Abstract
The study was designed to test the feasibility and child clinical outcomes for a group-based application of Trauma-focused Cognitive Behavior Therapy (TF-CBT) for orphaned children with unresolved grief in Moshi, Tanzania. Sixty-four orphaned children with at least mild symptoms of unresolved grief and/or traumatic stress and their guardians participated in the open trial. The evidence-based TF-CBT protocol was adapted for group delivery, resulting in 12 weekly sessions for child and guardians separately with conjoint activities and three individual visits. Using a task-sharing approach, the intervention was delivered by lay counselors with no prior mental health experience. Primary outcomes assessed were symptoms of unresolved grief and posttraumatic stress (PTS); secondary outcomes included symptoms of depression and overall behavioral adjustment. All assessments were conducted pre-treatment, post-treatment, and 3- and 12-months after the end of treatment. Results showed improved scores on all outcomes post-treatment, sustained at 3 and 12 months. Effect sizes (Cohen’s d) for baseline to post-treatment were 1.36 for child reported grief symptoms; 1.87 for child-reported PTS, and 1.15 for caregiver report of child PTS.
Keywords: orphaned children, trauma-focused cognitive behavioral therapy, unresolved grief, sub-Saharan Africa
Reports highlight the large number of children orphaned in low- and middle-income countries (LMIC) with high prevalence HIV/AIDS. An estimated 16.6 million children have had at least one parent die from the disease, and 90 percent live in sub-Saharan Africa (Joint United Nations Programme on HIV/AIDS [UNAIDS], 2012). Orphaned children in LMIC have high rates of unmet psychological needs (Kieling et al., 2011) and limited access to mental health care (Saxena, Thornicroft, Knapp, & Whiteford, 2007). When treatment is available, rarely does it have prior evidence of effectiveness (Patel, Flisher, Nikapota, & Malhotra, 2008). Researchers advocate for translating evidence-based treatments (EBT) from the high-income settings (HIC) in which they were developed and tested to the geographical and cultural demands of resource-limited areas (e.g., Patel, Chowdhary, Rahman, & Verdeli, 2011), using a task-sharing approach (World Health Organization [WHO], 2007).
The death of a parent can be the most stressful event in a child’s life (UNAIDS, United Nations Children’s Fund, & U. S. Agency for International Development, 2004; Rotheram-Borus, Weiss, Alber, & Lester, 2005). Studies with African youth have found that those orphaned have higher rates of unresolved grief, posttraumatic stress symptoms (PTS), depression, suicidal thoughts (12.2% vs. 2.7%), anxiety, behavior problems, and a negative outlook on their life (32.5% vs. 5.5%; Atwine, Cantor-Graae, & Bajunirwe, 2005; Cluver, Gardner & Operario, 2007;). In a qualitative study designed to develop an assessment of the needs of orphaned children, guardians indicated that one of their main difficulties was the child’s ongoing grief; they said they did not know how to help the child with this sadness (O’Donnell, Nyangara, Murphy, & Nyberg, 2008.) Psychological consequences of parental death can be exacerbated by the nature of the death, other life changes, stigma, separation from siblings, and other potentially traumatic circumstances (Andrews, Skinner, & Zuma, 2006; Whetten et al., 2011; Kaplow, Howell, & Layne, 2014). Unresolved grief became the focus of this study.
Debate over the best term for grief-related symptoms is ongoing: maladaptive grief reaction, traumatic grief, complicated grief, unresolved grief, among others (Cohen, Mannarino, Greenberg, Padlo, & Shipley, 2002; Melhem, Moritz, Walker, Shear, & Brent, 2007; Nader & Layne, 2009; Maercker & Lalor, 2012). We use the term unresolved grief to capture clinically significant symptoms continuing at least six months after parental death (e.g., Melhem et al., 2007; Kaplow et al., 2014), including preoccupation with the deceased, detachment from others, and distress with memories of the deceased.
WHO guidelines recommend “structured psychological interventions” (Tol, Barbui, & van Ommeren, 2013, p. 478) for bereavement and Cognitive Behavioral Therapy (CBT) with a trauma focus for PTS (see WHO, 2013). Trauma-focused CBT (TF-CBT) was chosen for this study with symptomatic orphaned children because it has a strong evidence base (i.e., approximately 14 prior randomized controlled trials) and the flexibility to address both PTS and unresolved grief (Dorsey, Woods, & Briggs, 2011). Our work builds on two prior studies in the US demonstrating efficacy for TF-CBT for Childhood Traumatic Grief (TF-CBT for CTG) delivered individually (Cohen, Mannarino, & Knudsen, 2004; Cohen, Mannarino, & Deblinger, 2006; Cohen, Mannarino, & Staron, 2006). The grief-based protocol for TF-CBT has not yet been tested for groups or in LMIC.
