This study ascertains the levels of educational attainment among state health agency employees as well as the correlates of attainment.
Keywords: educational attainment, governmental public health, public health education, Public Health Workforce Interests and Needs Survey (PH WINS), public health workforce, workforce development
Context:
Educational attainment is a critical issue in public health workforce development. However, relatively little is known about the actual attainment of staff in state health agencies (SHAs).
Objective:
Ascertain the levels of educational attainment among SHA employees, as well as the correlates of attainment.
Design:
Using a stratified sampling approaching, staff from SHAs were surveyed using the Public Health Workforce Interests and Needs Survey (PH WINS) instrument in late 2014. A nationally representative sample was drawn across 5 geographic (paired adjacent HHS) regions. Descriptive and inferential statistics were analyzed using balanced repeated replication weights to account for complex sampling. A logistic regression was conducted with attainment of a bachelor's degree as the dependent variable and age, region, supervisory status, race/ethnicity, gender, and staff type as independent variables.
Setting and Participants:
Web-based survey of SHA central office employees.
Main Outcome Measure:
Educational attainment overall, as well as receipt of a degree with a major in public health.
Results:
A total of 10 246 permanently-employed SHA central office staff participated in the survey (response rate 46%). Seventy-five percent (95% confidence interval [CI], 74-77) had a bachelor's degree, 38% (95% CI, 37-40) had a master's degree, and 9% (95% CI, 8%-10%) had a doctoral degree. A logistic regression showed Asian staff had the highest odds of having a bachelor's degree (odds ratio [OR] = 2.8; 95% CI, 2.2-3.7) compared with non-Hispanic whites, and Hispanic/Latino staff had lower odds (OR = 0.6; 95% CI, 0.4-0.8). Women had lower odds of having a bachelor's degree than men (OR = 0.5; 95% CI, 0.4-0.6). About 17% of the workforce (95% CI, 16-18) had a degree in public health at any level.
Conclusions:
Educational attainment among SHA central office staff is high, but relatively few have formal training of any sort in public health. This makes efforts to increase availability of on-the-job training and distance learning all the more critical.
Who are public health professionals? No single degree or certification characterizes this group.
Committee on Educating Public Health Professionals for the 21st Century (2002)1
The definition of public health has been debated for the better part of the last century,2–6 inhibiting efforts to standardize the education of public health practitioners.1,7–16 Focus on definitional issues has obscured the reality that most individuals who work in governmental public health agencies have no formal training in the field.1,17 However, to date, there have not been credible, nationally representative data that document either the scope of this issue or the workforce and its education more broadly.
More than a decade ago, the Institute of Medicine (recently renamed the National Academy of Medicine, or NAM) Committee on Educating Public Health Professionals for the 21st Century made several noteworthy recommendations regarding training the public health workforce of the future, including the definition of a public health professional—“a person educated in public health or a related discipline who is employed to improve health through a population focus. Nearly all public health professionals encompassed by this definition would have earned at least a baccalaureate degree.” Taken together with the observation that a “small portion” of the workforce receives formal training in public health, the NAM recommended schools and programs of public health focus on training future senior leaders of governmental public health, as opposed to training students to every potential level or position within a health department.1 Another challenge has arisen in the past 30 years: in addition to a potentially (but unknown) small proportion of the governmental public health workforce being trained in public health, relatively few graduates of schools and programs in public health end up in careers in governmental public health. Alumni surveys conducted in the 1970s and 1980s showed that fewer than 20% of alumni were employed in governmental public health, and data suggest that the proportion may be lower today.18–22
A lack of formal education in public health has necessitated a focus on in-place training and, more recently, distance learning. Substantial work has been done to identify core competencies for the various disciplines that constitute the public health workforce,23–39 including, most notably, the development of the Council of Linkage's Core Competencies model that specifies the competencies across position type and supervisory status/seniority of position.14 From a workforce development perspective, comprehensive approaches are key to identifying the universe of potential needs and opportunities for training in public health. Yet, this comprehensive focus makes it difficult to prioritize the “most important” needs. Previously, state- or regionally oriented Public Health Training Centers (PHTCs) routinely conducted assessments of the training needs of public health practitioners. However, these disparate and varied assessments could not be combined into a national assessment of training needs due to different instruments being utilized and populations surveyed across the PHTCs.26
A challenging confluence exists in public health workforce development. On the one hand, region-, profession-, and silo-specific training requirements fracture national workforce development efforts. On the other hand, a lack of systems-wide assessment of priorities within postgraduate/on-the-job training makes picking the most important trainings for the field extremely difficult. These challenges remain profound more than a decade after the NAM's 2002 report.1 In part to address these concerns, and in part to quantify other important needs and perceptions of the public health workforce, the Public Health Workforce Interests and Needs Survey (PH WINS) was conducted in fall of 2014. PH WINS also allows for the first-ever characterization of educational attainment by degree and major/concentration for the public health workforce.
This article has 3 primary aims. First, we use PH WINS data to explore the educational attainment by degree level (bachelor's, master's, and doctoral), generally, of the state governmental public health workforce. We focus especially on the attainment of bachelor's degrees due to the NAM's recognition and expectation that participants in the public health workforce should have a bachelor's degree. Second, we use PH WINS data to explore the extent to which public health professionals have formal training in public health. Finally, we discuss the implications of our findings for public health workforce development, including the importance of on-the-job and distance training for public health practitioners.
Methods
This article characterizes educational attainment of the public health workforce, including the proportion of the workforce with various types of public health degrees. It does so through the use of PH WINS. Detailed methods for the development and fielding of PH WINS are written about extensively elsewhere.40 In brief, PH WINS assessed the interests, needs, and perceptions of the public health workforce and complements organizationally oriented studies fielded by the Association of State and Territorial Health Officials and the National Association of County & City Health Officials. Development of PH WINS began in 2013 after a summit of leadership from more than 30 disciplines in public health identified crosscutting training needs for the workforce.26,40 A technical expert panel was convened to draft a sampling approach, create an instrument, and plan for the survey's fielding. This project received a determination of “exempt” from the Chesapeake Institutional Review Board (Pro00009674).
The instrument drew largely on previously used items from workforce development surveys from public health and elsewhere,40 including the Centers for Disease Control and Prevention Technical Assistance and Service Improvement Initiative: Project Officer Survey; the 2009 Epidemiology Capacity Assessment; the United States Office of Personnel Management Annual Survey/Federal Employee Viewpoint Survey; the Public Health Foundation Worker Survey; the Bowling Green State University Job in General Scale; and the University of Michigan Public Health Workforce Schema.40 The instrument underwent cognitive interviewing with public health practitioners, and the instrument was pretested with 3 groups of staff in state health agencies and local health departments (LHDs). The instrument was fully fielded across 3 sample frames in fall 2014. The frames included a state health agency frame, a Big Cities Health Coalition frame,41 and a pilot of LHDs. From the first frame, we constructed a nationally representative sample of central office staff employed in a permanent capacity by the health department (ie, not temporary staff), and stratified by 5 geographic regions (paired, contiguous HHS regions). We constructed appropriate weights using balanced repeated replication to account for complex sampling, any differential nonresponse by the 5 regions, and demographic characteristics.
