Abstract
Purpose
To estimate quality-adjusted life expectancy (QALE) loss among US adults due to depression and QALE losses associated with the increased risk of suicide attributable to depression.
Method
We ascertained depressive symptoms using the eight-item Patient Health Questionnaire (PHQ-8) on the 2006, 2008, and 2010 Behavioral Risk Factor Surveillance System (BRFSS) surveys. We estimated health-related quality of life (HRQOL) scores from BRFSS data (n = 276,442) and constructed life tables from US Compressed Mortality Files to calculate QALE by depression status. QALE loss due to depression is the difference in QALE between depressed and non-depressed adults. QALE loss associated with suicide deaths is the difference between QALE from only those deaths that did not have suicide recorded on the death certificate and QALE from all deaths including those with a suicide recorded on the death certificate.
Results
At age 18, QALE was 28.0 more years for depressed adults and 56.8 more years for non-depressed adults, a 28.9-year QALE loss due to depression. For depressed adults, only 0.41 years of QALE loss resulted from deaths by suicide, and only 0.26 years of this loss could be attributed to depression.
Conclusion
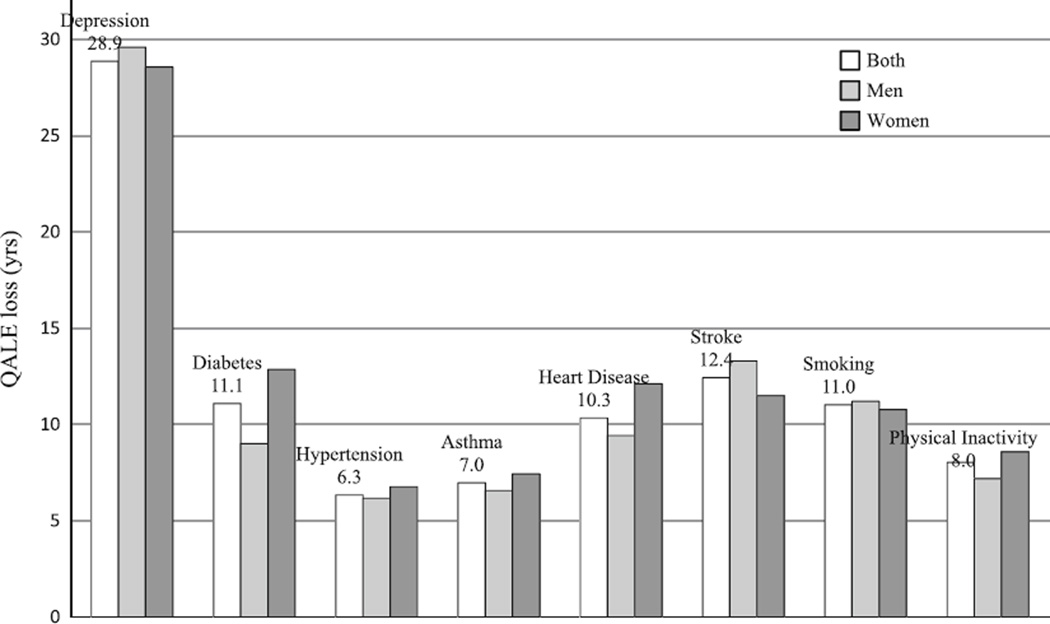
Depression symptoms lead to a significant burden of disease from both mortality and morbidity as assessed by QALE loss. The 28.9-year QALE loss at age 18 associated with depression markedly exceeds estimates reported elsewhere for stroke (12.4-year loss), heart disease (10.3-year loss), diabetes mellitus (11.1-year loss), hypertension (6.3-year loss), asthma (7.0-year loss), smoking (11.0-year loss), and physical inactivity (8.0-year loss).
Keywords: Depression, Suicide, Health-related quality of life (HRQOL), Quality-adjusted life expectancy (QALE), Life expectancy
Introduction
Depression can include several symptoms associated with cognition, negative affect, anxiety, and somatization and can present in individuals in various ways including brief symptoms that often resolve on their own or frequently recurring symptoms that can lead to chronic debilitating mental illness [1]. The prevalence for one kind of chronic depression, major depression, is relatively consistent across large nationally representative surveys: 6.7 % in the past 12 months and 16.6 % over a lifetime [2]. When symptoms that may indicate depression occur within the past 2 weeks, the prevalence of major depression ranges from 3.0 to 3.5 % [3]. When any such symptoms occur within the last 2 weeks, including major depression as well as episodic depression, the prevalence of depression ranges from 7 to 9 % [3].
Depression is a risk factor for many chronic conditions such as cardiovascular diseases and neurological disorders and is associated with risky behaviors such as drug, tobacco, and alcohol abuse [4–7]. Depression is also associated with poor health-related quality of life (HRQOL) and increases the number of years of life lived with disabilities [8, 9]. Depression can be life threatening and has been associated with excess mortality and substantially lower life expectancy [10, 11]. In a longitudinal study of elderly individuals followed up to 48 months, individuals diagnosed with major depression were twice as likely to die as those without depression [12]. Although this increased mortality risk may be indirectly caused by chronic conditions including diabetes and obesity and risky behaviors such as alcohol and drug use, depression alone is likely to be directly responsible through suicide for a proportion of its increased mortality risk [13, 14]. Most individuals who commit suicide have psychiatric illnesses [15]. In a systematic review of risk factors associated with suicide among depressed individuals, many of the most important risk factors included symptoms and conditions associated with depression such as more severe depression (OR = 2.20), hopelessness (2.20), anxiety (OR = 1.59), and the misuse of alcohol and drugs (OR = 2.17) [16]. In one longitudinal study, 8 % of individuals with a major depressive disorder attempted suicide over an 18-month period [17]. However, these studies have many methodological weaknesses that include less representative samples of older patients in clinical settings with multiple chronic conditions, especially those with serious mental illness [12, 17]. Estimates are lacking of the long-term health consequences and losses among representative samples of individuals with depression compared to individuals without depression across their entire life spans as well as comparisons of health losses for those with depression compared to those with other chronic conditions. The magnitude of the impact of depression on suicide and the number of years of life lost due to the increased risk of suicide among those with depression are also unknown [13, 17].
Much of the lifetime burden of disease of depression is associated with the early age of onset of depression. In the National Comorbidity Survey (NCS), the median ages of onset for major depression, dysthymia, and bipolar disorders were 32, 31, and 25 years, respectively [2, 18], significantly younger than the ages of onset for most other chronic conditions such as heart disease and diabetes. Several different methods are available to assess the lifetime burden of disease for a condition such as the years lived with a disability (YLDs), disability-adjusted life years (DALYs), and quality-adjusted life years (QALYs) [19]. In the Global Burden of Disease Study that estimated YLDs worldwide for all infectious and chronic disease conditions, depression was the second leading cause of YLDs [8, 9]. Furthermore, when major depression is combined with other psychiatric conditions that include significant depressive symptoms (e.g., dysthymia and bipolar disorder), this combined estimate for depression is the leading health condition worldwide in terms of DALYs and YLDs [20].