There is a growing number of studies on EBT in LMIC, though most focus on adults (e.g., Bolton et al., 2003; Rahman, Malik, Sikander, Roberts, & Creed, 2008; Patel et al., 2010; Bass et al., 2013). Two studies provide examples of TF-CBT trials with children in LMIC. The first is an open trial in Zambia with children exposed to a range of traumatic events (e.g., sexual abuse, domestic violence; Murray et al., 2013). The individually delivered intervention was significantly associated with reductions in PTS. The second is a randomized controlled trial (RCT) in the Democratic Republic of Congo with war-exposed and sexually exploited female adolescents (O’Callaghan, McMullen, Shannon, Rafferty, & Black, 2013); group-based TF-CBT was predictive of reduced PTS, depression, anxiety, and conduct problems.
The present study is an open trial of TF-CBT in Moshi, Tanzania designed to examine the feasibility and clinical outcomes of a group-based application of TF-CBT with children who were single or double orphans with unresolved grief and/or PTS symptoms and their guardians. Goals included demonstrating the ability of lay counselors to learn and deliver the intervention, child/guardian participation and acceptance, and positive child outcomes.
Method
Participants
Children and guardians were identified by local community organizations (e.g., AIDS service organizations), asked to refer children with emotional difficulties that seemed to be associated with parental death. Child inclusion criteria were: a) 7–13 years old; b) residence in a family home; c) single or double orphan; d) age three or older when parent died; e) parental death at least six months prior; f) caregiver willingness to participate; and g) child and/or guardian report of at least mild symptoms of unresolved grief or PTS. Children younger than three at the time of parental death were not eligible as they might not have easy access to memories of the parent or the death. Those referred were visited at home after they gave permission for the organization to release contact information.
Procedures
Two focus groups were conducted. The adult group was comprised of ten local stakeholders from service organizations, faith-based groups, and HIV/AIDS treatment-providing groups. The adolescent group included ten youth, none of whom were recently orphaned and (to our knowledge) none were living with HIV/AIDS. There was a US-based group leader (R. Whetten), a Kiswahili translator, and a recorder. Questions focused on local standards for talking with children about death, how children and guardians handle grief, and possible challenges of talking about death in groups. Consensus was that the intervention would be acceptable and beneficial and that groups should be divided by sex and age (7–10; 11–13). Participants noted that caregivers often did not know how to help sad children, and children often were reluctant to broach topics related to death with their guardians.
Intervention
TF-CBT for CTG was adapted to be delivered in groups separated by child gender and age. The second author (S. Dorsey), a national TF-CBT trainer, adapted the TF-CBT for CTG protocol (Cohen, Mannarino, & Deblinger, 2006) to have 12 weekly group sessions (see Table 1) in collaboration with the trained lay counselors. Adaptation for group delivery followed guidelines from Deblinger, Stauffer, and Steer’s (2001) group-based TF-CBT with sexually abused children. Three individual visits, between groups four and seven, were added for the narrative creation following the Cognitive-Behavioral Intervention for Trauma in Schools model (Stein et al., 2003).
Table 1.
TF-CBT PRACTICE and Grief-Focused Components
| Session | Components (delivered in parallel, concurrent groups1) | Guardian Only |
|---|---|---|
| 1 | Psychoeducation: grief, trauma, and PTS | Parenting skills (PS): Praise |
| 2 | Relaxation; affective expression and modulation: strategies in relation to trauma cues | PS: Positive child-guardian time |
| 3 | Cognitive coping: Cognitive triad; Correcting maladaptive cognitions | PS: Effective instructions |
| 4 | Rationale for Trauma narration; Neutral narration (practice with a fun event beginning to end, with details, feelings, and thoughts) | |
| IS21 | 1:1 individual trauma narrative (TN) meeting separately with child and guardian | |
| 5 | TN review, each child individually (not in group format); Group relaxation activities; Preparation for conjoint TN sharing | PS: Rewards |
| IS2 | 1:1 individual TN | |
| 6 | TN review; Preparation for conjoin TN sharing | PS: Positive attention and ignoring; In vivo mastery: overcoming generalized trauma-related fears |
| IS3 | 1:1 individual TN | |
| 7 | TN review; Cognitive processing of trauma (common child thoughts) | |
| 8 | In vivo mastery; Conjoint child-guardian session3: Share child’s TN | |
| 9 | Acknowledge the death/what has been lost; Address ambivalent feelings in the relationship, as appropriate; In vivo mastery; Conjoint: Children share ambivalent feelings activity with the guardians | PS Review |
| 10 | Preserve positive memories; In vivo mastery; Conjoint: Share positive memories activity | |
| 11 | Develop new relationships: commit to ongoing positive relationships; In vivo mastery; Conjoint: Share relationships activity | |
| 12 | Enhancing Safety & Treatment closure: TF-CBT review and planning for future reminders |
60-minute groups for child and guardian, delivered separately and concurrently, covering common components and some guardian only components. Guardian-child conjoint activities where noted.
Individual Sessions (IS) conducted at the child’s home or a community space; approximately one hour.
Guardians came into children groups, sat with their individual child and engaged dyadically for approximately 20 minutes of the hour session. Guardians were prepared to normalize feelings and provide support and praise.
