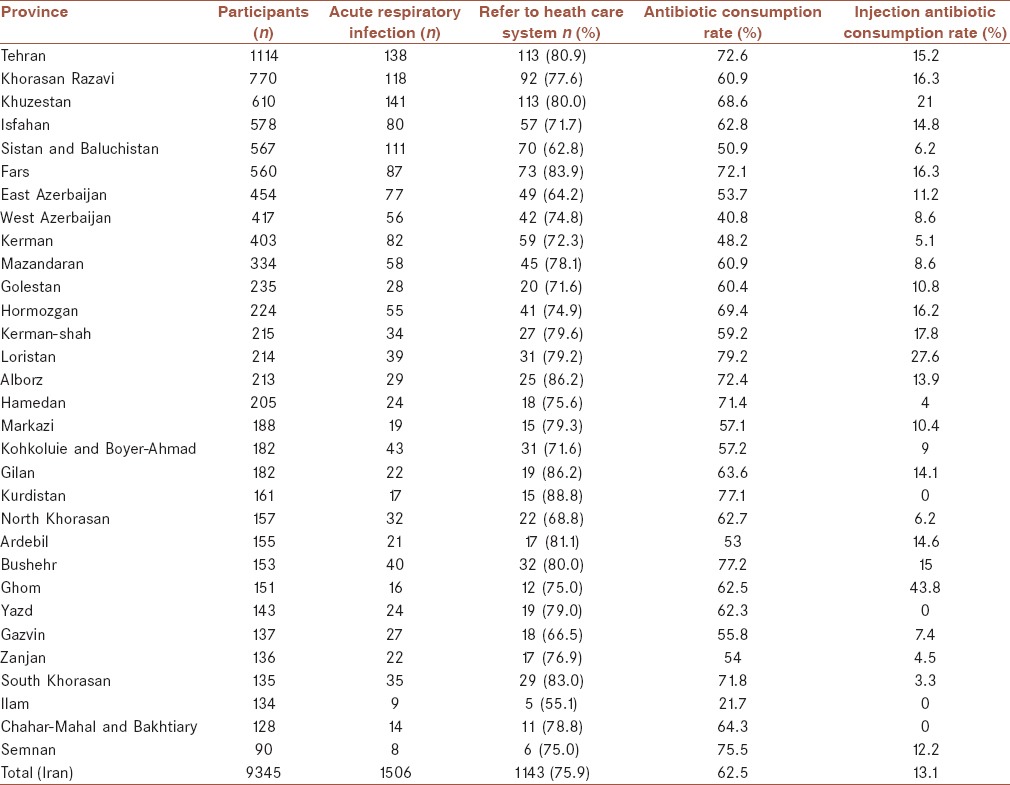
Referral to private clinics were higher in urban than in rural areas (43.4 vs. 30.4%; P < 0.001) [Table 1]. Antibiotics were utilized by 715 (62.6%) children. The rate of antibiotic consumption was >75% in Loristan, Bushehr, Kurdistan, and Semnan states. Injection antibiotics were used for 150 (13.1%) patients. Injection antibacterials were advised to more than 20% of infected children in Ghom, Loristan, and Fars provinces [Table 2].
Table 1.
Total number of participant children in accordance to place of residence and referral health care system
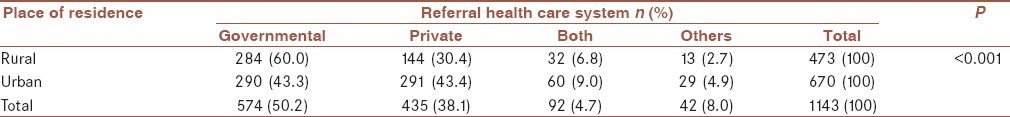
Table 2.