QALYs and an associated measure, quality-adjusted life expectancy (QALE), take into account both the years of life lost and the relative severity of disease, making it possible to quantify the total health losses of both non-fatal and fatal mortality outcomes for affected patients or a target population [19, 21–23]. The burden of disease for non-fatal outcomes for QALYs and QALEs use preference-based HRQOL measures to assess both how a person perceives her/his health and how much that person values one health state versus another state. Preference-based HRQOL measures capture respondents’ health states using a summary score anchored at 0 (dead) and 1 (perfect health) [19]. Thus, 1 year of life lived at a health state valued at 0.5 is assessed as 0.5 quality-adjusted life years (QALYs), the same as only a half year of life lived in perfect health [21, 22]. QALE at a certain age is defined and calculated as the average number of QALYs throughout the remainder of expected life [21, 22]. One advantage of QALE over DALY or YLD is that QALE uses the health state value to weight life years, so that calculating QALE loss due to depression could be useful for evaluating the economic cost of depression and for analyzing the cost-effectiveness of treatments and interventions [19, 21–23].
The first aim of this study is to estimate QALE losses due to depression for US adults and to compare such losses due to depression with previously reported losses due to five other common chronic conditions (stroke, heart disease, diabetes mellitus, hypertension, and asthma) and two significantly harmful health behaviors, smoking and physical inactivity. The second aim of this study is to estimate QALE loss due to increased risk of suicide death attributable to depression. This is the first study we are aware of to estimate QALE losses due to depression as well as losses due to increased risk of suicide death attributable to depression.
Materials and methods
We calculated QALE loss due to depression in four steps. First, using data from the Behavioral Risk Factor Surveillance System (BRFSS), we calculated HRQOL values as a function of age and depression outcome. Second, we estimated age-specific mortality rates stratified by depression status using the Compressed Mortality File. Third, using the estimated age-specific mortality rates from step 2, we constructed life tables to calculate life expectancy as a function of depression and estimate years of life lost due to depression. Fourth, we calculated QALE by combining estimated HRQOL values from step 1 and life tables from step 3. We calculated QALE by depression outcome and estimated QALE loss due to depression.
Sample
The Behavioral Risk Factor Surveillance System (BRFSS), a state-based annual health survey of non-institutionalized civilian US residents, uses random-digit-dialed telephone survey methods to ascertain sociodemographic characteristics, behavioral risk factors, and health outcomes in a population-based random sample of adults 18 years or older [24–26].
BRFSS has included the eight-item Patient Health Questionnaire (PHQ-8) depression scale as an optional module to estimate depressive symptoms and depression status during 2006, 2008, and 2010 [27]. The PHQ-8 is a valid diagnostic and severity measure for depressive disorders in large clinical studies [28] and for estimating depression prevalence [3, 27, 29]. Thirty-six States and the District of Columbia administered the PHQ-8 at least once during these three survey years, yielding a total sample size of 276,442. Current depression in this study is defined as PHQ-8 index ≥10 [27]. The PHQ-8 score of ≥10 has 88 % sensitivity and 88 % specificity for major depression and represents clinically significant depressive symptoms [4, 28, 30].
The BRFSS includes information on respondent sociodemographic characteristics, risky behaviors, and certain diseases related to current depression. We included these variables in analyses of the depression outcome to assess potential associations with these variables. The sociodemographic characteristics analyzed in this study included age, sex, race/ethnicity, marital status, and educational achievement. The risky behaviors included were weight differences from normal weight based on the body mass index (BMI)—underweight (BMI < 18.5 kg/m2), overweight (25 ≤ BMI <30 kg/m2), and obese (BMI ≥ 30.0 kg/m2); current cigarette smoking (respondents who report both having smoked at least 100 cigarettes in their lifetimes and currently smoke); physical inactivity (respondents who report doing no physical activity or exercise during the past 30 days other than that for their regular job); and heavy alcohol drinking (men who report having three or more alcoholic drinks per day and women who report having two or more alcoholic drinks per day). We also assessed associations with cardiovascular-related diseases [had either a heart attack (myocardial infarction), angina or coronary heart disease, or a stroke].
Non-fatal health loss due to depression
Non-fatal health loss due to depression was defined and calculated as the decrease in HRQOL scores for those with current depression compared to those without current depression. The BRFSS questionnaire includes a set of four HRQOL questions that asks respondents to report their general health status (excellent, very good, good, fair, or poor) and the numbers of physically unhealthy days, mentally unhealthy days, and days with activity limitation during the past 30 days [31]. We applied a published mapping algorithm to obtain values of EuroQol Group’s EQ-5D index, a preference-based HRQOL measurement, from the four BRFSS HRQOL items [32, 33]. This algorithm provides valid estimates of EQ-5D scores with a relative bias of less than 1 % of the actual observed EQ-5D [33].
We calculated mean EQ-5D, standardized to the year 2010 US population, for those with current depression and those without current depression, and then estimated the difference in age-adjusted EQ-5D between those with current depression and those without current depression as the non-fatal health loss due to depression.
Fatal health loss due to depression
Fatal health loss due to depression was defined as years of life lost due to depression and was operationalized as the difference in life expectancy between those with current depression and those without current depression [34]. Life expectancy at a given age is the expected/average number of years of life remaining starting at that age and is calculated from age-specific mortality rates [35, 36]. The National Center for Health Statistics compiles death data for the US population from death certificates and makes these data available to the public in the Compressed Mortality File at http://wonder.cdc.gov. The US Census Bureau provides annual population estimates (accessible at www.census.gov/popest/states/asrh/). Both sets of data include age, gender, and other basic demographics, and can be used to estimate age-specific mortality rates for the US population overall, by sex, and by some race/ethnicity subgroups.
Because age-specific mortality rates stratified by depression status are not available, these rates were estimated from three variables—age-specific mortality rates of total population, the proportion of the population with depression, and the hazard ratio of death for those with depression relative to those without depression [37]. We estimated the proportion of the population with depression from the BRFSS and the hazard ratios from the 1999–2004 National Health and Nutrition Examination Survey (NHANES) data as linked to the National Death Index through December 31, 2006 (http://www.cdc.gov/nchs/data_access/data_linkage/mortality/nhanes_99_04_ linkage.htm).
