Abstract
Depressive syndrome and disorders increase substantially during adolescence. Little is known, however, about how individual symptoms of depression change over the course of this developmental period. The present study examined within-person changes in symptom severity of each individual symptom of depression, utilizing longitudinal data collected across six years of adolescence. Adolescent gender and family relationship variables were tested as predictors of the symptom trajectories (i.e., intercept and slope). Adolescents and their mothers (N = 240) were first evaluated when youth were in grade 6 (M = 11.86 years old; SD = 0.56; 54% female) and then annually through grade 12. Individual symptoms of depression were assessed by a clinical interviewer using the Children’s Depression Rating Scale-Revised (CDRS-R). Mothers and youth also completed measures about their relationship on the Children’s Report of Parent Behavior Inventory and the Family Environment Scale. Results showed that all depressive symptoms increased linearly over time except psychomotor disturbances and problems with concentration and decision making, which were best represented by a quadratic growth model. Sex differences were found such that significantly more rapid increases in worthlessness/guilt were found for girls than boys, and concentration/decision making problems decreased significantly for boys, but not girls. Poor family relationship quality (mother-reported) predicted a significantly faster rate of increase in adolescents’ symptoms of anhedonia, appetite/weight changes, and fatigue. High maternal psychological control (youth-reported) also predicted a faster rate of increase in anhedonia. Study limitations, future research directions, and clinical implications of the findings are discussed.
Keywords: adolescents, symptoms of depression, family relationship quality, parenting
Depression in adolescence carries risk not only for developing recurrent depressive episodes throughout life, but also for impairment in multiple domains of adolescent development, including cognitive and social functioning as well as physical health (e.g., Glied & Pine, 2002; Kovacs & Goldston, 2002). Depression has been described as a symptom, a syndrome, and a diagnostic disorder (Compas, Ey, & Grant, 1993; Hankin, Fraley, Lahey, & Waldman, 2005). The symptom of depression is sad mood, and typically is measured as a single item on a questionnaire or clinical interview. The syndrome of depression is defined as a set of symptoms that covary at the same point in time. Total scores on self-report questionnaires such as the Children’s Depression Inventory (CDI, Kovacs, 1981) or the Affective Problems subscale of the Youth Self-report (YSR, Achenbach & Rescorla, 2001), and clinician ratings on the Children’s Depression Rating Scale (Poznanski, Mokros, Grossman, & Freeman, 1985) are measures of the syndrome of depression. Finally, depressive disorders are defined as a specific set of symptoms that covary (i.e., the syndrome) and have a particular course, prognosis, etiology, and response to treatment.
The rates of depression measured both as a categorical diagnosis and as a total score on a dimensional syndrome inventory increase significantly during adolescence (Cole et al., 2002; Garber, Keiley, & Martin, 2002; Ge, Lorenz, Conger, Elder, & Simons, 1994; Hankin et al., 1998; Twenge & Nolen-Hoeksema, 2002). For example, Cole et al. (2002) showed that syndromal measures of depressive symptoms increased linearly between grades 5 to 7 and grades 6 to 8. A meta-analysis of cross-sectional studies revealed an increase in girls’ depressive symptoms from ages 13 to 16 (Twenge & Nolen-Hoeksema, 2002). Others have shown that depression syndrome scores follow a curvilinear pattern during adolescence (Garber et al., 2002), particularly among girls (Ge et al., 1994).
There is a growing emphasis on depression as being a continuous rather than categorical construct, and an increasing recognition of the importance of examining individual symptom patterns over time (Cole et al., 2011; Ruscio & Ruscio, 2000). Research on adolescent depression, however, has focused almost exclusively on the syndrome or diagnosis; much less is known about how each individual symptom that comprises the syndrome of depression changes across adolescence. Although the benefits of examining individual symptoms have been clearly articulated for quite some time (e.g., Costello, 1992; Persons, 1986), few empirical investigations have actually done so. Understanding the course and predictors of individual symptoms of depression is important for several reasons. First, documenting the developmental trajectories of individual symptoms of depression may increase our ability to recognize an emerging depressive disorder prior to its full onset (Weiss & Garber, 2003). Second, understanding how and when individual symptoms of depression change over time may provide clues to mechanisms underlying the disorder (Kendler, Zachar, & Craver, 2011). Third, determining the trajectories of the individual symptoms of depression can help clinicians decide which ones to target for early intervention and prevention (Conradi, Ormel, & de Jonge, 2011; Rabin, Kaslow, &Rehm, 1984; Sorensen, Nissen, Mors, & Thomsen, 2005).
The few studies of developmental changes in individual symptoms of depression have been based on cross-sectional designs in which the prevalence or frequency of symptoms among younger versus older children has been compared (Fu-I & Wang, 2008; Mitchell, McCauley, Burke, & Moss, 1988; Ryan et al., 1987; Sorensen et al., 2005; Yorbik, Birmaher, Axelson, Williamson, & Ryan, 2004). Although these cross-sectional studies have shown that the prevalence of most individual symptoms of depression is greater in older as compared to younger children, they preclude drawing conclusions about systematic within-person changes in individual depressive symptoms during adolescence, which is when the overall rates of depressive syndrome are known to be increasing (e.g., Hankin et al., 1998). First, cross-sectional studies and between-subject designs cannot be used to determine intra-individual change. Second, studies have focused on frequency counts of symptoms or their categorical presence versus absence, rather than on the dimensional severity of each symptom across time. Third, participants in these studies have been mostly from clinic samples of youth with diagnosed depressive disorders rather than from community or at-risk samples. Fourth, the age cut-offs for comparing younger children to adolescents have been arbitrary and inconsistent across studies. That is, children classified as “young” in one study may be categorized as “adolescents” in another study. For example, in Yorbik et al. (2004), younger children were between 5.6 and 12.9 years, whereas in the studies by Sorensen et al. (2005) and Fu-I and Wang (2008) children ages 12 or 13 were in the older group.
The few longitudinal studies of depressive symptoms have examined concordance or stability of symptoms endorsed over adolescence (e.g., Lewinsohn, Pettit, Joiner, & Seeley, 2003; Pine, Cohen, Cohen, & Brook, 1999). In a sample followed from adolescence to early adulthood, Lewinsohn et al. (2003) tracked the frequency of symptoms that occurred during major depressive episodes (MDEs) and found that anhedonia was the most stable symptom across episodes. Overall, however, there was low concordance among the depressive symptoms endorsed from one episode to the next; that is, prior symptoms were not particularly predictive of the symptoms experienced in subsequent episodes.
There may be meaningful within-person variability in depressive symptoms over time. Keller, Neale, and Kendler (2007) noted that the presentation of depression is heterogeneous, or “flexible,” depending upon the specific adverse life events to which individuals are exposed prior to their MDE, and therefore symptoms might not be stable over time. Evidence of differences in the heritability of individual symptoms also suggests that each depressive symptom might follow a distinct course of its own (Jang, Livesly, Taylor, Stein, & Moon, 2004). Moreover, some symptoms may have different trajectories from childhood to adolescence partially due to changes in cognitive or biological development (e.g., Fu-I & Wang, 2008; Weiss & Garber, 2003).
Evidence of between-subjects rank ordering of symptoms across time or episodes, however, is not necessarily informative about continuity in the severity of the symptoms over time. That is, stability in the rank order of symptoms indicates whether between-person differences are sustained, but does not reflect intra-individual changes in symptom severity. Thus, conclusions about within-person stability of depressive symptoms may be overinflated when only the rank order of symptoms across individuals is examined (e.g., Minor, Champion, & Gotlib, 2005).
Longitudinal studies of within-person changes in symptom severity have been conducted in adults over the course of treatment for depression. Some studies have found similar growth patterns among different individual symptoms of depression (e.g., Bhar et al., 2008; Rabin et al., 1984), whereas other studies have demonstrated that certain symptoms show more rapid and early improvements during treatment than others (e.g., Fournier et al., 2013). Whether or not these results also hold for adolescents with neither a depressive diagnosis nor treatment is not yet known. A primary aim of the present prospective study was to address some of the methodological gaps in the literature by examining within-person changes in symptom severity among the individual symptoms of depression, utilizing longitudinal data collected in adolescents at varied risk for depression.
