Abstract
Plague, an often-fatal zoonotic disease caused by Yersinia pestis, is characterized by epizootic and quiescent periods. How Y. pestis is maintained during inter-epizootic periods is poorly understood, but soil has been implicated as a potential reservoir. Although previous studies have suggested that Y. pestis is able to survive in soil for weeks or months, it is unclear whether or not it is infectious to susceptible hosts. Here we investigate the potential for Y. pestis to infect mice through close contact with contaminated soil under laboratory conditions. In an attempt to approximate the natural conditions under which animals would be exposed to Y. pestis-contaminated soil, mouse cages filled with soil from a plague-endemic region were held at temperature and humidity ranges observed in ground squirrel burrows. These laboratory “burrows” were contaminated with highly bacteremic blood (> 108 cfu/mL) to simulate the introduction of infectious material from a dying animal during an epizootic. Outbred Swiss-Webster mice with scarified skin patches were held on contaminated soil for 10 days and monitored for signs of illness. Following exposure to contaminated soil, one animal of 104 became infected with Y. pestis. None of the remaining animals seroconverted following a 21-day holding period. Under our experimental conditions, which maximized the likelihood of contact between susceptible mice and contaminated soil, transmission efficiency from soil to mice was 0.96% (95% CI 0.17, 5.25%). This suggests that although transmission of Y. pestis from contaminated soils is possible, it is not likely a major transmission route under natural conditions.
Keywords: Plague, Soil, Transmission, Yersinia pestis.
Introduction
Plague is a rodent-associated zoonotic disease caused by the gram-negative bacterium Yersinia pestis (Gage and Kosoy 2005). Although plague is most commonly transmitted through the bite of infected fleas, other routes of infection are possible, including cutaneous or oral exposure, and inhalation of infectious droplets (Poland and Dennis 1999). Plague epizootics, or periods of rapid transmission, occur sporadically, but how plague bacteria are maintained during quiescent or inter-epizootic periods is poorly understood. Nonetheless, researchers have proposed several mechanisms (Eisen and Gage 2009). These include the existence of low-level transmission of plague bacteria among enzootic hosts and their fleas (Pollitzer and Meyer 1961; Gage and Kosoy 2005), hibernation of Y. pestis-infected rodent hosts (Bizanov and Dobrokhotova 2007), and survival in fleas or their feces (Bazanova et al. 1997, 2007). Others have proposed that soil may serve as a reservoir of Y. pestis (Baltazard et al. 1963; Mollaret 1963; Drancourt et al. 2006; Ayyadurai et al. 2008). According to this controversial but long-standing hypothesis, it is thought that hosts that have died of plague infection, particularly during epizootics, may contaminate soil; the bacteria may survive for many months in the soil and remain infectious to susceptible hosts.
Evidence that Y. pestis may persist in soil was first presented by Yersin (1894), who claimed to have recovered an isolate from the floors of a mud hut where humans had died of plague. More recent studies have described the ability of Y. pestis to survive for many months in both live and autoclaved soils (Mollaret 1963; Ayyadurai et al. 2008), and for at least 3 weeks under field conditions (Eisen et al. 2008). Karimi (1963) demonstrated that contaminated soil contained viable plague bacteria for up to 11 months after animals died of plague in the protected environment of rodent burrows. In each of these studies, animals were needle inoculated with Y. pestis-contaminated soil to demonstrate infectiousness. Therefore, while these studies suggest that Y. pestis may remain viable and virulent for weeks or months in soil, they do not address whether contaminated soil can be infectious to susceptible hosts through natural contact.
Results from early transmission experiments of the Indian Plague Research Commission (1906) showed that mud floors heavily contaminated with Y. pestis cultures were infectious to guinea pigs up to 12 h post-contamination. The researchers noted, however, that transmission ceased once the floors were no longer moist with culture. This suggests that infectiousness of contaminated soil was only transient. In a similar experiment, Mollaret and associates (1963) exposed burrowing and non-burrowing animals to soil contaminated either “weakly” or “heavily” with Y. pestis culture, observing transmission to burrowing jirds (Meriones vinogradovi) and white mice under both conditions, while transmission to non-burrowing guinea pigs and white rats was observed only following exposure to more heavily contaminated soil. Although this study demonstrated that contaminated soil could be infectious through natural modes of exposure, the amounts of bacteria used to contaminate the soil were poorly defined, and it is unclear if transmissible levels were within a biologically-plausible range.
