Abstract
Objective
Despite a prevailing assumption that adult ADHD is a childhood-onset neurodevelopmental disorder, no prospective-longitudinal study has described the childhoods of the adult-ADHD population. We report follow-back analyses of ADHD cases diagnosed in adulthood, alongside follow-forward analyses of ADHD cases diagnosed in childhood, in one cohort.
Method
Participants belonged to a representative birth cohort of 1,037 individuals born in Dunedin, New Zealand in 1972-73 and followed to age 38, with 95% retention. Symptoms of ADHD, associated clinical features, comorbid disorders, neuropsychological deficits, GWAS-derived polygenic risk, and life impairment indicators were assessed. Data sources were participants, parents, teachers, informants, neuropsychological testing, and administrative records. Adult ADHD diagnoses used DSM5 criteria, apart from onset-age and cross-setting corroboration, which were study outcomes.
Results
As expected, the childhood-ADHD group showed 6% prevalence, male excess, childhood comorbid disorders, neurocognitive deficits, polygenic risk, and, despite having outgrown their ADHD diagnosis, residual adult life impairment. As expected, the adult-ADHD group showed 3% prevalence, gender balance, adult substance dependence, adult life impairment, and treatment contact. Unexpectedly, the childhood-ADHD and adult-ADHD groups comprised virtually non-overlapping sets; 90% of adult-ADHD cases lacked a history of childhood ADHD. Also unexpectedly, the adult-ADHD group did not show tested neuropsychological deficits in childhood or adulthood, nor did they show polygenic risk for childhood ADHD.
Conclusion
Findings raise the possibility that adults presenting with the ADHD symptom picture may not have a childhood-onset neurodevelopmental disorder. If this finding is replicated, then the disorder's place in the classification system must be reconsidered, and research must investigate the etiology of adult ADHD.
Introduction
“I didn't outgrow my ADHD. Did you? Your ADHD. Own it.”
-- Shane Victorino. Athlete and philanthropist.
(Advertisement on the website of Sports Illustrated, from the “ADHD Own it” campaign, www.ownyouradhd.com)
Diagnosing ADHD in adults draws much of its legitimacy from the assumption that it is the same disorder as childhood ADHD, with the same neurodevelopmental etiology, affecting the same individuals from childhood to adulthood. DSM-5 places adults' ADHD alongside children's ADHD within the category of neurodevelopmental disorders, and states, “ADHD begins in childhood” (pg.61). Consensus statements recommend treating adult ADHD on the grounds that it is a continuation from childhood ADHD(1) (http://www.nice.org.uk/guidance/cg72). However, to our knowledge the dual assumptions that adult ADHD is a neurodevelopmental disorder and begins in childhood remain untested by a prospective-longitudinal study of the childhoods of adults with ADHD.
A test is lacking because developmental research on adult ADHD has been limited to two designs, each with a shortcoming that limits inference about childhood origins of adult ADHD(2). Studies with the first design have followed up children with ADHD who were referred, diagnosed, and treated years ago(3-6). This design offers the advantage of prospective childhood data. However, clinical samples have the disadvantage of initial referral biases that limit inference about adult outcomes(7-10). Moreover, follow-ups of clinical childhood-ADHD samples have not yielded many participants who meet adult-ADHD criteria(3-6). Studies with the second design have surveyed adult ADHD in community samples(11-14). This design offers the advantage of substantial numbers of adult-ADHD cases who are unbiased by treatment seeking, as well as controls who represent the non-ADHD population. However these studies have the disadvantage that they must rely on participants' retrospective recall for assessing childhood onset and pre-adult etiological factors. Retrospective recall entails sources of invalidity that limit inference about the developmental origins of adults with disorder(15-17).
We report findings from a third design, a prospective longitudinal study of a representative birth cohort. Within this cohort, we undertook a follow-forward analysis of ADHD cases diagnosed in childhood and a follow-back analysis of ADHD cases diagnosed in adulthood. Our aim was to test whether the correlates of adult ADHD are the same as those of childhood ADHD(18).
Methods
Sample
Participants are members of the Dunedin Study, a longitudinal investigation of health and behavior in a complete birth cohort. Study members (N=1,037; 91% of eligible births; 52% male) were all individuals born between April 1972 and March 1973 in Dunedin, New Zealand, who were eligible based on residence in the province and who participated in the first assessment at age 3. The cohort represents the full range of socioeconomic status on NZ's South Island and matches the NZ National Health and Nutrition Survey on adult health indicators (e.g., BMI, smoking, GP visits)(19). Cohort members are primarily white; fewer than 7% self-identify as having partial non-Caucasian ancestry, matching the South Island. Assessments were carried out at birth and ages 3, 5, 7, 9, 11, 13, 15, 18, 21, 26, 32, and, most recently, 38 years, when 95% of the 1,007 study members still alive took part. At each assessment, each study member is brought to the research unit for a full day of interviews and examinations.
Childhood ADHD diagnosis
We used the Dunedin Study's group of children diagnosed with ADHD at ages 11, 13, and 15 years in 1984-1988, as previously reported(20-25). Symptoms were ascertained using the Diagnostic Interview Schedule for Children-Child Version at ages 11 and 13 by a child psychiatrist and at age 15 by trained interviewers. Symptoms were also ascertained at these ages through parent and teacher checklists. Symptom onset before age 7 as required by DSM-III was confirmed using brief parent/teacher checklists gathered at ages 5 and 7. Research diagnoses followed DSM-III and identified 61 children (see Supplementary Table 1).
Adult ADHD diagnosis
Symptoms were ascertained when participants were age 38 through private structured diagnostic interviews by trained interviewers with mental-health-related tertiary qualifications and clinical experience. Interviewers were blind to prior data. The reporting period was the past 12 months. Our interview included behavioral examples relevant for adults; 27 items(26-29) were used to operationalize the 18 symptoms of DSM-5 ADHD(30) (Supplementary Table 2). Because informant-confirmation and presence of ADHD symptoms in childhood are outcome measures in this article, they were not required for diagnosis. Research diagnoses otherwise followed DSM-5 and identified 31 adults (Supplementary Table 1).
Comparison controls were 920 participants never diagnosed with ADHD by the Study.
Correlates
This article reports more than fifty measures, selected because they are identified as correlates of ADHD by DSM-5. Most have been previously published from the Dunedin Study. Supplementary Table 1 describes each measure.