PH WINS addressed 4 major areas of inquiry: training needs, workplace environment and job satisfaction, perceptions about national trends, and demographics.42 This article focuses on the educational attainment of the public health workforce and the correlates of that attainment. PH WINS obtained data on degrees obtained, as well as data from an open-ended question about the relevant type/major/concentration for each degree attained. Approximately 15 000 text answers were categorized into 37 majors and topical areas within different types of associate's, bachelor's, master's, and doctoral degrees. Descriptive analyses were performed. Inferential analyses included pairwise comparisons using the Tukey test for multiple comparisons and the Pearson χ2 test, as appropriate. Logistic regression was performed, with attainment of at least a bachelor's degree as the dependent variable. Selection of independent variables was based on theoretical importance from a literature review; the final model included age, geographic region, supervisory status,* race/ethnicity, gender, and staff type.† Akaike information criterion was also used in model selection. For comparison to the weighted central office staff analysis, we also ran one similar model using unweighted responses from all 3 frames, adding in worker setting (SHA central office vs local or regional health department).
Results
Across all SHA employees at central, regional, or local offices, a total of approximately 40 000 were selected for participation in PH WINS. Of those, 19 171 responded (a 48% response rate). Among central office employees of SHAs, after accounting for undeliverable e-mails and individuals who confirmed they had left their position, the response rate was 46% (n = 10 246). The identified population of interest was 41 617 SHA central office employees in the United States, in line with previously published the Association of State and Territorial Health Officials' estimates.43 Overall, about a quarter of the central office public health workforce in the United States participated in PH WINS. Demographics of the workforce are explored in depth elsewhere in this supplement.42 Women constituted the majority of the workforce at 72% (95% confidence interval [CI], 70.5-73.4). The majority of employees did not hold a supervisory role (66.9%; 95% CI, 65.5-68.4), were non-Hispanic white (70.0%; 95% CI, 68.8-71.1), and had at least a bachelor's degree (75.5%; 95% CI, 74.2-76.7). The average age was 48.3 years (95% CI, 48.0-48.6). Staff had worked in their position for 6.4 years on average (6.2-6.6), in their current agency for 11.2 years on average (11.0-11.4), and 14.0 years in public health on average (13.7-14.3). Those in management positions had been in management for 11.3 years on average (10.8-11.8).
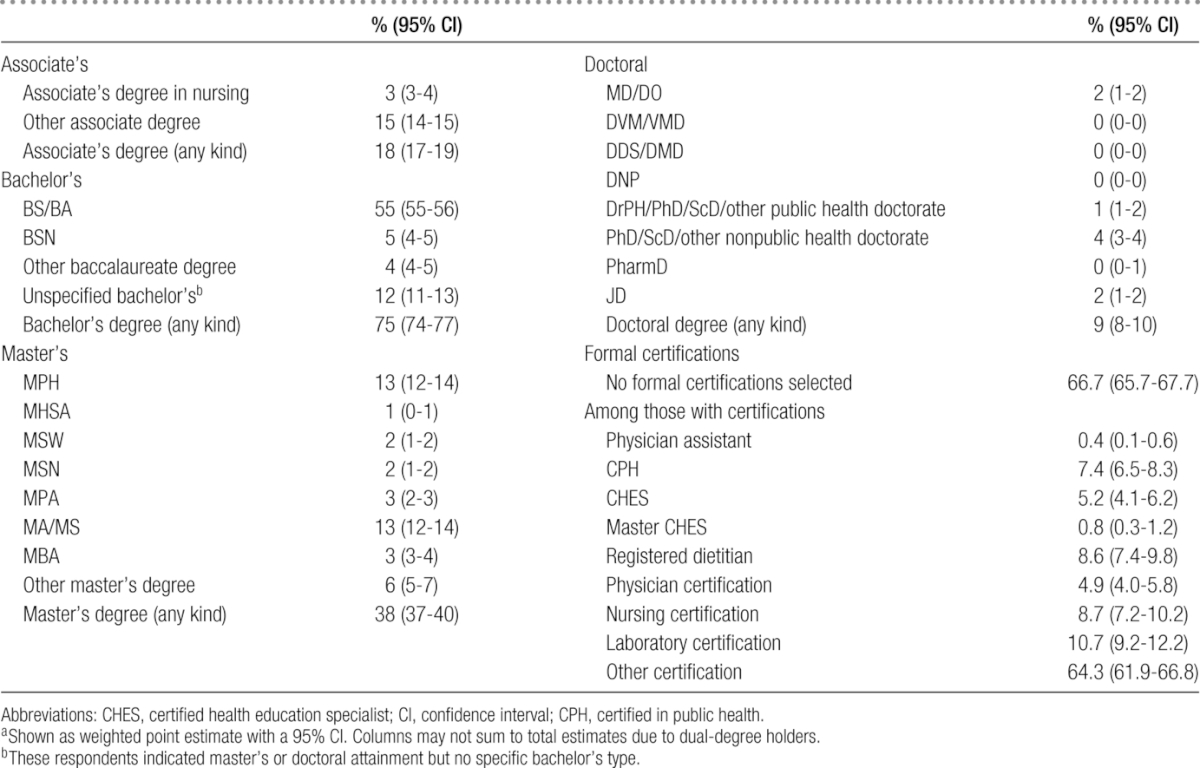
As Table 1 shows, while the majority of the workforce had a bachelor's degree, a smaller percentage held a master's degree of any type (38.3%; 95% CI, 36.6-40.0), and even fewer held a doctoral degree (PhD/DrPH or similar, MD/DO, JD, etc) (9.3%; 95% CI, 8.3-10.3). In addition, a fairly small proportion had an associate's degree of any type (17.9%; 95% CI, 17.1-18.6). A relatively small proportion of the workforce had formal degrees in public health, including 2% (95% CI, 1.8-2.6) with a bachelor's in public health, 13% with a MPH (95% CI, 12-14), and a doctoral degree in public health (1% of staff; 95% CI, 1-2). Another form of education attainment measured in PH WINS was certification. Receipt of a certification was indicated by 33% of respondents (95% CI, 32-34). Among those who indicated they had a certification, about 10.7% had a laboratory certification (95% CI, 9.2-12.2), 8.7% had a nursing certification (95% CI, 9.2-12.2), 8.6% were registered dietitians (95% CI, 7.4-9.8), 7.4% were certified in public health (95% CI, 6.5-8.3), 5.2% were certified health education specialists (95% CI, 4.1-6.2), 4.9% had a physician certification (95% CI, 4.0-5.8), and 64% had some other certification (95% CI, 61.9-66.8).
TABLE 1 •. Educational Attainment of the State Health Agency Central Office Workforcea.
