Abstract
Background:
Dyslipidemia is considered as an important modifiable risk factor for cardiovascular disease (CVD). The link between childhood dyslipidemia and occurrence of atherosclerosis and its sequels in adulthood are well-documented. This study aimed to systematically review the prevalence of dyslipidemia among Iranian children and adolescents.
Materials and Methods:
An electronic search was conducted on studies published from January 1990 to January 2014. The main international electronic data sources were PubMed and the NLM Gateway (for MEDLINE), Institute of Scientific Information (ISI), and SCOPUS. For Persian databases, we used domestic databases with systematic search capability including IranMedex, Irandoc, and Scientific Information Database (SID). We included all available population-based studies and national surveys conducted in the pediatric age group (aged <21 years).
Results:
In this review, 1772 articles were identified (PubMed: 1464; Scopus: 11; ISI: 58; SID: 90; IranMedex: 149; Irandoc: 57). During three refine steps and after removing of duplicates, 182 articles related to the study domain were selected. After quality assessment, 46 studies were selected for text appraisal, of which 26 qualified articles were evaluated at the final step. The prevalence range of hypercholesterolemia, hypertriglyceridemia, elevated low-density lipoprotein cholesterol, and low high-density lipoprotein cholesterol (HDL-C) were 3-48%, 3-50%, 5-20% and 5-88%, respectively. Low HDL-C and hypertriglyceridemia were the most prevalent lipid disorders in this group of population.
Conclusion:
Dyslipidemia is a common health problem among Iranian children and adolescents. Few data were available in preschool children. This finding provides useful information for health policy makers to implement action-oriented interventions for prevention and early control of this important CVD risk factor.
Keywords: Dyslipidemia, Iran, lipid profile, pediatrics, prevalence, systematic review
INTRODUCTION
Metabolic risk factors (MRFs) including dyslipidemia are considered as the most important determinants of emerging noncommunicable diseases worldwide as reported by the Global Burden of Disease (GBD) studies in 1990, 2000, and 2013.[1,2,3,4,5,6,7,8] Dyslipidemia is the disorder of lipoprotein metabolism that result in elevated levels of total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), triglycerides, or decreased high-density lipoprotein cholesterol (HDL-C).[9] It is considered as an important modifiable risk factor for cardiovascular disease (CVD) and leading cause of morbidity and mortality worldwide.[10]
Though most of its types are not associated with significant adverse health outcomes in childhood, but a growing body of evidence indicated the tracking of CVD risk factors and a link between childhood dyslipidemia and occurrence of atherosclerosis and its sequels in adulthood.[11,12] It is reported that 40–55% of children with dyslipidemia will have hyperlipidemia during adulthood.[13] It is well-established that subclinical atherosclerotic abnormalities, which result in CVD events, occurs in childhood.[14]
The recent striking increase of CVD risk factors in the pediatric age group, especially in developing countries, suggests that this group of population is at risk of epidemic of premature CVD in the near future.[15,16] Prevention and control of CVD risk factors, including dyslipidemia, from early life may act as primordial, primary, or secondary prevention.[17] To address this issue, we need scientific evidences on a different aspect of disorder epidemiology. Several studies worldwide have investigated the prevalence of dyslipidemia in children and adolescents, and have reported a wide range of variety in different regions.[18,19,20]
Iran has been experiencing a rapid epidemiological transition, and is facing a double burden of the diseases due to urbanization and nutrition transition.[21,22] A nationwide survey conducted in Iranian and adolescents reported a prevalence of 45.7% for dyslipidemia, notably in terms of low HDL-C and hypertriglyceridemia.[23] There are also few regional studies in this field in Iran, but the findings are scattered or are limited to different subgroups of population. There are a few studies on the sub national distribution of the disorder among children, and there is no information about their trends and their effects on the health.[24,25,26]
It seems that a comprehensive epidemiological feature of dyslipidemia would help us to provide baseline information regarding the burden of disease, research priorities, appropriate allocation of health system resources, and establishing proper screening programs.[27,28,29]
Therefore, it can be assumed that planning preventive programs from early life may be considered as a priority for the health system to attenuate the burden of CVDs. The aim of the current study was to systematically review the prevalence of dyslipidemia among Iranian children and adolescents to provide baseline information for policy makers for future preventative and interventional strategies at individual and public health levels.
MATERIALS AND METHODS
This nationwide study was conducted in the framework of the national and sub-national burden of diseases study. The details of the study are reported previously.[30,31]
This study was designed as a systematic review on the prevalence of dyslipidemia among Iranian pediatric population at national and sub-national levels in Iran, from 1990 to 2013. Regional ethics committee of Isfahan University of Medical Sciences and Tehran University of Medical Sciences approved the protocol of the current systematic review.
Search strategy
By an electronic search, studies published from January 1990 to January 2014 were used. The main international electronic data sources were PubMed and the NLM Gateway (for MEDLINE), Institute of Scientific Information (ISI), and SCOPUS. For Persian documents, domestic databases with systematic search capability including Iranmedex, Irandoc, and Scientific Information Database (SID), were used. For each database, strategies were run separately regarding the detailed practical instruction including filters and refining processes.
The search terms limited to:
National, provincial, district, community population-based studies,
The pediatric age group, that is, under 23 years
Iran,
Human subject, and without restriction on language.
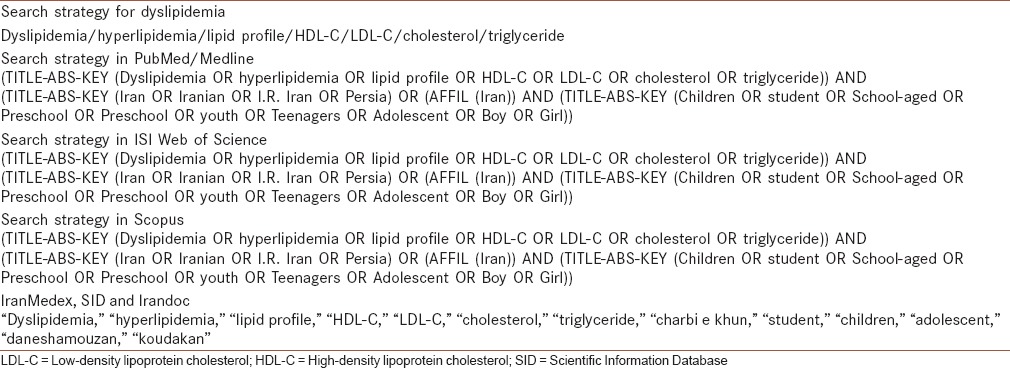
The medical subject headings and Emtree of Scopus were used to reach the most comprehensive and efficient search. For the national search engines, the Persian keywords were equivalent to their English search terms, and all probable combinations were considered [Table 1]. We excluded papers of nonpopulation-based studies or those with duplicate citation. For multiple publications of the same population, only the article with largest sample size was included.
Table 1.
Search strategy for dyslipidemia in Iranian pediatric population
National data sources
We used the aggregated data of Childhood and Adolescence Surveillance and Prevention of Adult Non-Communicable Disease (CASPIAN I and III) study as the main available national data source for the cardio MRFs of children and adolescents in Iran.[32,33]
Study selection and quality evaluation
The entire text or summary of all searched articles, documents, and reports were extracted. After reviewing and studying the titles of documents, the repeated items were excluded, and then, the full texts of articles were carefully studied by researchers. The related articles were selected, and the irrelevant ones were excluded.
The quality of the documents was evaluated independently by two research experts for the objective of each research project, study method, sample size, sampling method, data collection tool, variables evaluation status, and the studied target group. Using Cohen's kappa statistic, the kappa statistic for agreement for quality assessment was 0.92. After selection of eligible papers, data were extracted to predefined standard electronic data extraction sheets.