Here we investigate the potential for Y. pestis-contaminated soil to infect susceptible hosts through natural routes of exposure within a simulated burrow environment. In order to maximize the potential for transmission from contaminated soil, we attempted to mimic the conditions in rodent burrows that might play a role in the survival and transmission of Y. pestis from soil (e.g., maintaining temperature and relative humidity within the range observed in rodent burrows, and the use of live [non-sterilized] soil collected from prairie dog burrows that recently experienced plague epizootics). Plague-susceptible outbred mice were allowed natural contact with Y. pestis-contaminated live soil, and efforts were made to maximize the likelihood of transmission via cutaneous, oral, and respiratory routes.
Materials and Methods
Species and strains of bacteria and mice
A fully virulent North American strain of Y. pestis (biovar Orientalis), designated CO96-3188 (Pgm +, pMT1 +, pCD1 + ), was used to contaminate field-collected soil. Plague bacteria were grown overnight in heart infusion broth (BD Biosciences, Franklin Lakes, NJ) on a shaking incubator at 37°C and 250 rpm. The culture was then pelleted by centrifugation at 1800g, washed with 0.85% sterile saline, and resuspended in Sprague-Dawley strain defibrinated rat blood (Bioreclamation, Jericho, NY), to a final concentration of 108–109 cfu/mL. This range of bacteremia reflects terminal bacterial loads observed in hosts (Sebbane et al. 2005), and maximizes the likelihood of contact between sentinel mice and bacteria in the contaminated soil. Blood was held at 37°C before and after the addition of Y. pestis and until use. A 100-μL aliquot of this suspension was serially diluted in saline and plated in duplicate onto 6% sheep blood agar (Centers for Disease Control and Prevention, Atlanta, GA) to determine bacterial concentrations for each replicate. The plates were incubated at 28°C for 48 h prior to enumeration of colony-forming units (cfu).
A total of 104 6- to 8-week-old female CD-1 mice obtained from a specific pathogen-free colony maintained at the Division of Vector-Borne Diseases, CDC (Fort Collins, CO) were used as sentinels. To maximize the likelihood of percutaneous exposure to Y. pestis in the contaminated soil and to simulate natural conditions under which small mammals often have abrasions on their skin, the mice were scarified as described by Taylor and colleagues (1996). The mice were sedated by IP injection with ketamine (75 mg/kg) and dexmedetomidine (0.5 mg/kg), and a 1-cm2 area on the lateral surface of the thigh was shaven and superficially abraded using the tip of a needle (26G, 5/8”) to create a cross-hatched pattern on the skin. Following the scarification procedure, atipamezole was administered IP (5.0 mg/ kg) to reverse the effects of the dexmedetomidine (Hahn 2005).
Animal housing and soil
Experimental soil cages were designed to maximize interactions between sentinel mice and Y. pestis-contaminated soil. Soil was collected on two sampling dates in January and March 2011, from an active prairie dog colony within the Cathy Fromme Prairie (Fort Collins, CO). Routine surveillance of these colonies by Fort Collins Natural Areas staff revealed that the sampled colony experiences plague epizootics frequently, with the most recent epizootic documented in May 2009. A total of 52 individual samples were collected from a depth of 0.3–1.0 meter at random points within the boundaries of the colony using a gas-powered handheld hole digger (General Equipment Co., Owatonna, MN). Individual soil samples were collected in gallon-sized plastic bags, and were then transported and stored at room temperature for up to 2 weeks until use.