All TF-CBT components covered by the PRACTICE acronym were included: Psychoeducation, Parenting, Relaxation, Affective Modulation, Cognitive Coping, Trauma Narrative and Processing, In Vivo Exposure, and Enhancing Safety. The initial components build the foundation for understanding how loss affects children and teaching coping skills. Trauma Narrative and Processing facilitates children talking about distressing memories. The Trauma Narrative (TN) was created in individual sessions and then shared with the guardian. Children reviewed the TN during subsequent group sessions (groups five through seven) to support desensitization. During groups five through seven, the guardians discuss their own feelings and ways to support the children.
All sessions had the same elements: 1) refreshments; 2) a review of the previous group; 3) teaching new components (didactics and practice of skills); 4) a homework assignment; and 5) a preview of next group. Group sessions were one hour on Saturdays in community buildings. Each included eight children with a separate, concurrent group for guardians. Four groups were held in an urban location and four in rural Moshi. Individual sessions lasted approximately one hour. Guardians were provided with transportation costs.
Lay counselor and interviewer training, fidelity, and supervision
The two US-based investigators who conducted the training in Moshi are not fluent in Kiswahili; however, the four lay counselors were bilingual in Kiswahili and English. Three of the lay counselors had some university-level education; three had prior experience working with children; and none had mental health experience.
The counselors received an initial 10-day, in-person training (K. O’Donnell & S. Dorsey) focused on the TF-CBT protocol, education about grief, and counseling basics. Training included didactics and practice with coaching and feedback. Counselors then practiced with expert oversight (in-person; via Skype) for approximately one month. Two interviewers were also trained during this period. In-person supervision in Tanzania occurred on four additional occasions during the project.
Protocol fidelity was monitored closely, following procedures in prior LMIC RCTs (Bolton et al., 2003). Counselors completed weekly reports of fidelity for each group in report templates developed for this study, and recorded individual notes about each child and guardian. The first two authors reviewed reports prior to weekly supervision calls and discussed them in detail during the calls.
All study activities were approved by the Institutional Review Boards (IRBs) at Duke University, Kilimanjaro Christian Medical Center in Moshi, and the National Institute for Medical Research in Tanzania in Dares Salaam. Informed consent from the guardian and assent from the child included agreement to the screening for at least mild symptoms of grief and PTS and, then, for group participation. Measures, consent forms, and assent forms were translated and back-translated by bilingual native Kiswahili speakers. The study was designed with independent interviewers; but interviews for groups five and six were conducted by the counselors because of staffing shortages at the local collaborating agency (post hoc analyses involved testing whether interviewer [counselor vs. independent interviewer] affected outcomes; see Discussion).
Measures
The primary outcome measures for participating children were indicators of unresolved grief and PTS. Secondary aims addressed child depression and overall behavioral and emotional wellbeing.
Unresolved grief was assessed by child report only using the 10-item Grief Screening Scale (GSS; Layne, Pynoos, Savjak, & Steinberg, 1998). Responses are on a scale from 0 to 4 (None, Little, Some, Much, and Most). Layne et al. (2008) reported internal consistency (a = .86) for the GSS used in a school-based study with Bosnian adolescents. Eligibility for study inclusion was a cut-off score of 10 on the GSS.
Children (20 items) and guardians (21 items) were assessed for PTS using the UCLA Post Traumatic Stress Disorder-Reaction Index (UCLA PTSD-RI; Steinberg, Brymer, Decker, & Pynoos, 2004). International studies report inter-rater reliability and criterion-related validity with children in Zambia (Murray et al., 2011) and Somalia (Ellis, Lhewa, Charney, & Cabral, 2006), showing convergent validity with the Depression Self-Rating Scale (r = .72, p < .001) and the War Trauma Screening Scale (r = .59, p < .001). Findings demonstrated internal consistency in the Somalia study (a = 0.85; Ellis et al., 2006). Items are rated on a Likert scale from 0–4 (None, Little, Some, Much, and Most). Eligibility for the study was identified by a cutoff total score of 15 as an indicator of at least mild symptoms as reported by child or guardian.
The 20-item Strengths and Difficulties Questionnaire (SDQ; Goodman, 1997) was used to indicate child behavioral and emotional wellbeing and difficulties via guardian report; child self-report is limited to age 11 and older, so it was not used. Responses are rated as Not True, Somewhat True, and Certainly True. The SDQ is used in many international studies and translated into 43 languages. It compares well with the Child Behavior Checklist (Achenbach, 1991; Goodman & Scott, 1999). Investigations of psychometric properties indicate internal consistency (a = .73; Goodman, 2001).
The Short Mood and Feelings Questionnaire (SMFQ; Angold et al., 1995) is a 13-item screening tool for child depression with child and caregiver versions. Scores are scaled True, Sometimes True, and Not True. The investigators demonstrated that a single depression factor explained SMFQ item inter-correlations (Messer et al., 1995). Criterion-related validity was shown using the Childhood Depression Inventory (Kovacs, 1992) and the Schedule for Affective Disorders and Schizophrenia (Ambrosini, 2000), among others.