RESULTS
In this review, 1772 articles were identified through electronic database search (PubMed: 1464; Scopus: 11; ISI: 58; SID: 90; IranMedex: 149; Irandoc: 57). During three refine steps and after removing of duplicates, 182 articles related to the study domain were selected. After quality assessment, 46 studies were selected for text appraisal, of which 26 qualified articles were evaluated at the final step.[34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59] Overall, 4 of 26 articles were from the CASPIAN I and III studies [Figure 1]. Three of the selected papers were from Tehran Lipid and Glucose Study, which is a cohort study, the rest of papers were cross–sectional studies conducted in different parts of Iran.
Figure 1.
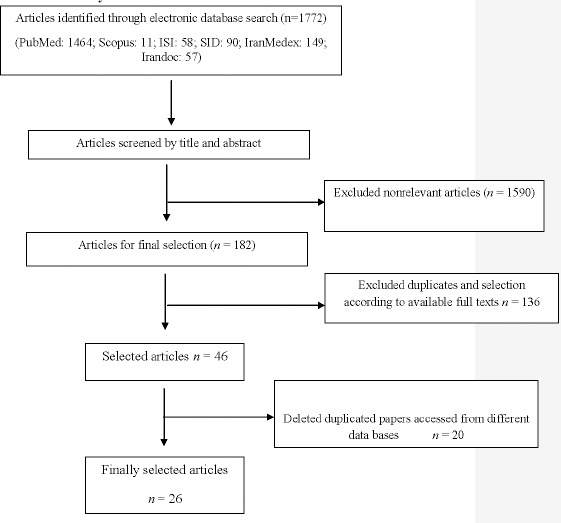
Flowchart of study selection
Considering the whole data of systematic review results and national data sources; the number of total population and points of data were 40,440, and 92, respectively. From reported points of data, 36 of them were for total population and 29 and 27 of them were for girls and boys, respectively. As well as regarding the geographically distribution, we find 2 national, 7 provincial, and 5 district level points of data.
The difference between two above values is related to some cases that did not report separation of two different sexes or in some of the studies, the studied population were only girls.
One of the articles (1 out of 26) was related to lipid measurements in the neonatal period.[43] According to that study, female neonates had higher TC and HDL-C than male neonates (81.4 ± 28.3 vs. 75.2 ± 21.1, P = 0.02, and 31.18 ± 9.97 vs. 28.8 ± 8.7, P = 0.02, respectively).