Sex Differences in Symptom Trajectories
Females are twice as likely as males to experience depression, and self-reported depressive symptom scores have been found to increase more rapidly for girls than boys (Cole et al., 2002). This sex difference emerges in adolescence (e.g., Hankin et al., 1998; Twenge & Nolen-Hoeksema, 2002). Whether specific symptoms of depression increase at a faster rate for girls than boys is not known, however. Identifying sex differences in the trajectories of individual depressive symptoms can further our understanding of possible mechanisms that place girls at increased risk for developing depression.
Cross-sectional studies of depressed girls and boys have indicated that certain symptoms, including appetite and weight changes (Roberts, Lewinsohn, & Seeley, 1995), feelings of worthlessness and guilt (Fu-I & Wang, 2008; Roberts et al., 1995), and suicidal ideation (Yorbik et al., 2004) are more prevalent in girls than boys, whereas concentration problems are more prevalent in boys (Fu-I & Wang, 2008). Baji et al. (2009) showed that girls endorsed more anhedonia and sleep problems, but did not find sex by age interactions, indicating that boys’ and girls’ trajectories on these particular symptoms may not differ. Kovacs (2001) and Lewinsohn et al. (2003) reported that depression symptom patterns were similar for males and females. Thus, evidence of sex differences in individual symptoms of depression has not been consistent. Moreover, sex differences in changes in individual symptoms over time have not been examined. Therefore, a second goal of the present prospective study was to explore sex differences in individual depressive symptom trajectories over adolescence.
Family Processes as Predictors of Symptom Trajectories
What predicts changes in the specific symptoms of depression over adolescence? This question has important implications for the early identification of risk factors to target for the prevention of escalations in depressive symptoms and disorders during this salient developmental period. The family environment, particularly the parent-child relationship and the overall quality of family relationships, has been shown to be a robust predictor of children’s adjustment and overall mental health (Cummings & Davies, 2010; Kaslow, Deering, & Racusin, 1994; Sheeber, Hops, & Davis, 2001) and has been consistently implicated as a risk factor in the onset and course of depression in youth (Fleming & Offord, 1990; Sheeber et al., 2001).
With regard to specific parenting behaviors, greater parental acceptance is associated with better child adjustment (e.g., Elgar, Mills, McGrath, Waschbusch, & Brownridge, 2007; McFarlane, Bellissimo, & Norman, 1995), whereas inconsistent, harsh discipline and psychological control are related to higher levels of adolescent depressive symptoms (e.g., Barber, 1996; El-Sheikh, Hinnant, Kelly, & Erath, 2010; Silk, Morris, Kanaya, & Steinberg, 2003). Additionally, the overall climate of the family environment also has been linked to internalizing problems (Kaslow et al., 1984; Lau & Kwok, 2000; Sheeber et al., 2001). Higher levels of conflict and low levels of cohesiveness and expressiveness in the family have been found to be associated with higher levels of depressive symptoms in adolescents (e.g., Aydin & Oztütüncü, 2001; Sheeber, Hops, Alpert, Davis, & Andrews, 1997). Finally, a few studies have shown that the family environment predicts certain individual symptoms of depression, such as depressed mood and low self-esteem (Plunkett, Henry, Robinson, Behnke, & Falcon, 2007), sleep disturbance (e.g., El-Sheikh, Buckhalt, & Mize, 2006), disordered eating (e.g., Blodgett Salafia, Schaefer, & Haugen, 2013), and attention problems (e.g., Jester et al., 2005). The third aim of the current study was to examine two dimensions of the family environment -- maternal parenting behavior and the overall quality of family relationships -- as possible predictors of adolescents’ individual depressive symptom trajectories.
In summary, the current six-year prospective study investigated within-person changes in the severity of each of the ten individual symptoms that comprise major depressive disorder, during a developmental period (i.e., adolescence) when the rates of depression are known to be increasing. Further, the present study tested adolescent gender and family environment variables as possible predictors of the individual symptom trajectories, over and above mothers’ current level of depressive symptoms (i.e., risk).
Method
Participants
Participants were 240 mothers and children who were first assessed in sixth grade (M = 11.86 years old; SD = 0.56; 54% female), and then annually through grade 12. The child sample was 81.5% Caucasian, 14.8% African American, and the remaining 3.7% were Hispanic, Native American, or reported “Other.” Families were predominantly working class (e.g., nurse’s aide, sales clerk) to middle class (e.g., store manager, teacher) with a mean socioeconomic status (Hollingshead, 1975) of 41.67 (SD = 13.29).
Procedures
Parents of fifth grade children from metropolitan public schools were invited to participate in a study about parents and children. A brief health history questionnaire and a letter describing the project were sent to over 3,500 families. We used a high-risk research design that involved including youth who varied in risk as a function of their mother’s history of depressive disorders to increase variability on the constructs of interest (e.g., depressive symptoms, family environment) and reduce potential restriction of range often seen in normative community samples (Kovacs, 1981). Of the 1,495 families interested in participating, the 587 mothers who had endorsed either a history of depression, use of antidepressants, or no history of psychopathology were interviewed further by telephone. Of these 587 screened, 238 families were excluded because the mothers did not indicate sufficient symptoms to meet criteria for a depressive disorder (38%), had other psychiatric disorders that did not also include a depressive disorder (19%), were no longer interested (21%), they or the target child had a serious medical condition (14%), the target child was in a different grade (6%), or the family had moved out of the area (2%). The remaining 349 mothers who indicated during the screening calls that they had had a history of depression or had had no psychiatric problems were interviewed further with the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders diagnoses (Spitzer, Williams, Gibbon, & First, 1990). Of the 349 mothers interviewed, 109 were excluded because the mother indicated a history of a psychiatric diagnosis that did not also include a mood disorder or the mother or child had a serious medical condition. The final sample of 240 families consisted of 185 mothers who had histories of depressive disorders (e.g., Major Depressive Disorder; Dysthymia) and 55 mothers who were lifetime free of psychopathology. Inter-rater reliability, calculated on a random subset of 25% of these interviews, yielded 94% agreement (kappa = .88) for diagnoses of depressive disorders.
Children were first assessed in sixth grade and then yearly through 12th grade. Research assistants, unaware of the mother’s psychiatric history, interviewed the mother and child separately and administered the questionnaires. There was 19% attrition from the first to last assessment. Families were unavailable due to scheduling difficulties, being too busy, no longer interested, or moving away. Mothers and children who dropped out did not differ on initial levels of any of the individual depressive symptoms or on any of the other study variables, except that mothers who dropped out reported higher levels of maternal psychological control, t(225) = 2.63, p = .01. The analytic approach used in the current study utilized all available data such that participants with incomplete data were included in analyses (Raudenbush & Bryk, 2002). All study procedures were approved by the institutional review board for the protection of human subjects. Mothers provided informed consent, and children signed an assent form. Mothers and youth were compensated for their time at each annual assessment.
Measures
Adolescents’ depressive symptoms
The Children’s Depression Rating Scale-Revised (CDRS-R; Poznanski et al., 1985) is a brief semi-structured clinical interview that assesses the severity of individual symptoms of depression experienced in the last two weeks. Mothers and youths were interviewed separately about the adolescents’ symptoms; eight symptoms were rated on a 7-point severity scale (1 = no symptom to 7 = severe level of symptoms with significant impairment); two symptoms (sleep problems, appetite changes) were rated on a 5-point scale. The CDRS-R provides individual ratings for each of ten symptoms of depression: sad mood, irritability, anhedonia, sleep problems, fatigue, appetite/ weight changes, psychomotor disturbance (retardation or agitation), low self-esteem or excessive guilt, problems with concentration or decision making, and suicidal ideation, and a total score. On the CDRS-R, interviewers use information obtained from both the mother and child to rate each symptom (Poznanski et al., 1985). The CDRS-R has good internal consistency, construct validity, inter-rater reliability, and can capture changes in specific symptoms over time (Jain et al., 2007; Mayes, Berstein, Haley, Kennard, & Emslie, 2010). Reliability of the CDRS-R ratings at each time point was ≥ .72. The CDRS-R was not administered in grade 10 due to funding constraints.
