Abstract
Background:
Migarine is the most common headache around the world including Iran. In recent years, Vitamin D deficiency has been shown to a global health problem. A few studies have been determined inverse association between serum levels of Vitamin D with a headache. So, in this study, we investigated the effect of Vitamin D supplementation on symptoms and C-reactive protein (CRP) among patients with migraine.
Materials and Methods:
This study was randomized, double-blind, and controlled-placebo clinical trial. Sixty-five migraine patients aged 10-61 years were included for analysis. Vitamin D was administrated for 10 weeks with 50,000 IU dosage of Vitamin D per week. Multivariate analysis of covariate and univariate analysis of covariate were done to determine the effects of Vitamin D supplementation on symptoms, including severity, duration, frequency of headache, and the headache diary result (HDR).
Results:
Mean headache frequency and HDR had significant difference among two groups (5.9 ± 7.0 vs. 7.0 ± 6.0, P = 0.06 and 85.0 ± 134.2 vs. 132.1 ± 147.1, P = 0.04). But, a mean difference of headache frequency was marginally significant (P = 0.06). These values were lower among the intervention group compared to placebo group. The association was not observed between CRP with migraine disease.
Conclusion:
In this study, we shown Vitamin D supplementation may be useful in decreasing frequency of headache attacks and HDR among patients with migraine.
Keywords: C-reactive protein, headache, migraine, Vitamin D
INTRODUCTION
Headache is prevalent among children and adolescents.[1] The most common types of primary headache disorders are migraine and tension headaches, which involves 80% of people in the world.[2]
Migraine is a neurological,[3] progressive, debilitating, and chronic disorder.[4] Migraine pains are caused by the release of pain-producing inflammatory materials around the nerves and blood vessels of the head.[5]
The main feature of the migraine attacks are headache,[6] last several hours to 2-3 days[5] and is often intense,[6] pulsatile, and unilateral.[5] Another related symptoms include nausea, sometimes vomiting, sensitivity to light and sound,[5] neck pain and muscle tension.[7] Migraine is associated with approximately 2-fold more risk of ischemic attacks.[8] Also, migraine in adults are related to seasonal allergies, asthma, epilepsy, continuous nightmares, atopic disorders, stroke, cardiovascular disorders, sleep problems, motion sickness, epistaxis, and in reproductive age is associated with preeclampsia and uterine bleeding.[1] The most common reason of migraine is hunger or not eating adequate food, which is important specially among the young people.[6] Migraine is nineteenth cause of disability worldwide[9] that includes 10-20% of the population in the life.[10] Recent information demonstrate that 1 out of 4 American adults, suffer from frequent or severe headache including migraine.[1] The prevalence of migraine is more common in women compared with men.[6] Prevalence of migraine in Turkey 16.4%,[11] European adults 14.7%,[12] England (7.6% in men and 18.3% in women),[13] Germany 13.4%,[2] Africa (3-7%)[5] and in Asia (3% among men and 10% among women).[5]
Also, a migraine headache is one of the common types of headaches in Iran.[14]
In recent years, Vitamin D deficiency has been identified as a global health issue.[15] Vitamin D deficiency has been identified among 30-80% children and adults in the world.[16]
In Iran, the prevalence of Vitamin D deficiency is 75.1% in women and 72.1% in men.[17] Vitamin D deficiency is related to different kinds of disorders including musculoskeletal disorders, cancer, autoimmune disorders, cardiovascular disorders, kidney disorders, mental disorders, skin disorders, etc.[18] Previous studies have determined that lower levels of Vitamin D are associated with higher headache,[18,19,20,21,22] but a few evidence have been determined. No clinical trial study has been performed in this field.
According to the previous findings, Vitamin D supplementation can decrease inflammatory factors such as C-reactive protein (CRP).[23] Also according to theory of neurogenic inflammation in migraine pathogenesis[24,25] and because of increased CRP levels in response to inflammation among patients with migraine,[26,27] we assessed effect Vitamin D supplementation on CRP. So, the aim of present study is to investigate the effect of Vitamin D supplementation on symptoms and CRP among migraine patients.
MATERIALS AND METHODS
The present study was randomized, double-blind clinical trial, and controlled with placebo. This study was performed among migraine patients in Isfahan city at Khorshid Clinic and Imam Mousa Sadr Clinic in autumn 2012. At baseline, 90 migraine patients aged 10-61 years participated. Confirmation of migraine disease was done by a neurologist. The informed consent form was taken from all participants. For ethical approval, the proposal was approved by the Ethics Committee of Isfahan University of Medical Sciences and was recorded in the website of Iranian Registry of Clinical Trials (IRCT2012122911763N4).