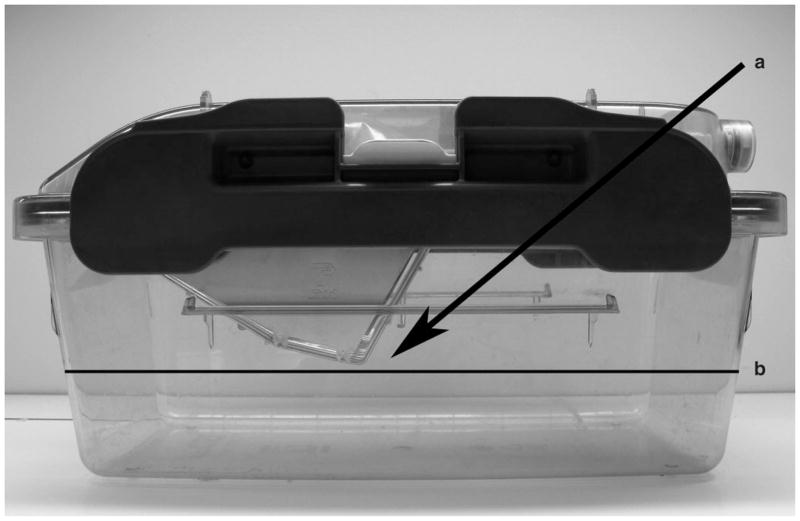
To construct soil cages, the individual soil samples were mixed together in large plastic tubs until homogeneous. Approximately 3 kg of this soil was added to each of 52 Isocage mouse cages with micro-isolator tops (Tecniplast, Exton, PA). Enough soil was added to contact the bottom of the wire food rack in each cage (Fig. 1). Soil at this depth formed a barrier beneath the wire food rack where 108–109 cfu of Y. pestis suspended in 1 mL of rat blood was added to the surface of the soil. Food was placed on the surface of the soil on both sides of the barrier, both to encourage animals to burrow through the Y. pestis-contaminated area, and to expose animals to potentially infectious soil during feeding. During a pilot study of this cage design, mice dug and burrowed in this area within hours of being placed in the cages (Centers for Disease Control and Prevention, Division of Vector Borne Diseases Animal Care and Use Protocol 08-006).
FIG. 1.
Soil cage construction, showing soil fill line (b). Infectious blood spike was added in a line beneath the wire food rack (a).
Environmental conditions within the soil cages were designed to mimic those of rodent burrows because carcasses of animals naturally infected with Y. pestis might contaminate soil in these structures during an epizootic. Baudinette (1972) reported that relative humidity and temperature readings ranged between 68 and 95% and 15 and 27°C within ground squirrel burrows. These target ranges for temperature and relative humidity within the experimental soil cages were maintained through facility controls, the use of room humidifiers, and the addition of water to the surface of soil within each cage. During the initial assembly of each cage, 60 mL of deionized water was added per kilogram of soil. To maintain initial soil moisture, the cages were kept closed and were not placed on the Isocage ventilation rack until after the soil was contaminated with Y. pestis-infected blood and sentinel mice had been added as described below. For the next 10 days, on alternate days the cages were opened and the soil was humidified by the addition of 100 mL of deionized water dispersed by a handheld mister (Zoo Med, San Luis Obispo, CA). Temperature and relative humidity values within each cage were recorded using a HOBO Data Logger (Onset, Pocasset, MA) at hourly intervals until day 11 post-contamination.
Immediately following recovery from anesthesia, two scarified mice were added to each cage (n = 52 cages total) within 4–8 h of the addition of Y. pestis-spiked blood. Scarified sentinel animals were then held for 10 days in Isocages containing contaminated soil, and observed for signs of illness (e.g., hunched posture, slow response to stimulus, or ruffled fur). Animals showing signs of infection following introduction to experimental cages were euthanized in accordance with international animal care and use committee guidelines (Centers for Disease Control and Prevention, Division of Vector Borne Diseases Animal Care and Use Protocol 09-010), and liver and spleen samples were collected at necropsy. At 11 days post-contamination, the remaining animals were transferred from soil cages to Isocages with standard bedding and held for at least 21 days to monitor for seroconversion. Between days 31 and 35 post-contamination, the animals were bled by cardiac puncture under anesthesia and euthanized. Blood serum was collected by centrifugation, and stored at −20°C until serological testing was performed.
Evidence that mice were infected with Y. pestis through contact with contaminated soil
Liver and spleen tissues collected from animals showing signs of illness were tested for the Y. pestis-specific Fraction 1 (F1) antigen using a direct fluorescent antibody assay and examined by fluorescence microscopy. Infection was confirmed by culture isolation followed by a Y. pestis-specific bacteriophage lysis assay (Chu 2000). To confirm that the source of infection was Y. pestis-spiked blood, rather than a strain that persisted in the field-collected live (non-sterilized) soil, mouse culture isolates and the strain used to generate the blood spike were compared using pulsed-field gel electrophoresis (PFGE) typing with Asc1 following a standard PulseNet protocol (Centers for Disease Control and Prevention for PulseNet USA 2006). Blood serum collected from asymptomatic animals between days 31 and 35 post-contamination was tested for the presence of Y. pestis-specific antibody by a passive hemagglutination inhibition test. Any sample showing a positive result at a titer of 1:16 or greater was considered positive (Chu 2000).