Maternal depression
Mothers completed the Beck Depression Inventory (BDI; Beck, Ward, Mendelson, Mock, &Erlbaugh, 1961), which assesses affective, cognitive, behavioral, and somatic symptoms. For each item, respondents choose one of four statements that best describes how they had been feeling during the past two weeks. The 21 items are scored 0-3 and summed to create a total score ranging from 0 to 63. The BDI has good validity in both psychiatric (Beck et al., 1961) and community samples (Beck, Steer, & Garbin, 1988). Internal consistency of mothers’ initial BDI scores was .90. Mothers with a history of depression reported significantly higher levels of depressive symptoms (M = 8.60, SD = 8.13) than mothers without a history of depression (M = 1.49, SD = 2.01), t (234) = 6.41, p < .001.
Family variables
In Grade 6, children and mothers completed child- and parent-versions, respectively, of the Children’s Report of Parent Behavior Inventory (CRPBI; Schaefer, 1964; Schludermann & Schludermann, 1970). The CRPBI contains 108 items about parents’ child-rearing behaviors and includes 18 subscales representing three dimensions: acceptance/ rejection -- the extent to which the parent expresses care and affection for the child (e.g., “My mother… tells me how much she loves me." "…gives me a lot of care and attention."); autonomy/ psychological control -- the extent to which the parent controls the child through indirect psychological methods such as inducing guilt, instilling anxiety, and/or withdrawing love (e.g., “My mother…is always telling me how I should behave." "…feels hurt when I don't follow her advice"); and firm/ lax control -- the extent to which the parent consistently enforces compliance by making rules or threatening punishment (e.g., “My mother…sees to it that I know exactly what I may or may not do." “…sticks to a rule instead of allowing a lot of exceptions."). Youth rated the degree of similarity between the behavior described and their mother using a 3-point scale a (0 = like, 1 = somewhat like, or 2 = not like). Mothers used this 3-point scale to rate how similar they were to the behaviors described. Internal consistency for these dimensions in this sample were, respectively, .95, .79, and .77 for children's report, and .87, .77, and .77 for mothers' report. Mothers’ and children’s reports on each subscale of the CRPBI were significantly correlated (acceptance/ rejection r = .35, psychological control r = .31, firm/ lax control r = .26, all p < .001). No significant mean difference was found between mothers’ and children’s reports of maternal acceptance; children reported higher levels of maternal psychological control, t(224) = 10.233, p < .001, and lower levels of firm control, t(224) = 5.82, p < .001, than mothers reported about themselves.
Mothers and children also completed the Family Environment Scale (FES; Moos & Moos, 1994), which included 36 true-false items about their family (e.g., “We fight a lot in our family.” “There is a feeling of togetherness in our family.”). The Family Relationship Index (FRI) is a composite of three subscales: cohesion (degree of commitment and support among family members), expressiveness (degree to which family members are encouraged to express their feelings), and conflict (degree to which family members openly express conflict). Higher FRI scores reflect better family relationship quality. Cronbach’s alpha for the FRI index was .82 and .84 for adolescent- and mother-reports, respectively. Mothers’ and children’s FRI scores were significantly correlated (r = .28, p < .001).
Data Analysis Plan
Trajectories of individual symptoms
Hierarchical linear models (HLM; Raudenbush & Bryk, 2002) were run to model trajectories of each depressive symptom. The Level 1 model estimated yearly, within-individual changes in each symptom during the six-year study period; the Level 2 model aggregated these person-level estimates to provide estimates for the average growth trajectory for the sample. The deviance statistic in HLM 6.06 was used to determine whether a linear or quadratic growth model best fit the data for each symptom. Time was coded such that the intercept represented the average level of each symptom at the beginning of the study (grade 6). The Benjamini-Hochberg’s false discovery rate correction (set at alpha=.05; Benjamini & Hochberg, 1995) was used to control for the multiple tests conducted. These corrected results are presented in Table 2 and Supplemental Tables 1-5,
Table 2.
Mother-reported Family Relationship Quality as a Predictor of Individual Symptom Trajectories
| Parameter | Sad Mood | Anhedonia | Irritability | Sleep Problems |
Fatigue | |||||
|
| ||||||||||
| Fixed Effects | ||||||||||
|
| ||||||||||
| Level 1 | b (SE) | p | b (SE) | p | b (SE) | p | b (SE) | p | b (SE) | p |
| Intercept | 1.82 (.04) | .000 | 1.30 (.03) | .000 | 2.13 (.04) | .000 | 1.36 (.04) | .000 | 1.23 (.04) | .000 |
| Time | .03 (.02) | .056 | .09 (.01) | .000 | .06 (.01) | .000 | .11 (.02) | .000 | .20 (.01) | .000 |
| Time * Time | -- | -- | -- | -- | -- | |||||
|
| ||||||||||
| Level 2 | ||||||||||
| Mothers’ BDI | .01 (.01) | .328 | .01 (.005) | .290 | .005 (.01) | .439 | .01 (.01) | .359 | .01 (.005) | .041 |
| Sex | .11 (.09) | .210 | −.06 (.07) | .389 | −.08 (.09) | .365 | −.03 (.08) | .738 | .05 (.07) | .459 |
| FRI | −.02 (.01) | .098 | −.01 (.01) | .307 | −.04 (.01) | .000 | −.004 (.01) | .643 | −.002 (.01) | .778 |
| Time * BDI | .00 (.00) | .997 | .001 (.002) | .587 | .002 (.002) | .448 | .002 (.002) | .495 | −.001 (.002) | .550 |
| Time * Sex | .06 (.03) | .039 | .042 (.03) | .118 | .04 (.03) | .125 | .07 (.03) | .022 | .05 (.03) | .105 |
| Time * FRI | −.002 (.003) | .490 | −.01 (.003) | .009 | −.004 (.003) | .172 | −.01 (.004) | .077 | −.01 (.003) | .012 |
| Time * Time * BDI | -- | -- | -- | -- | -- | |||||
| Time * Time * Sex | -- | -- | -- | -- | -- | |||||
| Time * Time * FRI | -- | -- | -- | -- | -- | |||||
|
| ||||||||||
| Parameter | Appetite/Weight Changes |
Psychomotor Disturbance |
Concentration/ Indecision |
Low Self-esteem/ Guilt |
Suicidal Ideation | |||||
|
| ||||||||||
| Fixed Effects | ||||||||||
|
| ||||||||||
| Level 1 | b (SE) | p | b (SE) | p | b (SE) | p | b (SE) | p | b (SE) | p |
| Intercept | 1.32 (.03) | .000 | 1.15 (.03) | .000 | 1.27 (.04) | .000 | 2.14 (.05) | .000 | 1.02 (.01) | .000 |
| Time | .05 (.01) | .000 | −.06 (.03) | .024 | .16 (.04) | .000 | .08 (.01) | .000 | .01 (.01) | .036 |
| Time * Time | -- | .01 (.004) | .002 | −.01 (.01) | .035 | -- | -- | |||
|
| ||||||||||
| Level 2 | ||||||||||
| Mothers’ BDI | .003 (.01) | .545 | .01 (.004) | .003 | .002 (.01) | .801 | .01 (.01) | .040 | .00 (.002) | .806 |
| Sex | .07 (.07) | .317 | .03 (.05) | .608 | .04 (.09) | .656 | .005 (.10) | .959 | .003 (.02) | .895 |
| FRI | −.01 (.01) | .275 | −.002 (.01) | .685 | −.01 (.01) | .179 | −.03 (.01) | .019 | −.01 (.003) | .015 |
| Time * BDI | .00 (.002) | .822 | −.01 (.004) | .006 | −.01 (.01) | .315 | −.00 (.002) | .714 | .00 (.000) | .850 |
| Time * Sex | .04 (.02) | .110 | −.03 (.05) | .599 | −.19 (.09) | .023 | .08 (.03) | .007 | .01 (.01) | .587 |
| Time * FRI | −.01 (.003) | .008 | −.01 (.01) | .228 | −.02 (.01) | .029 | −.004 (.003) | .204 | −.00 (.00) | .833 |
| Time * Time * BDI | -- | .002 (.001) | .004 | .001 (.001) | .372 | -- | -- | |||
| Time * Time * Sex | -- | .01 (.01) | .518 | .03 (.01) | .016 | -- | -- | |||
| Time * Time * FRI | -- | .001 (.001) | .249 | .003 (.002) | .065 | -- | -- | |||
Note. BDI = Mothers’ Beck Depression Inventory score, FRI = Family Relationship Index.