Number of under 5 children with acute respiratory tract infection and the rate of referral to health care system, total and injection antibiotic consumption in provinces of Iran in 2010
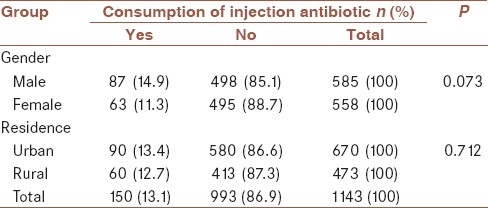
The frequency of receiving antibiotics was higher in urban than in rural inhabitants (66.0% vs. 57.7%; P < 0.05) [Table 3]. In contrast, there was no significant difference in antibiotic usage between two genders [Table 3]. In addition, the rate of prescribed injection antibiotic was similar in both genders as well as in rural and urban areas [Table 4].
Table 3.
Antibiotic consumption rate in children <5 years with recent cough in Iran in accordance to gender and residence group
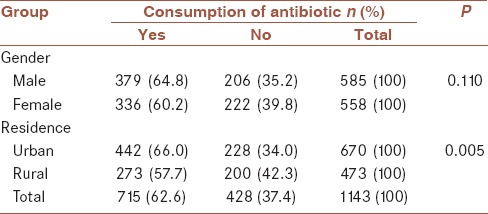
Table 4.
Injection antibiotic consumption rate in children <5 years with recent cough in Iran in accordance to gender and residence group
DISCUSSION
This nationwide study showed that 62.6% of the children with acute cough during the previous 2 weeks had used antibiotics. This is a very high percentage, compared to similar studies conducted in other countries as United States in 2011,[11] Norway in 2003,[12] and United Kingdom in 2004,[13] which were reported to be 21%, 27% and 31%, respectively. However, the high percentage of antibiotic usage in the current survey is consistent with some studies in other countries as Malaysia in 2011[14] and United Kingdom in 1990,[15] and also in the Eastern Mediterranean region.[6]
It has been estimated that 90% of children seeking care for respiratory infections has an illness consistent with viral etiology and do not benefit from antibiotic therapy.[4]
Underlying reasons for overuse of antibiotics despite scientific disagreement is multifaceted and vary from one country to another. In many situations, the misconception of patients and physicians concerning the effectiveness of antibiotics is the main barrier in the logic use of antibacterial agents. A common scenario is a patient who thinks antibiotics are needed for all infections and so insist on antibiotics, and a physician who do not have enough time to explain why antibiotics are not necessary and therefore simply prescribe them to save time. Another setting is a patient who requests antibiotics for a viral infection and a physician who gain income from the patients and so advises them to obtain patient expectations. Physicians, who have not enough information or experience in the differentiation of bacterial from nonbacterial illnesses frequently advise antibiotics. Furthermore, physicians who are overly cautious excessively prescribe antibiotics in viral infections to protect their patients from complications of the diseases.[5,15]
In some countries including Iran, self-medication of antibiotics due to over the counter sale of them is an important additional problem. In these countries most drugs, particularly antibiotics, can be obtained from pharmacies without the need for a prescription. In these communities, some people who cannot afford doctor consultations, just go to pharmacies and prepare medications to reduce their payment.[2,16]
It is necessary to declare potential barriers inappropriate use of antibiotics in each community and to plan strategies for reducing the overall and broad spectrum usage of antibiotics.[1] Effective measures in other communities were combinations of interventions including dissemination of clinical practice guidelines, training courses for physicians, follow-up meetings, and feedback to physicians, group education for physicians’ assistants and for pharmacists, posters for waiting rooms, brochures and hand out to the patients, and restriction of over-the-counter sale of antibiotics.[15,17] Although certain interventions in Iran have been targeted at reducing inappropriate prescribing of antibiotics and injection medicines,[18] more focused interventions aiming at reducing inappropriate use of medicines for children are required.