Data related to children below 6 years old were available only in Tehran Lipid and Glucose Study.[39,47] Accordingly, prevalence of hypercholesterolemia, hypertriglyceridemia, elevated LDL-C, and low HDL-C among children below 6 years old were 8% (95%CI: 5.47-11.12), 3% (95%CI: 1.6-5.34), 10% (95%CI: 7.10-5.34), and 12% (95%CI: 8.93-15.8), respectively. All types of dyslipidemia in this age group except hypertriglyceridemia were significantly higher in girls than boys.[39]
Most of the studies (76.9%; 20/26) presented data related to children above 6 years old. The findings of CASPIAN I and III studies which were the only nationwide study in children aged 6-18 years, showed that estimate prevalence rate of hypercholesterolemia, hypertriglyceridemia, elevated LDL-C and low HDL-C in CASPIAN I (2003-2004) was 6.4% (5.27-7.13), 24.5% (23.29-15.07), 6.3% (5.63-7.03), and 24.8% (23.58-26.08), respectively. Estimated prevalence rate of hypercholesterolemia, hypertriglyceridemia, elevated LDL-C, and low HDL-C in CASPIAN III (2009-2010) was 5.6% (5.0-6.20), 7.9% (7.2-8.6), 5.7% (5.1-6.3), and 35.36% (34.1-36.6), respectively.
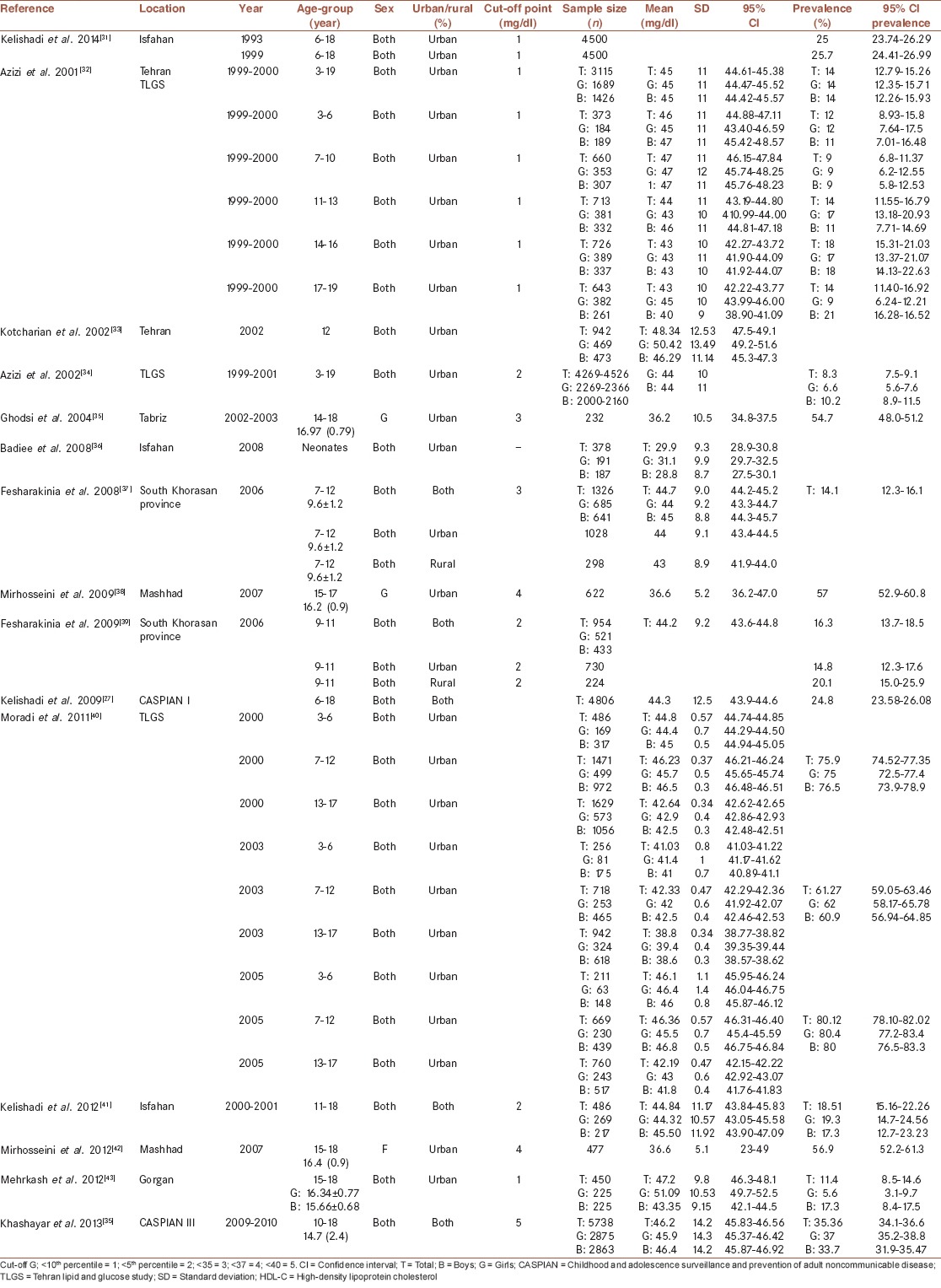
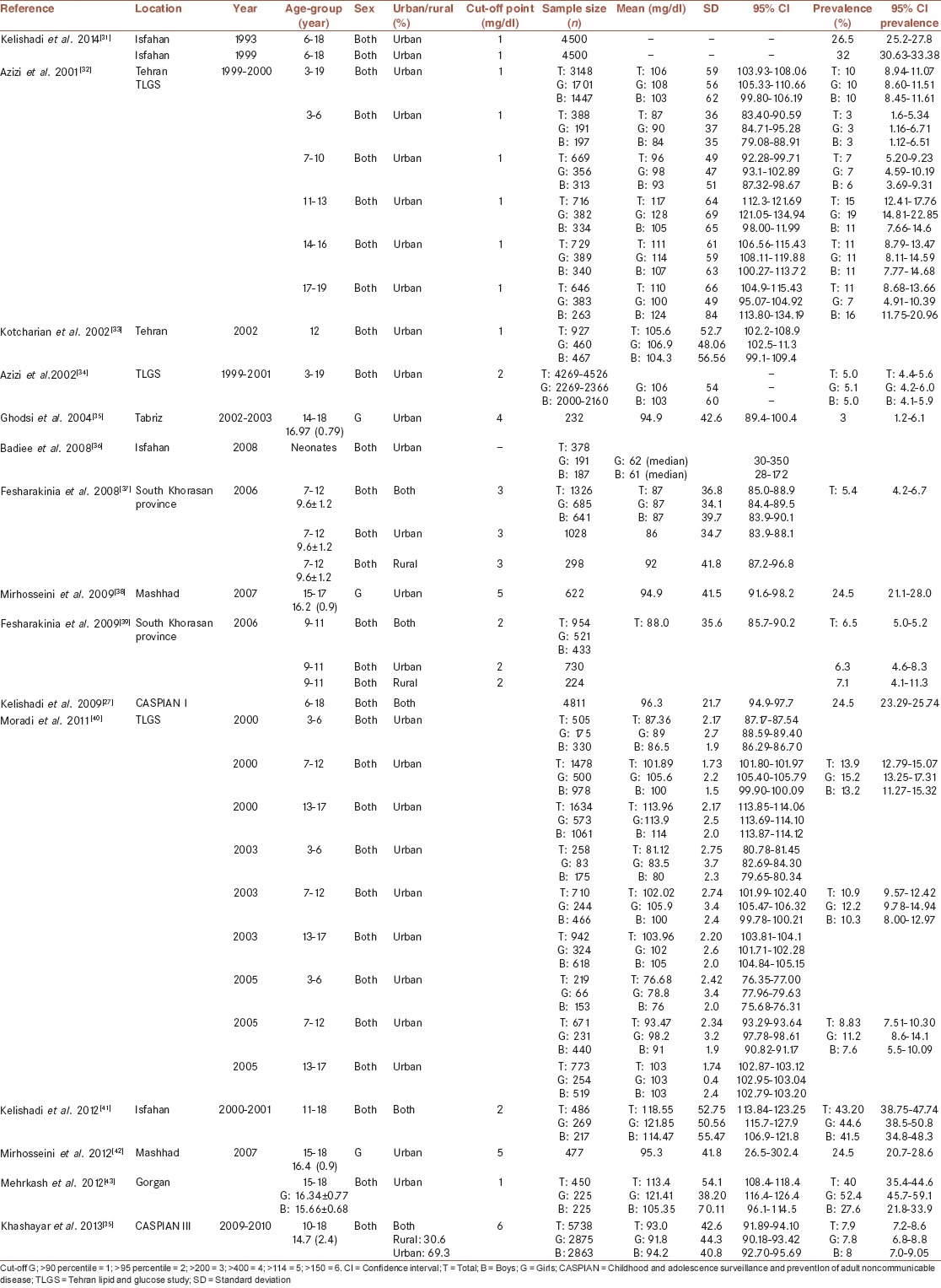
Tables 2–5 represent the prevalence of hypercholesterolemia, hypertriglyceridemia, elevated LDL-C, and low HDL-C in population-based studies in Iranian children and adolescences during 1990-2013. The prevalence of different types of dyslipidemia was based on definitions used in mentioned studies.
Table 2.
The prevalence of hypercholesterolemia in population-based studies in Iranian children and adolescences of Iran: 1990-2013
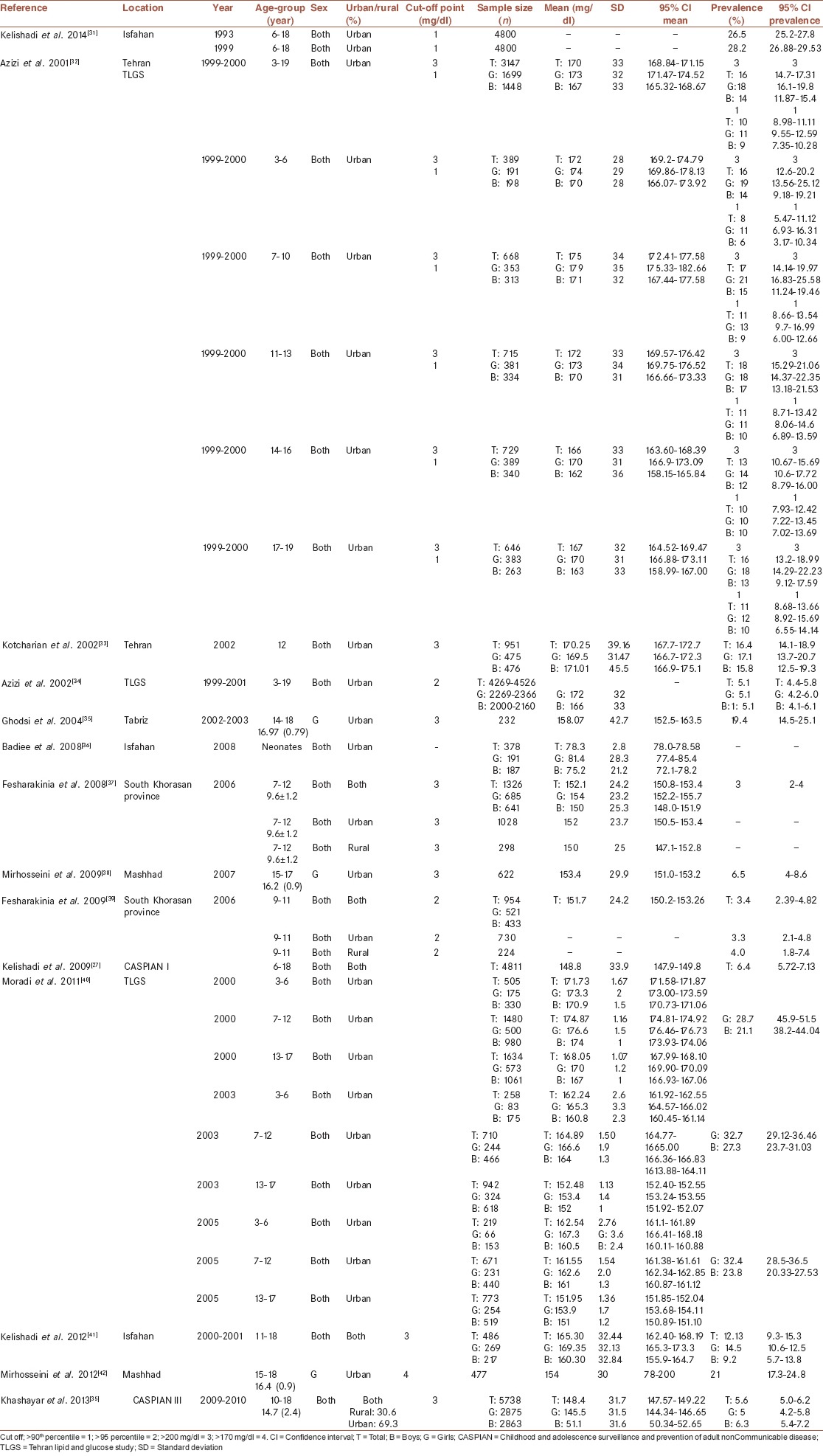
Table 5.