As shown in Table 2, the majority of SHA central office employees had at least a bachelor's degree across most major demographic variables. Each ascending level of supervisory status saw higher proportions of that group with bachelor's degrees, with nonsupervisor being the lowest (68.1% with a bachelor's; 95% CI, 66.3-70) and executive being the highest (94.2%; 95% CI, 91.7-96.8). No differences among regions were statistically significant. A smaller proportion of women had a bachelor's degree compared to men (P < .001), and a higher proportion of those under the mean age of the workforce, 48 years, had a bachelor's (80.5%; 95% CI, 79.5-81.4) than those 48 years and older (71.6% had a bachelor's; 95% CI, 69.3-73.8). Asian staff were the racial/ethnic group with highest educational attainment on average, including the group with the largest proportion holding a bachelor's degree at 88.0% overall (95% CI, 85.2-90.7). A statistically significantly smaller proportion of Hispanic staff and Native Hawaiian/Other Pacific Islander staff had a bachelor's degree than Asian staff and non-Hispanic white staff. There were not statistically significant differences between black/African American staff and non-Hispanic white staff.
TABLE 2 •. Proportion of Staff With Bachelor's Degrees.
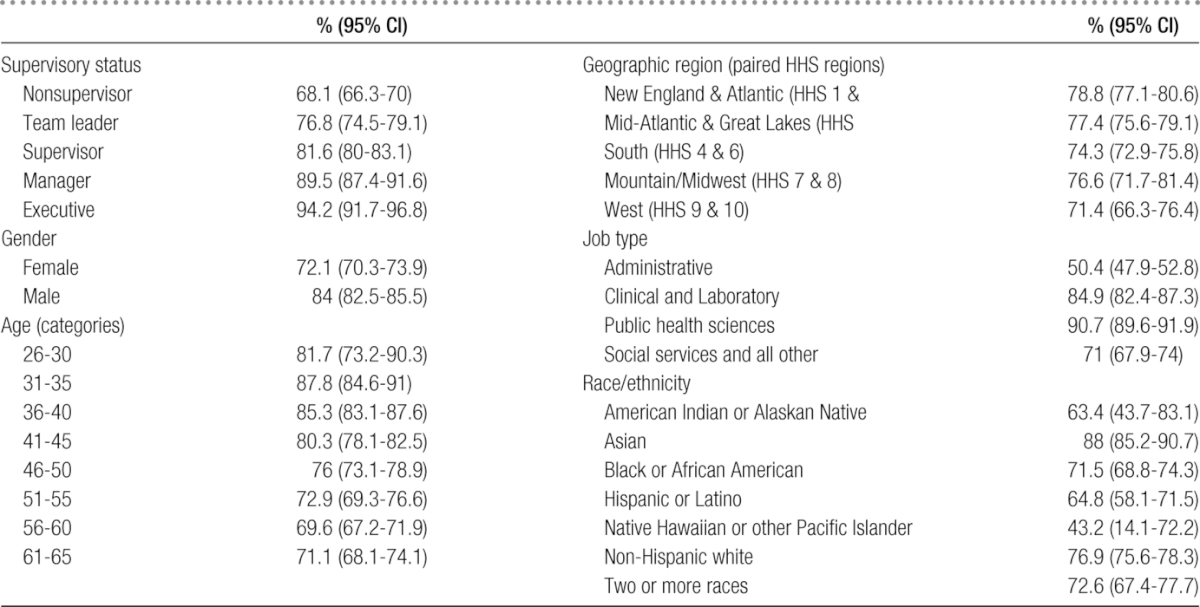
Findings were similar in examining educational attainment at the master's and doctoral levels (data not shown). Just over 31% of nonsupervisors had a master's degree (95% CI, 28.6-33.4) and 5.3% (95% CI, 4.6-6.1) had a doctoral degree, compared with 58.4% (95% CI, 50.8-66.0) of executives attaining a master's degree and 31% (95% CI, 27.0-35.0) attaining a doctoral degree of some type. Overall, approximately 37.6% (95% CI, 36-39.2) of men and 38.8% (95% CI, 36.3-41.2) of women had master's degrees. Approximately 13.5% of men (95% CI, 11.3-15.7) had a doctoral degree, and 7.6% (95% CI, 6.6-8.5) of women had doctoral degrees. Black/African American staff, Asian staff, and non-Hispanic white staff had similar proportions with master's degrees in the high 30% to mid-40% range. Approximately 30% (95% CI, 25.1-34.8) of Hispanic staff had a master's degree, a statistically significant difference from the groups mentioned earlier. More than 20.8% of Asian staff (95% CI, 17.0-24.7) had a doctoral degree, significantly higher than non-Hispanic white staff (9.2%; 95% CI, 8.0-10.4), black/African American staff (6.7%; 95% CI, 4.1-9.2), and Hispanic staff (7.1%; 95% CI, 5.5-8.6). Regional differences were not statistically significant for master's degree attainment overall. At the doctoral level, HHS regions 1 & 2 (the Northeast) had the highest proportion of staff with a doctoral degree (11.9%; 95% CI, 10.4-13.4), with HHS regions 3 & 5 (Mid-Atlantic and Great Lakes) and 4 & 6 (the South) having just over 8% of staff with doctoral degrees, HHS regions 7 & 8 (Mountain/Midwest) having just under 7% of staff with doctoral degrees. HHS regions 9 & 10 (the West) had a point estimate of 10.4% of staff with doctoral degrees, but a wide-ranging CI on that estimate (95% CI, 5.5-15.3). Approximately 90% of staff in the public health sciences had a bachelor's degree (95% CI, 89.6-91.9) compared with half of administrative staff (95% CI, 47.9-52.8; P < .001).
Regression results
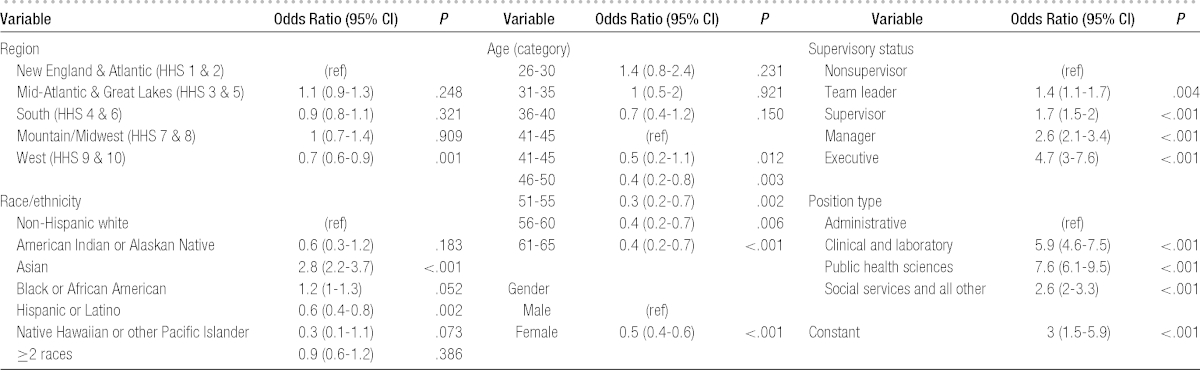
To ascertain the meaningfulness of differences in educational attainment illustrated in Table 2 and reported earlier, we ran a logistic regression with bachelor's degree attainment as the dependent variable and demographic variables as the independent variables (Table 3). After accounting for other covariates of interest, the model suggests regional differences are not statistically significantly different, with the exception of HHS regions 9 & 10; odds of a staff holding a bachelor's degree in that region are 30% lower than in HHS regions 1 & 2 (P = .008). Differences in attainment due to supervisory status are substantial, with executives having the highest odds of holding a bachelor's degree (OR = 4.7; 95% CI, 3.0-7.6). Holding all else constant, women had lower odds of attaining a bachelor's degree than men (P < .001). Compared with non-Hispanic white staff, Asian staff had 180% higher odds of having a bachelor's degree (P < .001). Hispanic staff had lower odds than non-Hispanic white staff (P = .002), holding all else constant. Compared with individuals in administrative positions, those in clinical or laboratory positions had higher odds of having a bachelor's degree (OR = 5.9; 95% CI, 4.6-7.5), as did those who held a public health science position (OR = 7.6; 95% CI, 6.1-9.5). Staff younger than 40 years had significantly higher odds of having a bachelor's degree than those older than 40 years.