In this study, 13.1% of children who had ARTI received an injection form of the antibacterial agent. To our knowledge, there is no previous report about injection antibiotic usage in ARTI of children in Iran and also in other countries. Most children with an acute cough have a viral infection and do not benefit from antibiotics. A minority of them have acute bacterial sinusitis, concurrent acute otitis media, or bacterial pneumonia in which very uncommonly an injection antibiotic is necessary.[1,4] Therefore, consumed injection antibiotics for respiratory infections in the current study are overtly high. Injection antimicrobials have the potential to produce severe adverse reactions as anaphylaxis and local injury or infection. The rationale for this type of inappropriate advice of antibiotics probably is similar to causes of the excessive use of antibiotics, that is, unscientific insist of the patients, entail of the patient's expectations by physicians to save time and income, and unscientific believe of the physicians on rapid and complete effect of injection antibiotics in common respiratory infections.
Our study shows the rate of oral or injectable antibiotic usage in Loristan, Bushehr, Tehran, Fars, and Alborz states is considerably higher than mean national consumption rate. In contrast, antibiotic consumption in Ilam, West Azerbaijan, Kerman, and Sistan and Baluchistan provinces was less than other states [Table 2]. Although the small sample size in some areas precludes definite estimation of antibiotic usage in these states, the difference in cultures and beliefs about the effect of antibiotics might explain this variation.
Our findings show that the possibility of getting antibiotic was higher in children living in urban areas compared to rural districts. In urban regions, 66.0% of children who sought care for cough ultimately received an antibiotic while this rate was 57.7% in rural parts. This can be explained by the fact that in urban areas many families prefer to seek medical advice in private offices than governmental clinics. Obtaining patient's medical expectations is more convenient in private offices compared to governmental health centers. In our study, 43.4% of the urban and 30.4% of the rural inhabitants received medical advice in private centers [Table 1].
Study limitations and strengths
This study has some important limitations. The data do not provide information about the actual diagnosis of children who received antibiotics. Moreover, there is no information about the source of the advice of antibiotics, that is, physicians or health care workers prescription, or self-medications. The other limitation is that no information exists about the presence of fever or coryza, and also the appropriateness of the type, dose, and courses of advised antibiotics.
The strength of this study is its nationwide coverage with a multi-stage stratified cluster-random selection of the participants, which guarantees the representativeness of the results for the whole community. The other strength is the accurate measurement of antibiotic consumption rate by face-to-face interviews at the home where the drugs were being used. The third strength is a measurement of outpatient injection antibiotic usage in children with acute respiratory problems in addition to total antibiotic utilization. To the best of our knowledge, no previous study has provided this information in Iran and other neighbor countries.
CONCLUSION
The prevalence of total and injection antibiotics usage in Iranian children aged <5 years with ARTI is alarmingly high. Therefore, interventions to reduce antibiotic utilization for children are urgently needed.
AUTHOR'S CONTRIBUTION
All authors contributed in the study concept, conducting the analyses, drafting and revising the paper. All authors confirmed the final draft for submission and accept the responsibility for the paper content.
ACKNOWLEDGMENTS
This study was conducted as part of a national health survey.
Footnotes
Source of Support: Nil
Conflicts of Interest: None declared.