Results
Prevalence and continuity
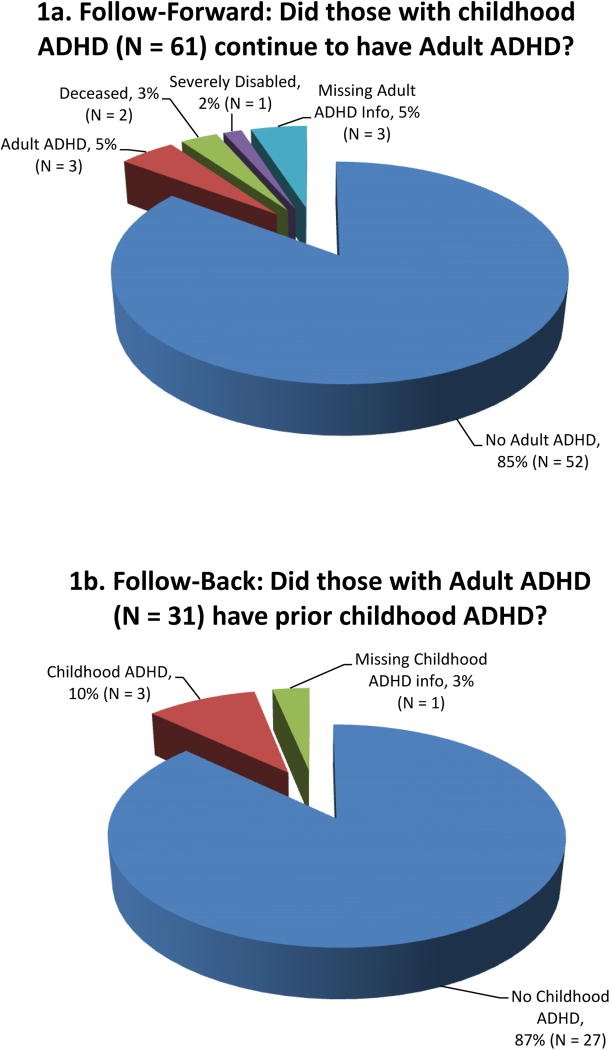
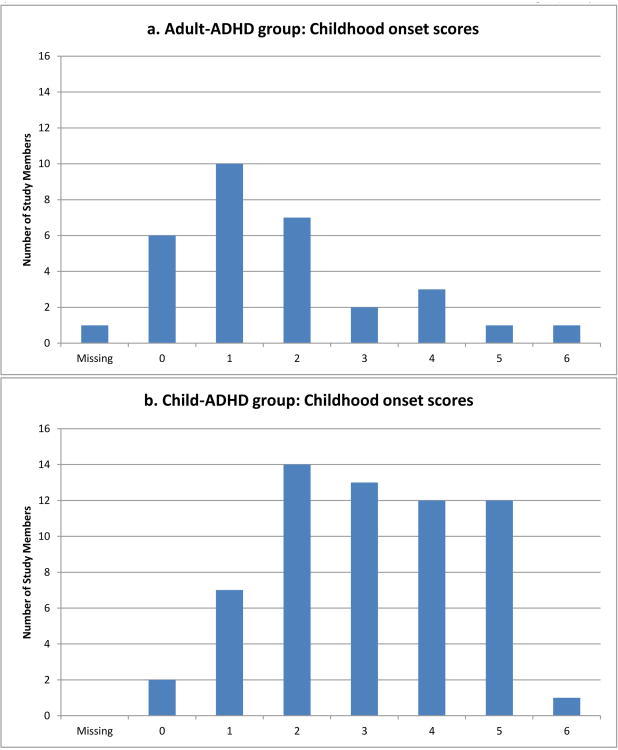
The cohort prevalence of ADHD was 6% in childhood and 3% at age 38 (Table 1), corresponding to previous estimates among children(31-33) and adults(34,35). Unexpectedly, childhood and adult diagnoses comprised virtually non-overlapping sets of individuals (Figure 1). Follow-forward from childhood-ADHD to adult-ADHD revealed that only 3 (5%) of the cohort's 61 childhood cases still met diagnostic criteria at age 38 (Figure 1a). It was not the case that many childhood-ADHD cases' adult symptom levels fell just below the 5-symptom adult diagnostic threshold (Figure 2). Follow-back showed these 3 individuals constituted only 10% of the cohort's 31 ADHD cases at age 38 (Figure 1b). These 3 individuals were retained in both the child-ADHD and adult-ADHD groups for subsequent analyses.
Table 1.
Diagnostic features of ADHD as diagnosed in childhood and adulthood in the Dunedin cohort.
| Control | Childhood ADHD | Child vs. Ctrl | Control | Adult ADHD | Adult vs. Ctrl | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | N | % | N | χ2 | p-value | % | N | % | N | χ2 | p-value | |
| Prevalence | 91.2 | 920 | 6.0 | 61 | -- | -- | 91.2 | 920 | 3.1 | 31 | -- | -- |
| % Male | 49.1 | 452 | 78.7 | 48 | 17.61 | < 0.001 | 49.1 | 452 | 61.3 | 19 | 1.74 | 0.187 |
| Measures taken in childhood | M | SD | M | SD | F | p-value | M | SD | M | SD | F | p-value |
|
|
||||||||||||
| ADHD symptom onset before age 12 (Age 5-11 years) | ||||||||||||
| Combined parent/teacher report, (z-score) | -0.11 | 0.89 | 1.60 | 1.02 | 184.52 | < 0.001 | -0.11 | 0.89 | 0.33 | 0.95 | 6.10 | 0.014 |
| Confirmation across settings at time of diagnosis (Age 11-13-15 years) | ||||||||||||
| Parent Report (z-score) | -0.09 | 0.90 | 1.18 | 1.29 | 95.40 | < 0.001 | -0.09 | 0.90 | 0.09 | 1.17 | 0.83 | 0.364 |
| Teacher Report (z-score) | -0.14 | 0.84 | 1.82 | 1.19 | 257.24 | < 0.001 | -0.14 | 0.84 | 0.31 | 0.94 | 6.63 | 0.010 |
| Measures taken in adulthood | M | SD | M | SD | F | p-value | M | SD | M | SD | F | p-value |
|
|
||||||||||||
| Confirmation by Informant-report (age 38 years) | ||||||||||||
| Inattention Symptoms (z-score) | -0.09 | 0.77 | 0.87 | 2.20 | 51.81 | < 0.001 | -0.09 | 0.77 | 0.90 | 1.83 | 41.87 | < 0.001 |
| Hyperactive/Impulsive Symptoms (z-score) | -0.08 | 0.84 | 0.81 | 1.86 | 48.20 | < 0.001 | -0.08 | 0.84 | 0.74 | 1.69 | 26.25 | < 0.001 |
| Parent Retrospective Recall in participants' thirties | % | N | % | N | χ2 | p-value | % | N | % | N | χ2 | p-value |
|
|
||||||||||||
| Study Member had ADHD or symptoms as a child | 4.0 | 35 | 22.8 | 13 | 19.51 | < 0.001 | 4.0 | 35 | 13.3 | 4 | 4.18 | 0.041 |
| Self-Reports at age 38 years | M | SD | M | SD | F | p-value | M | SD | M | SD | F | p-value |
|
|
||||||||||||
| Life Impairment by ADHD (z-score) | -0.09 | 0.87 | 0.29 | 1.23 | 10.36 | < 0.001 | -0.09 | 0.87 | 2.26 | 1.45 | 209.35 | < 0.001 |
| Life Satisfaction (z-score) | 0.05 | 0.97 | -0.37 | 1.01 | 8.07 | 0.005 | 0.05 | 0.97 | -0.87 | 1.33 | 24.98 | < 0.001 |
| % | N | % | N | χ2 | p-value | % | N | % | N | χ2 | p-value | |
|
|
||||||||||||
| Waste time searching for lost or forgotten things (%) | 6.5 | 56 | 9.1 | 5 | 1.22 | 0.270 | 6.5 | 56 | 48.4 | 15 | 47.18 | < 0.001 |
| Underachiever, not living up to potential (%) | 6.2 | 54 | 5.5 | 3 | 0.03 | 0.861 | 6.2 | 54 | 45.2 | 14 | 42.45 | < 0.001 |
| Exhausting or draining to others (%) | 2.0 | 17 | 3.6 | 2 | 0.63 | 0.428 | 2.0 | 17 | 29.0 | 9 | 42.47 | < 0.001 |
| Accidents or injuries from over-doing it (%) | 1.2 | 10 | 3.6 | 2 | 1.85 | 0.174 | 1.2 | 10 | 19.4 | 6 | 28.91 | < 0.001 |
| Drive too fast, excessive speeding (%) | 3.5 | 30 | 3.6 | 2 | 0.05 | 0.832 | 3.5 | 30 | 22.6 | 7 | 18.71 | < 0.001 |
| Tailgate cars in front, follow too closely (%) | 2.5 | 22 | 5.5 | 3 | 1.29 | 0.256 | 2.5 | 22 | 32.3 | 10 | 43.07 | < 0.001 |
| Medication for ADHD (%), Ages 21-38 | 0.1 | 1 | 1.8 | 1 | 4.11 | 0.043 | 0.1 | 1 | 12.9 | 4 | 21.86 | < 0.001 |
Notes: Statistical tests included sex as a covariate. M=mean, SD=Standard deviation.