Data Analysis
The internal consistency of translated measures was assessed using Cronbach’s alpha (Cronbach, 1951). Bivariate analyses tested for baseline differences in outcome variables by child sex, younger versus older groups, and urban versus rural setting. Mixed-effects linear regression models were used to assess changes from baseline to subsequent assessments. Models were estimated with random intercepts for each child to account for time-invariant differences between children; children were nested within groups. Parameter estimates on indicator variables for each follow-up were used to describe the magnitude of change relative to baseline. Regression analyses controlled for child age and sex, rural versus urban setting, months since last parent death, caregiver sex, orphan status, relationship to caregiver, and the baseline value for the outcome of interest. Joint F-tests on interactions between follow-up assessment time-point and group-membership assessed group-level differences in outcome changes over time. Effect sizes for the two primary outcomes were calculated using Cohen’s d. All analyses were conducted using STATA 13.1 (Stata Statistical Software, Release 13).
Results
Internal Consistency
Internal consistency was tested for the measures translated into Kiswahili. The internal consistency for the PTSD-RI was “acceptable” for the child self-report (a =.70) and for the guardian report (a = .81). For the GSS, a = .62, “questionable”. For SDQ (a =.78), and with SMFQ (a = 0.75 for guardian report; a = 0.80 for child self-report) internal consistency was deemed acceptable.
Participants
Seventy-four children were referred and screened; nine did not meet the clinical eligibility, and one guardian declined participation. Children (N = 64) were 6.9 to 13.7 years old. ). Group assignment unpredictably resulted in the inclusion of one child less than 7 years and one 11-year-old in the younger group. Children in the younger groups were 6.9 to 11.3 years old (M = 9.3, SD = 1.2), and the older group ranged from 11.0 to 13.7 years old (M = 12.2, SD = 0.8). Guardian participants were over 90% female, predominantly mothers or grandmothers (see Table 2). Nearly 40% of the children were living with one biological parent, and one-fourth were double orphans.
Table 2.
Description of study participants
| N | % | |
|---|---|---|
| Total child and guardian dyads | 64 | 100.0 |
| Guardian | ||
|
| ||
| Gender | ||
| Male | 6 | 9.4 |
| Female | 58 | 90.6 |
| Relationship to child | ||
| Biological mother | 21 | 32.8 |
| Biological father | 2 | 3.1 |
| Grandparent | 25 | 39.1 |
| Aunt/uncle | 11 | 17.2 |
| Other relative | 4 | 6.3 |
| Not related | 1 | 1.6 |
| Child | ||
|
| ||
| Gender | ||
| Male | 32 | 50.0 |
| Female | 32 | 50.0 |
| Orphan status | ||
| One parent died, living with biological parent | 28 | 43.8 |
| One parent died, not living with biological parent | 21 | 32.8 |
| Both parents died | 15 | 23.4 |
Study attrition was low. One guardian who replaced an original guardian declined to continue following the end of treatment interview, and there was one loss to follow-up after the 3-month post-treatment interview. There were no dropouts during the intervention; weekly attendance was over 95%.
Screening and Baseline Assessments
Ninety-seven percent of the referred children reached the cut-off score of 10 on the GSS (range: 4–29, Mdn = 19.5). Ninety-five percent met the eligibility cut-off of 15 for child report on the PTSD-RI (range: 10–52, Mdn = 24.7), and 63% met eligibility by guardian report (range: 0–46, Mdn = 18.5). Ninety-two percent were eligible using cut-off scores on both.
Table 3 shows the clinical outcomes data at pre-treatment end of treatment, and at 3- and 12-months after end of treatment. Bivariate analyses are presented in Table 4. Younger children had higher PTS (t = 2.15; p = .036) and depression (t = 3.66; p < .001) by child report and greater overall difficulties by guardian report (t = 2.15; p = .036). Children living in urban areas had significantly higher PTS and depression as reported by children and guardians (all p < .04), and lower overall wellbeing (SDQ) reported by guardians (t = −2.11; p = .039). There were no baseline differences for males versus females
Table 3.
Symptom Scores at Baseline, End of Treatment, and at 3- and 12-Month Follow-Up after End of Treatment
| Baseline | End of treatment | 3-month follow-up | 12-month follow-up | ||
|---|---|---|---|---|---|
| UCLA Posttraumatic Stress Disorder - Reaction Index: Total | |||||
| Guardian | N | 62 | 60 | 62 | 61 |
| Mean (sd) | 19.6 (10.8) | 7.8 (8.2) | 6.4 (7.3) | 4.9 (7.7) | |
| Child | N | 64 | 64 | 63 | 61 |
| Mean (sd) | 26.1 (9.1) | 10.2 (9.2) | 7.8 (7.5) | 5.1 (5.5) | |
| Strengths and Difficulties Questionnaire (SDQ): Total Difficulties | |||||
| Guardian | N | 64 | 64 | 63 | 61 |
| Mean (sd) | 11.9 (6.5) | 7.0 (5.9) | 6.6 (5.2) | 4.8 (4.2) | |
| Grief Screening Scale (GSS): Total | |||||
| Child | N | 64 | 64 | 63 | 61 |
| Mean (sd) | 19.5 (5.5) | 11.3 (4.9) | 10.0 (4.9) | 8.0 (3.8) | |
| Short Moods and Feelings Questionnaire (SMFQ): Total | |||||
| Guardian | N | 64 | 64 | 63 | 61 |
| Mean (sd) | 5.4 (4.1) | 2.0 (3.8) | 2.3 (3.5) | 1.1 (3.1) | |
| Child | N | 64 | 63 | 63 | 61 |
| Mean (sd) | 9.2 (5.9) | 2.9 (4.5) | 1.4 (2.9) | 1.0 (2.1) | |
| Range | [0; 24.0] | [0; 20.0] | [0; 13.0] | [0; 13.0] | |
SD – Standard deviation
Table 4.