QALE loss due to depression
Like life expectancy, quality-adjusted life expectancy (QALE) at a certain age is the expected/average number of quality-adjusted life years (QALYs) remaining starting at that age and is calculated from age-specific mortality rates and corresponding average HRQOL scores [23, 36]. We constructed life tables to calculate life expectancy and QALE using the age-specific mortality rates and EQ-5D scores. For each year age interval (18–24, 25–34,…, 85 +), we obtained the mortality rates (per year per person) by dividing the numbers of deaths in that age interval by the number of persons in that age interval in the population. We assumed a constant probability of death during each age interval and could thus obtain estimated years of life within the interval [35, 36]. We calculated the QALYs during each age interval by multiplying the life-years within an interval by the corresponding mean EQ-5D value. Life expectancy and QALE for those at a certain age (such as 18 years old) are the average life years and QALYs starting from this age to the last age interval, respectively.
We used the estimated age-specific mortality rates and EQ-5D scores, stratified by depression status, to construct depression-specific life tables and to calculate QALE by respondents’ depression status. Similar to years of life lost due to depression, QALE loss due to depression was defined and estimated as the difference in QALE between those with current depression and those without current depression [37, 38].
QALE loss due to increased risk of suicide death
Suicide deaths are a subset of deaths from all causes. Suicide-associated QALE loss is defined as the impact on QALE due to additional deaths through suicide. This does not include losses due to non-fatal suicide attempts. We calculated this loss as the difference between the QALE from using only those deaths that did not have suicide recorded on the death certificate and the QALE from using all deaths including those with a suicide recorded. Because the risk of suicide is higher among those with depression than among those without depression, we estimated the additional QALE loss due to this increased risk of suicide death attributable to depression as the difference in the suicide-associated QALE loss between those with and those without depression.
Ethics
This analysis used de-identified data produced by federal agencies in the public domain. Data were downloaded from the Centers for Disease Control and Prevention website (ftp://cdc.gov/pub).
Results
We first report our descriptive results (Table 1). Approximately, 9.1 % of US adults were currently depressed based on responses to the PHQ-8. The prevalence of current depression was higher among adults 18–64 years old than older adults. After age adjustment, the prevalence of depression was statistically associated with sex, race/ethnicity, marital status, and education. Specifically, the prevalence of depression was higher among women than men; black non-Hispanics than other race/ethnicity groups; divorced, separated, or never married adults than married, widowed, or unmarried cohabiting adults; and adults with less education than those with more education. Current depression was also more common among those who were underweight or obese, current cigarette smokers, physically inactive, and heavy alcohol drinkers. Those who had cardiovascular diseases were more than twice (20.1 %) as likely to be currently depressed as those who did not have cardiovascular disease (8.0 %). Nearly half (45.6 %) of adults who reported “poor” general health and 22.1 % of adults who reported “fair” general health were currently depressed.
Table 1.
Proportions of Current Depression among US adults by various characteristics
| Characteristics | Proportion of current depression |
||
|---|---|---|---|
| N | Percentagea | SE (%) | |
| All | 276,442 | 9.1 | 0.13 |
| Age | |||
| 18–44 | 85,974 | 9.6 | 0.21 |
| 45–64 | 116,716 | 10.0 | 0.20 |
| 65+ | 73,752 | 5.3 | 0.17 |
| Sex | |||
| Men | 105,354 | 7.1 | 0.44 |
| Women | 171,080 | 11.0 | 0.44 |
| Race/ethnicity | |||
| White non-Hispanics | 217,215 | 8.6 | 0.43 |
| Black non-Hispanics | 26,234 | 11.8 | 0.54 |
| Hispanics | 14,505 | 9.4 | 0.65 |
| Others | 16,526 | 8.7 | 0.65 |
| Marital status | |||
| Married/widowed/unmarried couples | 196,679 | 7.2 | 0.44 |
| Divorced/separated/never married | 79,057 | 13.5 | 0.46 |
| Education | |||
| <High School | 25,306 | 17.2 | 0.73 |
| High school/some college | 158,346 | 10.1 | 0.44 |
| College graduate | 92,485 | 4.6 | 0.41 |
| Body mass index (BMI) category, (kg/m2) | |||
| <18.5 (underweight) | 4,476 | 13.4 | 1.23 |
| 18.5 to <25 (normal weight) | 93,014 | 7.4 | 0.45 |
| 25 to <30 (overweight) | 96,844 | 7.6 | 0.45 |
| ≥30 (obese) | 72,421 | 13.2 | 0.48 |
| Current smoking | |||
| Yes | 50,206 | 17.9 | 0.54 |
| No | 225,337 | 6.9 | 0.41 |
| Physical activity | |||
| Yes | 207,032 | 6.6 | 0.41 |
| No | 69,215 | 17.1 | 0.56 |
| Heavy alcohol drinking | |||
| Yes | 13,443 | 12.6 | 0.85 |
| No | 258,662 | 8.9 | 0.42 |
| Cardiovascular diseases | |||
| Yes | 30,246 | 20.1 | 0.75 |
| No | 244,031 | 8.0 | 0.43 |
| Self-rated general health | |||
| Excellent | 52,535 | 2.2 | 0.43 |
| Very Good | 90,222 | 4.1 | 0.42 |
| Good | 83,350 | 9.5 | 0.53 |
| Fair | 34,696 | 22.1 | 0.72 |
| Poor | 14,869 | 45.6 | 1.06 |
SE standard error of estimate
Weighted proportions of depression, for subgroups except age group itself, proportions were adjusted by age
We also observed gender differences in the magnitude of associations between some of these predictors and current depression. For example, compared to women with depression, men with depression were more likely to have cardiovascular diseases (age-adjusted OR = 1.6), to be heavy drinkers (OR = 2.1), to be current smokers (OR = 1.3), and to be divorced, separated, or never married (OR = 1.2).
We now report our analytic results (Tables 2, 3, 4). For those with depression, the age-adjusted EQ-5D index was 0.598, 0.307 points (34 %) lower than those without depression (0.905) (Table 2). Across subgroups defined by age, sex, race/ethnicity, and simultaneously by race and sex, those who were depressed had consistently lower EQ-5D scores than those who were not depressed. This adverse impact of depression on the EQ-5D index was significantly larger for those 65 years old or older (0.509 points lower) than those 18–44 years old (0.213 points lower) or those 45–64 years old (0.413 points lower); larger for men (0.327 points lower) than women (0.304 points lower); and larger for white non-Hispanics (0.337 points lower) than black non-Hispanics (0.266 points lower) and Hispanics (0.229 points lower).
Table 2.