REFERENCES
- 1.Rossignoli A, Clavenna A, Bonati M. Antibiotic prescription and prevalence rate in the outpatient paediatric population: Analysis of surveys published during 2000-2005. Eur J Clin Pharmacol. 2007;63:1099–106. doi: 10.1007/s00228-007-0376-3. [DOI] [PubMed] [Google Scholar]
- 2.Mohanna M. Self-medication with Antibiotic in Children in Sana'a City, Yemen. Oman Med J. 2010;25:41–3. doi: 10.5001/omj.2010.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schindler C, Krappweis J, Morgenstern I, Kirch W. Prescriptions of systemic antibiotics for children in Germany aged between 0 and 6 years. Pharmacoepidemiol Drug Saf. 2003;12:113–20. doi: 10.1002/pds.786. [DOI] [PubMed] [Google Scholar]
- 4.Arroll B. Antibiotics for upper respiratory tract infections: An overview of Cochrane reviews. Respir Med. 2005;99:255–61. doi: 10.1016/j.rmed.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 5.Fischer T, Fischer S, Kochen MM, Hummers-Pradier E. Influence of patient symptoms and physical findings on general practitioners’ treatment of respiratory tract infections: A direct observation study. BMC Fam Pract. 2005:6–6. doi: 10.1186/1471-2296-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rashidian A, Jahanmehr N, Jabbour S, Zaidi S, Soleymani F, Bigdeli M. Bibliographic review of research publications on access to and use of medicines in low-income and middle-income countries in the Eastern Mediterranean Region: Identifying the research gaps. BMJ Open. 2013;3:e003332. doi: 10.1136/bmjopen-2013-003332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goossens H, Ferech M, Vander Stichele R, Elseviers M. ESAC Project Group. Outpatient antibiotic use in Europe and association with resistance: A cross-national database study. Lancet. 2005;365:579–87. doi: 10.1016/S0140-6736(05)17907-0. [DOI] [PubMed] [Google Scholar]
- 8.Turett GS, Blum S, Fazal BA, Justman JE, Telzak EE. Penicillin resistance and other predictors of mortality in pneumococcal bacteremia in a population with high human immunodeficiency virus seroprevalence. Clin Infect Dis. 1999;29:321–7. doi: 10.1086/520209. [DOI] [PubMed] [Google Scholar]
- 9.Spellberg B, Guidos R, Gilbert D, Bradley J, Boucher HW, Scheld WM, et al. The epidemic of antibiotic-resistant infections: A call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis. 2008;46:155–64. doi: 10.1086/524891. [DOI] [PubMed] [Google Scholar]
- 10.Rashidian A, Khosravi A, Khabiri R, Khodayari-Moez E, Elahi E, Arab M, et al. Tehran: Ministry of Health and Medical Education; 2012. Islamic Republic of Iran's Multiple Indicator Demograpphic and Healh Survey (IrMIDHS) 2010. [Google Scholar]
- 11.Misurski DA, Lipson DA, Changolkar AK. Inappropriate antibiotic prescribing in managed care subjects with influenza. Am J Manag Care. 2011;17:601–8. [PubMed] [Google Scholar]
- 12.Gjelstad S, Dalen I, Lindbaek M. GPs’ antibiotic prescription patterns for respiratory tract infections — Still room for improvement. Scand J Prim Health Care. 2009;27:208–15. doi: 10.3109/02813430903438718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meropol SB, Chen Z, Metlay JP. Reduced antibiotic prescribing for acute respiratory infections in adults and children. Br J Gen Pract. 2009;59:e321–8. doi: 10.3399/bjgp09X472610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kho BP, Ong CM, Tan FT, Wee CY. Antibiotic prescribing for upper respiratory tract infections in sarawak district hospitals. Med J Malaysia. 2013;68:136–40. [PubMed] [Google Scholar]
- 15.Arnold SR, Straus SE. Interventions to improve antibiotic prescribing practices in ambulatory care. Cochrane Database Syst Rev. 2005;19:CD003539. doi: 10.1002/14651858.CD003539.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muras M, Krajewski J, Nocun M, Godycki-Cwirko M. A survey of patient behaviours and beliefs regarding antibiotic self-medication for respiratory tract infections in Poland. Arch Med Sci. 2013;9:854–7. doi: 10.5114/aoms.2012.29217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bjerrum L, Munck A, Gahrn-Hansen B, Hansen MP, Jarboel D, Llor C, et al. Health Alliance for Prudent Prescribing, Yield and Use of Antimicrobial Drugs in the Treatment of Respiratory Tract Infections (HAPPY AUDIT) BMC Fam Pract. 2010:11–29. doi: 10.1186/1471-2296-11-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soleymani F, Rashidian A, Dinarvand R, Kebriaeezade A, Hosseini M, Abdollahi M. Assessing the effectiveness and cost-effectiveness of audit and feedback on physician's prescribing indicators: Study protocol of a randomized controlled trial with economic evaluation. Daru J Pharm Sci. 2012;20:88. doi: 10.1186/2008-2231-20-88. [DOI] [PMC free article] [PubMed] [Google Scholar]