Bivariate analyses of baseline (pre-treatment) measures
| Younger | Older | Females | Males | Rural | Urban | ||
|---|---|---|---|---|---|---|---|
| UCLA Posttraumatic Stress Disorder – Reaction Index (UCLA PTSD – RI): Total symptoms score | |||||||
| Guardian report | n | 31 | 31 | 31 | 31 | 32 | 30 |
| M (SD) | 21.7 (12.7) | 17.6 (8.3) | 17.6 (11.4) | 21.6 (10.0) | 16.9 (9.6) | 22.5 (11.5)* | |
| Child report | n | 32 | 32 | 32 | 32 | 32 | 32 |
| M (SD) | 28.5 (10.1) | 23.8 (7.3)* | 25.4 (8.7) | 26.8 (9.5) | 23.8 (6.3) | 28.5 (10.7)* | |
|
| |||||||
| Strengths and Difficulties Questionnaire (SDQ): Total Difficulties score | |||||||
| Guardian report | n | 32 | 32 | 32 | 32 | 32 | 32 |
| M (SD) | 13.6 (6.6) | 10.2 (5.9)* | 11.5 (7.4) | 12.3 (5.4) | 10.0 (6.2) | 13.8 (6.2)* | |
|
| |||||||
| Grief Screening Scale (GSS): Total score | |||||||
| Child report | n | 32 | 32 | 32 | 32 | 32 | 32 |
| M (SD) | 20.6 (5.3) | 18.4 (5.5) | 18.6 (5.5) | 20.4 (5. 4) | 18.4 (6.0) | 20.6 (4.7) | |
|
| |||||||
| Short Moods and Feelings Questionnaire (SMFQ): Total score | |||||||
| Guardian report | n | 32 | 32 | 32 | 32 | 32 | 32 |
| M (SD) | 5.5 (3.6) | 5.3 (4.5) | 5.4 (3.7) | 5.4 (4.5) | 4.3 (3.5) | 6.4 (4.4)* | |
| Child report | n | 32 | 32 | 32 | 32 | 32 | 32 |
| M (SD) | 11.6 (5.7) | 6.7 (5.0)** | 9.5 (6.7) | 8.9 (4.9) | 7.6 (5.3) | 10.8 (6.0)* | |
Note:
p < .05;
p< .001
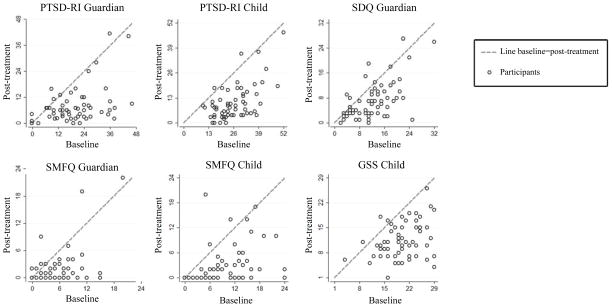
Outcome Analyses
Children had reduced symptoms on all measures by the end of treatment, with improvements sustained at 3- and 12-months (all p < .001; see Table 5). The same p-values were observed when mixed models were analyzed with children nested in groups; intraclass correlations were low, ranging from 0.006 to 0.229, thus we present findings from the parsimonious, disaggregated models. Change scores from baseline to end of treatment are shown in Figure 1; a point along the 45° line indicates no change, a point below shows the reduction in that score. Greater distance from the line indicates a greater change. The magnitude of symptom change did not differ systematically with child age or sex. Children with more symptoms reported by self or guardian at baseline showed greater improvement by the end of treatment (for all measures p < .001, except the guardian report on SMFQ at end of treatment (p = 0.028).
Table 5.
Estimated changes in symptoms scores relative to baseline
| End of treatment | 3-month follow-up | 12-month follow-up | ||
|---|---|---|---|---|
| UCLA Post Traumatic Stress Disorder Reaction Index: Total symptoms score | ||||
| Guardian | b | −11.24*** | −12.73*** | −14.42*** |
| se | (1.213) | (1.435) | (1.558) | |
| Child | b | −15.68*** | −17.91*** | −20.78*** |
| se | (1.018) | (1.496) | (1.908) | |
|
| ||||
| Strengths and Difficulties Questionnaire (SDQ): Total Difficulties score | ||||
| Guardian | b | −4.84*** | −5.00*** | −6.69*** |
| se | (0.568) | (0.705) | (0.754) | |
|
| ||||
| Grief Screening Scale: Total score | ||||
| Child | b | −7.92*** | −9.36*** | −11.36*** |
| se | (0.909) | (1.001) | (0.821) | |
|
| ||||
| Short Moods and Feelings Questionnaire (SMFQ): Total score | ||||
| Guardian | b | −3.33*** | −3.03*** | −4.15*** |
| se | (0.365) | (0.379) | (0.422) | |
| Child | b | −5.79*** | −7.33*** | −7.84*** |
| se | (0.679) | (0.983) | (0.871) | |
significance at the p< .001 level
Regression analyses were controlled for child age and sex, rural versus urban setting, months since last parent death, caregiver sex, orphan status, relationship to caregiver, and the baseline value for outcome of interest.