To demonstrate that Y. pestis can remain viable for at least 10 days (the length of time the mice were exposed to blood-contaminated soil) in a blood substrate alone, blood was spiked with Y. pestis as described above. Aliquots of this Y. pestis-spiked blood were maintained at room temperature in 1.5-mL microcentrifuge tubes, and then plated in duplicate on 6% SBA plates each day for 10 days to determine the concentration of viable bacteria at each time point.
Data analysis
Hourly temperature and humidity readings were averaged across the 44 replicate cages with HOBO meters. Descriptive statistics on humidity and temperature readings, as well as transmission efficiency, were calculated using the JMP 9 statistical software package (SAS Institute, Cary, NC).
Results
Quantitative plating of Y. pestis-spiked blood confirmed that the soil within each experimental cage was contaminated with highly bacteremic blood. All cages contained between 9.7 × 108 and 2.22 × 109 cfu, with a mean of 1.55 × 109 cfu per cage. Mice were observed digging through and traveling across this blood-contaminated area within minutes of their addition to the cages, and creating soil burrows within days. Plating of Y. pestis-spiked blood over the course of 10 days in the absence of live soil demonstrated a slight reduction in viable organisms. The initial blood spike contained 1.10 × 1010 cfu/mL, and 1.15 × 109 cfu/mL at the end of 10 days.
Hourly temperature and humidity readings were collected from inside the experimental cages during the 10 days the animals were held on contaminated soil. Because eight of the HOBO meters failed during the course of the experiment, data are reported for only 44 of the 52 cages. Temperatures recorded inside the soil cages ranged from 17.5–23.2°C, with a mean of 18.9°C (SD 1.0°C). In-cage relative humidity readings ranged from 37.7–99%, with a mean of 74.2% (SD 5.4%). All temperature values fell within the range described for ground squirrel burrows (15–27°C; Baudinette 1972), while 10% of relative humidity readings were outside the target range of 68–95%. However, only 2.3% of recorded relative humidity points fell outside the 65–95% range, and many of the aberrant readings occurred when the cages were opened for humidity maintenance and animal care procedures.
Transmission of Y. pestis from contaminated soil was observed in 1 mouse of the 104 exposed. At approximately 60 h following introduction to the cage, the mouse showed signs of infection and was euthanized. Spleen and liver tissues collected at necropsy were positive for Y. pestis by direct fluorescent antibody staining, and infection of both tissues was confirmed by bacteriophage lysis of cultures recovered from the tissues. Subsequent PFGE analysis of the isolate demonstrated that its PFGE pattern was indistinguishable from the PFGE pattern of the strain used to contaminate the soil cage, suggesting that the infectious Y. pestis did not originate from the live soil itself. The remaining mice (n = 103) survived the duration of the study, and none had developed antibodies to Y. pestis 31–35 days after initial exposure to Y. pestis-contaminated soil. Because transmission between co-housed individuals was not observed, mice were not pooled in statistical analyses, and a maximum likelihood analysis estimated a transmission efficiency of 0.96% (95% CI 0.17%,5.25%).
Discussion
We have demonstrated that, consistent with the soil reservoir hypothesis (Mollaret 1963; Baltazard et al. 1963; Drancourt et al. 2006; Ayyadurai et al. 2008), mice can acquire Y. pestis infection from contaminated soil. However, for soil to serve as a long-term reservoir under a natural system, the bacteria must remain infectious for long periods of time, and animals must acquire infection from contaminated soil through normal behaviors such as burrowing, eating from the soil surface, and coming into direct contact with the soil itself. Under our experimental conditions we aimed to optimize the likelihood of transmission by exposing mice to high concentrations of bacteria within confined, environmentally-controlled conditions. Even under these conditions that maximized rodent contact with contaminated soil, transmission efficiency of Y. pestis from contaminated soil to susceptible mice was low compared to that reported for transmission by Oropyslla montana or Xenopsylla cheopis, the principal Y. pestis vectors in North America and throughout the world, respectively (Eisen et al. 2009).