Impact of depression on EQ-5D scores and life expectancy (LE)
| Characteristics | Not depression |
Depression |
Difference |
Not depression |
Depression |
Difference |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HRQOLa | SE | HRQOLa | SE | Lossb | SE | LE at age 18c |
SE | LE at age 18d |
SE | LE Loss at age 18d |
SE | |
| All | 0.905 | 0.001 | 0.598 | 0.005 | 0.307 | 0.005 | 63.7 | 0.05 | 47.3 | 0.05 | 16.4 | 0.06 |
| By age | ||||||||||||
| 18–44 | 0.934 | 0.001 | 0.721 | 0.006 | 0.213 | 0.006 | 63.7 | 0.05 | 47.3 | 0.05 | 16.4 | 0.06 |
| 45–64 | 0.892 | 0.001 | 0.479 | 0.008 | 0.413 | 0.008 | 38.0 | 0.05 | 24.0 | 0.04 | 14.0 | 0.06 |
| 65+ | 0.838 | 0.002 | 0.330 | 0.013 | 0.509 | 0.014 | 20.8 | 0.05 | 10.5 | 0.03 | 10.3 | 0.05 |
| By sex | ||||||||||||
| Men | 0.912 | 0.002 | 0.585 | 0.009 | 0.327 | 0.010 | 61.2 | 0.08 | 43.0 | 0.07 | 18.2 | 0.10 |
| Women | 0.899 | 0.003 | 0.595 | 0.006 | 0.304 | 0.006 | 66.1 | 0.08 | 50.8 | 0.12 | 15.3 | 0.17 |
| By race/ethnicity | ||||||||||||
| White non-Hispanics | 0.910 | 0.003 | 0.572 | 0.006 | 0.337 | 0.007 | 63.5 | 0.05 | 47.4 | 0.05 | 16.1 | 0.06 |
| Black non-Hispanics | 0.894 | 0.003 | 0.627 | 0.011 | 0.266 | 0.011 | 61.1 | 0.22 | 42.6 | 0.10 | 18.5 | 0.21 |
| Hispanics | 0.890 | 0.003 | 0.661 | 0.015 | 0.229 | 0.015 | 69.2 | 0.49 | 51.2 | 0.18 | 18.0 | 0.46 |
| By sex and race/ethnicity | ||||||||||||
| White non-Hispanic men | 0.917 | 0.003 | 0.571 | 0.010 | 0.346 | 0.011 | 61.1 | 0.08 | 43.2 | 0.07 | 17.9 | 0.10 |
| White non-Hispanic women | 0.903 | 0.003 | 0.573 | 0.007 | 0.330 | 0.008 | 65.8 | 0.08 | 50.8 | 0.12 | 15.0 | 0.17 |
| Black non-Hispanic men | 0.898 | 0.002 | 0.637 | 0.024 | 0.261 | 0.024 | 57.4 | 0.27 | 37.5 | 0.21 | 19.9 | 0.25 |
| Black non-Hispanic women | 0.890 | 0.003 | 0.623 | 0.011 | 0.268 | 0.011 | 64.5 | 0.39 | 46.6 | 0.25 | 18.0 | 0.52 |
| Hispanic men | 0.899 | 0.004 | 0.661 | 0.030 | 0.238 | 0.030 | 66.7 | 0.60 | 46.6 | 0.32 | 20.1 | 0.55 |
| Hispanic women | 0.882 | 0.004 | 0.662 | 0.015 | 0.220 | 0.016 | 71.7 | 0.89 | 54.8 | 0.52 | 16.9 | 1.10 |
SE standard error of estimate
EQ-5D index, for subgroups except age group itself, age-adjusted EQ-5D index
Decrease in EQ-5D index for those with depression
Life expectancy at age 18 years. For the three ages, life expectancy at age 18, 45, and 65 years, respectively
Life expectancy loss due to depression at age 18 years. For the three ages, life expectancy loss at age 18, 45, and 65 years, respectively
Table 3.
Impact of depression on quality-adjusted life expectancy (QALE)
| Characteristics | Not depression |
Depression |
Difference |
|||
|---|---|---|---|---|---|---|
| QALE at age 18a | SE | QALE at age 18a | SE | QALE loss at age 18b | SE | |
| All | 56.8 | 0.08 | 28.0 | 0.19 | 28.9 | 0.21 |
| At ages | ||||||
| At 18 | 56.8 | 0.08 | 28.0 | 0.2 | 28.9 | 0.21 |
| At 25 | 50.5 | 0.08 | 22.7 | 0.2 | 27.8 | 0.20 |
| At 35 | 41.5 | 0.08 | 16.1 | 0.2 | 25.4 | 0.19 |
| At 45 | 32.8 | 0.08 | 10.4 | 0.2 | 22.3 | 0.17 |
| At 55 | 24.7 | 0.08 | 6.6 | 0.1 | 18.1 | 0.17 |
| At 65 | 17.3 | 0.08 | 3.5 | 0.1 | 13.8 | 0.17 |
| At 75 | 11.2 | 0.10 | 1.8 | 0.1 | 9.4 | 0.16 |
| At 85 | 6.9 | 0.14 | 0.9 | 0.1 | 6.0 | 0.15 |
| By sex | ||||||
| Men | 55.2 | 0.10 | 25.6 | 0.33 | 29.6 | 0.35 |
| Women | 58.4 | 0.14 | 29.8 | 0.24 | 28.6 | 0.28 |
| By race/ethnicity | ||||||
| White non-Hispanics | 56.9 | 0.07 | 27.6 | 0.23 | 29.3 | 0.24 |
| Black non-Hispanics | 53.7 | 0.27 | 26.9 | 0.37 | 26.8 | 0.46 |
| Hispanics | 58.0 | 1.58 | 31.6 | 0.87 | 26.4 | 1.76 |
| By sex and race/ethnicity | ||||||
| White non-Hispanic men | 55.4 | 0.09 | 25.6 | 0.37 | 29.7 | 0.38 |
| White non-Hispanic women | 58.4 | 0.10 | 29.2 | 0.28 | 29.2 | 0.30 |
| Black non-Hispanic men | 51.0 | 0.35 | 24.9 | 0.66 | 26.0 | 0.72 |
| Black non-Hispanic women | 56.2 | 0.41 | 28.6 | 0.45 | 27.6 | 0.63 |
| Hispanic men | 59.1 | 0.84 | 28.2 | 1.25 | 30.8 | 1.48 |
| Hispanic women | 57.9 | 2.36 | 34.2 | 1.13 | 23.7 | 2.58 |
SE Standard error of estimate
QALE at age 18 years. For the eight ages, QALE at age 18, 25, 35, 45, 55, 65, 75, and 85 years, respectively
QALE loss due to depression at age 18 years. For the eight ages, QALE loss at age 18, 25, 35, 45, 55, 65, 75, and 85 years, respectively
Table 4.