Bolded p-values indicate the parameter is significant after applying the Benjamini-Hochberg correction for multiple tests. -- denotes parameter not estimated in model. Variance parameters not presented, but are available upon request. Time was coded so that the intercept represents level of the symptom in grade 6. Sex coded as −.5 = boys, .5 = girls.
Predictors of individual symptom trajectories
Predictors were added to Level 2 models to examine whether individual variability in adolescents’ trajectories was accounted for by differences in sex, parenting, or family relationship quality. First, we tested sex as a predictor of adolescent’s symptom trajectories by including it as a predictor of the intercept and slope parameters. In the next analyses, we tested the three subscales of the CRPBI representing the three parenting dimensions (acceptance, firm control, psychological control) simultaneously as predictors of adolescents’ trajectories. Finally, a separate model was examined with family relationship quality (FRI) as a predictor. Maternal depressive symptoms at baseline (i.e., risk), was included in all analyses as a predictor of both the intercept and slope.
Results
Table 1 presents descriptive information for the individual depressive symptoms scores across time. Unconditional hierarchical linear growth models indicated that all depressive symptoms systematically changed from grade 6 to grade 12 (see Supplemental Table 1). Compared to a quadratic growth model, linear growth models best fit the data for the core symptoms of sad mood and irritability, as well as symptoms of sleep problems, fatigue, appetite/weight changes, low self-esteem/guilt, and suicidal ideation, indicating linear increases in these symptoms each year during adolescence. Although the deviance statistic in HLM indicated that a quadratic model provided a better fit to the data for anhedonia, the quadratic slope was not significant (b = −.01, p = .09); therefore, the more parsimonious linear growth model was used in further analyses for anhedonia.
Table 1.
Mean, Standard Deviation, and Range of Individual Depressive Symptom Scores
| Grade 6 | Grade 7 | Grade 8 | Grade 9 | Grade 11 | Grade 12 | ||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Depressive Symptoms | Range | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) |
| Sad Mood | 1-7 | 1.87 (.84) | 1.86 (.93) | 1.80 (.81) | 1.83 (.84) | 2.01 (1.15) | 2.05 (1.26) |
| Anhedonia | 1-7 | 1.23 (.49) | 1.47 (.70) | 1.45 (.73) | 1.64 (.91) | 1.84 (1.13) | 1.78 (1.14) |
| Irritability | 1-7 | 2.11 (.84) | 2.27 (.90) | 2.25 (.93) | 2.28 (.97) | 2.52 (1.20) | 2.45 (1.22) |
| Sleep Problems | 1-5 | 1.37 (.71) | 1.50 (.85) | 1.54 (.81) | 1.63 (.90) | 1.98 (1.28) | 2.01 (1.28) |
| Fatigue | 1-7 | 1.27 (.58) | 1.40 (.70) | 1.52 (.74) | 1.81 (.92) | 2.41 (1.01) | 2.36 (1.14) |
| Appetite /Weight Change | 1-5 | 1.35 (.65) | 1.45 (.74) | 1.32 (.58) | 1.46 (.75) | 1.55 (.92) | 1.60 (1.00) |
| Psychomotor Disturbance | 1-7 | 1.16 (.48) | 1.07 (.31) | 1.09 (.35) | 1.11 (.48) | 1.27 (.58) | 1.30 (.80) |
| Low Self-esteem/Guilt | 1-7 | 2.04 (.88) | 2.41 (.92) | 2.26 (.80) | 2.35 (.83) | 2.57 (.98) | 2.63 (1.17) |
| Concentration/Indecision | 1-7 | 1.24 (.61) | 1.51 (.94) | 1.45 (.81) | 1.56 (.87) | 1.72 (1.05) | 1.65 (1.07) |
| Suicidal Ideation | 1-7 | 1.03 (.20) | 1.05 (.38) | 1.01 (.10) | 1.09 (.40) | 1.12 (.51) | 1.06 (.36) |
Note. N = 240 at grade 6. CDRS-R was not administered in Grade 10.
For concentration difficulties/indecision and psychomotor disturbance, a quadratic growth model fit the data best. Specifically, concentration and decision making difficulties were initially systematically increasing in grade 6 (linear slope = .15, SE = .04, p < .001), although the rate of change slowed down each year (quadratic slope = −.014, SE = .007, p = .04). Psychomotor disturbances were initially linearly decreasing in grade 6 (linear slope = −.05, SE = .02, p = .04), and the rate of decline slowed each year (quadratic slope = .014, SE = .004, p < .001), eventually showing a sharp rise in psychomotor symptoms from grades 9 to 12. Importantly, there was significant individual variability in all growth parameters; therefore, we were able to test potential predictors of adolescent’s symptom trajectories.
Sex differences in depressive symptom trajectories
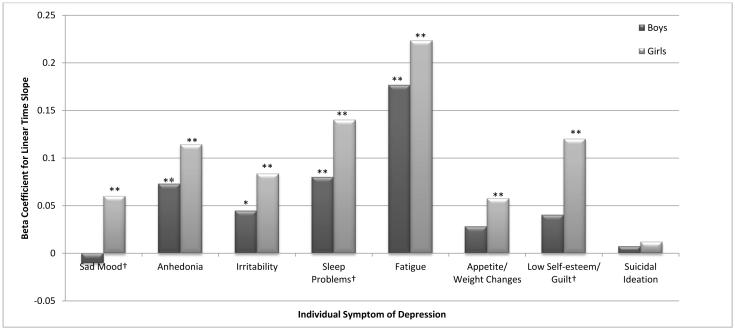
Significant sex by time interactions were found indicating sex differences in the trajectories of the four individual symptoms: sad mood (b = .07, SE = .03, p=.025), sleep problems (b = .07, SE = .03, p=.03), low self-esteem/guilt (b = .09, SE = .03, p=.003), and concentration problems/indecision (interaction with linear slope: b = −.21, SE = .08, p=.018; interaction with quadratic slope: b = .04, SE =.01, p=.01 (see Figure 1, and Supplemental Table 2). Simple slope analyses in HLM indicated that low self-esteem/guilt increased for girls (b = .12, SE = .02, p< .0001) but not for boys (b = .04, SE = .02, p = .07). In contrast, concentration problems/indecision systematically changed for boys (linear slope = .26, SE = .06, p< .0001; quadratic slope = −.03, SE = .01, p< .0001), but not for girls (linear slope = .05, SE = .06, p = .34; quadratic slope = .003, SE = .01, p = .75). Sleep disturbances increased at a faster rate for girls (b = .14, SE = .02, p < .001) than boys (b = .08, SE = .02, p < .001). No sex differences in levels of sad mood were found in grade 6, but sadness linearly increased for girls (b = .06, SE = .02, p = .004) but not for boys (b = −.01, SE = .02, p = .72).
Figure 1.
Predicted yearly change in individual symptoms of depression for boys and girls.
Note. Yearly change plotted for symptoms that demonstrated linear change over time. Concentration/indecision and psychomotor disturbance showed quadratic change and are not depicted in figure. Analyses controlled for maternal depressive symptoms.
* = slope significant at p< .05; ** = slope significant at p< .01; † = slopes for boys and girls significantly different from each other.