Figure 1.
Childhood-ADHD and adult-ADHD groups comprised virtually non-overlapping sets.
Figure 2.
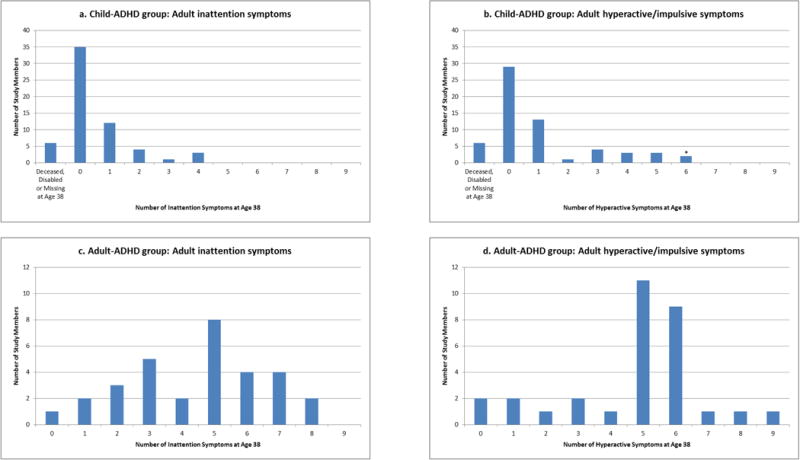
The adult-ADHD and child-ADHD groups did not overlap. This was not simply because many childhood-ADHD cases just missed the 5-symptom threshold for adult diagnosis. Panels a and b show how many childhood-ADHD cases (N = 61) had each level of adult-ADHD inattention and hyperactive/impulsive symptoms. For comparison, panels c and d show how many adult-ADHD cases (N = 31) had each level of adult symptoms. (3 individuals who had ADHD as a child and as an adult are included in all graphs.) * 2 Study members with current schizophrenia at age 38 were excluded from the adult-ADHD diagnosis, per DSM5.
Sex distribution (Table 1)
Childhood-ADHD cases were predominantly male. Among adult-ADHD cases there was no significant sex difference. All subsequent significance tests included sex as a covariate.
Prospective onset before age 12 (Table 1)
Parent/teacher reports from ages 5, 7, 9, and 11 years averaged for this article documented extremely elevated symptoms before age 12 (as required by DSM5) for the childhood-ADHD group (Effect Size(ES)=1.60SD), but only mildly elevated symptoms for the adult-ADHD group (ES=.33SD). For example, few adult-ADHD cases scored at least one symptom rated “2=certainly” by their elementary-school teachers (Figure 3), whereas most childhood-ADHD cases had more than one symptom rated “2=certainly”.
Figure 3.
Few adult-ADHD cases had childhood onset before age 12 years. We used the available items rated by teachers at child ages 5, 7, 9, and 11: “very restless, often running about or jumping up and down, hardly ever still,” “squirmy fidgety child,” “poor concentration, short attention span.” Items were rated 0=does not apply, 1=applies somewhat, or 2=certainly applies, yielding a range from 0 to 6. Ratings were summed at each age, then averaged across ages 5, 7, 9, and 11. Panel a shows few adult-ADHD group members (N = 31) scored at least one symptom rated “2=certainly” by their teachers. For comparison, panel b shows that most childhood-ADHD group members (N = 61) scored more than one symptom rated “2=certainly.” (3 individuals who had ADHD as a child and as an adult are included in all graphs.)
Cross-setting confirmation in childhood (Table 1)
As expected, childhood-ADHD cases' mean symptom scores were extremely elevated according to parents (ES=1.18SD) and teachers (ES=1.82SD) at the time of diagnosis (ages 11,13,15). In contrast, adult-ADHD cases' mean symptom scores were not different from controls according to parents (ES=.09SD), and were only modestly elevated according to teachers (ES=.31SD).
Cross-setting confirmation in adulthood (Table 1)
At age 38, symptom checklists were mailed to informants who knew the participant well. According to informants, as adults the childhood-ADHD group had significantly elevated symptoms of inattention (ES=.87SD) and hyperactivity/impulsivity (ES=.81SD). Informants also reported elevated symptoms for the adult-ADHD group (ES=.90SD, .74SD).
Retrospective parental recall of onset before age 12 years (Table 1)
Many adult patients rely on their parents' memories of childhood symptom onset. Among childhood-ADHD cases, only 22% had parents who recalled that their child had core ADHD symptoms or was diagnosed with ADHD. Thus 78% of documented childhood-ADHD cases were forgotten twenty years later. Also, implausibly, 35 controls' parents recalled evidence that their child had had ADHD.
ADHD-associated self-perceived adult impairment (Table 1)
At age 38, on a 1-5 interference scale, former-ADHD children reported that ADHD symptoms were impairing their adult work and family lives, a significant albeit modest difference (ES=.29SD). Childhood-ADHD cases were also significantly less satisfied with life than were controls. However, the childhood-ADHD group denied problems such as being disorganised, under-achieving, exhausting others, over-doing it, or risky driving.
The impairment story was worse for ADHD adults. They reported markedly elevated impairment as a result of ADHD-associated problems (ES=2.26SD), felt less satisfied with their lives, and reported problems stemming from being disorganised, under-achieving, exhausting or draining others, having accidents from over-doing it, and risky driving (tailgating, speeding).
ADHD medication (Table 1)
This cohort was unmedicated for ADHD during childhood, as prescribing was extremely rare in NZ in the 1970's-80's. ADHD medication has remained rare among NZ adults. ADHD medication (methylphenidate, d-amphetamine, atomoxetine) was ever used during adulthood by only 5 persons; 1 control participant with illicit methylphenidate use, and 4 adult-ADHD participants, of whom 1 had also had childhood ADHD. (Only 1 childhood-ADHD and 2 adult-ADHD cases took ADHD medication at the time of the age-38 assessment.)
Mental health in childhood (Table 2)
Table 2.
Mental health comorbidity associated with ADHD as diagnosed in childhood and adulthood.