Additional quality-adjusted life expectancy (QALE) loss associated with the increased risk of suicide attributable to depression
| Sex | Depression | Use all-cause mortality |
Use non-suicide mortality |
Loss to suicide |
|||
|---|---|---|---|---|---|---|---|
| QALEa | SE | QALEa | SE | Lossb | SE | ||
| Both | Yes | 27.97 | 0.19 | 28.38 | 0.20 | 0.41 | 0.01 |
| No | 56.84 | 0.08 | 56.99 | 0.08 | 0.15 | 0.01 | |
| Additional lossc | 0.26 | 0.01 | |||||
| Men | Yes | 25.64 | 0.33 | 26.40 | 0.35 | 0.76 | 0.03 |
| No | 55.24 | 0.10 | 55.45 | 0.10 | 0.21 | 0.01 | |
| Additional lossc | 0.55 | 0.03 | |||||
| Women | Yes | 29.80 | 0.24 | 30.02 | 0.24 | 0.22 | 0.02 |
| No | 58.38 | 0.14 | 58.46 | 0.14 | 0.08 | 0.02 | |
| Additional lossc | 0.14 | 0.02 | |||||
SE standard error of estimate
Calculated QALE at age
QALE loss at age 18 due to additional deaths by suicide
Additional QALE loss at age 18 due to increased risk of suicide among those with depression
The life expectancy at age 18 years was 47.3 more years for those with depression and 63.7 more years for those without depression. This 16.4-year (26 %) decrease represents the years of life lost due to depression, starting at age 18. The loss in life expectancy at age 18 for men with depression was 18.2 years, significantly more than the 15.3 years of life lost for women with depression (p < 0.0001). Although the decreases in EQ-5D index were larger for white non-Hispanics than for other groups, the losses in life expectancy due to depression were significantly less for white non-Hispanics (16.1 years) than for black non-Hispanics (18.5 years) and for Hispanics (18.0 years).
The lower EQ-5D and life expectancy among those with depression yield a significantly lower QALE among those with depression (Table 3). The QALE for an 18-year-old with depression, for example, was 28.0 years, 28.9 years less than that of an 18-year-old without depression (56.8 years). This represents a decrease of QALE by more than half (51 %) for those with depression. Although QALE declined with age, depression-associated QALE losses were significant at all ages. For example, an 85-year-old person with depression had a significantly lower QALE (0.9 year) than an 85-year-old person without depression (6.9 years), a 6.0-year loss in QALE. The depression-associated QALE loss at age 18 was significantly larger among men (29.6-year loss) than among women (28.6-year loss) and larger among white non-Hispanics (29.3-year loss) than among black non-Hispanics (26.8 years) and among Hispanics (26.4-year loss), though this difference between white non-Hispanics and Hispanics was not statistically significant (p = 0.1).
The second aim of this study estimated suicide-associated QALE loss (Table 4). For those with depression, the calculated QALE at age 18 using non-suicide mortality rates was 28.38 years, 0.41 years more than that using mortality rates including suicides (27.97 years). Thus, death by suicide contributed 0.41 years of QALE loss for those with depression. Similarly, death by suicide contributed only 0.15 years of QALE loss for those without depression. This 0.26-year difference (0.26 = 0.41–0.15) was the additional QALE loss associated with the increased risk for suicide among those with depression. Men lost more QALE to suicide death than women did, both for those with depression and those without depression. The additional QALE loss for men with depression due to their increased risk of death through suicide was 0.55 years, more than threefold that of the 0.14-year additional loss for women with depression.
Finally, we conducted a sensitivity analysis to examine the impact of suicide misclassification within death certificates on the QALE loss due to suicide. We included all unknown accident deaths as suicide deaths (i.e., new suicides = recorded suicides + unknown accident deaths) and recalculated the QALE loss due to suicide. The new calculated value of the additional QALE loss associated with the increased risk for suicide among depressed adults increased from 0.26 years to 0.29 years of QALE loss.
Discussion
These analyses confirmed previous studies suggesting large adverse impacts of depression on both fatal and non-fatal outcomes [4, 13, 39]. The estimated burden of disease for depression for depressed individuals during their entire life span starting at age 18 was 28.9 years of QALE loss, a loss of more than half their QALE at this age. This result is consistent with previous studies that have shown a dramatic decrease in life expectancy for those with serious mental illnesses [40, 41]. This 28.9-year loss in QALE also markedly exceeds that of other chronic conditions such as stroke (12.4-year loss), heart disease (10.3-year loss), diabetes mellitus (11.1-year loss), hypertension (6.3-year loss), and asthma (7.0-year loss), and the risk factors such as smoking (11.0-year loss) and physical inactivity (8.0-year loss) reported previously (Fig. 1) [22, 37, 42]. This QALE loss also mirrors other studies concluding that depression is the top health condition worldwide in terms of disability-adjusted life years (DALYs) [20]. At least three reasons may explain this excessive QALE loss. First, the non-fatal health losses due to depression appear significantly larger than the loss due to each of the other chronic conditions mentioned previously. Major depressive disorder contributed 917 years lived with a disability (YLDs) per 100,000 persons annually, more than those of these five other chronic conditions mentioned above combined (821 YLDs per 100,000) [9]. In our study, depression decreased the EQ-5D index by 0.307 points, equivalent to a decrease in the EQ-5D index from having no chronic conditions to having between five and six chronic conditions [43] and significantly more than the 0.07–0.16 point decrease associated with any of the five other conditions and the two risky behaviors [22, 37, 42]. Second, depression affected mortality and life expectancy more than the other conditions. People with serious mental illness, which includes clinical depression, died an average of 25 years sooner than those in the general population [44]. In this study, depression decreased life expectancy at age 18 by 16.4 years, significantly more than that of the other five chronic conditions [22] and two risky behaviors [37, 42], which ranged from 3.1 years (hypertension) to 9.8 years (stroke). Third, much of the lifetime burden of disease associated with depression is based on its early age of onset. The median ages of onset for major depression (32 years), dysthymia (31 years), and bipolar disorders (25 years) are significantly younger than those for most other chronic conditions such as heart disease and diabetes mellitus [2]. For example, about 75 % of heart disease and 84 % of stroke occur first after age 55 [22]. In this study, the depression prevalence was significantly higher among younger persons (9.8 % for those < 65 years) than older persons (5.3 % for those ≥65 years).
Fig. 1.