TABLE 3 •. Results of Logistic Regression on the Correlates of Bachelor's Degree Attainment.
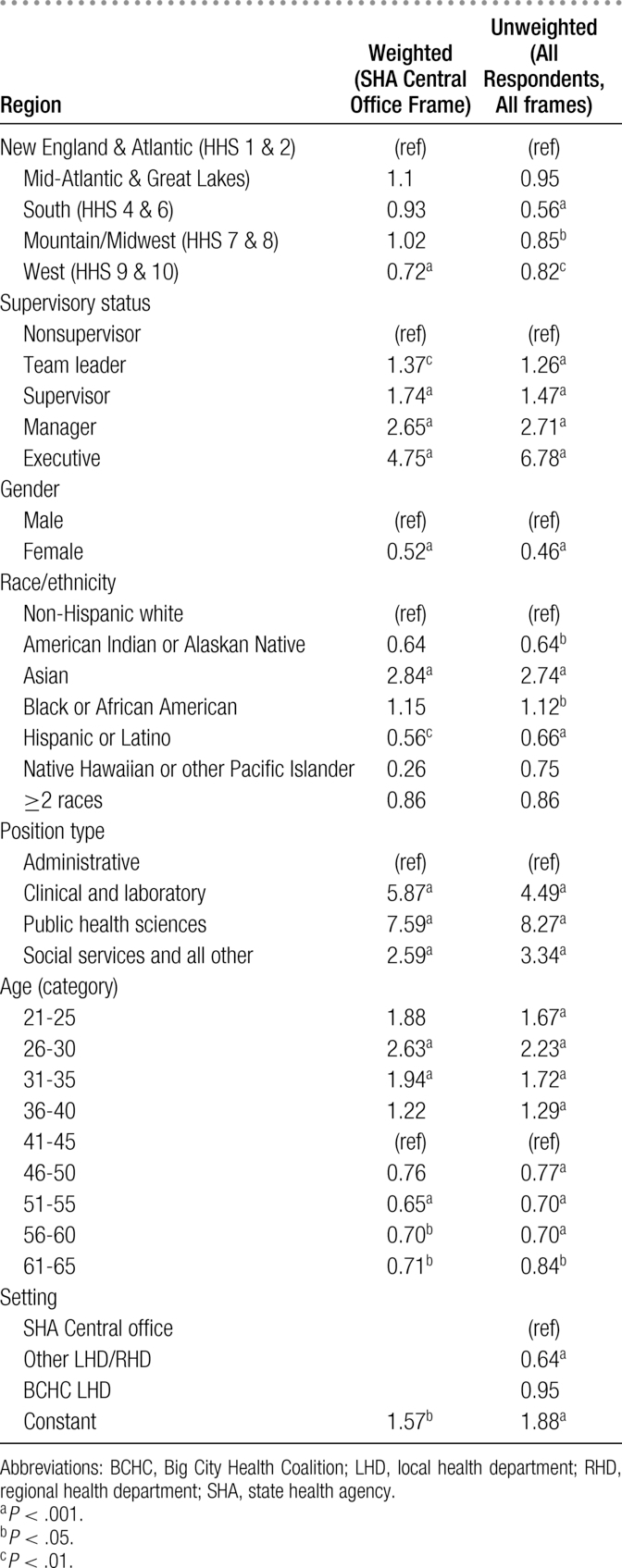
Beyond the analysis of the central state health department workforce, a similar model was run using unweighted data from all sampling frames within PH WINS for comparison. This model includes an indicator to delineate whether the staff work in the SHA central office, a Big City Health Coalition health department, or in another local or regional health department. This model showed staff in Big City Health Coalition departments had similar attainment to state employees, and staff in other LHDs/RHDs had significantly lower odds of having a bachelor's degree, all else equal (OR = 0.64; 95% CI, 0.59-0.69). The effect sizes of other independent variables were similar; Appendix Table 1 shows comparisons of these models.