Parenting dimensions as predictors of depressive symptom trajectories
Because sex differences were found for some symptoms, we included sex as a control variable (on intercepts and slopes) in the remaining analyses along with maternal depressive symptoms, resulting in more conservative estimates of the family process variables as predictors of adolescents’ symptom trajectories. Youth-reported maternal psychological control significantly predicted trajectories of anhedonia (b = .13, SE = .04, p = .004) such that anhedonia increased at a faster rate when levels of maternal psychological control were high (see Supplemental Table 3). Youth-reported maternal psychological control also predicted steeper increases in irritability (b = .09, SE = .05, p = .043) and appetite/weight problems (b = .08, SE = .04, p = .049). With regard to initial levels of symptoms in grade 6, youth-reported maternal acceptance predicted lower levels of irritability (b = −.41, SE = .14, p = .006) and suicidal ideation (b = −.13, SE = .04, p = .003). Youth-reported firm control was related to higher levels of sad mood (b = .54, SE = .19, p = .005) in grade 6 (see Supplemental Table 3). Mother-reported maternal acceptance predicted self-esteem/guilt (b = −.17, SE = .08, p = .033) and maternal firm control predicted irritability (b = −.15, SE = .08, p = .047), such that self-esteem/ guilt and irritability increased at a slower rate when acceptance and firm control, respectively, were high (see Supplemental Table 4).
Family relationship quality as a predictor of depressive symptom trajectories
Worse family relationship quality, as reported by mothers, significantly predicted steeper linear increases in adolescents’ symptoms of anhedonia (b = −.01, SE = .003, p = .009), fatigue (b = −.01, SE = .003, p = .012) and appetite/weight problems (b = −.01, SE = .003, p = .008); steeper decreases in concentration problems (b = −.02, SE = .01, p = .029); and higher levels of irritability (b = −.04, SE = .01, p< .001) in grade 6 (see Table 2). Worse family relationship quality, as reported by adolescents, also predicted higher levels of irritability (b = −.03, SE = .01, p = .001), appetite/weight problems (b = −.02, SE = .01, p = .016), self-esteem/guilt symptoms (b = −.03, SE = .01, p = .002), and suicidal ideation (b = −.01, SE = .003, p< .001) in grade 6 (see Supplemental Table 5), but did not predict symptom trajectories.
Discussion
This study examined how individual symptoms of depression changed across adolescence, using advanced multilevel modeling analyses that account for within-person changes in symptom severity as well as individual differences in symptom trajectories. Extending previous research, the present six-year longitudinal study makes a unique contribution to the literature by (a) tracking changes in individual depressive symptoms during the developmental period (i.e., adolescence) when rates of depression increase, (b) focusing on changes in within-individual severity of symptoms rather than simply on the presence or absence of symptoms at different points in time, and (c) testing potential predictors of these symptom trajectories.
Several important results emerged. First, we found significant within-person changes in the severity of individual symptoms of depression during adolescence. All symptoms increased linearly over time; for psychomotor disturbance, this increase occurred at grade 9, and for concentration problems/indecision the increase slowed over time. The findings are consistent with cross-sectional studies of clinical samples that have shown a higher prevalence rate of the individual symptoms of depression in older as compared to younger children (e.g., Baji et al., 2009; Ryan et al., 1987; Sorensen et al., 2005; Yorbik et al., 2004). The current study extends prior evidence of increases in depressive symptoms defined categorically by demonstrating growth in the severity of depressive symptoms as defined dimensionally.
One symptom, psychomotor disturbance (i.e., psychomotor retardation or agitation), evidenced a quadratic growth pattern in which the symptom initially decreased, and decelerated over time, but eventually showed a sharp increase from grade 9 to 12. In a recent study of depressive symptoms in youth, Cole and colleagues (2011) used item-response theory and found that psychomotor disturbance was more likely to occur at more severe as compared to more mild levels of depression. Thus, the presence and worsening of psychomotor disturbance in a middle adolescent may be a particularly important sign of problems and therefore should be evaluated further.
A second important finding of the present study was that sex differences emerged for the symptom trajectories of sad mood, sleep disturbance, low self-esteem/guilt, and problems with concentration/decision making. Specifically, girls showed increases in sad mood over time, and faster increases in both sleep disturbance and low self-esteem/guilt than boys. In contrast, concentration/decision making difficulties significantly worsened for boys, but did not change for girls. These sex differences in the trajectories of low self-esteem/guilt and concentration/decision making problems were particularly robust, remaining significant even after accounting for multiple tests. The sex differences in symptom trajectories observed here are consistent with studies showing increases in worthlessness among girls during adolescence (Roberts et al., 1995), greater sleep disruptions in adolescent girls than boys (Baji et al., 2009), and more problems with concentration and decision making among boys than girls (Fu-I & Wang, 2008).
Typically, studies have explored sex differences in the rates of new or recurrent depressive episodes (e.g., Lewinsohn et al., 2003) or in the presence or total number of depressive symptoms in girls versus boys. In contrast, the current study is the first to demonstrate sex differences in changes in the severity of individual depressive symptoms over time. Interestingly, at the first assessment in grade 6, girls and boys did not differ significantly in their levels of any of the symptoms of depression. An absence of significant sex differences in depressive symptoms prior to adolescence is consistent with existing literature (Costello, Foley, & Angold, 2006; Twenge & Nolen-Hoeksema, 2002). Thus, differences in initial symptom levels cannot account for the observed sex differences in symptom trajectories found here.
Some theories of depression suggest that cognitive vulnerabilities such as low self-esteem and negative attributions about the self increase the risk of depression, particularly in females (e.g., Cambron, Acitelli, & Pettit, 2009; Hankin & Abramson, 2001). The present finding of increases in the severity of low self-esteem in girls over adolescence is compatible with this perspective. Biological factors such as pubertal hormones are suggested to partially explain sex differences in depression (Angold, Costello, &Worthman, 1998; Oldehinkel, Verhulst, &Ormel, 2011). Recently, sleep disturbance has received increased attention as a possible transdiagnostic process underlying various forms of psychopathology (Harvey, Murray, Chandlar, & Soehner, 2011), but has not yet been a specific focus of theories about sex differences in depression. Overall, the current results highlight which depressive symptoms become more severe in girls during adolescence, and therefore should be assessed carefully.
A third key finding of the present study was that individual differences in adolescents’ symptom trajectories were predicted by family relationship variables. Adolescents’ perceptions of maternal psychological control in sixth grade significantly predicted faster growth in adolescents’ anhedonia. Additionally, the quality of the family environment as reported by mothers predicted trajectories of adolescents’ anhedonia, fatigue, and appetite/weight problems, such that these symptoms increased at a faster rate when families were low in cohesion and expressiveness and high in conflict. An association between family dysfunction and adolescent depression has been well-documented (see Cummings & Davies, 2010; Sagrestano, Paikoff, Holmbeck, & Fendrich, 2003; Sheeber et al., 2001). The current study demonstrated a significant link between family relationship quality and the progression of some individual depressive symptom levels over adolescence.
Notably, the trajectory of anhedonia, which is a core symptom of major depression, was significantly predicted by perceived parental behavior and the quality of the family environment, over and above level of maternal depression. Although boredom and disinterest are common in adolescents (Larson & Richards, 1991; Sharp, Caldwell, Graham, & Ridenour, 2006), the present study showed that the symptom of anhedonia became worse at a faster rate when maternal psychological control was high and the overall quality of family relationships was poor. This result is consistent with evidence of an inverse relation between parental control and adolescents’ motivation during their free time (Sharp et al., 2006). Given recent calls for more process-oriented research in the study of families and youth adjustment (Cummings & Davies, 2010), these findings suggest that a loss of interest, motivation, or pleasure in activities may be one pathway through which the family environment impacts adolescents’ mental health. For youth living with dysfunctional family relationships, a loss of interest or withdrawal from activities may be one way for teens to detach from the family and thereby decrease their exposure to a stressful home environment. Whereas avoidance might be adaptive in the short-term, such behavior can spill over to other domains of functioning (e.g., reduced school performance) resulting in more long-term impairment. Given the centrality of anhedonia in depressive disorder, special attention to this symptom in adolescents and further screening for indicators of family dysfunction when serious anhedonia is observed may be warranted.
A strength of the current study was the use of multiple informants and methods of assessment. In particular, adolescents’ depressive symptoms were based on clinical interviews, and measures of parenting and the family environment were based on reports from mothers and adolescents. Using information from multiple reporters reduced the likelihood that the observed results were due solely to mono-method reporter bias. Notably, mothers’ perceptions of family relationship quality predicted adolescents’ symptom trajectories, whereas adolescents’ perceptions did not. In contrast, adolescents’ but not mothers’ reports of maternal psychological control predicted faster increases in adolescents’ anhedonia over time.