Data including age, gender, weight, height, waist circumference, body mass index (BMI), education, medical history, use of vitamin, and mineral supplements, migraine symptoms, serum levels of Vitamin D, calcium, phosphorus, albumin, and CRP were collected for all patients. BMI was calculated by the weight (kg) divided to squared height (m2).
Assessment form of migraine disease was completed by a neurologist for all participants.
Inclusion criteria were including confirmation of migraine disease by neurologist, tendency to participate in the study. And exclusion criteria contains cardiovascular, liver, kidney, primary hyperparathyroidism diseases, tension headache, and hypervitaminosis D, use of magnesium, calcium, B12, B9, B6, Vitamin D supplements, corticosteroids, and oral contraceptive in pregnancy.
All patients were referred for the laboratory to assess the serum levels of calcium, phosphorus, albumin, Vitamin D, CRP. Seventy-seven patients were placed in intervention and control groups. Thirty-nine patients in intervention group and 38 patients in the control group were located with simple randomization method. Patients were used supplementation or placebo of Vitamin D (50,000 IU/week) during 10 weeks (Zahravi company). The message was sent to all patients every week to remind participants for use of Vitamin D supplementation.
Also, 3-day food record were completed by patients every 2 weeks for dietary intakes. At the end, 65 patients were remained including 33 patients in intervention group and 32 patients in control group. At final, patients were examined for migraine symptoms (severity, mean duration of headache attacks, and frequency of attacks per month), and CRP.
Serum levels of Vitamin D were checked before and after the intervention. Food intakes of patients were analyzed using Nutritionist version 4 (N4) software to assess macronutrients and micronutrients.[28]
Biochemical assessment
At the first and end of the study, serum levels of 25(OH)D were measured by enzyme-linked immunosorbent assay (ELISA) method. According to ELISA method in laboratory, serum Vitamin D levels were categorized as: Deficient (serum levels <12 ng/ml); insufficient (serum levels between 12 and 30 ng/ml) and sufficient (serum levels more than 30 ng/ml). At first and the end of the intervention, CRP was measured. Also, for the diagnosis of primary hyperparathyroidism was measured calcium, phosphorus, and albumin at the first study.
Migraine assessment
Confirmation of migraine disease was done by a neurologist. For all patients, severity, mean duration of headache attacks and frequency of attacks per month was completed by a neurologist. Migraine severity was determined using Visual Analog Scale.[29,30] The headache diary result (HDR) was measured as: Duration of headache × frequency of headache.[29,30]
Statistical analysis
Statistical analysis was performed by the SPSS version 18.0 software (SPSS, Inc., Chicago, IL, USA). The presence or absence of difference in mean food intakes among two groups were analyzed by independent t-test. Severity, frequency, and duration of headaches attacks and HDR variables were not normal, so this variables changed on the logarithm until to be normal. Multivariate analysis of covariate including MANCOVA was done to determine the effects of Vitamin D supplementation on symptoms including severity, duration, and frequency of headache attacks. In addition, univariate analysis of covariate including ANCOVA was performed to investigate the effect of Vitamin D supplementation on HDR.
RESULTS
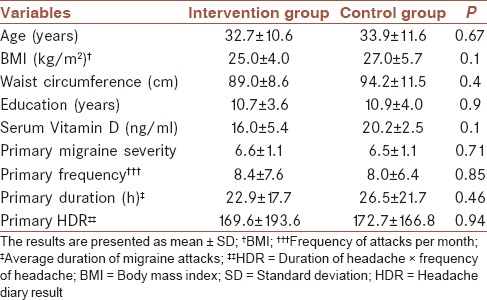
In this study, 65 patients were enrolled in the intervention and control groups (33 patients in the intervention group and 32 patients in the control group). Twenty-five females and 8 males in the intervention group and 22 females and 10 males in the control group were enrolled. General and clinical information of patients are shown in Table 1. Thirty-three patients with mean age of 32.7 ± 10.6 in the intervention group and 32 patients with mean age of 33.9 ± 11.6 in the control group were enrolled. Mean BMI, waist circumference, and education levels were higher among control group in compared with the intervention group. The primary mean of migraine severity and frequency was higher in the intervention group in compared with control group. But, the primary average of migraine duration and HDR was higher in the control group compared to the intervention group. Also, secondary average of migraine severity, frequency, duration and HDR was higher in control group compared to intervention group, respectively, (5.9 ± 1.5 vs. 5.0 ± 2.0), (7.0 ± 6.0 vs. 5.9 ± 7.0), (21.7 ± 17.0 vs. 13.6 ± 4.0), (132.1 ± 147.1 vs. 85.0 ± 134.2).