The rodent burrow represents a unique and stable environment protected from light, temperature, and humidity extremes. However, it is unknown if the biological, chemical, or structural characteristics of live soil within this microenvironment might affect the survivability of Y. pestis. If this is indeed the case, variations in key soil characteristics could aid in defining the geographic distribution of plague foci. To date, many studies focusing on Y. pestis persistence outside of mammalian hosts or vectors have shown short-term survival. For example, Y. pestis A1122 was shown to remain viable on organic substrates (paper) for only 120 h (Rose et al. 2003). In sterilized sand, phosphate-buffered saline suspensions of Y. pestis were shown to be viable by standard culture for up to 30 weeks (Ayyadurai et al. 2008). We were able to demonstrate the viability of the virulent Y. pestis strain used in our transmission study in a blood substrate in the absence of live soil over the course of 10 days. Within live soil, however, many factors could alter the survival rate of Y. pestis. For example the addition of organic nutrients from animal wastes or carcasses could enhance survival of the organism. Others have suggested that survival of Y. pestis might be extended through protozoal encystment (Pushkareva 2003), or within the biofilms of soil nematodes (Darby et al. 2002; Eisen et al. 2008). In the absence of these types of positive biological associations, molecular evidence suggests that Y. pestis lacks the genomic elements necessary for prolonged survival outside the host (Achtman et al. 1999; Chain et al. 2004), and competition with soil organisms could limit the ability of free-living Y. pestis to persist in numbers sufficient to produce infection in a new host. Based on the time between when the single infected mouse in our study was exposed to contaminated soil and when it showed signs of infection (60 h post exposure), it appears that infectiousness was greatest within 1 day of contamination, and we did not see evidence of prolonged infectiousness under our experimental conditions.
In the absence of an appropriately selective medium or the use of mice to test contaminated soil via needle inoculation (which was not conducted because of animal welfare concerns), we were unable to determine how long Y. pestis remained viable, and at what concentration, under our experimental conditions. Nonetheless, consistent with earlier results (Indian Plague Research Commission 1906), our data suggest the infectious period was short-lived. Thus we have demonstrated that although burrowing rodents can acquire Y. pestis from highly-contaminated soil, the transmission efficiency is low, which calls into question the hypothesis of soil serving as the primary mechanism of transmission during inter-epizootic periods. These findings may be important in assessing the need for bio-remediation in the unlikely event of an intentional release of Y. pestis.
Acknowledgments
We thank John Young, Ryan Pappert, and Laurel Respicio-Kingry, CDC National Center for Emerging and Zoonotic Infectious Diseases, Division of Vector-Borne Diseases, for providing assistance with processing and evaluating diagnostic specimens; and the Fort Collins Natural Areas Program staff for their advice regarding soil collection. This research was supported in part by an appointment to the Emerging Infectious Diseases (EID) Fellowship Program administered by the Association of Public Health Laboratories (APHL) and funded by the CDC.
Footnotes
Author Disclosure Statement
No competing financial interests exist.
References
- Achtman M, Zurth K, Morelli C, et al. Yersinia pestis, the cause of plague, is a recently emerged clone of Yersinia pseudotuberculosis. Proc Nat Acad Sci USA. 1999;96:14043–14048. doi: 10.1073/pnas.96.24.14043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayyadurai S, Houhamdi L, Lepidi H, et al. Long-term persistence of virulent Yersinia pestis in soil. Microbiology. 2008;154:2865–2871. doi: 10.1099/mic.0.2007/016154-0. [DOI] [PubMed] [Google Scholar]
- Baltazard M, Karimi Y, Eftekhari M, et al. The interepizootic preservation of plague in an inveterate focus Working hypotheses. Bull Soc Pathol Exot Filiales. 1963;56:1230–1245. [PubMed] [Google Scholar]
- Baudinette RV. Energy metabolism and evaporative water loss in the California ground squirrel. J Comp Physiol. 1972;81:57–72. [Google Scholar]
- Bazanova LP, Maevskii MP, Khabarov AV. An experimental study of the possibility for the preservation of the causative agent of plague in the nest substrate of the long-tailed suslik. Med Parazitol (Mosk) 1997:37–39. [PubMed] [Google Scholar]
- Bazanova LP, Nikitin A, Maevskii MP. Conservation of Yersinia pestis in winter by Citellophilus tesquorum altaicus females and males. Med Parazitol (Mosk) 2007:34–6. [PubMed] [Google Scholar]
- Bizanov G, Dobrokhotova ND. Experimental infection of ground squirrels (Citellus pygmaeus Pallas) with Yersinia pestis during hibernation. J Infect. 2007;54:198–203. doi: 10.1016/j.jinf.2006.02.012. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention for PulseNet USA. [accessed on February 21, 2012];One-day (24–28 h) standardized laboratory protocol for molecular typing of Yersinia pestis by pulsed-field gel electrophoresis (PFGE) 2006 Available at http://www.cdc.gov/pulsenet/protocols/yersinia_Apr2006.pdf.