Discrepancies in findings based on mother versus adolescent report are common (De Los Reyes, 2011; Tein, Roosa, & Michael, 1994). Differences between informants can be meaningful, reflecting each reporter’s unique perceptions of the family environment (Kraemer et al., 2003) and are not simply due to measurement error or one reporter being more valid than the other (De Los Reyes, 2011; De Los Reyes & Kazdin, 2008). Indeed, De Los Reyes and Kazdin (2008) argued that when information from multiple reporters is discrepant, “each provides reliable and valid information; it is not the case that some are ‘right’ and others ‘wrong’” (p. 48). The finding in the current study that adolescents’, but not their mothers’, reports about maternal psychological control were significantly related to teens’ depressive symptoms is consistent with previous research showing a stronger relation of children’s report of parenting to youths’ depression (e.g., Bruce et al., 2006). Thus, differences across informants highlight the importance of assessing both mothers’ and adolescents’ perceptions of the family and parenting when examining predictors of change in adolescents’ psychopathology over time.
Limitations of the study provide directions for future research. First, participants in this sample were primarily European American and represented children at varied risk for depression based on their mother’s depression history. The findings may not generalize to other racial or ethnic groups, to a purely community sample, or to adolescents whose parents have psychopathology other than depression. Nevertheless, the high risk research design is used frequently among researchers investigating depression in adolescents (e.g., Abela et al., 2005; Lau, Rijsdijk, Gregory, McGuffin, & Eley, 2007; Talati, Weissman, & Hamilton, 2013). Studying offspring of individuals with a particular disorder is recommended when trying to identify risk factors associated with the disorder, particularly prior to its onset (Ingram & Siegle, 2009). High risk samples also provide greater variability in depressive symptoms, thereby reducing problems with restriction of range that could impact the strength of the observed associations.
Second, although a strength and contribution of this prospective study was the longitudinal data collected across six years during adolescence, the data were correlational, and therefore no conclusions can be drawn about the directions of the observed relations. Within-person changes in individual symptoms could have been due to one or more unmeasured third variables that correlate with child age, such as changes in cognitive, emotional, biological, and social development that occur during this time. Similarly, the relation between the family variables and adolescents’ symptom trajectories may have been due to other unmeasured third variables (e.g., genes, stress), which could have affected both family processes and symptom trajectories. It also is possible that symptoms that occurred prior to the initial assessment, and thus were not measured here, may have contributed to the parenting and family relationship variables assessed in grade 6. Future research should explore other individual and contextual characteristics (e.g., quality of peer relationships) that also might predict which depressive symptoms worsen more quickly over time and contribute to individual differences in adolescents’ symptom trajectories.
Third, this study used family variables assessed in grade 6 to show that the parent-child relationship and the quality of family relationships in early adolescence predicted changes in adolescents’ depressive symptoms across time. Family relationships, however, also change during this developmental period (e.g., Kouros, Cummings, & Davies, 2010). Precisely how such changes in the family and in adolescents’ depressive symptoms may affect each other (e.g., bidirectional relations) needs to be explored. Fourth, this study examined maternal parenting behaviors. Future studies should assess the extent to which the parenting behaviors of fathers also predict the trajectories of individual depressive symptoms during adolescence.
In the current study, we could not test whether the slopes of the various symptom trajectories differed significantly from each other, given the data analytic technique used here. Thus, although we can conclude that eight symptoms of major depression followed linear growth trajectories and two followed a quadratic growth trajectory, we could not determine which symptoms changed more rapidly than others. Finally, although we tested linear and quadratic growth models, which are reasonable growth patterns during this six-year period, symptom trajectories quite possibly follow more complex patterns of change as adolescents enter adulthood, and therefore also should be explored in the future.
Despite recognition that studying individual symptoms is important for advancing theories about syndromes and disorders (Costello, 1992; Persons, 1986), investigations of individual symptoms of depression during adolescence, when risk for depression markedly rises, have been rare. The present study is one of the first to examine within-person changes in each individual symptom of depression from early- through mid-adolescence; notably, the findings revealed significant individual variability in each depressive symptom. Future research needs to identify the mechanisms underlying this variability. Discovering predictors of individual growth in symptoms then can guide the selection of targets for preventive interventions.
Finally, an important clinical implication of these findings is that interventions directed at improving parent-child relationships and the overall quality of the family environment may help alter the trajectories of some individual symptoms of depression in youth. Although targeting family processes has been recommended (Kaslow et al., 1994; Sheeber et al., 2001), evidence of the efficacy of such family-focused treatments for depression in adolescents is still limited (Restifo & Bögels, 2009). Early interventions that promote positive parent-child and family interactions may be beneficial not only in improving adolescent’s depressive symptoms, but also in preventing these symptoms from escalating into a full depressive episode. Results of this study showed that severity of the individual symptoms of depression increased during adolescence. Future research needs to determine at what point such increases in symptom severity begin to interfere with adolescents’ overall level of functioning, and also for which symptoms increasing severity predicts the subsequent onset of a full depressive episode.
Supplementary Material
Acknowledgments
Author Note: This work was supported in part by grants from the National Institute of Mental Health (R29 MH454580; K02 MH66249), NICHD Grant P30HD15052, and a Faculty Scholar Award (1214-88) and grant (173096) from the William T. Grant Foundation awarded to Garber. Kouros is a former trainee (2008-2011) on NIMH training grant T32-MH18921. We appreciate the cooperation of the Nashville Metropolitan School District, Drs. Binkley and Crouch, and we especially thank the parents and children who participated in the project.
Contributor Information
Chrystyna D. Kouros, Southern Methodist University
Judy Garber, Vanderbilt University.
References
- Abela JRZ, Hankin BL, Haigh EA, Adams P, Vinokuroff T, Trayhern L. Interpersonal vulnerability to depression in high-risk children: The role of insecure attachment and reassurance seeking. Journal of Clinical Child and Adolescent Psychology. 2005;34:182–192. doi: 10.1207/s15374424jccp3401_17. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-age Forms & Profiles. University of Vermont, Research Center for Children, Youth, and Families; Burlington: 2001. [Google Scholar]
- Angold A, Costello EJ, Worthman CM. Puberty and depression: The roles of age, pubertal status, and pubertal timing. Psychological Medicine. 1998;28:51–61. doi: 10.1017/s003329179700593x. [DOI] [PubMed] [Google Scholar]
- Aydin B, Oztütüncü F. Examination of adolescents’ negative thoughts, depressive mood, and family environment. Adolescence. 2001;36:77–83. [PubMed] [Google Scholar]
- Baji I, Lopez-Duran NL, Kovacs M, George CJ, Mayer L, Kapornai K, Vetro A. Age and sex analyses of somatic complaints and symptom presentation of childhood depression in a Hungarian clinical sample. Journal of Clinical Psychiatry. 2009;70:1467–1472. doi: 10.4088/JCP.08m04918. [DOI] [PubMed] [Google Scholar]