Educational attainment by degree area
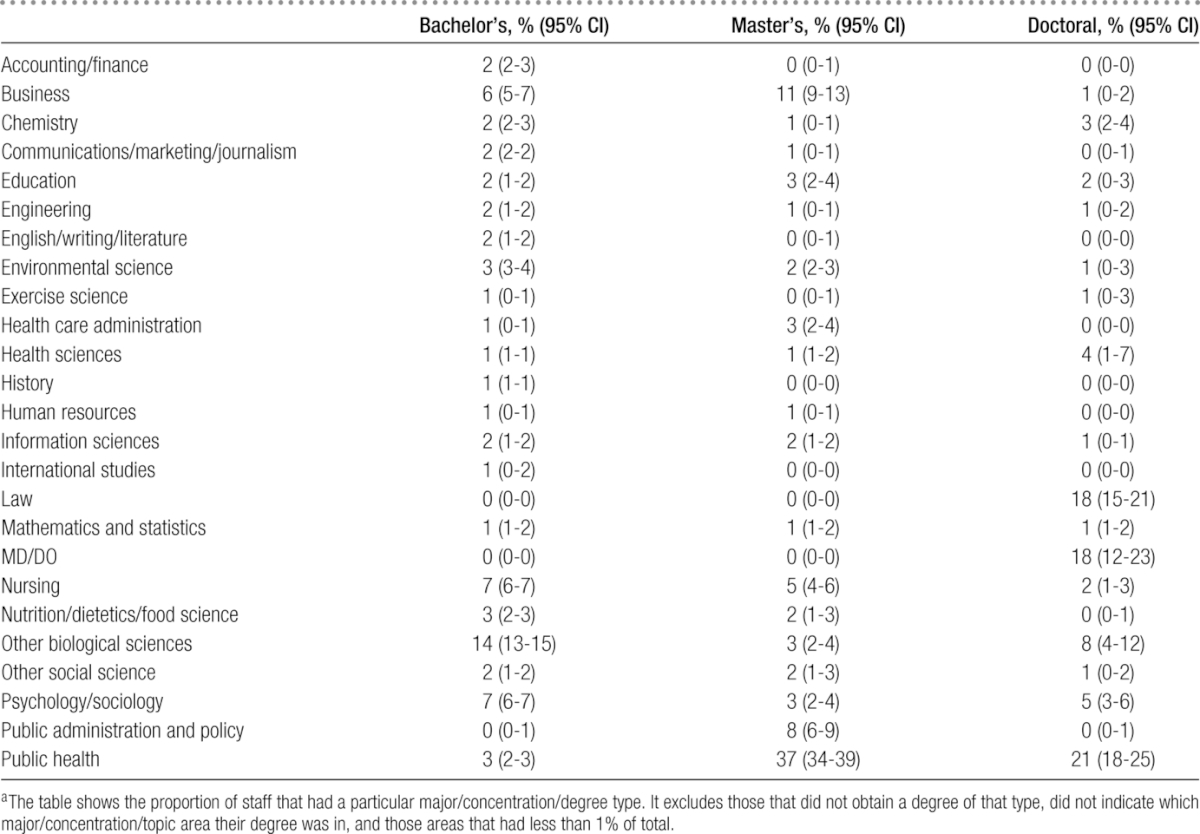
After indicating what types of degrees they had attained, respondents to PH WINS were also asked to indicate the major/concentration/topic area within that degree. Approximately 15 000 open-ended responses were categorized into 37 majors/concentrations/topic areas across bachelor's, master's, and doctoral degrees, one of which was public health. The results are shown in Table 4. Among bachelor's degree recipients indicating their major, business, nursing, biological sciences, and psychology/sociology were the most commonly reported areas. Among master's recipients indicating a degree type, public health was the most common area: 38% had some sort of master's degree in public health (95% CI, 36-40), almost exclusively through the master's in public health (MPH) degree. Overall, 12.8% of the workforce reported attaining an MPH (95% CI, 11.7-13.8). Among those with master's degrees who indicated their degree type, 11% reported having a business degree of some sort (most typically an MBA). Among doctoral degree recipients, public health, law, and MD/DO degrees were the most common.
TABLE 4 •. Majors and Concentrations by Degree Level Among Recipientsa.
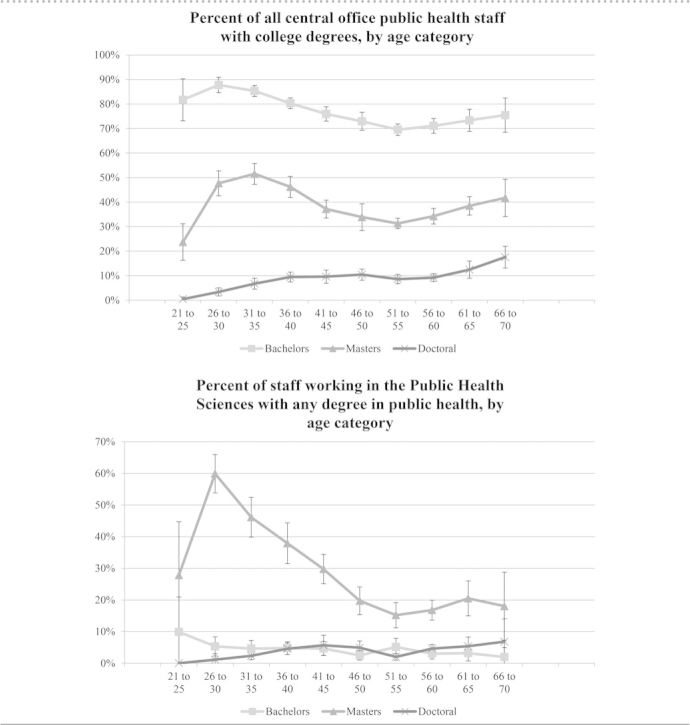
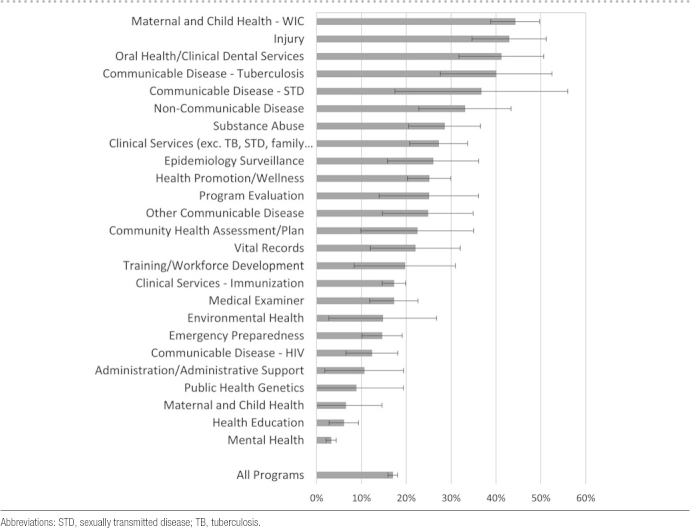
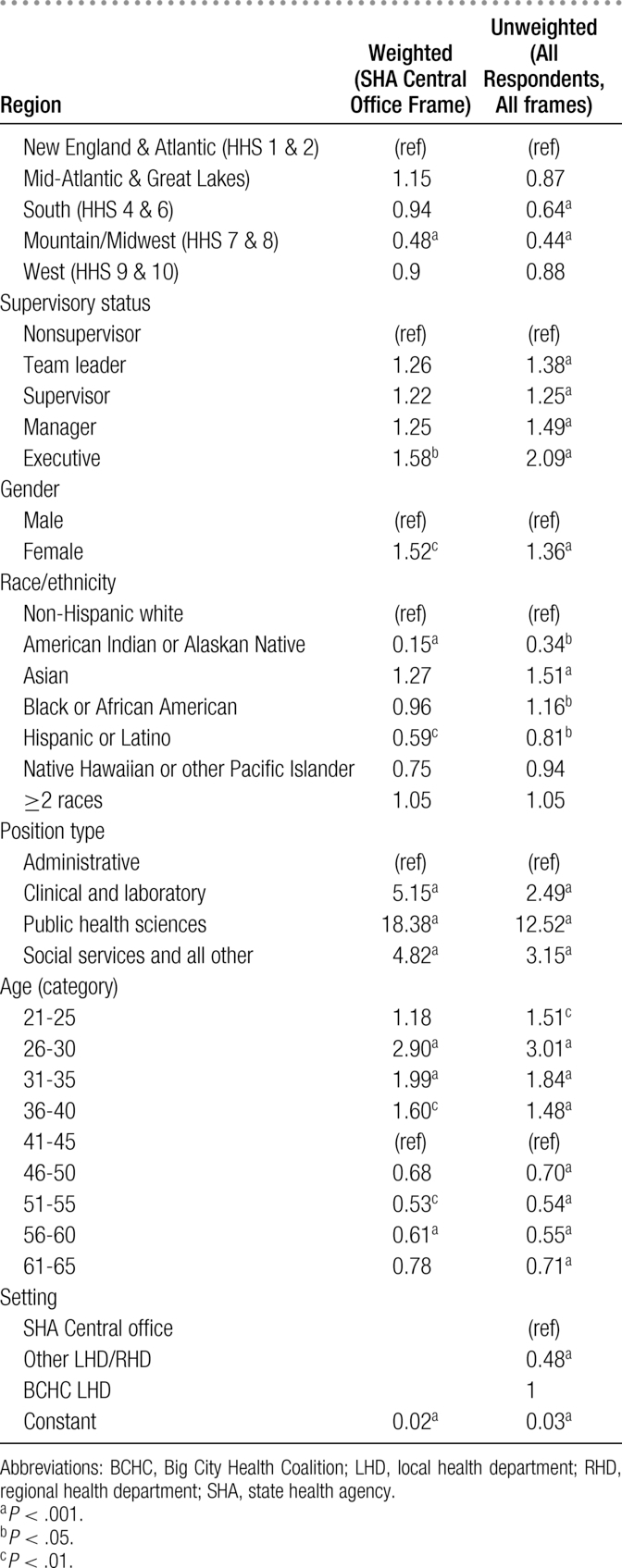
Overall, a relatively small proportion of the workforce had a degree in public health at any level—17.0% (95% CI, 15.9-18.0). This varied considerably by demographic characteristics such as age (Figure 1) and position type (Figure 2). Among all administrative staff, about 2.3% (95% CI, 1.5-3.0) have a degree in public health at any level. About 11.5% of clinical and laboratory staff (95% CI, 8-14), 31.4% of public health sciences staff (95% CI, 30-33), and 10.6% of Social Services and All Other Staff (95% CI, 9.1-12.1) have a public health degree of some type. Replicating the logistic regression and substituting attainment of any public health degree as the dependent variable showed some variation regionally (see Appendix Table 2). Only one category of supervisory status was more likely to have a public health degree of any type (executive, P = .015) than the reference category (nonsupervisor). Women had higher odds of having a public health degree of any type than men (OR = 1.5; 95% CI, 1.15-1.99). Compared with non-Hispanic white staff, Hispanic/Latino staff and American Indian/Alaskan Native staff were less likely to have a public health degree of any type (P < .001 for each, respectively). No other statistically significant differences across racial/ethnic groups were observed. Compared with staff in administrative positions, those in the public health sciences were much more likely to have a public health degree (OR = 18.4; 95% CI, 13.3-25.3). Staff younger than 40 years had higher odds of having a public health degree than those older than 40 years. Among central office employees of SHAs, epidemiology, communicable disease, noncommunicable disease, injury, and oral health were the program areas that had the highest proportion of staff reporting a public health degree at any level (Figure 2). However, no area saw a majority of its workers with a degree at any level in public health.
FIGURE 1 •.
Percentage of Public Health Workers With Any College Degree (Top) and With a Public Health Degree (Bottom), by Degree Type and Respondent Age (Category)
FIGURE 2 •.
Proportion of Public Health Staff With a Degree in Public Health (Any Level), by Program Type.
Discussion
Highlights from the PH WINS study
PH WINS confirms that the vast majority of employees in governmental public health departments do not have formal training in public health, although most do have college degrees at higher levels than other areas of government.44 Even among the staff within the public health sciences, less than half the workers reported a public health degree at any level. Bachelor's degrees in public health appear to be growing among the youngest populations of staff, although data are limited because of the rapid evolution of these programs. This may be associated with greater availability of the degree.45 While doctoral degrees in public health were somewhat uncommon in the governmental public health workforce, a master's degree in public health of some type—most typically an MPH—was the most common of all master's degrees.