Comparison of quality-adjusted life expectancy (QALE) losses due to depression, diabetes mellitus [22], hypertension [22], asthma [22], heart disease [22], stroke [22], smoking [37], and physical inactivity [42]
Although age-adjusted depression prevalence rates in women exceeded those in men, the QALE losses associated with depression were one year more in men than in women. This difference in QALE losses between men and women resulted from the difference in the impacts on both fatal and nonfatal outcomes. Men lost significantly more years of life and experienced larger EQ-5D losses to depression than women. Compared to women with depression, men with depression were more likely to have cardiovascular diseases, to be heavy drinkers, to be current smokers, and to be divorced, separated, or never married. All of these factors are associated with poor health outcomes. Depression also has a much large impact on mortality among men than women [13, 45, 46]. Among three race/ ethnicity subgroups in our study, depression decreased the EQ-5D index more but decreased life expectancy less in white non-Hispanics than in black non-Hispanics and Hispanics, though the combined QALE loss among white non-Hispanics (28.6-year loss) significantly exceeded that among black non-Hispanics (25.8-year loss).
Our descriptive analyses of depression confirmed previous studies of associations between depression and some sociodemographic characteristics, risky behaviors, and diseases [4–7, 13, 39]. Although these variables are potential confounders for the decreased QALE among depressed individuals, our QALE estimates were not adjusted for these factors. Therefore, the term “QALE loss due to depression” does not suggest a causal relationship. However, our estimated QALE loss due to depression markedly exceeds that of diseases associated with depression, such as heart diseases and stroke, and risky behaviors, such as smoking and physical inactivity [22, 37, 42]. In addition, our study used similar methods to these previous studies and is consistent with currently accepted methods in the literature. These findings strongly suggest that depression contributes lower QALE among individuals with depression independent of these diseases and risk factors.
Depression may be directly related to the increased risk of death through suicide [13, 14] because a large proportion of persons who committed suicide had pre-existing depression [1, 47]. Nonetheless, in this study, suicide contributed very little to QALE loss for both those with depression (0.41 years) and those without depression (0.15 years). Only 0.26 years of additional QALE losses for those with depression could be attributed to their increased risk of suicide. This 0.26 years of QALE loss was much smaller than the nearly 30 years of overall QALE loss due to depression: Only 0.9 % (1.8 % for men and 0.5 % of for women) of the depression-associated QALE loss was due to the increased risk of suicide among those with depression. This most likely results from the fact that, although many who die from suicide suffer from mental disorders [48], almost all of those individuals diagnosed with a mental disorder including those with clinical depression do not die directly from suicide but from other causes [3, 13, 49]. Only 1.4 % (2.3 % for men and 0.58 % for women) of all deaths among US adults had an underlying cause of suicide, even though suicide is the second leading cause of death among those aged 15–24 years [1, 50]. Related to this, depression usually is associated with inactivity, lethargy, and a general decline in health practices and self-care which puts those with depression at higher risk for other chronic conditions [47]. Because the Compressed Mortality File, compiled from death certificates, might underreport suicides and misclassify some suicide deaths as unknown deaths from injuries [51, 52], this study may have underestimated the impact of suicide on QALE loss. However, our sensitivity analysis showed that even attributing all unknown deaths from injuries as suicide deaths increased the estimated additional QALE loss associated with the increased risk for suicide among those with depression only 0.03 years, from 0.26 years to 0.29 years.
This study has several weaknesses. First, the PHQ-8 is not a clinical diagnostic tool for diagnosing depression but has been used primarily as a screening instrument for estimating the prevalence of depression in the general population. This would tend to reduce the accuracy and the reliability of the population estimates relative to a clinical diagnosis or interview. Second, the reporting of depressive symptoms might show mode effects that may have affected our estimates; individuals administered face-to-face interviews tend to report better health (social desirability effects) than those interviewed by telephone [3, 53]. The estimated prevalence of current depression using the BRFSS, a telephone survey, was higher (9.1 %) than the estimates using the NHANES, an in-person interview (6.8 %) [3]. However, such a higher estimated prevalence for depression would have resulted in a relatively small change in the estimated depression-associated QALE loss. For example, if we had used the estimated depression prevalence from the NHANES (6.8 % overall), the estimated QALE loss due to depression would be 28.6 years, only 0.23 year less than the 28.9 years of the estimated QALE loss based on the estimated 9.1 % overall depression prevalence from the BRFSS. Third, the BRFSS data are collected via telephone interviews using a random-digit-dialed methodology that most likely underestimates the prevalence of depression because the study population includes only non-institutionalized household members. However, our analysis demonstrates that underestimating depression prevalence would have a small effect on the estimation of QALE loss due to depression. Fourth, our estimated hazard ratios from the NHANES linked mortality data exceed others reported in the literature [12, 45], and using larger estimates of these hazard ratios would overestimate depression-associated QALE losses. If we had used the smaller estimated hazard ratio by Sullivan et al. [12] and Zheng et al. [45], the estimated QALE losses would be 26.2 years (28.1 years for men and 25.0 years for women). However, such estimates were not statistically significantly different from the estimated QALE losses in this study. Fifth, this study relies on the BRFSS’s unhealthy days questions to estimate preference-based HRQOL scores indirectly rather than on direct measurements of these scores. Therefore, our estimates of QALE loss are likely to be smaller than the true values due to “regression to the mean” [32–37]. One study estimated the bias of estimated QALE loss using the estimated EQ-5D scores and found that this bias was less than 2.5 % of that using the actual EQ-5D questions [36]. Finally, not all the US states used the PHQ-8 questionnaire. Thus, if the prevalence of depression in the states using this questionnaire differed from that in the states not using this questionnaire, these results may not be fully generalizable to the entire US population. However, our analysis above on the small effects of differences in estimated depression prevalence on QALE loss due to depression may mitigate this lack of generalizability.
This study is the first we know of to estimate burden of disease for depression by comparing the QALE for currently depressed persons to that for non-depressed persons. QALE is a single index that encompasses both depression-related fatal and nonfatal outcomes. Therefore, our results are particularly useful in directly comparing the burdens of disease for depression to the burdens of disease for other chronic conditions and risky behaviors and for estimating the economic costs of depression among U.S adults [19–23]. The overall burden of depression was at least twice as large as the burdens of some common chronic conditions such as stroke, heart disease, diabetes mellitus, hypertension, and asthma and of the risk factor of smoking. This information could be useful to local and state authorities when setting health priorities and when dealing with mental problems in the general adult population [54, 55]. These results will also likely to motivate the development of improved prevention efforts and strategies for individuals at risk for depression and suicide [56–58].
Acknowledgments
This study (Jia) is supported by a CDC contract (No. 200-2011-M-41977).
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
Contributor Information
Haomiao Jia, Department of Biostatistics, Mailman School of Public Health, and School of Nursing, Columbia University, 617 West 168th, Street, New York, NY 10032, USA, hj2198@columbia.edu.