Figure 1.
Scatterplots comparing baseline and post-treatment the Posttraumatic Stress Disorder Reaction-Index (PTSD-RI), the Strengths and Difficulties Questionaire (SDQ), the Short Mood and Feelings Questionaire (SMFQ), and the Grief Screening Scale (GSS) scores for guardian and child participants
Effect sizes (Cohen’s d) were calculated for the primary outcomes from baseline to end of treatment. The effect size for child reported symptoms of grief was 1.36. Children improved on self-reported PTS (d = 1.87) and on the guardian report of child PTS (d = 1.15).
Discussion
This report describes an open trial of TF-CBT for children with unresolved grief and PTS. Minimal adaptation of the TF-CBT for CTG model consisted of developing a group protocol with individual TN sessions, and using local examples and analogies. These findings are consistent with previous reports that only limited modification is needed for EBT from HIC to be feasible in LMIC (e.g., Murray et al., 2013, Patel et al., 2011).
Participating children were at least mildly symptomatic with 92% meeting the cut-off scores for both unresolved grief and PTS. Of note, children were referred for being symptomatic, so these data do not represent the general population. Both children and guardians reported improved child symptoms at the end of treatment and at the post-treatment follow-ups. The reduction in PTS is similar to two other studies of TF-CBT in sub-Saharan Africa (Murray et al., 2013; O’Callaghan et al., 2013). The post hoc analyses of possible differences in outcome scores by interviewers (versus counselors) found no differences. Children with more symptoms at baseline showed the most improvement, which may have been, in part, due to floor effects on the measures or regression to the mean.
The counselors delivered the intervention with high fidelity, per qualitative assessment, despite having limited prior mental health experience. These findings are consistent with other work with trained lay counselors (Patel et al., 2011).
The study has limitations. It was uncontrolled, prohibiting attributing positive findings to the intervention alone. Improvements may reflect natural symptom progression over time. The follow-up interviews for groups five and six, conducted by counselors, might have been biased by social desirability. Despite analyses suggesting no differences by interviewer, the independence of counselors and interviewers is critical. Other possible mediators of change, such as the guardian-child relationship, guardian mental health status and change with treatment, tribe, religion, and guardian HIV status were not examined. Finally, the effect of the nature of parental death could not be examined because these data were not collected; the actual cause of the death is often not known or not reported accurately due to stigma.
Our team is currently conducting a RCT of TF-CBT for symptomatic orphaned children in Tanzania and Kenya (NIMH R01 MH96633;Whetten & Dorsey, MPIs) that utilizes the feasibility study counselors as local supervisors of newly trained lay counselors, hopefully leading to even greater local capacity and ownership.
Acknowledgments
The study was funded by the National Institutes of Health (Whetten, K.: R34MH081764).
We are very grateful for the counselors and interviewers who brought this treatment model to their community with grace and competence: Bibiana Gali, Leonia Rugalabamu, Luililiaeli Mfangavo, Simon Joseph, and Suzan Kitomari. We are also thankful to Karthik Balasubramanian for all of his assistance in coordinating the project.
Contributor Information
Karen O’Donnell, The Center for Child and Family Health, Duke University.
Shannon Dorsey, University of Washington.
Wenfeng Gong, Johns Hopkins University.
Jan Ostermann, Duke University.
Rachel Whetten, Duke University.
Judith A. Cohen, Drexel University College of Medicine
Dafrosa Itemba, Tanzania Women’s Research Foundation.
Rachel Manongi, Kilimanjaro Christian Medical Center.
Kathryn Whetten, Duke University.