This study also shows significant differences in educational attainment by age, race, and gender, after accounting for supervisory status, region, and position type. In the youngest employees (younger than 35 years), more than a quarter of the workforce reported attaining an MPH. Differences in attainment by age are largely in line with other fields and disciplines.46 More than a decade ago, the NAM observed that MPHs and related master's degrees have been and should continue to be the standard entry degree in public health. PH WINS data bear out that MPHs are the most common degree but are not a “standard” in that the majority of the workforce does not have one, even among those working within the public health sciences. Fewer than 1 in 8 staff older than the average age (48 years) have an MPH or any other public health–oriented degree. Gender differences in educational attainment have particularly important implications, given the higher proportion of women than men in the governmental public health workforce. The causes of these differences may be difficult to assess, as both genders have significantly higher educational attainment than the general population (of approximately 18%-20%).47 However, in the general population, women 25 to 50 years old have higher attainment of bachelor's and master's degree than men of the same age group. Differences in race/ethnicity are also not easily explained. Relative levels of educational attainment largely mirror those of the general population.47 However, the actual proportion of non-Hispanic white staff in public health is higher than in the general population. Unlike other demographic characteristics where disparities appear largely to exist by age, approximately the same percentage is white in the 21-25 and 25-30 age groups as the average. This may have important implications, given reports from the Association of Schools and Programs of Public Health and others that the racial and ethnic composition of public health students in nigher education is considerably more diverse than higher education overall.45,48,49
As Figure 1 highlights, only 1 age group (26-30) had a majority of staff working within the public health sciences with any type of degree in public health. More generally, the figure shows a striking difference by age, where younger staff have more formal training in public health, on average, than their older counterparts. Further research is warranted to determine whether this represents a trend, or if there are unique factors (ie, job competition during the recession) that make this cohort better educated than others.
This work also raises another important conceptual consideration. The NAM called for the “public health workforce” to have a minimum of a bachelor's degree, and to aspire to an increasingly professional/educated workforce performing public health functions. However, many working in government agencies perform essential and supportive functions that might not be defined within the “public health” field; for example, budget and procurement, executive assistants, security guards, maintenance, and other support and administrative functions that might also be performed in other government agencies with different subject matter focus. To address this, in reporting our results, we work to distinguish these roles between functional areas and job classifications—for example, administrative versus public health sciences versus clinical and laboratory versus social services and “all other.” Looking at these functional areas separately clarifies that the education and training levels of those with direct public health functions exceed the overall average for those working in public health agencies, but that a majority still do not have formal education in public health.
Going forward, to more accurately characterize the nature of the workforce and to target training, it may be important for researchers to consider ways to more regularly classify and report the “public health workforce” by the nature of their work, rather than solely by their employment in a public health agency. This would allow more precise measurement of the education of those performing public health functions (the focus of the NAM recommendations), reduce complications that arise from interstate differences in how support functions are managed (eg, contracted or centralized in support agencies), and more narrowly define training needs of the workforce.