The prevalence of low HDL-C in population-based studies in Iranian children and adolescences of Iran: 1990-2013
In Table 2, the prevalence rates of hypercholesterolemia reported by national and regional studies, in different age and sex groups are presented. The number of total population and points of data were 40,440, and 89 (34 for total, 29 for girls and 26 for boys), respectively. A wide range of hypercholesterolemia was reported by mentioned studies. Some of them reported a rate of <10%, some between 10% and 20% and there were studies which reported >30%. The rate was 5-7% and 5-6% in CASPIAN I and III, respectively. It seems that hypercholesterolemia was more prevalent among girls, but it was not different between urban and rural areas.
In Table 3, the prevalence rates of hypertriglyceridemia in different age and sex groups reported by national and regional studies are presented. The number of total population and points of data were 39782 and 76 (29 for total, 25 for girls and 22 for boys), respectively. Reported prevalence rates of hypertriglyceridemia varied with a range of 3-50%. The rate was 24-26% and 7-9% in CASPIAN I and III, respectively. The rate was similar between urban and rural. The prevalence rates regarding gender differences were varied in different studies.
Table 3.
The prevalence of hypertriglyceridemia in population-based studies in Iranian children and adolescences of Iran: 1990-2013
Reported prevalence rates of elevated LDL-C reported by national and regional studies according to age and sex groups are presented in Table 4. The number of total population and points of data were 38,194 and 92 (36 for total, 27 for girls and 29 for boys), respectively. The range of elevated LDL-C in Iranian children and adolescences were between 5% and 20%, there was one report for 30%. The rate was 5-7% in both CASPIAN I and III studies. The rate was similar between urban and rural. The prevalence rates regarding gender differences were varied in different studies.
Table 4.
The prevalence of elevated LDL-C in population-based studies in Iranian children and adolescences of Iran: 1990-2013
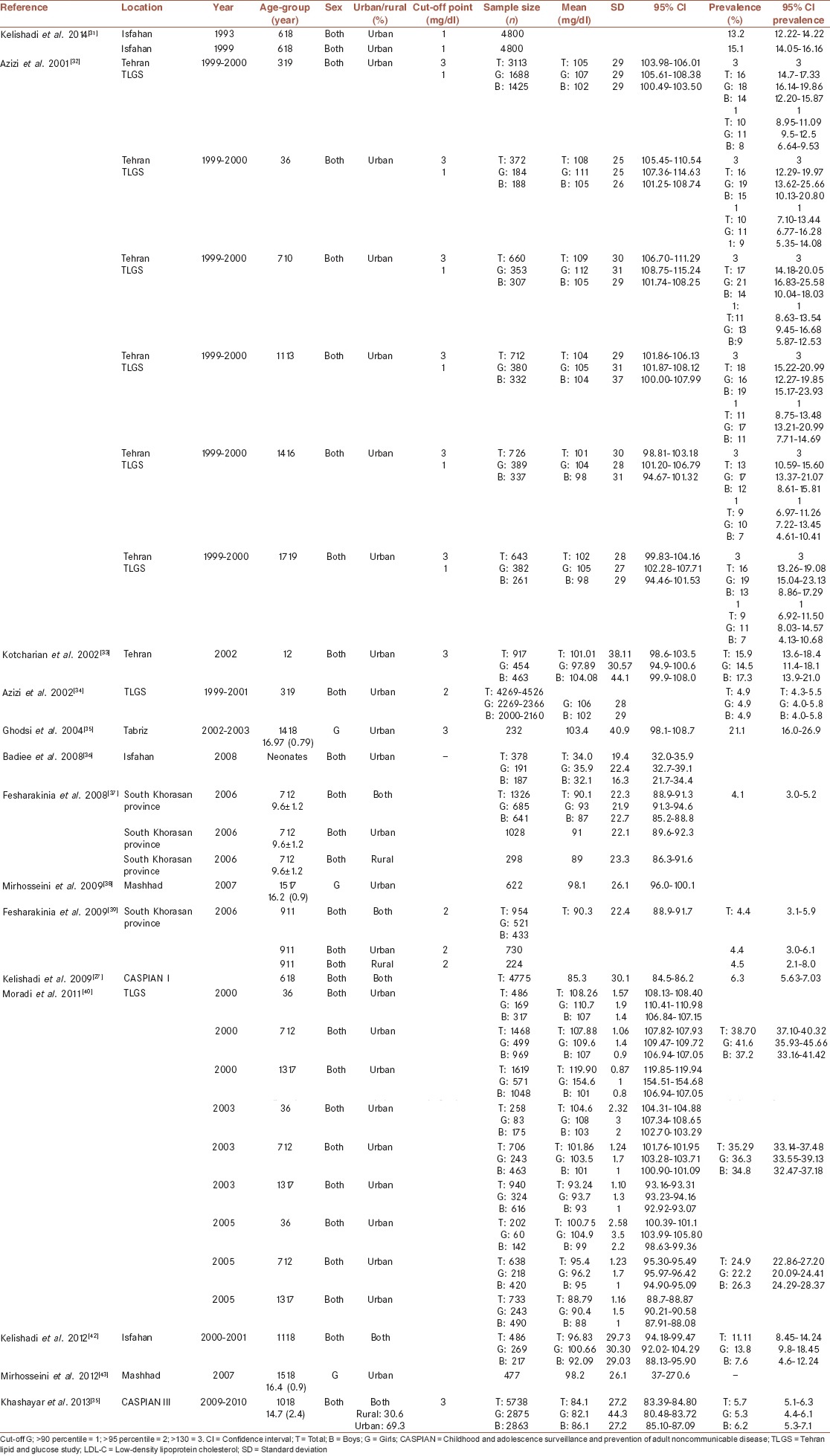
The prevalence rates of low HDL-C according to national and regional reports in different age and sex groups are presented in Table 5. The number of total population and points of data were 40,194 and 77 (30 for total, 25 for girls and 22 for boys), respectively. The prevalence of low HDL-C has been reported to be between 6% and 33%, there were two studies with a higher rate of low HDL-C (53–57%) among adolescents. The rate was 24-26% and 34-37% in CASPIAN I and III, respectively. The rate of low HDL-C was higher in one study among the rural population. The prevalence rates regarding gender differences were varied in different studies.
DISCUSSION
In this study, we systematically reviewed studies that reported the prevalence of dyslipidemia among Iranian pediatric population. Iranian neonates have a higher level of TG in comparison with other countries.[43] Hypertriglyceridemia and low HDL-C are considered as the most common lipid disorder among Iranian children and adolescents (34, 35, 38-450).[31,34]
Children with dyslipidemia are predicted to have symptomatic coronary artery disease before the age of 30.[60] So that it shall be considered as the main target of intervention for preventive strategies.[61] Some experts propose screening of dyslipidemia in children and adolescents.[11]
Available data have indicated an increasing prevalence rate of dyslipidemia in most countries worldwide. A recent study indicated that dyslipidemia is affecting 1 in 5 adolescents, although most are mild or moderate abnormalities.[62]
The National Health and Nutrition Examination Survey (NHANES) (1999-2006) in the United States of America (USA) have reported that the prevalence of dyslipidemia among 3,125 youths aged 12-19 years was 20.3%.[63] But, according to a recent report, the prevalence of hypercholesterolemia, high LDL-C, and high TG continue to decrease in the USA.[64] The increasing trend is more significant in developing countries as Iran because of urbanization, epidemiologic transition, notably nutrition transition.[65,66]
In our literature review, we did not find any systematic review on the prevalence of dyslipidemia among children. Prevalence of dyslipidemia among the adult Iranian population was reported in a recent study.[67] Data regarding the prevalence of dyslipidemia in different parts of the world are obtained from cross–sectional, longitudinal, and national studies.
In the current study, the most commonly used sources of data were from different surveys of the CASPIAN study, as the only nationwide study in this field in Iran.[28,34,35] In addition, the data of a number of community-based epidemiological studies at smaller scales were included, as well.