References
- Achenbach TM. Manual for the child behavior checklist/4–18 and 1991 profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1991. [Google Scholar]
- Ambrosini PJ. Historical development and present status of the Schedule for Affective Disorders and Schizophrenia for school-age children (K-SADS) Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39(1):49–58. doi: 10.1097/00004583-200001000-00016. [DOI] [PubMed] [Google Scholar]
- Andrews G, Skinner D, Zuma K. Epidemiology of health and vulnerability among children orphaned and made vulnerable by HIV/AIDS in sub-Saharan Africa. AIDS Care. 2006;18(3):269–276. doi: 10.1080/09540120500471861. [DOI] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research. 1995;5:237–249. Retrieved from http://devepi.duhs.duke.edu/AngoldMFQarticle.pdf. [Google Scholar]
- Atwine B, Cantor-Graae E, Bajunirwe F. Psychological distress among AIDS orphans in rural Uganda. Social Science & Medicine. 2005;61(3):555–564. doi: 10.1016/j.socscimed.2004.12.018. [DOI] [PubMed] [Google Scholar]
- Bass JK, Annan J, McIvor Murray S, Kaysen D, Griffiths S, Cetinoglu T, Bolton PA. Controlled trial of psychotherapy for Congolese survivors of sexual violence. New England Journal of Medicine. 2013;368(23):2182–2191. doi: 10.1056/NEJMoa1211853. [DOI] [PubMed] [Google Scholar]
- Bolton P, Bass J, Neugebauer R, Verdeli H, Clougherty KF, Wickramaratne P, Weissman M. Group interpersonal psychotherapy for depression in rural Uganda: A randomized controlled trial. Journal of the American Medical Association. 2003;289(23):3117–3124. doi: 10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Deblinger E. Treating trauma and traumatic grief in children and adolescents. New York, NY: Guilford Press; 2006. [Google Scholar]
- Cohen JA, Mannarino AP, Greenberg T, Padlo S, Shipley C. Childhood traumatic grief: Concepts and controversies. Trauma, Violence, & Abuse. 2002;3(4):307–327. doi: 10.1177/1524838002237332. [DOI] [Google Scholar]
- Cohen JA, Mannarino AP, Knudsen K. Treating childhood traumatic grief: A pilot study. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(10):1225–1233. doi: 10.1097/01.chi.0000135620.15522.38. [DOI] [PubMed] [Google Scholar]
- Cohen JA, Mannarino AP, Staron VR. A pilot study of modified Cognitive Behavioral Therapy for Childhood Traumatic Grief (CBT-CTG) Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(12):1465–1473. doi: 10.1097/01.chi.0000237705.43260.2c. [DOI] [PubMed] [Google Scholar]
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16(3):297–334. Retrieved from http://psych.colorado.edu/~carey/courses/psyc5112/readings/alpha_cronbach.pdf. [Google Scholar]
- Deblinger E, Stauffer LB, Steer RA. Comparative efficacies of supportive and cognitive behavioral group therapies for young children who have been sexually abused and their non-offending mothers. Child Maltreatment. 2001;6(4):332–343. doi: 10.1177/1077559501006004006. [DOI] [PubMed] [Google Scholar]
- Dorsey S, Briggs EC, Woods BA. Cognitive Behavioral Treatment for Posttrau-matic Stress Disorder in children and adolescents. Child and Adolescent Psychiatric Clinics of North America. 2011;20(2):255–269. doi: 10.1016/j.chc.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis HB, Lhewa D, Charney M, Cabral H. Screening for PTSD among Somali adolescent refugees: Psychometric properties of the UCLA PTSD Index. Journal of Traumatic Stress. 2006;19(4):547–551. doi: 10.1002/jts.20139. [DOI] [PubMed] [Google Scholar]
- Goodman R. The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology & Psychiatry. 1997;38(5):581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman R, Scott S. Comparing the Strengths and Difficulties Questionnaire and the Child Behavior Checklist: Is small beautiful? Journal of Abnormal Child Psychology. 1999;27(1):17–24. doi: 10.1023/A:1022658222914. [DOI] [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the Strengths and Difficulties Questionnaire (SDQ) Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS) Global report: UNAIDS report on the global AIDS epidemic. Geneva, Switzerland: 2012. Retrieved from http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/20121120_UNAIDS_Global_Report_2012_with_annexes_en.pdf. [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS), United Nations Children’s Fund (UNICEF), & U.S. Agency for International Development. Children on the brink 2004: A joint report of new orphan estimates and a framework for action. New York, NY: UNICEF; 2004. (Contract No. HRN-C-00-00-0004-00) Retrieved from http://www.unicef.org/publications/cob_layout6-013.pdf. [Google Scholar]
- Kaplow J, Howell K, Layne C. Do circumstances of the death matter? Identifying socioenvironmental risks for grief-related psychopathology in bereaved youth. Journal of Traumatic Stress. 2014;27(1):42–49. doi: 10.1002/jts.21877. [DOI] [PubMed] [Google Scholar]
- Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, Rahman A. Child and adolescent mental health worldwide: Evidence for action. The Lancet. 2011;378(9801):1515–1525. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory (CDI) New York: Multi-health Systems, Inc; 1992. [Google Scholar]
- Layne CM, Saltzman WR, Poppleton L, Burlingame GM, Pašalić A, Duraković E, Pynoos RS. Effectiveness of a school-based group psychotherapy program for war-exposed adolescents: A randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(9):1048–1062. doi: 10.1097/CHI.0b013e31817eecae. [DOI] [PubMed] [Google Scholar]