PH WINS confirms a long-held belief that formal education in public health is uncommon among governmental public health workers. Actual levels of formal public health training should be cause for concern for 2 reasons. First, any differences that exist in the availability of on-the-job training in public health,1 coupled with low levels of formal public health training, are likely promoting wide disparities between and among health departments in capacity and capability to conduct the work of the public health enterprise. Second, despite managers and executives having a degree in public health relatively more frequently than other position types, fewer than 1 in 4 have formal training in public health. As a result, it remains unclear if schools and programs of public health are meeting their stated goal of training today's public health leaders, or those of the future; although younger staff have higher levels of training, only a minority workers younger than 40 years have formal training in public health. We concur with the NAM's findings that the field of public health has many disciplines, and so many different types of formal education may be appropriate. However, the lack of formal public health training, even among positions within the public health sciences, may suggest a redoubling of efforts is needed in making available high-quality, affordable executive master's and doctoral degrees for mid-career public health practitioners. More broadly, a relatively low proportion of workers formally trained in public health—even among management—heighten the need for additional postgraduate and on-the-job training.
Limitations
This project has several limitations worth noting. Data in this project were weighted to create a nationally representative sample. While use of nonresponse adjustment and poststratification incorporated into the balanced repeated replication method of weighting allows for robust estimators, there remains some risk that differential nonresponse may exist. That is, that those who elected not to respond to the survey may be different from those who did. Differential nonresponse was not observed by state, or region. Furthermore, we believe that threats to validity due to nonresponse bias are attenuated because of an acceptable response rate of 46%, which exceeded the project's original goal of 35%; because respondents had similar demographic characteristics to reported totals by state; and because of extensive poststratification and representative weighting efforts. PH WINS is a cross-sectional survey of the workforce in late 2014. While it is appropriate to make comparisons between, for example, different estimates by age group, it would not be appropriate to characterize our findings as “trends”; repeat studies would be needed to identify trends over time. A final limitation is that the open-text categorization of educational degree majors/concentrations may have introduced error into those estimates, since researchers had to make choices about how to code those responses. The wide variety of major types (almost 40) and extensive checking and reexamination of open-text responses partially addresses this concern.
Conclusions
The public health workforce of the early 21st century has relatively high levels of overall educational attainment. Data from the first-ever nationwide individual-level survey of the public health workforce suggest that younger staff in health departments are attaining higher levels of education and more commonly in public health. However, even among younger staff, only a minority hold a degree in public health at any level. A lack of formal education in public health continues to demonstrate a need for on-the-job training and distance learning options for the public health workforce.
APPENDIX TABLE 1 •. Comparison of Bachelor's Attainment Logistic Models (Weighted and Unweighted).
APPENDIX TABLE 2 •. Educational Attainment of a Public Health Degree (Any Level).
Nonsupervisors were defined as those who did not supervise other employees, as well as team leaders (provide employees with day-to-day guidance in work projects but do not have official supervisory responsibility or conduct performance appraisals). Supervisory positions include supervisors (provide employees' performance appraisals and approval of their leave but do not supervise other supervisors), managers (supervise ≥1 supervisors), and executive (member of senior executive service or equivalent).40
These items were collapsed from a list of job classifications respondents were asked to select as best representative of their position. This includes Administration & Business Support—Accountant/Fiscal, Clerical Personnel (Administrative Assistant, Secretary), Custodian, Grant and Contracts Specialist, Health Officer, Human Resources Personnel, Information Technology Specialist, Other Facilities/Operations worker, Public Health Agency Director, Public Information Specialist; Clinical and Laboratory & Behavioral Health Professional, Community Health Worker, Home Health Worker, Laboratory Aide/Assistant, Laboratory Developmental Scientist, Laboratory Scientist (Manager, Supervisor), Laboratory Scientist/Medical Technologist, Laboratory Technician, Licensed Practical/Vocational Nurse, Medical Examiner, Nutritionist, Other Oral Health Professional, Other Physician, Other Registered Nurse—Clinical Services, Other Veterinarian, Physician Assistant, Public Health Dentist, Public Health/Preventative Medicine Physician, Registered Nurse—Community Health Nurse, Registered Nurse—Unspecified; Public Health Science & Animal Control Worker, Behavioral Health Professional, Department/Bureau Director, Deputy Director, Engineer, Environmentalist, Epidemiologist, Health Educator, Other Management and Leadership, Other Professional and Scientific, Program Director, Public Health Manager/Program Manager, Public Health Veterinarian, Public Health Informatics Specialist, Sanitarian/Inspector, Technician, Statistician, Student - Professional and Scientific; Social Services and All Other & Social Services Counselor, Social Worker, Other.40
The Public Health Workforce Interests and Needs Survey (PH WINS) was funded by the de Beaumont Foundation. The de Beaumont Foundation and the Association of State and Territorial Health Officials acknowledge Brenda Joly, Carolyn Leep, Vicki Pineau, Lin Liu, Michael Meit, the PH WINS technical expert panel, and state and local health department staff for their contributions to the PH WINS.
The authors declare no conflicts of interest.
REFERENCES
- 1.Gebbie KM, Rosenstock L, Hernandez LM. Who Will Keep the Public Healthy?: Educating Public Health Professionals for the 21st Century. Washington, DC: National Academies Press; 2002. [PubMed] [Google Scholar]
- 2.Kindig DA. Understanding population health terminology. Milbank Q. 2007;85(1):139–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Winslow CE. The untilled fields of public health. Science. 1920;51(1306):23–33. [DOI] [PubMed] [Google Scholar]
- 4.Institute of Medicine. Committee for the Study of the Future of Public Health. The Future of Public Health. Washington, DC: National Academies Press; 1988. [Google Scholar]
- 5.Lenihan P, Welter C, Chang C, Gorenflo G. The operational definition of a functional local public health agency: the next strategic step in the quest for identity and relevance. J Public Health Manag Pract. 2007;13(4):357–363. [DOI] [PubMed] [Google Scholar]
- 6.Moulton AD, Halverson PK, Honore PA, Berkowitz B. Public health finance: a conceptual framework. J Public Health Manag Pract. 2004;10(5):377–382. [DOI] [PubMed] [Google Scholar]
- 7.Gebbie KM. The public health workforce: key to public health infrastructure. Am J Public Health. 1999;89(5):660–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Allegrante JP, Moon RW, Auld ME, Gebbie KM. Continuing-education needs of the currently employed public health education workforce. Am J Public Health. 2001;91(8):1230–1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lichtveld MY, Cioffi JP, Baker EL, Jr, et al. Partnership for front-line success: a call for a national action agenda on workforce development. J Public Health Manag Pract. 2001;7(4):1–7. [DOI] [PubMed] [Google Scholar]