| Control | Childhood ADHD | Child vs. Ctrl | Control | Adult ADHD | Adult vs. Ctrl | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | N | % | N | χ2 | p-value | % | N | % | N | χ2 | p-value | |
| Measures Taken in Childhood | ||||||||||||
| Conduct Disorder Diagnosis | 14.4 | 128 | 59.0 | 36 | 49.97 | < 0.001 | 14.4 | 128 | 31.0 | 9 | 5.08 | 0.024 |
| Depression Diagnosis | 4.6 | 41 | 27.9 | 17 | 42.41 | < 0.001 | 4.6 | 41 | 0.0 | 0 | 0.50 | 0.481 |
| Any Anxiety Diagnosis | 18.4 | 163 | 54.1 | 33 | 43.83 | < 0.001 | 18.4 | 163 | 13.8 | 4 | 0.29 | 0.589 |
| Measures Taken in Adulthood | ||||||||||||
| Adult Diagnoses | ||||||||||||
| PTSD a | 14.4 | 132 | 24.6 | 15 | 7.17 | 0.007 | 14.4 | 132 | 22.6 | 7 | 2.11 | 0.147 |
| Attempted Suicide a | 12.4 | 114 | 23.0 | 14 | 7.13 | 0.008 | 12.4 | 114 | 19.4 | 6 | 1.58 | 0.209 |
| Mania a | 1.0 | 9 | 0.0 | 0 | 0.00 | 0.992 | 1.0 | 9 | 0.0 | 0 | 0.09 | 0.765 |
| Major Depression c | 21.7 | 197 | 25.0 | 15 | 2.06 | 0.151 | 21.7 | 197 | 32.3 | 10 | 2.86 | 0.091 |
| Any Anxiety Disorder c | 27.6 | 251 | 31.7 | 19 | 2.83 | 0.093 | 27.6 | 251 | 32.3 | 10 | 0.75 | 0.386 |
| Substance Dependence (Alcohol, Drugs, Marijuana) c | 20.7 | 188 | 30.0 | 18 | 0.69 | 0.405 | 20.7 | 188 | 48.4 | 15 | 10.47 | 0.001 |
| Tobacco Dependence c | 23.4 | 212 | 28.3 | 17 | 0.86 | 0.353 | 23.4 | 212 | 38.7 | 12 | 3.90 | 0.048 |
| Medications for non-ADHD Mental Health Problem b | 14.0 | 122 | 25.5 | 14 | 7.61 | 0.006 | 14.0 | 122 | 48.4 | 15 | 23.65 | < 0.001 |
| Mental Health Treatment Contact b | 46.2 | 401 | 49.1 | 27 | 2.18 | 0.140 | 46.2 | 401 | 70.0 | 21 | 8.37 | 0.004 |
Note: Statistical test included sex as a covariate
Lifetime diagnosis;
Between ages 21-38;
Persistent diagnosis (2+ of 5 assessment time points)
As expected, childhood-ADHD cases had significantly elevated conduct disorder, depression, and anxiety as children. Although the adult ADHD group shared a childhood history of conduct disorder, this link was more prominent among childhood-ADHD cases (59%) than among adult-ADHD cases (31%).
Mental health in adulthood (Table 2)
Neither the childhood-ADHD nor the adult-ADHD group had significantly elevated rates of mania, depression, or anxiety disorders as adults. Adult-ADHD cases had significantly elevated rates as adults of persistently diagnosed dependence on alcohol, cannabis, or other drugs (48.4%), and persistent tobacco dependence (38.7%). Of adult-ADHD cases, between ages 21 and 38 a significant 70% reported contact with a professional for a mental-health problem (general practitioner, psychologist, psychiatrist, addiction treatment) and 48.4% of them had taken medication for a problem other than ADHD, in this order: depression, anxiety, psychological trauma, detox/substance treatment, and eating disorder.
Cognitive assessments in childhood (Table 3)
Table 3.
Neuropsychological assessment results associated with ADHD as diagnosed in childhood and adulthood.
| Control | Childhood ADHD | Child vs. Ctrl | Control | Adult ADHD | Adult vs. Ctrl | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | F | p-value | M | SD | M | SD | F | p-value | |
| Measures taken in childhood | ||||||||||||
| Brain Integrity, Age 3 (z-score) | 0.06 | 0.93 | -0.55 | 1.24 | 20.86 | < 0.001 | 0.06 | 0.93 | -0.13 | 0.94 | 1.09 | 0.296 |
| WISC-R Full-Scale IQ, Ages 7-11 (IQ units) | 101.12 | 13.79 | 89.43 | 16.17 | 44.43 | < 0.001 | 101.12 | 13.79 | 97.80 | 14.69 | 1.91 | 0.167 |
| Reading, Ages 7-11 (z-score) | 0.09 | 0.95 | -0.87 | 0.95 | 47.34 | < 0.001 | 0.09 | 0.95 | -0.38 | 0.97 | 5.91 | 0.015 |
| Trail-Making B, Age 13 (seconds) | 35.95 | 15.81 | 48.60 | 25.44 | 24.81 | < 0.001 | 35.95 | 15.81 | 35.12 | 10.47 | 0.05 | 0.823 |
| Rey Auditory Verbal, Delayed Recall, Age 13 (z-score) | 0.06 | 0.97 | -0.69 | 1.12 | 20.76 | < 0.001 | 0.06 | 0.97 | -0.21 | 1.04 | 1.23 | 0.268 |
| Measures taken in adulthood at age 38 | ||||||||||||
| WAIS-IV (IQ units) | ||||||||||||
| Full Scale IQ | 100.77 | 14.56 | 89.96 | 16.24 | 30.47 | < 0.001 | 100.77 | 14.56 | 96.94 | 18.14 | 2.29 | 0.131 |
| Verbal Comprehension Index | 100.57 | 14.79 | 91.80 | 15.58 | 22.09 | < 0.001 | 100.57 | 14.79 | 99.00 | 15.92 | 0.56 | 0.454 |
| Perceptual Reasoning Index | 100.60 | 14.65 | 93.43 | 17.03 | 15.17 | < 0.001 | 100.60 | 14.65 | 95.31 | 17.58 | 4.37 | 0.037 |
| Working Memory Index | 100.61 | 14.72 | 91.44 | 14.94 | 25.28 | < 0.001 | 100.61 | 14.72 | 98.68 | 18.04 | 0.84 | 0.360 |
| Processing Speed Index | 100.76 | 14.76 | 90.53 | 15.32 | 16.33 | < 0.001 | 100.76 | 14.76 | 96.45 | 14.96 | 1.62 | 0.203 |
| CANTAB Rapid Visual Processing | ||||||||||||
| A-Prime (Vigilance) (z-score) | 0.05 | 0.96 | -0.69 | 1.26 | 28.37 | < 0.001 | 0.05 | 0.96 | -0.23 | 1.18 | 2.28 | 0.132 |
| Total False Alarms (z-score) | -0.04 | 0.95 | 0.42 | 1.46 | 12.09 | < 0.001 | -0.04 | 0.95 | 0.37 | 1.15 | 5.13 | 0.024 |
| Trail-Making B (seconds) | 63.44 | 20.15 | 77.56 | 25.87 | 20.35 | < 0.001 | 63.44 | 20.15 | 69.87 | 22.78 | 2.55 | 0.111 |
| Rey Auditory Verbal, Delayed Recall (z-score) | 0.04 | 0.98 | -0.53 | 1.12 | 8.45 | 0.004 | 0.04 | 0.98 | -0.09 | 1.15 | 0.07 | 0.789 |
| Self-Reported Cognitive Complaints (z-scores) | -0.06 | 0.95 | 0.14 | 0.96 | 5.57 | 0.019 | -0.06 | 0.95 | 1.62 | 1.22 | 98.56 | < 0.001 |
| GWAS-discovered childhood-ADHD polygenic risk | ||||||||||||
| Polygenic risk score (z-score) | -0.01 | 0.98 | 0.28 | 1.00 | 4.14 | 0.042 | -0.01 | 0.98 | -0.08 | 0.98 | 0.12 | 0.728 |
Notes: Statistical tests included sex as a covariate. Childhood ADHD polygenic risk was analysed in Non-Maori Study members, N = 839 for control, N = 53 for Child ADHD group, N = 28 for Adult ADHD group; means and statistical tests were also adjusted for the potential of ethnic stratification. M=mean, SD=Standard deviation.
As expected, childhood-ADHD cases showed significant cognitive deficits. As a group, they scored .55SD below the norm on our composite measure of brain integrity at age 3. As school-aged children their IQ scores were 10 points below the norm. They exhibited deficits on reading achievement, the Trail-making-B test, a commonly used test of executive control, and on verbal-learning delayed recall. In comparison, adult-ADHD cases had evidenced no significant tested cognitive deficits as children, apart from mild reading delay.