- Barber BK. Parental psychological control: Revisiting a neglected construct. Child Development. 1996;67:3296–3319. [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MC. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Beck AT, Ward CF, Mendelson M, Mock J, Erlbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:53–63. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling for false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. Series B (Methodological) 1995;57:289–300. [Google Scholar]
- Bhar SS, Gelfand LA, Schmid SP, Gallop R, DeRubeis RJ, Hollon SD, Beck AT. Sequence of improvement in depressive symptoms across cognitive therapy and pharmacotherapy. Journal of Affective Disorders. 2008;110:161–166. doi: 10.1016/j.jad.2007.12.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blodgett Salafia EH, Schaefer MK, Haugen EC. Connections between marital conflict and adolescent girls’ disordered eating: Parent-adolescent relationship quality as a mediator. Journal of Child and Family Studies. 2013:1–11. [Google Scholar]
- Bruce AE, Cole DA, Dallaire DH, Jacquez FM, Pineda AQ, LaGrange B. Relations of parenting and negative life events to cognitive diatheses for depression in children. Journal of Abnormal Child Psychology. 2006;34:321–333. doi: 10.1007/s10802-006-9019-x. [DOI] [PubMed] [Google Scholar]
- Cambron MJ, Acitelli LK, Pettit JW. Explaining gender differences in depression: An interpersonal contingent self-esteem perspective. Sex Roles. 2009;61:751–761. [Google Scholar]
- Cole DA, Tram JM, Martin JM, Hoffman KB, Ruiz MD, Jacquez FM, Maschman TL. Individual differences in the emergence of depressive symptoms in children and adolescents: A longitudinal investigation of parent and child reports. Journal of Abnormal Psychology. 2002;111:156–165. [PubMed] [Google Scholar]
- Cole DA, Cai L, Martin NC, Findling RL, Youngstrom EA, Garber J, Forehand R. Structure and measurement of depression in youths: Applying item response theory to clinical data. Psychological Assessment. 2011;23:819–833. doi: 10.1037/a0023518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compas BE, Ey S, Grant KE. Taxonomy, assessment, and diagnosis of depression during adolescence. Psychological Bulletin. 1993;114:323–344. doi: 10.1037/0033-2909.114.2.323. [DOI] [PubMed] [Google Scholar]
- Conradi HJ, Ormel J, de Jonge P. Presence of individual (residual) symptoms during depressive episodes and periods of remission: A 3-year prospective study. Psychological Medicine. 2011;41:1165–1174. doi: 10.1017/S0033291710001911. [DOI] [PubMed] [Google Scholar]
- Costello CG. Research on symptoms versus research on syndromes: Arguments in favor of allocating more research time to the study of symptoms. British Journal of Psychiatry. 1992;160:304–308. doi: 10.1192/bjp.160.3.304. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Foley DL, Angold A. 10-year research up date review: The epidemiology of child and adolescent psychiatric disorders: II. Developmental epidemiology. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:8–25. doi: 10.1097/01.chi.0000184929.41423.c0. [DOI] [PubMed] [Google Scholar]
- Cummings EM, Davies PT. Marital conflict and children: An emotional security perspective. Guilford Press; New York: 2010. [Google Scholar]
- De Los Reyes A. Introduction to special section: More than measurement error: Discovering meaning behind informant discrepancies in clinical assessments of children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2011;40:1–9. doi: 10.1080/15374416.2011.533405. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. When the evidence says, “yes, no, and maybe so”. Current Directions in Psychological Science. 2008;17:47–51. doi: 10.1111/j.1467-8721.2008.00546.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elgar FJ, Mills RSL, McGrath PJ, Waschbusch DA, Brownridge DA. Maternal and paternal depressive symptoms and child maladjustment: The mediating role of parental behavior. Journal of Abnormal Child Psychology. 2007;35:943–55. doi: 10.1007/s10802-007-9145-0. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Buckhalt JA, Mize J, Acebo C. Marital conflict and disruption of children’s sleep. Child Development. 2006;77:31–43. doi: 10.1111/j.1467-8624.2006.00854.x. [DOI] [PubMed] [Google Scholar]
- El-Sheikh M, Hinnant JB, Kelly RJ, Erath S. Maternal psychological control and child internalizing symptoms: Vulnerability and protective factors across bioregulatory and ecological domains. Journal of Child Psychology and Psychiatry. 2010;51:188–198. doi: 10.1111/j.1469-7610.2009.02140.x. [DOI] [PubMed] [Google Scholar]
- Fleming JE, Offord DR. Epidemiology of childhood depressive disorder: A critical review. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29:571–580. doi: 10.1097/00004583-199007000-00010. [DOI] [PubMed] [Google Scholar]
- Fournier JC, DeRubeis RJ, Hollon SD, Gallop R, Shelton RC, Amsterdam JD. Differential change in specific depressive symptoms during antidepressant medication or cognitive therapy. Behaviour Research and Therapy. 2013;51:392–398. doi: 10.1016/j.brat.2013.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu-I L, Wang YP. Comparison of demographic and clinical characteristics between children and adolescents with major depressive disorder. RevistaBrasileira de Psiquiatria. 2008;30:124–131. doi: 10.1590/s1516-44462008000200007. [DOI] [PubMed] [Google Scholar]
- Garber J, Keiley MK, Martin NC. Developmental trajectories of adolescents’ depressive symptoms: Predictors of change. Journal of Consulting and Clinical Psychology. 2002;70:79–95. doi: 10.1037//0022-006x.70.1.79. [DOI] [PubMed] [Google Scholar]
- Ge X, Lorenz FO, Conger RD, Elder GH, Jr., Simons RL. Trajectories of stressful life events and depressive symptoms during adolescence. Developmental Psychology. 1994;30:467–483. [Google Scholar]
- Glied S, Pine D. Consequences and correlates of adolescent depression. Archives of Pediatrics and Adolescent Medicine. 2002;156:1009–1014. doi: 10.1001/archpedi.156.10.1009. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY. Development of gender differences in depression: An elaborated cognitive vulnerability-transactional stress theory. Psychological Bulletin. 2001;127:773–796. doi: 10.1037/0033-2909.127.6.773. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Abramson LY, Moffitt TE, Silva PA, McGee R, Angell KE. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology. 1998;107:128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- Hankin BL, Fraley RC, Lahey BB, Waldman ID. Is depression best viewed as a continuum or discrete category? A taxometric analysis of childhood and adolescent depression in a population-based sample. Journal of Abnormal Psychology. 2005;114:96–110. doi: 10.1037/0021-843X.114.1.96. [DOI] [PubMed] [Google Scholar]
- Harvey AG, Murray G, Chandlar RA, Soehner A. Sleep disturbance as transdiagnostic: Consideration of neurobiological mechanisms. Clinical Psychology Review. 2011;31(2):225–235. doi: 10.1016/j.cpr.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. Four factor index of social status. Yale University, New Haven, CT: 1975. Unpublished manuscript. [Google Scholar]
- Ingram RE, Siegle GJ. Methodological issues in the study of depression. In: Gotlib IH, Hammen CL, editors. Handbook of depression. 2nd Guilford Press; New York: 2009. pp. 69–92. [Google Scholar]
- Jain S, Carmody TJ, Trivedi MH, Hughes C, Bernstein, Morris DW, Rush AJ. A psychometric evaluation of the CDRS and MADRS in assessing depressive symptoms in children. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1204–1212. doi: 10.1097/chi.0b013e3180cc2575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang KL, Livesly WJ, Taylor S, Stein MB, Moon EC. Heritability of individual depressive symptoms. Journal of Affective Disorders. 2004;80:125–133. doi: 10.1016/S0165-0327(03)00108-3. [DOI] [PubMed] [Google Scholar]
- Jester JM, Nigg JT, Adams K, Fitzgerald HE, Putter LI, Wong MM, Zucker RA. Inattention/hyperactivity and aggression from early childhood to adolescence: Heterogeneity of trajectories and differential influence of family environment characteristics. Development and Psychopathology. 2005;17:99–125. doi: 10.1017/50954579405050066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaslow NL, Deering CG, Racusin GR. Depressed children and their families. Clinical Psychology Review. 1994;14:39–59. [Google Scholar]
- Keller MC, Neale MC, Kendler KS. Association of different adverse life events with distinct patterns of depressive symptoms. American Journal of Psychiatry. 2007;164:1521–1529. doi: 10.1176/appi.ajp.2007.06091564. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Zachar P, Craver C. What kinds of things are psychiatric disorders? Psychological Medicine. 2011;41:1143–1150. doi: 10.1017/S0033291710001844. [DOI] [PubMed] [Google Scholar]