Table 1.
General and clinical characteristics of patients with migraine
Deficiency, insufficiency, and sufficiency of Vitamin D were reported among 15.4%, 66.1% and 18.5% patients, respectively.
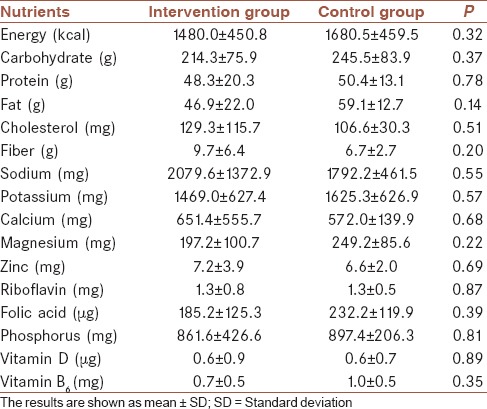
Food intakes were analyzed with the software. These results are shown in Table 2. No significant difference was observed between mean dietary intakes of patients among the intervention and control groups.
Table 2.
Food intakes of patients according to intervention and control groups
Multivariate analysis of covariate was used to determine the mean difference of severity, frequency, and headache duration in intervention and control groups. But for a mean difference of HDR in two groups, we used from univariate analysis of covariate. Severity, frequency, and duration of headaches attacks and HDR variables were not normal, so this variables changed on the logarithm until to be normal.
Multivariate analysis of covariance for age, sex, waist circumference, education, BMI, primary Vitamin D levels, primary severity, primary frequency, and duration of headache were controlled. In univariate analysis of covariate were controlled previous variables and, in addition, primary HDR. Results of the average comparison of severity, frequency, duration and HDR among intervention and control groups are shown in Table 3.
Table 3.
Comparison of severity, frequency, duration and HDR in intervention group and control group
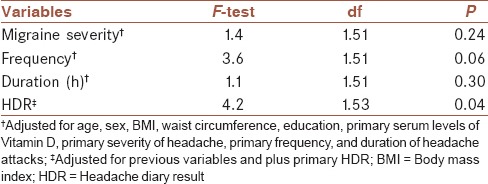
No significant difference was observed for mean severity and duration headache attacks among two groups. But, a mean difference of headache frequency was marginally significant (P = 0.06) and mean frequency of migraine was lower among intervention group to compared with control group (5.9 ± 7.0 vs. 7.0 ± 6.0). Mean HDR had significant difference among two groups (P = 0.04) that mean HDR was lower in the intervention group and compared to control group (85.0 ± 134.2 vs. 132.1 ± 147.1).
Two patients had positive CRP, however, other patients were negative CRP. One of two patients with positive CRP refused to continue. Thus, we can conclude that there were not a relationship between CRP with migraine.
DISCUSSION
In the present study, there was a significant difference in the mean daily headache among the intervention and control groups. Also, the mean difference in headache frequency was significance threshold between two groups. But, no association was shown in migraine with CRP.