Cognitive assessments in adulthood (Table 3)
Although childhood-ADHD cases may have out-grown their ADHD diagnosis, they did not out-grow their cognitive difficulties. At age 38 their IQs remained 10 points below the norm. Childhood-ADHD cases also showed a deficit on the CANTAB-Rapid Visual Processing “continuous performance test”; they earned under-par scores for attentional vigilance and made more false-alarm errors from jumping to respond too soon. They still had significant deficits on Trail-making-B and verbal-learning recall. Despite these tested deficits, childhood-ADHD cases self-reported only mildly elevated cognitive complaints (ES=.14SD).
In comparison, adult-ADHD cases had relatively few tested cognitive deficits as adults, apart from scoring significantly beneath controls on perceptual reasoning, and making more false alarms on the Rapid Visual Processing test. Despite their lack of tested deficits in childhood and relatively mild tested deficits in adulthood, our adult-ADHD cases reported many subjective cognitive complaints, scoring 1.62SD above the norm (and 1.48SD worse than childhood-ADHD cases).
Polygenic risk (Table 3)
A genome-wide polygenic risk score derived from genome-wide-association studies of childhood ADHD was significantly elevated in the childhood-ADHD group, but not in the adult-ADHD group.
Life functioning in adulthood (Table 4)
Table 4.
Adult life functioning associated with ADHD as diagnosed in childhood and adulthood.
| Control | Childhood ADHD | Child vs. Ctrl | Control | Adult ADHD | Adult vs. Ctrl | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | N | % | N | χ2 | p-value | % | N | % | N | χ2 | p-value | |
|
|
||||||||||||
| University Degree (%), age 38 | 30.3 | 263 | 10.9 | 6 | 6.65 | 0.010 | 30.3 | 263 | 20.0 | 6 | 1.14 | 0.286 |
| M | SD | M | SD | F | p-value | M | SD | M | SD | F | p-value | |
|
|
||||||||||||
| Personal Income (z-score), age 38 | 0.02 | 1.01 | -0.21 | 0.89 | 15.60 | < 0.001 | 0.02 | 1.01 | -0.14 | 0.90 | 2.62 | 0.106 |
| Savings Behavior (z-score), age 38 | 0.03 | 0.99 | -0.22 | 1.10 | 3.50 | 0.062 | 0.03 | 0.99 | -0.50 | 1.09 | 8.67 | 0.003 |
| Troubles w/ Debt, Cash Flow (z-score), age 38 | -0.05 | 0.93 | 0.50 | 1.39 | 15.30 | < 0.001 | -0.05 | 0.93 | 0.70 | 1.53 | 18.19 | < 0.001 |
| Credit Scores, age 33-38 a | 682.87 | 161.92 | 590.38 | 218.36 | 11.63 | < 0.001 | 682.87 | 161.92 | 597.07 | 198.13 | 5.89 | 0.016 |
| M | SD | M | SD | z | p-value | M | SD | M | SD | z | p-value | |
|
|
||||||||||||
| Months Receiving Government Benefits, age 21-38 a | 22.15 | 42.02 | 57.13 | 69.39 | 20.88 | < 0.001 | 22.15 | 42.02 | 39.63 | 57.77 | 6.87 | 0.009 |
| N of Accident Injury Insurance Claims, age 21-38 a | 6.52 | 6.93 | 10.91 | 13.23 | 1.92 | 0.056 | 6.52 | 6.93 | 9.94 | 9.47 | 2.94 | 0.003 |
| Number of Adult Criminal Convictions, age 18-38 a | 1.71 | 6.95 | 8.88 | 19.44 | 2.70 | 0.007 | 1.71 | 6.95 | 5.29 | 14.81 | 1.36 | 0.174 |
| Number of Driving-Related Convictions, age 18-38 a | 0.45 | 1.70 | 1.38 | 3.57 | 1.77 | 0.078 | 0.45 | 1.70 | 0.87 | 1.96 | 1.04 | 0.300 |
Notes: Statistical tests included sex as a covariate. M=mean, SD=Standard deviation.
Statistical tests also control for months spent living in NZ
Compared to controls, significantly fewer childhood-ADHD cases completed a university degree, and they reported significantly lower incomes, somewhat fewer saving behaviors, and more troubles with debt/cashflow. Administrative records revealed that childhood-ADHD cases had significantly lower credit ratings, longer duration of social welfare benefit receipt, more injury-related insurance claims, and more criminal convictions.
Although adult-ADHD cases did not differ from controls on university education or income, they reported significantly fewer saving behaviors and more troubles with debt/cashflow. Administrative records revealed that adult-ADHD cases also had significantly lower credit ratings, longer duration of social welfare benefit receipt, and more injury-related insurance claims than controls. Convictions were elevated, but did not reach significance.
Discussion
In 2013, DSM-5 newly formalized the criteria for diagnosing ADHD in adults. DSM-5, clinicians, and the public presume that adult ADHD is the same childhood-onset neurodevelopmental disorder as childhood ADHD, but is it? To answer this question, we described in parallel the life course of individuals who met criteria for the familiar diagnosis of childhood ADHD and the newer diagnosis of adult ADHD. Like previous follow-ups of individuals with childhood ADHD, we found that childhood-ADHD individuals tended to out-grow the full ADHD diagnosis but continued to experience difficulties in life adjustment into their thirties. Like previous surveys of adults with ADHD, we found these adults showed ample evidence of impairment warranting clinical intervention. However, our follow-back revealed that, in this cohort, this adult syndrome did not represent a continuation from a childhood-onset neurodevelopmental disorder. To our knowledge this is the first follow-back prospective study of the childhood origins of individuals diagnosed with DSM-5 adult ADHD; thus, our novel finding must be evaluated in other studies.
Our study offered certain design advantages. Our four-decade study supported both follow-forward and follow-back analyses of a representative birth cohort, in which ADHD cases were ascertained without bias by referral or treatment. Participants' self-reports could be supplemented by independent sources: parents, teachers, informants, formal cognitive testing, and administrative records.
This study also has limitations. First, as the findings were not hypothesized in advance, replication in other cohorts is imperative. Second, childhood ADHD was diagnosed using the then-available DSM-III, but that is inevitable. Third, as ADHD was deemed a childhood-only disorder by DSM-IIIR our study did not assess ADHD during the participants' twenties. Thus, we were unable to trace the decline in symptoms for childhood cases, or the emergence of symptoms for adult cases. Fourth, our adult-ADHD group was small, which limited statistical power and our ability to examine heterogeneity within this group. However, the non-significant effect sizes were very small, suggesting that lack of power was not the reason for lack of significant differences. Fifth, personality disorder was not ascertained. Sixth, we lacked neuroimaging data to test the neurodevelopmental hypothesis, but there is no multi-decade longitudinal neuroimaging study of a population-representative cohort. Finally, the fact that our cohort's ADHD cases were unbiased by clinical referral and largely untreated with ADHD medications is an advantage for studying the natural history of ADHD, but may be a disadvantage for clinicians needing an evidence base that generalizes to patients in treatment.
The childhood-ADHD group
The Dunedin cohort's childhood-ADHD cases conformed to expectations derived from past research about childhood ADHD(30). This conformity allays concerns about the use of this cohort for researching ADHD. The prevalence was 6% and most were boys. Childhood ADHD cases had the expected comorbid conditions, particularly conduct and anxiety disorders. They showed elevated polygenic risks identified in prior childhood-ADHD GWAS. They exhibited neuro-cognitive dysfunctions as young as age 3 years, and had poor cognitive test performance, consistent with the conceptualization of ADHD as a neurodevelopmental disorder(36,37).