- 10.Baker EL, Jr, Koplan JP. Strengthening the nation's public health infrastructure: historic challenge, unprecedented opportunity. Health Aff (Millwood). 2002;21(6):15–27. [DOI] [PubMed] [Google Scholar]
- 11.Gebbie K, Merrill J, Tilson HH. The public health workforce. Health Aff (Millwood). 2002;21(6):57–67. [DOI] [PubMed] [Google Scholar]
- 12.Gebbie K, Merrill J, Hwang I, Gebbie EN, Gupta M. The public health workforce in the year 2000. J Public Health Manag Pract. 2003;9(1):79–86. [DOI] [PubMed] [Google Scholar]
- 13.Moser JM. Core academic competencies for master of public health students: one health department practitioner's perspective. Am J Public Health. 2008;98(9):1559–1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Council on Linkages Between Academia and Public Health and Practice. Core Competencies for Public Health Professionals. Washington, DC: Public Health Foundation; 2010. [Google Scholar]
- 15.Public Health Functions Project. The Public Health Workforce: An Agenda for the 21st Century: A Report of the Public Health Functions Project. Darby, PA: DIANE Publishing; 1997. [Google Scholar]
- 16.Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376(9756):1923–1958. [DOI] [PubMed] [Google Scholar]
- 17.Hunter DJ, Lapp I, Frenk J. Education in Public Health. Am J Prev Med. 2014;47(5):S286–S287. [DOI] [PubMed] [Google Scholar]
- 18.Association of Schools and Programs of Public Health. ASPPH Graduate Employment Project: Common Questions Pilot. Washington, DC: Association of Schools and Programs of Public Health; 2015. [Google Scholar]
- 19.Rosenstock L, Silver GB, Helsing K, et al. Confronting the public health workforce crisis: ASPH statement on the public health workforce. Public Health Rep. 2008;123(3):395–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parlette N, Brand R, Gentry D, Gemmell M. Longitudinal Study of Graduates, Schools of Public Health 1956-1985. Washington, DC: Association of Schools of Public Health; 1992. [Google Scholar]
- 21.Moore FI, Hall TL, Chadderdon B, Williams K. Educational Data Project 1974-1979. Houston, TX: Association of Schools of Public Health; 1981. [Google Scholar]
- 22.Gemmell MK, Parsons WB, McCready C, Hannan PG. Schools of Public Health: Educational Data Project 1974-1979. Washington, DC: US Department of Health and Human Services, Public Health Service, Health Resources Administration, Bureau of Health Professions, Division of Associated Health Professions; 1980. [Google Scholar]
- 23.Gebbie KM, Turnock BJ. The public health workforce, 2006: new challenges. Health Aff (Millwood). 2006;25(4):923–933. [DOI] [PubMed] [Google Scholar]
- 24.Gebbie KM, Meier BM, Bakken S, et al. Training for interdisciplinary health research: defining the required competencies. J Allied Health. 2008;37(2):65–70. [PubMed] [Google Scholar]
- 25.Coronado F, Koo D, Gebbie K. The public health workforce: moving forward in the 21st century. Am J Prev Med. 2014;47(5)(suppl 3):S275–S277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaufman NJ, Castrucci BC, Pearsol J, et al. Thinking beyond the silos: emerging priorities in workforce development for state and local government public health agencies. J Public Health Manag Pract. 2014;20(6):557–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wright K, Rowitz L, Merkle A, et al. Competency development in public health leadership. Am J Public Health. 2000;90(8):1202–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ablah E, Tinius AM, Horn L, Williams C, Gebbie KM. Community health centers and emergency preparedness: an assessment of competencies and training needs. J Community Health. 2008;33(4):241–247. [DOI] [PubMed] [Google Scholar]
- 29.Barry MM, Allegrante JP, Lamarre MC, Auld ME, Taub A. The Galway consensus conference: international collaboration on the development of core competencies for health promotion and health education. Glob Health Promot. 2009;16(2):5–11. [DOI] [PubMed] [Google Scholar]
- 30.Gebbie K, Merrill J. Public health worker competencies for emergency response. J Public Health Manag Pract. 2002;8(3):73–81. [DOI] [PubMed] [Google Scholar]
- 31.Gillespie KN, Kurz RS, McBride T, Schmitz HH. Competencies for public health finance: an initial assessment and recommendations. J Public Health Manag Pract. 2004;10(5):458–466. [DOI] [PubMed] [Google Scholar]
- 32.Markenson D, DiMaggio C, Redlener I. Preparing health professions students for terrorism, disaster, and public health emergencies: core competencies. Acad Med. 2005;80(6):517–526. [DOI] [PubMed] [Google Scholar]
- 33.Patel AS, Powell TA, Woolard CD. Assessment of applied epidemiology competencies among the Virginia Department of Health workforce. Public Health Rep. 2008;123(suppl 1):119–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Scutchfield FD, Beaulieu J, Ireson C, Buege A. Public health competencies required by managed care organizations. J Public Health Manag Pract. 2002;8(5):22–29. [DOI] [PubMed] [Google Scholar]
- 35.Thoroughman D. Applied epidemiology competencies: experience in the field. Public Health Rep. 2008;123(suppl 1):8–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Honore PA. Aligning public health workforce competencies with population health improvement goals. Am J Prev Med. 2014;47(5)(suppl 3):S344–S345. [DOI] [PubMed] [Google Scholar]
- 37.Calhoun JG, Ramiah K, Weist EM, Shortell SM. Development of a core competency model for the master of public health degree. Am J Public Health. 2008;98(9):1598–1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Koo D, Birkhead GS, Reingold AL. Competency-based epidemiologic training in public health practice. Public Health Rep. 2008;123(suppl 1):1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hagopian A, Spigner C, Gorstein JL, et al. Developing competencies for a graduate school curriculum in international health. Public Health Rep. 2008;123(3):408–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Leider JP, Bharthapudi K, Pineau V, Lui L, Harper E. The methods behind PH WINS. J Public Health Manag Pract. 2015;21(suppl 6):S28–S35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leider JP, Castrucci BC, Hearne S, Russo P. Organizational characteristics of large urban health departments. J Public Health Manag Pract. 2015;21(suppl 1):S14–S19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sellers K, Leider JP, Harper M, et al. Highlights from the public health workforce interests and needs survey: the first nationally-representative survey of state health agency employee. J Public Health Manag Pract. 2015;21(suppl 6):S13–S27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Association of State and Territorial Health Officials. ASTHO Profile of Health. Vol 3. Washington, DC: Association of State and Territorial Health Officials; 2014. [Google Scholar]
- 44.US Office of Personnel Management. Federal Employee Viewpoint Survey Results. Washington, DC: US Office of Personnel Management.; 2014. [Google Scholar]
- 45.Leider JP, Castrucci BC, Plepys CM, Blakely C, Burke E, Sprague JB. Characterizing the growth of the undergraduate public health major: us, 1992-2012. Public Health Rep (Washington, DC: 1974). 2015;130(1):104–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.US Bureau of Labor Statistics. Educational Attainment for Workers 25 Years and Older by Detailed Occupation. Washington, DC: US Bureau of Labor Statistics; 2013. [Google Scholar]
- 47.US Census Bureau. Educational Attainment in the United States: 2013. Washington, DC: US Census Bureau; 2013. [Google Scholar]
- 48.Association of Schools of Public Health. Annual Data Report 2013. Washington, DC: Association of Schools of Public Health; 2013. [Google Scholar]
- 49.Duffus WA, Trawick C, Moonesinghe R, Tola J, Truman BI, Dean HD. Training racial and ethnic minority students for careers in public health sciences. Am J Prev Med. 2014;47(5):S368–S375. [DOI] [PubMed] [Google Scholar]