- Kouros CD, Cummings EM, Davies PT. Early trajectories of interparental conflict and externalizing problems as predictors of social competence in preadolescence. Development and Psychopathology. 2010;22:527–538. doi: 10.1017/S0954579410000258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. Rating scales to assess depression in school-aged children. Acta Peadopsychiatrica: International Journal of Child and Adolescent Psychiatry. 1981;46:305–315. [PubMed] [Google Scholar]
- Kovacs M. Gender and the course of major depressive disorder through adolescence in clinical referred youngsters. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1079–1085. doi: 10.1097/00004583-200109000-00017. [DOI] [PubMed] [Google Scholar]
- Kovacs M, Goldston D. Cognitive and social cognitive development of depression children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30:388–392. doi: 10.1097/00004583-199105000-00006. [DOI] [PubMed] [Google Scholar]
- Larson RW, Richards MH. Boredom in the middle school year: Blaming schools versus blaming students. American Journal of Education. 1991;99:418–443. [Google Scholar]
- Lau S, Kwok L. Relationship of family environment to adolescents’ depression and self-concept. Social Behavior and Personality. 2000;28:41–50. [Google Scholar]
- Lau JYF, Rijsdijk F, Gregory AM, McGuffin P, Eley TC. Pathways to childhood depressive symptoms: The role of social, cognitive, and genetic risk factors. Developmental Psychology. 2007;43:140–1414. doi: 10.1037/0012-1649.43.6.1402. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Pettit JW, Joiner TE, Seeley JR. The symptomatic expression of major depressive disorder in adolescents and young adults. Journal of Abnormal Psychology. 2003;112:244–252. doi: 10.1037/0021-843x.112.2.244. [DOI] [PubMed] [Google Scholar]
- Mayes TL, Bernstein IH, Haley CL, Kennard BD, Emslie J. Psychometric properties of the Children’s Depression Rating Scale-Revised in Adolescents. Journal of Child and Adolescent Psychopharmacology. 2010;20:513–516. doi: 10.1089/cap.2010.0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane AH, Bellissimo A, Norman GR. Family structure, family functioning, and adolescent well-being: The transcendent influence of parental style. Journal of Child Psychology and Psychiatry. 1995;36:847–864. doi: 10.1111/j.1469-7610.1995.tb01333.x. [DOI] [PubMed] [Google Scholar]
- Minor KL, Champion JE, Gotlib IH. Stability of DSM-IV criterion symptoms for major depressive disorder. Journal of Psychiatric Research. 2005;39:415–420. doi: 10.1016/j.jpsychires.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Mitchell J, McCauley E, Burke PM, Moss SJ. Phenomenology of depression in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1988;27:12–20. doi: 10.1097/00004583-198801000-00004. [DOI] [PubMed] [Google Scholar]
- Moos R, Moos B. Family Environment Scale manual: Development, applications, research. Third Consulting Psychologist Press; Palo Alta, CA: 1994. [Google Scholar]
- Oldehinkel AJ, Verhulst FC, Ormel J. Mental health problems during puberty: Tanner stage-related differences in specific symptoms. The TRAILS study. Journal of Adolescence. 2011;34:73–85. doi: 10.1016/j.adolescence.2010.01.010. [DOI] [PubMed] [Google Scholar]
- Persons JB. The advantage of studying psychological phenomena rather than psychiatric diagnoses. American Psychologist. 1986;41:1252–1260. doi: 10.1037//0003-066x.41.11.1252. [DOI] [PubMed] [Google Scholar]
- Pine DS, Cohen E, Cohen P, Brook J. Adolescent depressive symptoms as predictors of adult depression: Moodiness or mood disorder. American Journal of Psychiatry. 1999;156:133–135. doi: 10.1176/ajp.156.1.133. [DOI] [PubMed] [Google Scholar]
- Plunkett SW, Henry CS, Robinson LC, Behnke A, Falcon PC., III. Adolescent perceptions of parental behaviors, adolescent self-esteem, and adolescent depressed mood. Journal of Child and Family Studies. 2007;16:760–772. [Google Scholar]
- Poznanski E, Mokros HB, Grossman J, Freeman LN. Diagnostic criteria in childhood depression. The American Journal of Psychiatry. 1985;142:1168–1173. doi: 10.1176/ajp.142.10.1168. [DOI] [PubMed] [Google Scholar]
- Rabin AS, Kaslow NJ, Rehm LP. Changes in symptoms of depression during the course of therapy. Cognitive Therapy and Research. 1984;8:479–488. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd Sage; Thousand Oaks, CA: 2002. [Google Scholar]
- Restifo K, Bögels S. Family processes in the development of youth depression: Translating the evidence to treatment. Clinical Psychology Review. 2009;29:294–316. doi: 10.1016/j.cpr.2009.02.005. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Lewinsohn PM, Seeley JR. Symptoms of DSM-III-R major depression in adolescence: Evidence from an epidemiological survey. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:1608–1617. doi: 10.1097/00004583-199512000-00011. [DOI] [PubMed] [Google Scholar]
- Ruscio J, Ruscio AM. Informing the continuity controversy: A taxometric analysis of depression. Journal of Abnormal Psychology. 2000;109:473–487. [PubMed] [Google Scholar]
- Ryan ND, Puig-Antich J, Ambrosini P, Rabinovich H, Robinson D, Nelson B, Twomey J. The clinical picture of major depression in children and adolescents. Archives of General Psychiatry. 1987;44:854–861. doi: 10.1001/archpsyc.1987.01800220016003. [DOI] [PubMed] [Google Scholar]
- Sagrestano LM, Paikoff RL, Holmbeck GN, Fendrich M. A longitudinal examination of familiar risk factors for depression among inner-city African American adolescents. Journal of Family Psychology. 2003;17:108–120. [PubMed] [Google Scholar]
- Schaefer ES. Children’s reports of parental behavior: An inventory. Child Development. 1964;36:413–424. [PubMed] [Google Scholar]
- Schludermann E, Schludermann S. Replicability of factors in children’s reports of parent behavior (CRPBI) Journal of Psychology. 1970;76:239–249. [Google Scholar]
- Sharp EH, Caldwell LL, Graham JW, Ridenour TA. Individual motivation and parental influence on adolescents’ experiences of interest in free time: A longitudinal examination. Journal of Youth and Adolescence. 2006;35:359–372. [Google Scholar]
- Sheeber L, Hops H, Alpert A, Davis B, Andrews J. Family support and conflict: Prospective relations to adolescent depression. Journal of Abnormal Child Psychology. 1997;25:333–344. doi: 10.1023/a:1025768504415. [DOI] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Davis B. Family processes in adolescent depression. Clinical Child and Family Psychology Review. 2001;4:19–35. doi: 10.1023/a:1009524626436. [DOI] [PubMed] [Google Scholar]
- Silk JS, Morris AS, Kanaya T, Steinberg L. Psychological control and autonomy granting: Opposite ends of a continuum or distinct constructs? Journal of Research on Adolescence. 2003;13:113–128. [Google Scholar]
- Sorensen MJ, Nissan JB, Mors O, Thomson PH. Age and gender difference in depressive symptomatology and comorbidity: An incident sample of psychiatrically admitted children. Journal of Affective Disorders. 2005;84:85–91. doi: 10.1016/j.jad.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. User’s guide for the Structured Clinical Interview for DSM-III-R: SCID. American Psychiatric Association; Washington, DC: 1990. [Google Scholar]
- Talati A, Weissman MM, Hamilton SP. Using the high-risk family design to identify biomarkers for major depression. Philosophical Transactions of the Royal Society B: Biological Sciences. 2013;368:120–129. doi: 10.1098/rstb.2012.0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tein J, Roosa MW, Michaels M. Agreement between parent and child reports on parental behaviors. Journal of Marriage and Family. 1994;56:341–355. [Google Scholar]
- Twenge JM, Campbell WK. Age and birth cohort differences in self-esteem: A cross-temporal meta-analysis. Personality and Social Psychology Review. 2001;5:321–344. [Google Scholar]
- Twenge JM, Nolen-Hoeksema S. Age, gender, race, socioeconomic status, and birth cohort differences on the Child Depression Inventory: A meta-analysis. Journal of Abnormal Psychology. 2002;111:578–588. doi: 10.1037//0021-843x.111.4.578. [DOI] [PubMed] [Google Scholar]
- Weiss B, Garber J. Developmental differences in the phenomenology of depression. Development and Psychopathology. 2003;15:403–430. doi: 10.1017/s0954579403000221. [DOI] [PubMed] [Google Scholar]
- Yorbik O, Birmaher B, Axelson D, Williamson DE, Ryan ND. Clinical characteristics of depressive symptoms in children and adolescents with major depressive disorder. Journal of Clinical Psychiatry. 2004;65:1654–1659. doi: 10.4088/jcp.v65n1210. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.