As 38-year-old adults, the former-ADHD children also conformed to expectations derived from prior studies that have followed ADHD children to adulthood(5,18). Virtually all of them (except 3) no longer met full diagnostic criteria for ADHD. This is consistent with a prior meta-analysis reporting that only 16% of childhood-ADHD cases continue to meet diagnostic criteria into their twenties and this percentage continues declining thereafter(38). It was not the case that the group had symptoms just below the adult diagnostic threshold. Despite having shed their childhood diagnoses, they retained the neuropsychological deficits that signify ADHD as a neurodevelopmental disorder. Consistent with these deficits, few had managed a university degree and they were struggling financially. Many had experienced PTSD, a suicide attempt, injury-related insurance claims or adult criminal convictions. This former-ADHD group rated ADHD-symptoms as still exerting a mildly impairing effect on their adult lives.
The adult-ADHD group
The Dunedin cohort's adult-ADHD cases met DSM-5 diagnostic criterion A, five or more symptoms of inattention or of hyperactivity/impulsivity, in our interview. The group met criterion C, symptoms in two or more settings, through elevated symptom reports by informants. The group met criterion D, interference, as they rated their life impairment as extreme.
It must be said that we did not interview the participants about criterion B, onset before age 12, because retrospective recall of psychiatric symptoms across decades has poor validity, and yields false-negative reports of childhood-onset hyperactivity(39-41). Consistent with this, when parents were interviewed in our study members' thirties, 78% of childhood-ADHD cases' parents forgot their study member's onset before age 12 (despite having reported the child's symptoms at ages 5, 7, 9, and 11). Retrospective recall also yields false positives; 35 control-group cases were recalled by their parents as having childhood ADHD. Considering this invalidity, an alternative is to require prospective evidence of pre-age-12 symptoms (Fig. 3); doing so would yield a near-zero prevalence of full-DSM5-criterion adult ADHD (.03%). We suspect that, like us, clinicians often ignore the childhood-onset criterion for adult patients needing treatment.
With DSM-5 diagnoses made based on symptoms, we obtained a prevalence rate of about 3% and a near-equal sex balance, matching prior cross-sectional surveys of adult ADHD. However, contrary to our expectations we did not find evidence that adult ADHD so defined is a childhood-onset neurodevelopmental disorder. Our first hint was the elevated prevalence in women, which has been reported before, and differs from childhood ADHD. Second, when we exploited our study's prospective design, we found evidence that almost no ADHD-adults so diagnosed had ADHD as children. Moreover, these ADHD adults as a group had not had symptoms just below the threshold at the time of diagnosis; according to their parents' reports, their mean symptom score was normative then. Although teacher symptom ratings were mildly elevated, the elevation represented a level far below the threshold for diagnosis.
Third, and most surprising, as a group the adult-ADHD cases lacked the childhood neuropsychological deficits that are the signature of ADHD as a neurodevelopmental disorder. For example, their mean WISC-R IQ was only 2 IQ points below the population norm of 100. When re-tested at age 38, their mean WAIS-IV IQ was 3 points below the norm. They did not differ from controls on the WAIS-IV Working Memory index or a continuous-performance test of attentional vigilance, which are generally considered cardinal deficits in individuals with ADHD(42). Meta-analyses have reported wider cognitive differences between ADHD-adults and controls(43,44) but it should be remembered that studies in these meta-analyses were biased toward finding larger differences because they compared clinical ADHD patients versus controls who did not represent the range of cognitive abilities in the non-ADHD population(44,45). Despite lacking tested neuropsychological deficits, the adult-ADHD group reported elevated cognitive complaints in our interview, saying, for example, that they forget what they came to the shop to buy, can't think when the TV or radio is on, or have word-finding difficulty. This discrepancy between test scores and subjective complaints has been reported in adult ADHD before and is not yet understood(46,47) .
Treatment need
Our data suggest the possibility that adult ADHD may not be the same disorder as childhood ADHD. Does this imply that adults presenting with the ADHD symptom picture do not need treatment? Unequivocally no. Life interference that warrants treatment was independently confirmed by official records of injury-related insurance claims and low credit ratings. Treatment need was also indicated by the adults' self-reports that their lives tend to be marred by dissatisfaction, everyday cognitive problems, and troubles with debt, cash-flow and inadequate saving behaviors, and they tended to believe that they waste time because of being disorganized, have failed to fulfil their potential, are exhausting or draining to others, have accidents from over-doing it, and take risks while driving by tailgating and speeding. Interestingly, 70% of these adults reported mental health treatment contact during their twenties and thirties. As such, they were getting professional attention, but not the treatment-of-choice for ADHD; only 13% had been prescribed methylphenidate or atomoxetine. To be fair to their doctors, applying the ADHD diagnosis to adults was only highlighted by DSM-5 in 2013, after we made our diagnoses. In any case, we found ample evidence of treatment need, and treatment contact.
Diagnostic possibilities
The remaining question is, if these impaired adults do not have the neurodevelopmental disorder of ADHD, what do they have? At 38, this cohort is too young for prodromal dementia. The possibility of malingering has been raised(48,49), but this can be discarded as Dunedin Study members lack any motive to fabricate their reports to us.
A second possibility is that they should not have been diagnosed with ADHD, because their symptoms and impairment might be better explained by another disorder (exclusionary criterion E). Although they did not have elevated rates of depression or anxiety from ages 21-38, we know that as adults nearly half of them had persistent substance dependence as diagnosed on multiple occasions by the Study. It is tempting to conclude that adult ADHD is secondary to substance abuse. Unfortunately, our data cannot resolve whether substance abuse led to ADHD symptoms or adult-ADHD symptoms antedated substance abuse. Disentangling which symptoms are primary versus secondary is likewise difficult in clinical practice. Ubiquitous comorbidity for adults with ADHD has been reported before(12), suggesting the hypothesis that ADHD symptoms in adults in their thirties might be the psychiatric equivalent of fever, a syndrome that accompanies many different illnesses and is diagnostically non-specific, but signals treatment need. However, 55% of adult-ADHD cases had no other concurrent diagnosis at age 38; the ADHD symptom picture can present alone in adults.
A third intriguing possibility is that adult-ADHD is a bona fide disorder that has unfortunately been mistaken for the neurodevelopmental disorder of ADHD because of surface similarities, and given the wrong name. This possibility would illustrate an oft-bemoaned disadvantage of a diagnostic system based on symptoms alone without recourse to etiological information: over-reliance on face validity. We found little evidence that ADHD in adults had childhood onset. Interestingly, there is strong scientific consensus that it is extremely difficult to document childhood onset in adults with ADHD(3,50,51). The frequent interpretation has been that childhood-onset ADHD was there, but patients cannot remember it. Our finding suggests the contrary hypothesis that there is an adult-onset form of ADHD. If this hypothesis is supported by research, then adult ADHD's place in the DSM (and its diagnostic criteria) may need re-consideration. Ironically, by requiring childhood onset and a neuro-developmental root, DSM-5 leaves these impaired adults out of the classification system. We found little evidence that neuropsychological dysfunction is the core etiological feature of DSM-5 adult ADHD. Other research has uncovered different etiological factors for childhood versus adult ADHD, including heritability differences(52,53). Likewise, we found that childhood-ADHD-associated polygenic risk did not characterize adult ADHD. Unfortunately the assumption that adult ADHD is the same as childhood ADHD and therefore that its causes are already researched may be discouraging etiological research into adult ADHD. If our finding of no childhood-onset neurodevelopmental abnormality for the majority of adult-ADHD cases is confirmed by others, then the etiology for adults with an ADHD syndrome will need to be found.