In three case-report studies have been shown the role of Vitamin D in headache, including migraine.[18,20,21] Thys-Jacobs performed two case-reports on this issue in 1994.[20,21] A case-report study was performed in two female patients with migraine headache related to menstruation and premenstrual syndrome. In these two patients with low Vitamin D levels and with use of Vitamin D and calcium supplements (1600-1200 IU/day) were found significant decrease in migraine attacks and premenstrual symptoms in 2 months treatment.[20] Next study, was conducted among postmenopausal patients with migraine headache and low Vitamin D levels which with use of Vitamin D and calcium supplementations decreased the frequency and duration of migraine attacks, but the study was case-report study.[21] Prakash and Shah have been reported that use of Vitamin D and calcium supplementations (1500 IU Vitamin D3 and 1000 mg calcium per day) can be effective in headache improvement during 4-6 weeks. Although, Vitamin D was probably more important than compared with calcium in headache improvement.[18]
Two studies have found an inverse relationship between the serum Vitamin D levels with a headache.[19,22]
In 2008, Turner et al. reported that the prevalence of Vitamin D deficiency were 26% in 267 patients with chronic pain (25 patients with a headache).[31]
In a study performed in Norway, an inverse association was determined between headache with Vitamin D and also, the association was observed with adjustment for different variables such as age, sex, season, and geographical region.[22]
Wheeler have found that migraine patients have low levels of Vitamin D.[32] Prevalence and frequency of headaches was reported greater in Northern regions and areas with mean low temperature than in Southern regions in Greece.[33]
Serum levels of Vitamin D are higher among people in the lower latitudes that is a main factor for the low headache prevalence.[15]
In the else study, a significant association was not shown between serum Vitamin D levels and migraine headache, but significant relationship between nonmigraine headache with serum levels of Vitamin D was determined among nonsmokers group.[19]
In a study performed in Isfahan in autumn 2012 by Mottaghi et al., positive weak association was seen between serum levels of Vitamin D with HDR (P = 0.04, r = 0.19) and this relationship remained significant after adjusting confounding variables.[30]
One theory of migraine pathogenesis is neurogenic inflammation.[24,25] The CRP level, a marker of inflammation[26] and an acute-phase protein in blood, increases in response to inflammation.[24] CRP level has been described to be abnormal among patients with migraine, probably through vascular inflammation.[26,27]
Welch et al. reported a clinical report of 60 patients with migraine.[27] Findings demonstrated that 43% of the patients had increased CRP (defined as >3 mg/l), with a higher ratio in the patients without aura than in the patients with aura.[27]
A case–control study of 50 patients with migraine and 50 controls reported CRP level among migraineurs was higher (1.42 mg/l) compared to controls (0.90 mg/l) (P = 0.03).[34] CRP level was higher in patients without aura compared to controls, 2.11 mg/l versus 0.90 mg/l (P = 0.0002).[34]
Also, a Cohort study showed that CRP level was higher among patients with a history of migraine than in the women with no migraine history.[35] serum CRP levels were higher in the women without aura compared to women with aura.[35]
So, findings from these studies, suggest that CRP is modestly elevated among patients with migraine compared to controls.[26] But in our study, we didn't observe the relationship between CRP with migraine.
Amer and Qayyum reported a statistically significant inverse relationship between 25(OH)D at serum levels lower than 21 ng/ml with CRP. But described that 25(OH)D at serum level ≥21 ng/ml is associated with an increase in serum CRP. So, the role of Vitamin D supplementation to decrease inflammation is useful only among adults with lower serum 25(OH)D.[23]
The role of Vitamin D deficiency in the cause of headache is unfamiliar.[15]
The presence of alpha 1-hydroxylase enzyme, Vitamin D receptors and Vitamin D binding protein in the brain, especially hypothalamus[15] and low levels of magnesium[18] are the mechanism about the association between Vitamin D deficiency and headache. Because intestinal absorption of magnesium is dependent on Vitamin D.[18]
The strength of this study is the first clinical trial study in the world about the effect of Vitamin D supplementation on symptoms and CRP in patients with migraine. Sunlight exposure assessment was not measured in this study and was one limitation of our studies.
CONCLUSION
In summary, the present study showed that Vitamin D supplementation on the frequency and headaches diary result can be effective, although the effect on migraine frequency was significance threshold. But, no association was seen between migraine with CRP levels. Thus, it is required to do further clinical trial studies with larger sample size.
AUTHOR'S CONTRIBUTIONS
TM, FK, GA, RG designed, conducted and edited the manuscript. MM analyzed and interpreted data. All authors read and approved the final manuscript.
ACKNOWLEDGMENTS
The present study was supported by a grant (No. 391212) from Food Security Research Center, Isfahan University of Medical Sciences, Isfahan, Iran. We are grateful to Food Security Research Center in Isfahan.
Footnotes
Source of Support: Nil
Conflicts of Interest: No conflict of interests.