The results of this review showed that the prevalence range of hypercholesterolemia, hypertriglyceridemia, elevated LDL-C, and low HDL-C among Iranian children and adolescents were 3-48%, 3-50%, 5-20%, and 5-88%, respectively.
According to the results of Korea NHANES IV (2007-2009), the prevalence of hypercholesterolemia, high LDL-C, high TG, and low HDL-C was 6.5%, 4.7%, 10.1%, and 7.1%, respectively, among 2363 subjects aged 10-18 years.[18]
Prevalence of hypercholesterolemia among 200 schoolchildren aged 12-18 years was 50% in India.[68]
In a Study in Saudi Arabia, among 1390 boys and girls aged 9-12 years, the prevalence of hypercholesterolemia, elevated LDL-C, and hypertriglyceridemia is reported as 32.7%, 33.1%, and 34.1%, respectively.[19]
In a cross–sectional study in Thailand, among 348 schoolchildren aged 6-17.8 years, the prevalence of hypercholesterolemia and hypertriglyceridemia was 1.2% and 10.6%, respectively.[69]
Reported prevalence rate for different types of dyslipidemia in reviewed studies from Iran had a wide range. It may be due to differences in studied age and sex groups, genetic and ethnic background in various parts of a vast country like Iran, year of study, sampling methods, as well as different laboratory methods and the criteria used to define dyslipidemia in the pediatric age group.
Though comparing our results with other studies would not be conclusive enough because of differences in studied population, lab methods etc., it seems that the prevalence of dyslipidemia among Iranian children and adolescents is high specially hypertriglyceridemia and low HDL-C. The prevalence rate of hypertriglyceridemia and low HDL-C decreased and increased, respectively, from CASPIN I to III possibly due to factors such as studied population (23 provinces in CASPIAN I and 27 provinces in CASPIAN III), the age group studied (6–18 years in CASPIAN-I and 10–18 years in CASPIAN-III) and positive effect of some interventions or nationwide educational programs in this field.[34,35] In addition, the role of dietary habits, physical activity level, and nutrition transition in Iran should be considered as well.
Several studies demonstrated sex, race, and ethnic differences in lipid profiles and prevalence of dyslipidemia in different regions[70,71,72,73] of special concern are the ethnic differences in the type and the prevalence of dyslipidemia. While most studies conducted in Western countries documented high prevalence rates of elevated TC and LDL-C, many epidemiologic studies have shown a high prevalence of hypertriglyceridemia and low HDL-C in the adult and pediatric population of the Middle East, even among immigrants from this region to Western countries (367,367).
National studies in Iran revealed a markedly high prevalence of this disturbance in adults as well as in the pediatric age group, even in normal-weight children and adolescents.[34] Moreover, the 5th percentile of serum HDL-C level of Iranian children and adolescents is lower than their European and American counterparts suggesting that the leftward shift in the distribution of this trait among Iranians begins in childhood.[27,29]
Considering the results of the current review, the prevalence of dyslipidemia among rural and urban population was studied in few studies (CASPIAN study and Fesharakinia et al.). According to the results of CASPIAN study, dyslipidemia was more prevalent among urban population. In reminder studies, there was no significant difference between different type of dyslipidemia among rural and urban population except for low HDL-C, which was higher in rural areas.[46]
Some studies showed that dyslipidemia is more prevalent among children with higher socioeconomic levels and higher-income families.[74,75] Contrary, in a study in Ecuador, children in the rural area were 2.8 times more likely to have dyslipidemia than those from the urban area.[76] Unhealthy lifestyle, improper type of fat used for food preparation, using deep fried foods and unhealthy snacks may explain the differences in lipid levels and dyslipidemia in various living areas.
It seems that according to this review, the overall prevalence of dyslipidemia among females is higher than males. But regarding different types of dyslipidemia, the results had heterogeneity.
Several studies reported gender differences in the prevalence of dyslipidemia in children. Among Korean children, girls had higher TC and LDL-C than boys. Girls also tended to have higher HDL-C than boys after the age of 12-13 years, the period of pubertal development.[18]
Similar results obtained from a nationwide study in Japan among schoolchildren.[77] In a study in Turkey, among 2896 children (1467 girls, 1429 boys) aged 7-18 years, the prevalence of dyslipidemia according to nonHDL-C levels was higher (13.2%) in girls than boys (8.9%) (P < 0.001).[78] Whereas, using the data of NHANES 1999-2006 for participants aged 6-17 years, Ford et al. have reported a higher level of cholesterol and LDL-C among boys than girls.[60]
The main strength of this review is its novelty in the pediatric age group. There was limited number of comprehensive study for sub-national trends of the disorders in Iran.[79,80,81] The superiority of the findings of this review to the GBD studies is that we benefit from more data driven estimations rather than the model driven results.[1,4,5,6,7,8] We also benefited from all available national and sub-national sources of data alongside the advanced comprehensive search approaches. All of the domestic databases were searched exactly with all of English/Persian equivalent search terms. We had the availability to use the highest level of access to the published, available unpublished and gray literature, as well as the main national sources of CASPIAN study.[33,82]
We have also faced with some limitations. The most important limitations of this review were diversities related to the geographical scopes of studies (local, district, and national levels), quality of data, methodology of the studies and studied population (children, adolescents or both), which limited our ability to compare presented data. So that, findings of this review indicated that the reported prevalence range of all subgroups of dyslipidemia had large variations. It seems that because of ethical concerns and difficulties in blood sampling from young children, data were scarce on the prevalence of dyslipidemia among preschool-aged children, that is, under 5 years of age. Most studies included in this review have been conducted in school-aged children and adolescents. Moreover in almost all cases with missing data our contacts with the authors of the studies were not effective and did not provide us any additional data than those reported in their articles. Considering above, to comparing the results, aggregating the data, and imputing the trends, we provide more modern practical statistical methods.[30,83,84]
The implication of this study was that reviewing the results of different studies of dyslipidemia from different regions of Iran, in different years, age and sex groups provide us comprehensive baseline information in this field. Obtained data could be used for future studies and planning health-related policies in this regard.
CONCLUSION
Reviewing existing date in the field of children dyslipidemia in Iran, the results indicated that dyslipidemia is one of the common and important CVD risk factors among Iranian children, which emphasize on the necessity of effective interventional trials implementation.[31,85] The feature of dyslipidemia among Iranian children with a higher rate of hypertriglyceridemia and low HDL-C indicates the priority of our future interventions also. In addition, regarding the fact that few data were available in preschool children, it seems that screening of dyslipidemia considered as a priority for health care system in our country to eliminate the burden of disease and preventing it related increasing rate of CVD in future.
AUTHOR'S CONTRIBUTIONS
SH contributed in the conception of the work, conducting the study, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. RK contributed in the conception of the work, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. Sh Dj contributed in the conception of the work, conducting the study, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. FF contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. SHN contributed in the conception of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. MQ contributed in the conception of the work, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
ACKNOWLEDGMENTS
The study is granted by Ministry of Health and Medical Education of Islamic Republic of Iran and Setad-e-EjraieFarmane Imam.
Footnotes
Source of Support: Nil
Conflicts of Interest: None declared.