Supplementary Material
Acknowledgments
The Dunedin Multidisciplinary Health and Development Research Unit is supported by the New Zealand Health Research Council. This research received primary grant support from US-National Institute on Aging (AG032282) and UK Medical Research Council (MR/K00381X), and the Jacobs Foundation. We thank the members of the DSM-5 Working Group on ADHD and Disruptive Disorders, the Dunedin Study members, their families, Unit research staff, and Study founder Phil Silva. The study protocol was approved by the institutional ethical review boards of the participating universities. Participants and their parents gave informed consent before participating. TEM had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Philip Asherson received funds for consultancy or sponsored talks on behalf of Kings College London (KCL) for Shire, Lilly, Novartis, Janssen and PCM Scientific. He received research or education funds on behalf of KCL from Shire, Lilly, Novartis, Janssen, Vifor Pharma and QbTech.
Luis Augusto Rohde has been a member of the speakers' bureau/advisory board and/or acted as a consultant for Eli-Lilly, Janssen-Cilag, Novartis and Shire in the last three years. He receives authorship royalties from Oxford Press and ArtMed. He has also received travel awards from Shire for his participation at the 2014 APA meeting. The ADHD and Juvenile Bipolar Disorder Outpatient Programs chaired by him received unrestricted educational and research support from the following pharmaceutical companies in the last three years: Eli-Lilly, Janssen-Cilag, Novartis, and Shire.
Guilherme Polanczyk is supported by the National Council for Scientific and Technological Development (CNPq) [Bolsa de Produtividade em Pesquisa]. He has served as a speaker and/or consultant to Shire, developed educational material for Janssen-Cilag and Shire, and receives authorship royalties from Manole Editors.
Footnotes
Conflicts of interest: TM, RH, DB, DC, MH, HH, SH, MM, RP, SR, KS, BW, and AC have no conflicts of interest to report.
References
- 1.The European Network on Adult ADHD. European consensus statement on diagnosis and treatment of adult ADHD. BMC Psychiatry. 2010;10:69. doi: 10.1186/1471-244X-10-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cantwell D. Hyperactive children have grown up: What have we learned about what happens to them? Archives of General Psychiatry. 1985;42:1026–8. doi: 10.1001/archpsyc.1985.01790330110013. [DOI] [PubMed] [Google Scholar]
- 3.Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: Antisocial activities and drug use. Journal of Child Psychology & Psychiatry. 2004;45:195–211. doi: 10.1111/j.1469-7610.2004.00214.x. [DOI] [PubMed] [Google Scholar]
- 4.Biederman J, Petty CR, Woodworth KY, Lomedico A, Hyder LL, Faraone SV. Adult outcome of attention-deficit/hyperactivity disorder: A controlled 16-year follow-up study. Journal of Clinical Psychiatry. 2012;73:941–50. doi: 10.4088/JCP.11m07529. [DOI] [PubMed] [Google Scholar]
- 5.Klein RG, Mannuzza S, Olazagasti MAR, Roizen E, Hutchinson JA, Lashua EC, et al. Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Archives of General Psychiatry. 2012;69:1295–303. doi: 10.1001/archgenpsychiatry.2012.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Manuzza S, Klein R, Bessler A, Malloy P, LaPadula M. Adult psychiatric status of hyperactive boys grown up. American Journal of Psychiatry. 1998;155:493–8. doi: 10.1176/ajp.155.4.493. [DOI] [PubMed] [Google Scholar]
- 7.Berkson J. Limitations of the application of the fourfold table analysis to hospital data. Biometrics. 1946;2:47. [PubMed] [Google Scholar]
- 8.Cohen P, Cohen J. The clinician's illusion. Archives of General Psychiatry. 1984;41:1178–82. doi: 10.1001/archpsyc.1984.01790230064010. [DOI] [PubMed] [Google Scholar]
- 9.Gaub M, Carlson CL. Gender differences in ADHD: A meta-analysis and critical review. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1036. doi: 10.1097/00004583-199708000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Kokmen E, Ozsarfati Y, Beard CM, O'Brien PC, Rocca WA. Impact of referral bias on clinical and epidemiological studies of Alzheimer's disease. Journal of Clinical Epidemiology. 1996;49:79–83. doi: 10.1016/0895-4356(95)00031-3. [DOI] [PubMed] [Google Scholar]
- 11.Bernardi S, Faraone SV, Cortese S, Kerridge BT, Pallanti S, Wang SJ, et al. The lifetime impact of attention deficit hyperactivity disorder: Results for the National Epidomiologic Survey on Alcohol and Related Conditions (NESARC) Psychological Medicine. 2011;42:875–87. doi: 10.1017/S003329171100153X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kessler RC, Adler LA, Barkely RA, Biederman J, Conners CK, Demler O, et al. The prevalence and correlates of adult ADHD in the United States: Results from the National Comorbidity Survey Replication. American Journal of Psychiatry. 2006;163:716–23. doi: 10.1176/appi.ajp.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kooij JJS, Buitelaar J, Van den Oord EJ, Furer JW, Rijnders CAT, Hodiamont PPG. Internal and external validity of attention-deficit hyperactivity disorder in a population-based sample of adults. Psychological Medicine. 2005;35:817–27. doi: 10.1017/s003329170400337x. [DOI] [PubMed] [Google Scholar]
- 14.Matte B, Anselmi L, Salum GA, Kieling C, Gonzalves H, Menezes A, et al. ADHD in DSM-5: A field trial in a large, representative sample of 18- to 19-year old adults. Psychological Medicine. 2014:1–13. doi: 10.1017/S0033291714001470. Epub: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coughlin SS. Recall bias in epidemiologic studies. Journal of Clinical Epidemiology. 1990;43:87–91. doi: 10.1016/0895-4356(90)90060-3. [DOI] [PubMed] [Google Scholar]
- 16.Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne B, Polanczyk G, et al. How common are common mental disorders? Evidence that lifetime rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine. 2010;40:899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simon GE, Vonkorff M. Recall of psychiatric history in cross-sectional surveys - Implications for epidemiologic research. Epidemiologic Reviews. 1995;17:221–7. doi: 10.1093/oxfordjournals.epirev.a036180. [DOI] [PubMed] [Google Scholar]
- 18.Matte B, Rohde LA, Grevet EH. ADHD in adults: A concept in evolution. Attention Deficit Hyperactivity Disorders. 2012;4:53–62. doi: 10.1007/s12402-012-0077-3. [DOI] [PubMed] [Google Scholar]
- 19.Poulton R, Hancox R, Milne B, Baxter J, Scott K, Wilson N. The Dunedin Multidisciplinary Health and Development Study: are its findings consistent with the overall New Zealand population? New Zealand Medical Journal. 2006;119(1235) [PubMed] [Google Scholar]
- 20.Anderson JC, Williams S, McGee R, Silva PA. DSM-III disorders in preadolescent children. Prevalence in a large sample from the general population. Archives of General Psychiatry. 1987;44:69–76. doi: 10.1001/archpsyc.1987.01800130081010. [DOI] [PubMed] [Google Scholar]
- 21.Anderson J, Williams SM, McGee R, Silva PA. Cognitive and social correlates of DSM-III disorders in pre-adolescent children. Journal of the American Academy of Child & Adolescent Psychiatry. 1989;28:842–6. doi: 10.1097/00004583-198911000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Caspi A, Langley K, Milne B, Moffit TE, O'Donovan M, Owen MJ, et al. A replicated molecular genetic basis for subtyping antisocial behavior in ADHD. Archives of General Psychiatry. 2008;65:203–10. doi: 10.1001/archgenpsychiatry.2007.24. [DOI] [PubMed] [Google Scholar]