REFERENCES
- 1.Lateef TM, Cui L, Nelson KB, Nakamura EF, Merikangas KR. Physical comorbidity of migraine and other headaches in US adolescents. J Pediatr. 2012;161:308–13.e1. doi: 10.1016/j.jpeds.2012.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yoon MS, Katsarava Z, Obermann M, Fritsche G, Oezyurt M, Kaesewinkel K, et al. Prevalence of primary headaches in Germany: Results of the German Headache Consortium Study. J Headache Pain. 2012;13:215–23. doi: 10.1007/s10194-012-0425-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Battista J, Badcock DR, McKendrick AM. Migraine increases centre-surround suppression for drifting visual stimuli. PLoS One. 2011;6:e18211. doi: 10.1371/journal.pone.0018211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Inaloo S, Dehghani SM, Farzadi F, Haghighat M, Imanieh MH. A comparative study of celiac disease in children with migraine headache and a normal control group. Turk J Gastroenterol. 2011;22:32–5. doi: 10.4318/tjg.2011.0153. [DOI] [PubMed] [Google Scholar]
- 5.Headache Disorders. [Last accessed on 2004 Mar]. Available from: http://www.who.int/mediacentre/factsheets/fs277/en/
- 6.Steiner TJ. Lifting the Burden: The Global Campaign to Reduce the Burden of Headache Worldwide. Aids for management of common headache disorders in primary care. J Headache Pain. 2007;8:S26–9. [PubMed] [Google Scholar]
- 7.Unalp A, Dirik E, Kurul S. Prevalence and clinical findings of migraine and tension-type headache in adolescents. Pediatr Int. 2007;49:943–9. doi: 10.1111/j.1442-200X.2007.02484.x. [DOI] [PubMed] [Google Scholar]
- 8.Schürks M. Genetics of migraine in the age of genome-wide association studies. J Headache Pain. 2012;13:1–9. doi: 10.1007/s10194-011-0399-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mahdavi R, Tarighat Esfanjani A, Ebrahimi M, Talebi M, Ghaemmaghami J. Effects of oral magnesium for migraine prophylaxis. J Pharm Sci. 2009;15:103–8. [Google Scholar]
- 10.Schürks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T. Migraine and cardiovascular disease: Systematic review and meta-analysis. BMJ. 2009;339:b3914. doi: 10.1136/bmj.b3914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ertas M, Baykan B, Orhan EK, Zarifoglu M, Karli N, Saip S, et al. One-year prevalence and the impact of migraine and tension-type headache in Turkey: A nationwide home-based study in adults. J Headache Pain. 2012;13:147–57. doi: 10.1007/s10194-011-0414-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stovner LJ, Andree C. Prevalence of headache in Europe: A review for the Eurolight project. J Headache Pain. 2010;11:289–99. doi: 10.1007/s10194-010-0217-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Steiner TJ, Scher AI, Stewart WF, Kolodner K, Liberman J, Lipton RB. The prevalence and disability burden of adult migraine in England and their relationships to age, gender and ethnicity. Cephalalgia. 2003;23:519–27. doi: 10.1046/j.1468-2982.2003.00568.x. [DOI] [PubMed] [Google Scholar]
- 14.Safavi M, Nazari F, Mahmoody M. The relationship of migraine headache and life style among women. Iran J Nurs. 2008;21:89–100. [Google Scholar]
- 15.Prakash S, Mehta NC, Dabhi AS, Lakhani O, Khilari M, Shah ND. The prevalence of headache may be related with the latitude: A possible role of Vitamin D insufficiency? J Headache Pain. 2010;11:301–7. doi: 10.1007/s10194-010-0223-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andiran N, Çelik N, Akça H, Dogan G. Vitamin D deficiency in children and adolescents. J Clin Res Pediatr Endocrinol. 2012;4:25–9. doi: 10.4274/jcrpe.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moradzadeh K, Larijani B, Keshtkar AA, Hossein-Nezhad A, Rajabian R, Nabipour I, et al. Normative values of Vitamin D among Iranian population: A population based study. Int J Osteoporos Metab Dis. 2008;1:8–15. [Google Scholar]