Matthew M. Zack, Division of Population Health, National Center for Chronic, Disease Prevention and Health Promotion, Centers for Disease, Control and Prevention, Atlanta, GA, USA, mmz1@cdc.gov
William W. Thompson, Email: wct2@cdc.gov, Division of Population Health, National Center for Chronic, Disease Prevention and Health Promotion, Centers for Disease, Control and Prevention, Atlanta, GA, USA
Alex E. Crosby, Division of Violence Prevention, National Center for Injury, Prevention and Control, Centers for Disease Control and, Prevention, Atlanta, GA, USA, aec1@cdc.gov
Irving I. Gottesman, Department of Psychology, University of Minnesota, Twin Cities, MN, USA, gotte003@umn.edu
References
- 1.Goodwin FK, Jamison KR. Manic-depressive illness: bipolar disorders and recurrent depression. 2nd edn. New York: Oxford University Press; 2007. [Google Scholar]
- 2.Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 3.Reeves WC, Strine TW, Pratt LA, et al. Mental illness surveillance among adults in the United States. MMWR Surveill Summ. 2011;60(Suppl 3):1–29. [PubMed] [Google Scholar]
- 4.Krishnan KR, Delong M, Kraemer H, et al. Comorbidity of depression with other medical diseases in the elderly. Biol Psychiatry. 2002;52(6):559–588. doi: 10.1016/s0006-3223(02)01472-5. [DOI] [PubMed] [Google Scholar]
- 5.Kupfer DJ, Frank E. Comorbidity in depression. Acta Psychiatr Scand. 2003;(Suppl Suppl 418):57–60. doi: 10.1034/j.1600-0447.108.s418.12.x. [DOI] [PubMed] [Google Scholar]
- 6.Saluja G, Iachan R, Scheidt PC, Overpeck MD, Sun W, Giedd JN. Prevalence of and risk factors for depressive symptoms among young adolescents. Arch Pediatr Adolesc Med. 2004;158(8):760–765. doi: 10.1001/archpedi.158.8.760. [DOI] [PubMed] [Google Scholar]
- 7.Dickey B, Normand SL, Weiss RD. Medical morbidity, mental illness, and substance use disorders. Psychiatr Serv. 2002;53(7):861–867. doi: 10.1176/appi.ps.53.7.861. [DOI] [PubMed] [Google Scholar]
- 8.Lokkerbol J, Adema D, de Graaf R, et al. Non-fatal burden of disease due to mental disorders in the Netherlands. Soc Psychiatry Psychiatr Epidemiol. 2013;48(10):1591–1599. doi: 10.1007/s00127-013-0660-8. [DOI] [PubMed] [Google Scholar]
- 9.Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang CK, Hayes RD, Perera G, et al. Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS One. 2011;6(5):e19590. doi: 10.1371/journal.pone.0019590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fortes C, Mastroeni S, Alessandra S, et al. The combination of depressive symptoms and smoking shorten life expectancy among the aged. Int Psychogeriatr. 2012;24(4):624–630. doi: 10.1017/S1041610211002201. [DOI] [PubMed] [Google Scholar]
- 12.Sullivan MD, O’Connor P, Feeney P, et al. Depression predicts all-cause mortality: epidemiological evaluation from the ACCORD HRQL substudy. Diabetes Care. 2012;35(8):1708–1715. doi: 10.2337/dc11-1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dembling BP, Chen DT, Vachon L. Life expectancy and causes of death in a population treated for serious mental illness. Psychiatr Serv. 1999;50(8):1036–1042. doi: 10.1176/ps.50.8.1036. [DOI] [PubMed] [Google Scholar]
- 14.Simon GE, Rutter CM, Peterson D, et al. Does response on the PHQ-9 depression questionnaire predict subsequent suicide attempt or suicide death? Psychiatr Serv. 2013;64(12):1195–1202. doi: 10.1176/appi.ps.201200587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hawton K, van Heeringen K. Suicide. Lancet. 2009;373(9672):1372–1381. doi: 10.1016/S0140-6736(09)60372-X. [DOI] [PubMed] [Google Scholar]
- 16.Hawton K, Saunders K, Topiwala A, Haw C. Psychiatric disorders in patients presenting to hospital following self-harm: a systematic review. J Affect Disord. 2013;151(3):821–830. doi: 10.1016/j.jad.2013.08.020. [DOI] [PubMed] [Google Scholar]
- 17.Sokero TP, Melartin TK, Rytsälä HJ, et al. Prospective study of risk factors for attempted suicide among patients with DSM-IV major depressive disorder. Br J Psychiatry. 2005;186:314–318. doi: 10.1192/bjp.186.4.314. [DOI] [PubMed] [Google Scholar]
- 18.Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. 2012;21(3):169–184. doi: 10.1002/mpr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gold MR, Siegel JE, Russell RB, Weinstein MC. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996. [Google Scholar]
- 20.Murray CJ, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–2223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 21.Rosenberg MA, Fryback DG, Lawrence WF. Computing population-based estimates of health-adjusted life expectancy. Med Decis Making. 1999;19(1):90–97. doi: 10.1177/0272989X9901900111. [DOI] [PubMed] [Google Scholar]
- 22.Jia H, Zack MM, Thompson WW. The effects of diabetes, hypertension, asthma, heart disease, and stroke on quality-adjusted life expectancy. Value Health. 2013;16(1):140–147. doi: 10.1016/j.jval.2012.08.2208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brown DS, Jia H, Zack MM, Thompson WW, Haddix AC, Kaplan RM. Using health-related quality of life and quality-adjusted life expectancy for effective public health surveillance and prevention. Expert Rev Pharmacoecon Outcomes Res. 2013;13(4):425–427. doi: 10.1586/14737167.2013.818816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frazier EL, Franks AL, Sanderson LM. Using chronic disease data: a handbook for public health practitioners. Atlanta: Centers for Disease Control and Prevention; 1992. Using behavioral risk factor surveillance data; pp. 4.1–4.17. [Google Scholar]
- 25.Mokdad AH, Stroup DF, Giles WH Behavioral Risk Factor Surveillance Team. Public health surveillance for behavioral risk factors in a changing environment. Recommendations from the Behavioral Risk Factor Surveillance Team. MMWR Recomm Rep. 2003;52(RR–9):1–12. [PubMed] [Google Scholar]
- 26.Xu F, Town M, Balluz LS, et al. Surveillance for certain health behaviors among states and selected local areas—United States, 2010. MMWR Surveill Summ. 2013;62(1):1–247. [PubMed] [Google Scholar]
- 27.Dhingra SS, Kroenke K, Zack MM, Strine TW, Balluz LS. PHQ-8 days: a measurement option for DSM-5 major depressive disorder (MDD) severity. Popul Health Metr. 2011;9:11. doi: 10.1186/1478-7954-9-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1–3):163–173. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 30.Corson K, Gerrity MS, Dobscha SK. Screening for depression and suicidality in a VA primary care setting: 2 items are better than 1 item. Am J Manag Care. 2004;10(11 Pt 2):839–845. [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. Measuring healthy days: population assessment of health-related quality of life. US Department of Health and Human Services. Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion. Division of Adult and Community Health. 2000 http://www.cdc.gov/hrqol/pdfs/mhd.pdf.