- Layne CM, Pynoos RS, Savjak N, Steinberg A. Grief Screening Scale. Unpublished measure. Los Angeles, CA: University of California, Los Angeles; 1998. [Google Scholar]
- Maercker A, Lalor J. Diagnostic and clinical considerations in prolonged grief disorder. Dialogues in Clinical Neuroscience. 2012;14(2):167–176. doi: 10.31887/DCNS.2012.14.2/amaercker. Retrieved from http://www.dialogues-cns.org/wp-content/uploads/2012/06/DialoguesClinNeurosci-14-167.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melhem NM, Moritz G, Walker M, Shear MK, Brent D. Phenomenology and correlates of complicated grief in children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46(4):493–499. doi: 10.1097/chi.0b013e31803062a9. [DOI] [PubMed] [Google Scholar]
- Messer SC, Angold A, Costello EJ, Loeber R, van Kammen W, Stouthamer-Loeber M. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents: Factor composition and structure across development. International Journal of Methods in Psychiatric Research. 1995;5:251–262. Retrieved from http://devepi.duhs.duke.edu/MesserMFQarticle.pdf. [Google Scholar]
- Murray LK, Bass J, Chomba E, Imasiku M, Thea D, Semrau K, Bolton P. Validation of the UCLA Child Post Traumatic Stress Disorder–Reaction Index in Zambia. International Journal of Mental Health Systems. 2011;5(24):1–13. doi: 10.1186/1752-4458-5-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray LK, Familiar I, Skavenski S, Jere E, Cohen J, Imasiku M, Bolton P. An evaluation of trauma focused cognitive behavioral therapy for children in Zambia. Child Abuse & Neglect. 2013;37(12):1175–1185. doi: 10.1016/j.chiabu.2013.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nader L, Layne C. Maladaptive grieving in children and adolescents: Discovering developmentally linked differences in the manifestation of grief. Stress Points. 2009;23(5):12–15. [Google Scholar]
- O’Callaghan P, McMullen J, Shannon C, Rafferty H, Black A. A randomized controlled trial of Trauma-Focused Cognitive Behavioral Therapy for sexually exploited, war-affected Congolese girls. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(4):359–369. doi: 10.1016/j.jaac.2013.01.013. [DOI] [PubMed] [Google Scholar]
- O’Donnell K, Nyangara F, Murphy R, Nyberg B. Child Status Index Manual. 2. Chapel Hill, NC: Measure Evaluation; 2013. [Google Scholar]
- Patel V, Chowdhary N, Rahman A, Verdeli H. Improving access to psychological treatments: Lessons from developing countries. Behaviour Research & Therapy. 2011;49(9):523–528. doi: 10.1016/j.brat.2011.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V, Flisher AJ, Nikapota A, Malhotra S. Promoting child and adolescent mental health in low and middle income countries. Journal of Child Psychology & Psychiatry. 2008;49(3):313–334. doi: 10.1111/j.1469-7610.2007.01824.x. [DOI] [PubMed] [Google Scholar]
- Patel V, Weiss HA, Chowdhary N, Naik S, Pednekar S, Chatterjee S, Kirkwood BR. Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa, India (MANAS): A cluster randomised controlled trial. The Lancet. 2010;376(9758):2086–2095. doi: 10.1016/S0140-6736(10)61508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A, Malik A, Sikander S, Roberts C, Creed F. Cognitive behaviour therapy-based intervention by community health workers for mothers with depression and their infants in rural Pakistan: A cluster-randomised controlled trial. The Lancet. 2008;372(9642):902–909. doi: 10.1016/S0140-6736(08)61400-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Weiss R, Alber S, Lester P. Adolescent adjustment before and after HIV-related parental death. Journal of Consulting & Clinical Psychology. 2005;73(2):221–228. doi: 10.1037/0022-006X.73.2.221. [DOI] [PubMed] [Google Scholar]
- Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: Scarcity, inequity, and inefficiency. The Lancet. 2007;370(9590):878–889. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- Stein BD, Jaycox LH, Kataoka SH, Wong M, Tu W, Elliott MN, Fink A. A mental health intervention for schoolchildren exposed to violence: A randomized controlled trial. Journal of the American Medical Association. 2003;290(5):603–611. doi: 10.1001/jama.290.5.603. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The University of California at Los Angeles Post-traumatic Stress Disorder Reaction Index. Current Psychiatry Reports. 2004;6(2):96–100. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- Tol WA, Barbui C, van Ommeren M. Management of acute stress, PTSD, and bereavement: WHO recommendations. Journal of the American Medical Association. 2013;310(5):477–478. doi: 10.1001/jama.2013.166723. [DOI] [PubMed] [Google Scholar]
- Whetten K, Ostermann J, Whetten R, O’Donnell K, Thielman N the Positive Outcomes for Orphans Research Team. More than the loss of a parent: Potentially traumatic events among orphaned and abandoned children. Journal of Traumatic Stress. 2011;24(2):174–182. doi: 10.1002/ts.20625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Task shifting to tackle health worker shortages. Geneva, Switzerland: WHO; 2007. Retrieved from www.who.int/healthsystems/task_shifting_booklet.pdf. [Google Scholar]
- World Health Organization. Guidelines for the management of conditions specifically related to stress. Geneva, Switzerland: WHO; 2013. Retrieved from http://apps.who.int/iris/bitstream/10665/85119/1/9789241505406_eng.pdf. [PubMed] [Google Scholar]