- 18.Prakash S, Shah ND. Chronic tension-type headache with Vitamin D deficiency: Casual or causal association? Headache. 2009;49:1214–22. doi: 10.1111/j.1526-4610.2009.01483.x. [DOI] [PubMed] [Google Scholar]
- 19.Kjaergaard M, Eggen AE, Mathiesen EB, Jorde R. Association between headache and serum 25-hydroxyvitamin D: The Tromsø Study: Tromsø 6. Headache. 2012;52:1499–505. doi: 10.1111/j.1526-4610.2012.02250.x. [DOI] [PubMed] [Google Scholar]
- 20.Thys-Jacobs S. Vitamin D and calcium in menstrual migraine. Headache. 1994;34:544–6. doi: 10.1111/j.1526-4610.1994.hed3409544.x. [DOI] [PubMed] [Google Scholar]
- 21.Thys-Jacobs S. Alleviation of migraines with therapeutic Vitamin D and calcium. Headache. 1994;34:590–2. doi: 10.1111/j.1526-4610.1994.hed3410590.x. [DOI] [PubMed] [Google Scholar]
- 22.Knutsen KV, Brekke M, Gjelstad S, Lagerløv P. Vitamin D status in patients with musculoskeletal pain, fatigue and headache: A cross-sectional descriptive study in a multi-ethnic general practice in Norway. Scand J Prim Health Care. 2010;28:166–71. doi: 10.3109/02813432.2010.505407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Amer M, Qayyum R. Relation between serum 25-hydroxyvitamin D and C-reactive protein in asymptomatic adults (from the continuous National Health and Nutrition Examination Survey 2001 to 2006) Am J Cardiol. 2012;109:226–30. doi: 10.1016/j.amjcard.2011.08.032. [DOI] [PubMed] [Google Scholar]
- 24.Güzel I, Tasdemir N, Celik Y. Evaluation of serum transforming growth factor ß1 and C-reactive protein levels in migraine patients. Neurol Neurochir Pol. 2013;47:357–62. doi: 10.5114/ninp.2013.36760. [DOI] [PubMed] [Google Scholar]
- 25.Dalessio DJ. Vascular permeability and vasoactive substances: Their relationship to migraine. Adv Neurol. 1974;4:395–401. [PubMed] [Google Scholar]
- 26.Gudmundsson LS, Aspelund T, Scher AI, Thorgeirsson G, Johannsson M, Launer LJ, et al. C-reactive protein in migraine sufferers similar to that of non-migraineurs: The Reykjavik Study. Cephalalgia. 2009;29:1301–10. doi: 10.1111/j.1468-2982.2009.01865.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Welch KM, Brandes AW, Salerno L, Brandes JL. C-reactive protein may be increased in migraine patients who present with complex clinical features. Headache. 2006;46:197–9. doi: 10.1111/j.1526-4610.2006.00330.x. [DOI] [PubMed] [Google Scholar]
- 28.Sadre-Jahani S, Abolhassani M, Dehghani S, Jalili M, Talebpour M, Imani H, et al. Relationship between nutrient intake and body composition one year after bariatric surgery. Int Res J Appl Basic Sci. 2014;8:81–7. [Google Scholar]
- 29.Asadi B, Khorvash F, Najaran A, Khorvash F. Cyproheptadine versus propranolol in the prevention of migraine headaches in children. Pak J Med Sci. 2012;28:309–11. [Google Scholar]
- 30.Mottaghi T, Khorvash F, Askari G, Maracy MR, Ghiasvand R, Maghsoudi Z, et al. The relationship between serum levels of Vitamin D and migraine. J Res Med Sci. 2013;18:S66–70. [PMC free article] [PubMed] [Google Scholar]
- 31.Turner MK, Hooten WM, Schmidt JE, Kerkvliet JL, Townsend CO, Bruce BK. Prevalence and clinical correlates of Vitamin D inadequacy among patients with chronic pain. Pain Med. 2008;9:979–84. doi: 10.1111/j.1526-4637.2008.00415.x. [DOI] [PubMed] [Google Scholar]
- 32.Wheeler SD. Vitamin D deficiency in chronic migraine. Headache. 2008;48:S52–3. [Google Scholar]
- 33.Mitsikostas DD, Tsaklakidou D, Athanasiadis N, Thomas A. The prevalence of headache in Greece: Correlations to latitude and climatological factors. Headache. 1996;36:168–73. doi: 10.1046/j.1526-4610.1996.3603168.x. [DOI] [PubMed] [Google Scholar]
- 34.Vanmolkot FH, de Hoon JN. Increased C-reactive protein in young adult patients with migraine. Cephalalgia. 2007;27:843–6. doi: 10.1111/j.1468-2982.2007.01324.x. [DOI] [PubMed] [Google Scholar]
- 35.Kurth T, Ridker PM, Buring JE. Migraine and biomarkers of cardiovascular disease in women. Cephalalgia. 2008;28:49–56. doi: 10.1111/j.1468-2982.2007.01467.x. [DOI] [PubMed] [Google Scholar]