- Chain PS, Carniel E, Larimer FW, et al. Insights into the evolution of Yersinia pestis through whole-genome comparison with Yersinia pseudotuberculosis. Proc Nat Acad Sci USA. 2004;101:13826–13831. doi: 10.1073/pnas.0404012101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu MC. Laboratory Manual of Plague Diagnostic Tests. Geneva: Centers for Disease Control and Prevention and World Health Organization; 2000. p. 129. [Google Scholar]
- Darby C, Hsu JW, Ghori N, et al. Caenorhabditis elegans: plague bacteria biofilm blocks food intake. Nature. 2002;417:243–244. doi: 10.1038/417243a. [DOI] [PubMed] [Google Scholar]
- Drancourt M, Houhamdi L, Raoult D. Yersinia pestis as a telluric, human ectoparasite-borne organism. Lancet Infect Dis. 2006;6:234–241. doi: 10.1016/S1473-3099(06)70438-8. [DOI] [PubMed] [Google Scholar]
- Eisen RJ, Eisen L, Gage KL. Studies of vector competency and efficiency of North American fleas for Yersinia pestis: state of the field and future research needs. J Med Entomol. 2009;46:737–744. doi: 10.1603/033.046.0403. [DOI] [PubMed] [Google Scholar]
- Eisen RJ, Gage KL. Adaptive strategies of Yersinia pestis to persist during inter-epizootic and epizootic periods. Vet Res. 2009;40:1. doi: 10.1051/vetres:2008039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisen RJ, Petersen JM, Higgins CL, et al. Persistence of Yersinia pestis in soil under natural conditions. Emerg Infect Dis. 2008;14:941–943. doi: 10.3201/eid1406.080029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gage KL, Kosoy MY. Natural history of plague: perspectives from more than a century of research. Annu Rev Entomol. 2005;50:505–528. doi: 10.1146/annurev.ento.50.071803.130337. [DOI] [PubMed] [Google Scholar]
- Hahn N, Eisen RJ, Lane RS. Ketamine-medetomidine anesthesia with atipamezole reversal: Practical anesthesia for rodents under field conditions. Lab Anim (NY) 2005;34:48–51. doi: 10.1038/laban0205-48. [DOI] [PubMed] [Google Scholar]
- Indian Plague Research Commission. Reports on plague investigations in India: On the infectivity of floors grossly contaminated with cultures of B. pestis. J Hyg (Lond) 1906;6:509–518. doi: 10.1017/s0022172400003107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karimi Y. Natural preservation of plague in soil. Bull Soc Pathol Exot Filiales. 1963;56:1183–1186. [PubMed] [Google Scholar]
- Mollaret HH. Experimental preservation of plague in soil. Bull Soc Pathol Exot Filiales. 1963;56:1168–1182. [PubMed] [Google Scholar]
- Mollaret HH, Karimi Y, Eftekhari M, et al. Burrowing Plague. Bull Soc Pathol Exot Filiales. 1963;56:1186–1193. [PubMed] [Google Scholar]
- Poland JD, Dennis DT. Plague Manual: Epidemiology, Distribution, Surveillance and Control. Geneva: World Health Organization; 1999. Diagnosis and clinical manifestations; pp. 43–54. [Google Scholar]
- Pollitzer R, Meyer KF. The ecology of plague. In: May JM, editor. Studies in Disease Ecology. Hafner: Macmillan; 1961. pp. 433–590. [Google Scholar]
- Pushkareva VI. Experimental evaluation of interaction between Yersinia pestis and soil infusoria and possibility of prolonged preservation of bacteria in the protozoan oocysts. Zh Mikrobiol Epidemiol Immunobiol. 2003:40–44. [PubMed] [Google Scholar]
- Rose LJ, Donlan R, Banerjee SN, et al. Survival of Yersinia pestis on environmental surfaces. Appl Environ Microbiol. 2003;69:2166–2171. doi: 10.1128/AEM.69.4.2166-2171.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sebbane F, Gardner D, Long D, et al. Kinetics of disease progression and host response in a rat model of bubonic plague. Am J Pathol. 2005;166:1427–1439. doi: 10.1016/S0002-9440(10)62360-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor DM, McConnell I, Fraser H. Scrapie infection can be established readily through skin scarification in immunocompetent but not immunodeficient mice. J Gen Virol. 1996;77:1595–1599. doi: 10.1099/0022-1317-77-7-1595. [DOI] [PubMed] [Google Scholar]
- Yersin M. La peste bubonique a Hong-Kong. Ann Inst Pasteur. 1894;8:662–667. [Google Scholar]