REFERENCES
- 1.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murray CJ, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C, et al. GBD 2010: A multi-investigator collaboration for global comparative descriptive epidemiology. Lancet. 2012;380:2055–8. doi: 10.1016/S0140-6736(12)62134-5. [DOI] [PubMed] [Google Scholar]
- 3.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997;349:1498–504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 4.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349:1436–42. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 5.Lopez AD. The evolution of the Global Burden of Disease framework for disease, injury and risk factor quantification: Developing the evidence base for national, regional and global public health action. Global Health. 2005:1–5. doi: 10.1186/1744-8603-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ. Comparative Risk Assessment Collaborating Group. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–60. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 7.Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9·1 million participants. Lancet. 2011;377:557–67. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stevens GA, Singh GM, Lu Y, Danaei G, Lin JK, Finucane MM, et al. National, regional, and global trends in adult overweight and obesity prevalences. Popul Health Metr. 2012:10–22. doi: 10.1186/1478-7954-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haney EM, Huffman LH, Bougatsos C, Freeman M, Fu R, Steiner RD, et al. Rockville, MD: Agency for Healthcare Research and Quality (US); 2007. Screening for Lipid Disorders in Children and Adolescents. [PubMed] [Google Scholar]
- 10.Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: Summary report. Pediatrics. 2011;128(Suppl 5):S213–56. doi: 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Daniels SR. Screening and treatment of dyslipidemias in children and adolescents. Horm Res Paediatr. 2011;76(Suppl 1):47–51. doi: 10.1159/000329163. [DOI] [PubMed] [Google Scholar]
- 12.Psaty BM, Rivara FP. Universal screening and drug treatment of dyslipidemia in children and adolescents. JAMA. 2012;307:257–8. doi: 10.1001/jama.2011.1916. [DOI] [PubMed] [Google Scholar]
- 13.Hatami M, Tohidi M, Mohebi R, Khalili D, Azizi F, Hadaegh F. Adolescent lipoprotein classifications according to National Health and Nutrition Examination Survey (NHANES) vs. National Cholesterol Education Program (NCEP) for predicting abnormal lipid levels in adulthood in a Middle East population. Lipids Health Dis. 2012:11–107. doi: 10.1186/1476-511X-11-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zachariah JP, de Ferranti SD. NHLBI integrated pediatric guidelines: Battle for a future free of cardiovascular disease. Future Cardiol. 2013;9:13–22. doi: 10.2217/fca.12.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prasad DS, Kabir Z, Dash AK, Das BC. Childhood cardiovascular risk factors in South Asians: A cause of concern for adult cardiovascular disease epidemic. Ann Pediatr Cardiol. 2011;4:166–71. doi: 10.4103/0974-2069.84663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rodrigues AN, Abreu GR, Resende RS, Goncalves WL, Gouvea SA. Cardiovascular risk factor investigation: A pediatric issue. Int J Gen Med. 2013;6:57–66. doi: 10.2147/IJGM.S41480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weintraub WS, Daniels SR, Burke LE, Franklin BA, Goff DC, Jr, Hayman LL, et al. Value of primordial and primary prevention for cardiovascular disease: A policy statement from the American Heart Association. Circulation. 2011;124:967–90. doi: 10.1161/CIR.0b013e3182285a81. [DOI] [PubMed] [Google Scholar]
- 18.Yang S, Hwang JS, Park HK, Lee HS, Kim HS, Kim EY, et al. Serum lipid concentrations, prevalence of dyslipidemia, and percentage eligible for pharmacological treatment of Korean children and adolescents; data from the Korea National Health and Nutrition Examination Survey IV (2007-2009) PLoS One. 2012;7:e49253. doi: 10.1371/journal.pone.0049253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al-Shehri SN, Saleh ZA, Salama MM, Hassan YM. Prevalence of hyperlipidemia among Saudi school children in Riyadh. Ann Saudi Med. 2004;24:6–8. doi: 10.5144/0256-4947.2004.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mier N, Smith ML, Irizarry D, Carrillo-Zuniga G, Lee C, Trevino L, et al. Bridging research and policy to address childhood obesity among border Hispanics: A pilot study. Am J Prev Med. 2013;44:S208–14. doi: 10.1016/j.amepre.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 21.Motlagh ME, Kelishadi R, Amirkhani MA, Ziaoddini H, Dashti M, Aminaee T, et al. Double burden of nutritional disorders in young Iranian children: Findings of a nationwide screening survey. Public Health Nutr. 2011;14:605–10. doi: 10.1017/S1368980010002399. [DOI] [PubMed] [Google Scholar]
- 22.Sarrafzadegan N, Kelishadi R, Sadri G, Malekafzali H, Pourmoghaddas M, Heidari K, et al. Outcomes of a comprehensive healthy lifestyle program on cardiometabolic risk factors in a developing country: The Isfahan Healthy Heart Program. Arch Iran Med. 2013;16:4–11. [PubMed] [Google Scholar]
- 23.Kelishadi R, Ardalan G, Gheiratmand R, Ramezani A. Is family history of premature cardiovascular diseases appropriate for detection of dyslipidemic children in population-based preventive medicine programs? CASPIAN study. Pediatr Cardiol. 2006;27:729–36. doi: 10.1007/s00246-006-1391-3. [DOI] [PubMed] [Google Scholar]
- 24.Kelishadi R. Childhood overweight, obesity, and the metabolic syndrome in developing countries. Epidemiol Rev. 2007;29:62–76. doi: 10.1093/epirev/mxm003. [DOI] [PubMed] [Google Scholar]
- 25.Kelishadi R, Gharipour M, Sadri GH, Tavasoli AA, Amani A. Cardiovascular disease risk factors, metabolic syndrome and obesity in an Iranian population. East Mediterr Health J. 2008;14:1070–9. [PubMed] [Google Scholar]
- 26.Kelishadi R, Motlagh ME, Roomizadeh P, Abtahi SH, Qorbani M, Taslimi M, et al. First report on path analysis for cardiometabolic components in a nationally representative sample of pediatric population in the Middle East and North Africa (MENA): the CASPIAN-III Study. Ann Nutr Metab. 2013;62:257–65. doi: 10.1159/000346489. [DOI] [PubMed] [Google Scholar]
- 27.Smith SC, Jr, Jackson R, Pearson TA, Fuster V, Yusuf S, Faergeman O, et al. Principles for national and regional guidelines on cardiovascular disease prevention: A scientific statement from the World Heart and Stroke Forum. Circulation. 2004;109:3112–21. doi: 10.1161/01.CIR.0000133427.35111.67. [DOI] [PubMed] [Google Scholar]
- 28.Smith S, Voûte J, Fuster V. Principles for national and regional guidelines on cardiovascular disease prevention. Nat Clin Pract Cardiovasc Med. 2006;3:461. doi: 10.1038/ncpcardio0655. [DOI] [PubMed] [Google Scholar]
- 29.Labarthe DR. Boston: Jones & Bartlett Publishers; 2010. Epidemiology and Prevention of Cardiovascular Diseases: A Global Challenge. [Google Scholar]
- 30.Farzadfar F, Delavari A, Malekzadeh R, Mesdaghinia A, Jamshidi HR, Sayyari A, et al. NASBOD 2013: Design, definitions, and metrics. Arch Iran Med. 2014;17:7–15. [PubMed] [Google Scholar]