- 23.McGee R, Feehan M, Williams S, Anderson J. DSM-III disorders from age 11 to age 15 years. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:50. doi: 10.1097/00004583-199201000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Mill JS, Caspi A, McClay J, Sugden K, Purcell S, Asherson P, et al. The dopamine D4 receptor and the hyperactivity phenotype: A developmental-epidemiological study. Molecular Psychiatry. 2002;7:383–91. doi: 10.1038/sj.mp.4000984. [DOI] [PubMed] [Google Scholar]
- 25.Moffitt TE. Juvenile delinquency and Attention Deficit Disorder: Boys' developmental trajectories from age 3 to age 15. Child Development. 1990;61(3):893–910. doi: 10.1111/j.1467-8624.1990.tb02830.x. [DOI] [PubMed] [Google Scholar]
- 26.American Psychiatric Association. DSM-5: Options being considered for ADHD. Washington DC: American Psychiatric Association; 2010. Editor. [Google Scholar]
- 27.Barkley RA, Murphy KR, Fischer M. ADHD in adults: What the science says. New York: New York:Guilford Press; 2008. [Google Scholar]
- 28.Kessler RC, Green JG, Adler DA, Barkely RA, Chatterji S, Faraone SV, et al. Structure and diagnosis of adult attention-deficit/hyperactivity disorder: Analysis of expanded symptom criteria from the Adult ADHD Clinical Diagnostic Scale. Archives of General Psychiatry. 2010;2010:1168–78. doi: 10.1001/archgenpsychiatry.2010.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Manuzza S. DSM-V Disruptive Behavior Disorders Workgroup. American Psychiatric Association; Washington DC: 2008. Diagnosing ADHD in adults: DSM-IV controversies and DSM-V recommendations Review prepared for the American Psychiatric Association. [Google Scholar]
- 30.American Psychiatiric Association. Diagnostic and statistical manual of mental disorders. 5th. Washington DC: American Psychiatric Association; 2013. [Google Scholar]
- 31.Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: A systematic review and meta-regression analysis. American Journal of Psychiatry. 2007;164:942–8. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- 32.Polanczyk G, Willcut EG, Salum GA, Kieling C, Rhode LA. ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. International Journal of Epidemiology. 2014;43:434–42. doi: 10.1093/ije/dyt261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Willcut EG. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: A meta-analytic review. Neurotherapeutics. 2012;9:490–9. doi: 10.1007/s13311-012-0135-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fayyad J, De Graaf R, Kessler RC, Alonso J, Angermeyer M, Demyttenaere K, et al. Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. British Journal of Psychiatry. 2007;190:402–9. doi: 10.1192/bjp.bp.106.034389. [DOI] [PubMed] [Google Scholar]
- 35.Simon V, Czobor P, Balint S, Meszaros A, B I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: Meta-analysis. British Journal of Psychiatry. 2009;194:204–11. doi: 10.1192/bjp.bp.107.048827. [DOI] [PubMed] [Google Scholar]
- 36.Frazier TW, Demaree HA, Youngstrom EA. Meta-analysis of intellectual and neuropsychological test perfomances in attention-deficit/hyperactivity disorder. Neuropsychology. 2004;18:543–55. doi: 10.1037/0894-4105.18.3.543. [DOI] [PubMed] [Google Scholar]
- 37.Martinussen R, Hayden J, Hogg-Johnson S, Tannock R. A meta-analysis of working memory impairments in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2005:377–384. doi: 10.1097/01.chi.0000153228.72591.73. [DOI] [PubMed] [Google Scholar]
- 38.Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: A meta-analysis of follow-up studies. Psychological Medicine. 2006;36:159–65. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- 39.Henry B, Moffitt TE, Caspi A, Langley J, Silva PA. On the “remembrance of things past”: A longitudinal evaluation of the retrospective method. Psychological Assessment. 1994;6:92–101. [Google Scholar]
- 40.Miller CJ, Newcorn JH, Halperin JM. Fading memories: Retrospective recall inaccuracies in ADHD. Journal of Attention Disorders. 2010;14:7–14. doi: 10.1177/1087054709347189. [DOI] [PubMed] [Google Scholar]
- 41.Todd R, Huang H, Henderson C. Poor utility of the age of onset criterion of DSM-IV attention deficit/hyperactivity disorder: Recommendations for DSM-V and ICD-aa. Journal of Child Psychology & Psychiatry. 2008;49:942–9. doi: 10.1111/j.1469-7610.2008.01892.x. [DOI] [PubMed] [Google Scholar]
- 42.Barkley RA. Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychological Bulletin. 1997;121:65–94. doi: 10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- 43.Boonstra AM, Oosterlaan J, Sergeant JA, Buitellar JK. Executive functioning in adult ADHD: A meta-analytic review. Psychological Medicine. 2005;35:1097–108. doi: 10.1017/s003329170500499x. [DOI] [PubMed] [Google Scholar]
- 44.Hervey AS, Epstein JN, Curry JF. Neuropsychology of adults with attention deficit/hyperactivity disorder: A meta-analytic review. Neuropsychology. 2004;18:485–503. doi: 10.1037/0894-4105.18.3.485. [DOI] [PubMed] [Google Scholar]
- 45.Faraone SV, Biederman J, Doyle AE, Murray K, Petty CR, Adamson JJ, et al. Neuropsychological studies of late onset and subthreshold diagnoses of adult attention deficit/hyperactivity disorder. Biological Psychiatry. 2006;60:1081–7. doi: 10.1016/j.biopsych.2006.03.060. [DOI] [PubMed] [Google Scholar]
- 46.Barkley RA, Murphy KR. Impairment in occupational functioning and adult ADHD: The predictive utility of executive function (EF) ratings versus EF tests. Archives of Clinical Neuropsychology. 2010;25:157–73. doi: 10.1093/arclin/acq014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Biederman J, Petty CR, Fried R, Black S, Faneuil A, Doyle AE, et al. Discordance between psychometric testing and questionnaire-based definitions of executive function deficits in individuals with ADHD. Journal of Attention Disorders. 2008;12:92–102. doi: 10.1177/1087054707305111. [DOI] [PubMed] [Google Scholar]
- 48.Quinn CA. Detection of malingering in assessment of adult ADHD. Archives of Clinical Neuropsychology. 2003;18:4. [PubMed] [Google Scholar]
- 49.Suhr J, Hammers D, Dobbins-Buckland K, Zimak E, Hughes C. The relationship of malingering test failure to self-reported symptoms and neuropsychological findings in adults referred for ADHD evaluation. Archives of Clinical Neuropsychology. 2008;23:521–30. doi: 10.1016/j.acn.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 50.Kieling C, Kieling RR, Rohde LA, Frick PJ, Moffitt TE, Nigg JT, et al. The age at onset of attention deficit hyperactivity disorder. American Journal of Psychiatry. 2010;167:14–6. doi: 10.1176/appi.ajp.2009.09060796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McGough JJ, Barkley RA. Diagnostic controversies in adult attention deficit hyperactivity disorder. American Journal of Psychiatry. 2004;161:1948–56. doi: 10.1176/appi.ajp.161.11.1948. [DOI] [PubMed] [Google Scholar]
- 52.Franke B, Faraone SV, Sherson P, Buuitelaar J, Bau CDH, Ramos-Quiroga JA, et al. The genetics of attention deficit/hyperactivity disorder in adults, a review. Molecular Psychiatry. 2012;17:960–87. doi: 10.1038/mp.2011.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kessler RC, Adler LA, Barkely RA, Biederman J, Conners CK, Faraone SV, et al. Patterns and predictors of attention-deficit/hyperactivity disorder persistence into adulthood: Results from the National Comorbidity Survey Replication. Biological Psychiatry. 2005;57:1442–51. doi: 10.1016/j.biopsych.2005.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.