- 32.Jia H, Lubetkin EI. Estimating EuroQol EQ-5D scores from Population Healthy Days data. Med Decis Making. 2008;28(4):491–499. doi: 10.1177/0272989X07312708. [DOI] [PubMed] [Google Scholar]
- 33.Jia H, Zack MM, Moriarty DG, Fryback DG. Predicting the EuroQol Group’s EQ-5D index from CDC’s “Healthy Days” in a US sample. Med Decis Making. 2011;31(1):174–185. doi: 10.1177/0272989X10364845. [DOI] [PubMed] [Google Scholar]
- 34.Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289(2):187–193. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 35.Chiang CL. Statistical inference regarding life table functions. In: Chiang CL, editor. The life table and its applications. Malabar: Robert E. Krieger Publishers; 1984. pp. 153–167. [Google Scholar]
- 36.Jia H, Zack MM, Thompson WW. State quality-adjusted life expectancy for US adults from 1993 to 2008. Qual Life Res. 2011;20(6):853–863. doi: 10.1007/s11136-010-9826-y. [DOI] [PubMed] [Google Scholar]
- 37.Jia H, Zack MM, Thompson WW, Dube SR. Quality-adjusted life expectancy (QALE) loss due to smoking in the United States. Qual Life Res. 2013;22(1):27–35. doi: 10.1007/s11136-012-0118-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee HY, Hwang JS, Jeng JS, Wang JD. Quality-adjusted life expectancy (QALE) and loss of QALE for patients with ischemic stroke and intracerebral hemorrhage: a 13-year follow-up. Stroke. 2010;41(4):739–744. doi: 10.1161/STROKEAHA.109.573543. [DOI] [PubMed] [Google Scholar]
- 39.Chapman DP, Perry GS, Strine TW. The vital link between chronic disease and depressive disorders. Prev Chronic Dis. 2005;2(1):A14. [PMC free article] [PubMed] [Google Scholar]
- 40.Manderscheid R, Druss B, Freeman E. Data to manage the mortality crisis. Intl J Ment Health. 2008;37(2):49–68. [Google Scholar]
- 41.Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. Prev Chronic Dis. 2006;3(2):A42. [PMC free article] [PubMed] [Google Scholar]
- 42.Jia H, Lubetkin EI. Comparing quality-adjusted life expectancy at different levels of physical activity. J Phys Act Health. 2014;11(2):278–284. doi: 10.1123/jpah.2011-0368. [DOI] [PubMed] [Google Scholar]
- 43.Sullivan PW, Lawrence WF, Ghushchyan V. A national catalog of preference-based scores for chronic conditions in the United States. Med Care. 2005;43(7):736–749. doi: 10.1097/01.mlr.0000172050.67085.4f. [DOI] [PubMed] [Google Scholar]
- 44.National Association of State Mental Health Program Directors. Alexandria: Thirteenth in a series of technical reports; 2006. [Accessed 27 July 2014]. Morbidity and mortality in people with serious mental illness. http://www.nasmhpd.org/Publications/NASMHPDMedicalDirectorsCouncil.aspx. [Google Scholar]
- 45.Zheng D, Macera CA, Croft JB, Giles WH, Davis D, Scott WK. Major depression and all cause mortality among white adults in the United States. Ann Epidemiol. 1997;7(3):213–218. doi: 10.1016/s1047-2797(97)00014-8. [DOI] [PubMed] [Google Scholar]
- 46.Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. J Affect Disord. 2002;72(3):227–236. doi: 10.1016/s0165-0327(01)00413-x. [DOI] [PubMed] [Google Scholar]
- 47.Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33:395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- 48.Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- 49.Dickey B, Dembling B, Azeni H, Normand SL. Externally caused deaths for adults with substance use and mental disorders. J Behav Health Serv Res. 2004;31(1):75–85. doi: 10.1007/BF02287340. [DOI] [PubMed] [Google Scholar]
- 50.Hoyert DL, Xu J. Deaths: preliminary data for 2011. National vital statistics reports. 6. Vol. 61. Hyattsville: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 51.Rockett IR, Kapusta ND, Coben JH. Beyond suicide: action needed to improve self-injury mortality accounting. JAMA Psychiatry. 2014;71(3):231–232. doi: 10.1001/jamapsychiatry.2013.3738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rockett IR, Kapusta ND, Bhandari R. Suicide misclassification in an international context: revisitation and update. Suicidol Online. 2011;2:48–61. [Google Scholar]
- 53.Hays RD, Kim S, Spritzer KL, Kaplan RM, Tally S, Feeny D, Liu H, Fryback DG. Effect of mode and order of administration on generic health-related quality of life scores. Value Health. 2009;12:1035–1039. doi: 10.1111/j.1524-4733.2009.00566.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.National Research Council and Institute of Medicine. Preventing mental, emotional, and behavioral disorders among young people: progress and possibilities. Committee on the prevention of mental disorders and substance abuse among children, youth, and young adults: research advances and promising interventions. In: O’ Connell ME, Boat T, Warner KE, editors. Board on children, youth, and families, division of behavioral and social sciences and education. Washington: National Academies Press; 2009. [PubMed] [Google Scholar]
- 55.Institute of Medicine. Preventing mental, emotional, and behavioral disorders among young people: progress and possibilities. Washington: National Academies Press; 2009. [PubMed] [Google Scholar]
- 56.Cicchetti D. Resilience under conditions of extreme stress: a multilevel perspective. World Psychiatry. 2010;9(3):145–154. doi: 10.1002/j.2051-5545.2010.tb00297.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Snowden M, Steinman L, Frederick J. Treating depression in older adults: challenges to implementing the recommendations of an expert panel. Prev Chronic Dis. 2008;5(1):A26. [PMC free article] [PubMed] [Google Scholar]
- 58.Courtet P, Gottesman II, Jollant F, Gould TD. The neuroscience of suicidal behaviors: what can we expect from en-dophenotype strategies? Transl Psychiatry. 2011 doi: 10.1038/tp.2011.6. [DOI] [PMC free article] [PubMed] [Google Scholar]