- 31.Kelishadi R, Hovsepian S, Qorbani M, Jamshidi F, Fallah Z, Djalalinia S, et al. National and sub-national prevalence, trend, and burden of cardiometabolic risk factors in Iranian children and adolescents, 1990-2013. Arch Iran Med. 2014;17:71–80. [PubMed] [Google Scholar]
- 32.Motlagh ME, Kelishadi R, Ardalan G, Gheiratmand R, Majdzadeh R, Heidarzadeh A, et al. Rationale, methods and first results of the Iranian national programme for prevention of chronic diseases from childhood: CASPIAN Study. East Mediterr Health J. 2009;15:302–14. [PubMed] [Google Scholar]
- 33.Kelishadi R, Heshmat R, Motlagh ME, Majdzadeh R, Keramatian K, Qorbani M, et al. Methodology and Early Findings of the Third Survey of CASPIAN Study: A National School-based Surveillance of Students’ High Risk Behaviors. Int J Prev Med. 2012;3:394–401. [PMC free article] [PubMed] [Google Scholar]
- 34.Kelishadi R, Amirkhani A, Ardalan G, Ziaoddini H, Majdzadeh R. An overview of a national surveillance program in Iran for prevention of chronic non-communicable diseases from childhood: CASPIAN study. Iran J Public Health. 2009;38(Suppl 1):102–6. [Google Scholar]
- 35.Khashayar P, Heshmat R, Qorbani M, Motlagh ME, Aminaee T, Ardalan G, et al. Metabolic Syndrome and Cardiovascular Risk Factors in a National Sample of Adolescent Population in the Middle East and North Africa: The CASPIAN III Study. Int J Endocrinol. 2013:2013–702095. doi: 10.1155/2013/702095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schwandt P, Kelishadi R, Ribeiro RQ, Haas GM, Poursafa P. A three-country study on the components of the metabolic syndrome in youths: The BIG Study. Int J Pediatr Obes. 2010;5:334–41. doi: 10.3109/17477160903497043. [DOI] [PubMed] [Google Scholar]
- 37.Kelishadi R, Ardalan G, Gheiratmand R, Adeli K, Delavari A, Majdzadeh R, et al. Paediatric metabolic syndrome and associated anthropometric indices: The CASPIAN Study. Acta Paediatr. 2006;95:1625–34. doi: 10.1080/08035250600750072. [DOI] [PubMed] [Google Scholar]
- 38.Kelishadi R, Hashemipour M, Sarraf-Zadegan N, Amiri M. Trend of atherosclerosis risk factors in children of Isfahan. Asian Cardiovasc Thorac Ann. 2001;9:36–40. [Google Scholar]
- 39.Azizi F, Rahmani M, Madjid M, Allahverdian S, Ghanbili J, Ghanbarian A, et al. Serum lipid levels in an Iranian population of children and adolescents: Tehran lipid and glucose study. Eur J Epidemiol. 2001;17:281–8. doi: 10.1023/a:1017932212350. [DOI] [PubMed] [Google Scholar]
- 40.Kotcharian A, Mohammadi AA, Mojtahedzadeh R. Hyperlipidemia in 12 year-old children living in Tehran. Acta Med Iran. 2002;40:20–5. [Google Scholar]
- 41.Azizi F, Rahmani M, Emami H, Mirmiran P, Hajipour R, Madjid M, et al. Cardiovascular risk factors in an Iranian urban population: Tehran lipid and glucose study (phase 1) Soz Praventivmed. 2002;47:408–26. doi: 10.1007/s000380200008. [DOI] [PubMed] [Google Scholar]
- 42.Ghodsi D, Mahboob S, Omidvar N, Eezadifard S, Ostadrahimi A, Koshavar H. Lipid profile and its correlates with nutrition and socioeconomic status in adolescent girls in Tabriz high schools. Iran J Endocrinol Metab. 2004;6:55–62. [Google Scholar]
- 43.Badiee Z, Kelishadi R. Cord blood lipid profile in a population of Iranian term newborns. Pediatr Cardiol. 2008;29:574–9. doi: 10.1007/s00246-007-9149-0. [DOI] [PubMed] [Google Scholar]
- 44.Fesharakinia A, Zarban A, Sharifzadeh GR. Lipid profiles and prevalence of dyslipidemia in schoolchildren in south Khorasan Province, eastern Iran. Arch Iran Med. 2008;11:598–601. [PubMed] [Google Scholar]
- 45.Mirhosseini NZ, Yusoff NA, Shahar S, Parizadeh SM, Mobarhen MG, Shakery MT. Prevalence of the metabolic syndrome and its influencing factors among adolescent girls in Mashhad, Iran. Asia Pac J Clin Nutr. 2009;18:131–6. [PubMed] [Google Scholar]
- 46.Azita F, Asghar Z, Gholam-Reza S. Relationship of body mass index with serum lipids in elementary school students. Indian J Pediatr. 2009;76:729–31. doi: 10.1007/s12098-009-0169-z. [DOI] [PubMed] [Google Scholar]
- 47.Moradi S, Azizi F. Comparison of Risk Factors for Non-communicable Diseases among Children and Adolescents in Tehran, Iran in 2000, 2003, and 2006 Tehran Lipid and Glucose Study. Iran J Endocrinol Metab. 2011;13:128–36. [Google Scholar]
- 48.Kelishadi R, Mohammadifard N, Sarrazadegan N, Nouri F, Pashmi R, Bahonar A, et al. The effects of a comprehensive community trial on cardiometabolic risk factors in adolescents: Isfahan Healthy Heart Program. ARYA Atheroscler. 2012;7:184–90. [PMC free article] [PubMed] [Google Scholar]
- 49.Mirhosseini NZ, Shahar S, Ghayour-Mobarhan M, Parizadeh MR, Yusoff NA, Shakeri MT. Body fat distribution and its association with cardiovascular risk factors in adolescent Iranian girls. Iran J Pediatr. 2012;22:197–204. [PMC free article] [PubMed] [Google Scholar]
- 50.Mehrkash M, Kelishadi R, Mohammadian S, Mousavinasab F, Qorbani M, Hashemi ME, et al. Obesity and metabolic syndrome among a representative sample of Iranian adolescents. Southeast Asian J Trop Med Public Health. 2012;43:756–63. [PubMed] [Google Scholar]
- 51.Barzin M, Hosseinpanah F, Saber H, Sarbakhsh P, Nakhoda K, Azizi F. Gender Differences Time Trends for Metabolic Syndrome and Its Components among Tehranian Children and Adolescents. Cholesterol 2012. 2012 doi: 10.1155/2012/804643. 804643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hosseini-Esfahani F, Mousavi Nasl Khameneh A, Mirmiran P, Ghanbarian A, Azizi F. Trends in risk factors for cardiovascular disease among Iranian adolescents: The Tehran Lipid and Glucose Study, 1999-2008. J Epidemiol. 2011;21:319–28. doi: 10.2188/jea.JE20100162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ramezankhani A, Mehrabi Y, Mirmiran P, Azizi F. Comparison of anthropometric and biochemical indices of adolescents born during and after the Iran-Iraq war; Tehran Lipid and Glucose Study. Arch Iran Med. 2011;14:27–31. [PubMed] [Google Scholar]
- 54.Azizi F, Farahani ZK, Ghanbarian A, Sheikholeslami F, Mirmiran P, Momenan AA, et al. Familial aggregation of the metabolic syndrome: Tehran Lipid and Glucose Study. Ann Nutr Metab. 2009;54:189–96. doi: 10.1159/000217816. [DOI] [PubMed] [Google Scholar]
- 55.Daniels SR, Greer FR. Lipid screening and cardiovascular health in childhood. Pediatrics. 2008;122:198–208. doi: 10.1542/peds.2008-1349. [DOI] [PubMed] [Google Scholar]
- 56.Esmaillzadeh A, Mirmiran P, Azadbakht L, Etemadi A, Azizi F. High prevalence of the metabolic syndrome in Iranian adolescents. Obesity (Silver Spring) 2006;14:377–82. doi: 10.1038/oby.2006.50. [DOI] [PubMed] [Google Scholar]
- 57.Sarkhail P, Hadaegh F, Azizi F, Sarkhail P. Prevalence of dyslipidemia in Iranian children and its relationship with anthropometric indices (TLGS Study) Horme Res. 2008;70:132–3. [Poster presentation] [Google Scholar]
- 58.Ramezani F, Azizi F. Prevalence of hyperlipidemia in 3-19 years old children and adolescent of Tehran in 2000. Iran J Endocrinol Metab. 2005;7:249–53. [Google Scholar]
- 59.Mehrdad SM, Hossein Panah F, Azizi F. Determine the prevalence of metabolic syndrome among children 9-3 years old in Tehran Lipid and Glucose Study. Med J (Shahid Beheshti Med Sch) 2006;30:337–46. [Google Scholar]
- 60.Kavey RE, Allada V, Daniels SR, Hayman LL, McCrindle BW, Newburger JW, et al. Cardiovascular risk reduction in high-risk pediatric patients: A scientific statement from the American Heart Association Expert Panel on Population and Prevention Science; the Councils on Cardiovascular Disease in the Young, Epidemiology and Prevention, Nutrition, Physical Activity and Metabolism, High Blood Pressure Research, Cardiovascular Nursing, and the Kidney in Heart Disease; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research: Endorsed by the American Academy of Pediatrics. Circulation. 2006;114:2710–38. doi: 10.1161/CIRCULATIONAHA.106.179568. [DOI] [PubMed] [Google Scholar]
- 61.National Cholesterol Education Program (NCEP). Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Summary of the Third Report (Adult Treatment Panel III) J Am Med Assoc. 2001;269:3015–23. [PubMed] [Google Scholar]
- 62.de Ferranti SD. Childhood cholesterol disorders: The iceberg base or nondisease? Med Clin North Am. 2012;96:141–54. doi: 10.1016/j.mcna.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 63.Centers for Disease Control and Prevention (CDC). Prevalence of abnormal lipid levels among youths — United States, 1999-2006. MMWR Morb Mortal Wkly Rep. 2010;59:29–33. [PubMed] [Google Scholar]
- 64.Ford ES, Li C, Zhao G, Mokdad AH. Concentrations of low-density lipoprotein cholesterol and total cholesterol among children and adolescents in the United States. Circulation. 2009;119:1108–15. doi: 10.1161/CIRCULATIONAHA.108.816769. [DOI] [PubMed] [Google Scholar]
- 65.Gaziano TA, Bitton A, Anand S, Abrahams-Gessel S, Murphy A. Growing epidemic of coronary heart disease in low-and middle-income countries. Curr Probl Cardiol. 2010;35:72–115. doi: 10.1016/j.cpcardiol.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Esteghamati A, Khalilzadeh O, Mohammad K, Meysamie A, Rashidi A, Kamgar M, et al. Secular trends of obesity in Iran between 1999 and 2007: National Surveys of Risk Factors of Non-communicable Diseases. Metab Syndr Relat Disord. 2010;8:209–13. doi: 10.1089/met.2009.0064. [DOI] [PubMed] [Google Scholar]
- 67.Tabatabaei-Malazy O, Qorbani M, Samavat T, Sharifi F, Larijani B, Fakhrzadeh H. Prevalence of dyslipidemia in Iran: A systematic review and meta-analysis study. Int J Prev Med. 2014;5:373–93. [PMC free article] [PubMed] [Google Scholar]
- 68.Dholpuria R, Raja S, Gupta BK, Chahar CK, Panwar RB, Gupta R, et al. Atherosclerotic risk factors in adolescents. Indian J Pediatr. 2007;74:823–6. doi: 10.1007/s12098-007-0146-3. [DOI] [PubMed] [Google Scholar]
- 69.Rerksuppaphol S, Rerksuppaphol L. Prevalence of dyslipidemia in Thai schoolchildren. J Med Assoc Thai. 2011;94:710–5. [PubMed] [Google Scholar]
- 70.Kant AK, Graubard BI. Race-ethnic, family income, and education differentials in nutritional and lipid biomarkers in US children and adolescents: NHANES 2003-2006. Am J Clin Nutr. 2012;96:601–12. doi: 10.3945/ajcn.112.035535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Goff DC, Jr, Bertoni AG, Kramer H, Bonds D, Blumenthal RS, Tsai MY, et al. Dyslipidemia prevalence, treatment, and control in the Multi-Ethnic Study of Atherosclerosis (MESA): Gender, ethnicity, and coronary artery calcium. Circulation. 2006;113:647–56. doi: 10.1161/CIRCULATIONAHA.105.552737. [DOI] [PubMed] [Google Scholar]
- 72.Frank AT, Zhao B, Jose PO, Azar KM, Fortmann SP, Palaniappan LP. Racial/ethnic differences in dyslipidemia patterns. Circulation. 2014;129:570–9. doi: 10.1161/CIRCULATIONAHA.113.005757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kelishadi R, Schwandt P, Haas GM. Reference curves of anthropometric indices and serum lipid profile les in representative samples of Asian and European children. Arch Med Sci. 2008;4:329–35. [Google Scholar]
- 74.de Alcântara Neto OD, Silva Rde C, Assis AM, Pinto Ede J. Factors associated with dyslipidemia in children and adolescents enrolled in public schools of Salvador, Bahia. Rev Bras Epidemiol. 2012;15:335–45. doi: 10.1590/s1415-790x2012000200011. [DOI] [PubMed] [Google Scholar]
- 75.Misra A, Shrivastava U. Obesity and dyslipidemia in South Asians. Nutrients. 2013;5:2708–33. doi: 10.3390/nu5072708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ochoa-Avilés A, Andrade S, Huynh T, Verstraeten R, Lachat C, Rojas R, et al. Prevalence and socioeconomic differences of risk factors of cardiovascular disease in Ecuadorian adolescents. Pediatr Obes. 2012;7:274–83. doi: 10.1111/j.2047-6310.2012.00061.x. [DOI] [PubMed] [Google Scholar]
- 77.Okada T, Murata M, Yamauchi K, Harada K. New criteria of normal serum lipid levels in Japanese children: The nationwide study. Pediatr Int. 2002;44:596–601. doi: 10.1046/j.1442-200x.2002.01634.x. [DOI] [PubMed] [Google Scholar]
- 78.Uçar B, Kiliç Z, Dinleyici EC, Colak O, Günes E. Serum lipid profiles including non-high density lipoprotein cholesterol levels in Turkish school-children. Anadolu Kardiyol Derg. 2007;7:415–20. [PubMed] [Google Scholar]
- 79.Naghavi M, Abolhassani F, Pourmalek F, Lakeh M, Jafari N, Vaseghi S, et al. The burden of disease and injury in Iran 2003. Popul Health Metr. 2009:7–9. doi: 10.1186/1478-7954-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Esteghamati A, Meysamie A, Khalilzadeh O, Rashidi A, Haghazali M, Asgari F, et al. Third national Surveillance of Risk Factors of Non-Communicable Diseases (SuRFNCD-2007) in Iran: Methods and results on prevalence of diabetes, hypertension, obesity, central obesity, and dyslipidemia. BMC Public Health. 2009:9–167. doi: 10.1186/1471-2458-9-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Asgari F, Aghajani H, Haghazali M, Heidarian H. Non-communicable diseases risk factors surveillance in Iran. Iran J Public Health. 2009;38(Suppl 1):119–22. [Google Scholar]
- 82.Kelishadi R, Ardalan G, Qorbani M, Ataie-Jafari A, Bahreynian M, Taslimi M, et al. Methodology and Early Findings of the Fourth Survey of Childhood and Adolescence Surveillance and Prevention of Adult Non-Communicable Disease in Iran: The CASPIAN-IV Study. Int J Prev Med. 2013;4:1451–60. [PMC free article] [PubMed] [Google Scholar]
- 83.Kasaeian A, Eshraghian MR, Rahimi Foroushani A, Niakan Kalhori SR, Mohammad K, Farzadfar F. Bayesian autoregressive multilevel modeling of burden of diseases, injuries and risk factors in Iran 1990-2013. Arch Iran Med. 2014;17:22–7. [PubMed] [Google Scholar]
- 84.Parsaeian M, Farzadfar F, Zeraati H, Mahmoudi M, Rahimighazikalayeh G, Navidi I, et al. Application of spatio-temporal model to estimate burden of diseases, injuries and risk factors in Iran 1990-2013. Arch Iran Med. 2014;17:28–33. [PubMed] [Google Scholar]
- 85.Kelishadi R, Ardalan G, Adeli K, Motaghian M, Majdzadeh R, Mahmood-Arabi MS, et al. Factor analysis of cardiovascular risk clustering in pediatric metabolic syndrome: CASPIAN study. Ann Nutr Metab. 2007;51:208–15. doi: 10.1159/000104139. [DOI] [PubMed] [Google Scholar]


