Abstract
Objective
Both executive dysfunction (ED) measured by performance-based tasks, and dysexecutive behavior (DB) measured by behavioral rating scales, contribute to late-life depression and co-morbid disability. There is a modest positive association of ED and DB, but less is known about their relative contributions to core aspects of neuropsychiatric conditions, and whether they provide unique or redundant information.
Methods
Latent variable analyses were applied to ED, DB, depression, and disability data from 220 older patients with major depression and ED who had been enrolled in a psychosocial treatment study of depression. ED measures included the Trail Making Test, part B (TMB), Stroop Color Word Interference Test (CWIT), and Hopkins Verbal Learning Test-trail one (HVLT-1). The executive dysfunction scale from the Frontal Systems Behavior Scale (FrSBe), self and other-rated, served as the ratings-based measure of DB.
Results
The measurement model, with all four latent variables related to one another demonstrated good fit (RMSEA = .06). In the structural models, DB was associated with both depression (β=.61) and disability (β=.42), while ED was associated with depression (β=.43) but not with disability (β= .16). Social problem-solving accounted for 49% of the influence of DB on late-life depression, while ED was not related to social problem-solving.
Conclusion
ED and the lesser studied DB measures offer unique and complementary information. DB was robustly associated with late-life depression and disability. Patients with depression and executive dysfunction may be more likely to develop disability when they exhibit dysexecutive behavior and social problem-solving difficulties.
Keywords: late-life depression, dysexecutive behavior, executive function, neuropsychiatry, neuropsychology
Introduction
Depressed older adults often have executive dysfunction.1,2 The clinical expression of executive dysfunction includes disorganization, mental inflexibility, disinhibition, and poor problem-solving.3 Executive dysfunction (ED) predicts poor response of late-life depression to antidepressants,4-6 and may play a key role in its pathophysiology. 7,8 Amongst heterogeneous ED measures, those of verbal fluency, and response inhibition have been predicting poor response of late-life depression to antidepressants most consistently.5
Executive function is related to both cognitive and social/emotional dimensions of functioning. 9 It has been defined as the ability to organize a sequence of actions toward a goal, 10 or as the ability to activate and inhibit response sequences guided by internal neural representations whereby the frontal lobes ‘select’ contextually appropriate behavior from a range of behavioral ‘programs’ or routines.11 Most single neuropsychological tests are largely insufficient to capture the many dimensions of ED. For this reason, it is common practice in clinical neuropsychology to administer several different tests to ‘capture’ ED in each patient.12
A three-dimensional model of performance-based measures of executive functions has received empirical support.13,14 This model incorporates shifting of mental set with updating of information in working memory, and response inhibition. 13 A subsequent functional imaging investigation identified neural correlates for each of the executive function dimensions as well as for the common underlying factor.14 Studies using hierarchical factor analysis report that a common executive function factor accounts for much more of the variance among measures than do the specific factors.15 There is evidence for the validity of executive function composite scores.16 It is less clear how the common aspects of distinct dimensions of executive function, constructed from multiple tasks, might relate to neuropsychiatric disease, relative to the more commonly used verbal fluency or response inhibition tasks.
Dysexecutive behavior (DB) measures were developed to address the concern that brief performance-based procedures might lack ecological validity, or, the capacity to predict day-to-day functioning. 17 DB measures also have the advantage of ease of administration and interpretation, and could be administered in psychiatric waiting rooms, unlike performance-based executive function measures.7 The Frontal System Behavior Scale (FrSBe)18,19 is a questionnaire that measures DB associated with frontal subcortical deficits such as apathy, executive dysfunction and disinhibition. Although the authors use the label ‘executive dysfunction’ for one subscale they mean ratings of function in daily life as opposed to performances measured in the laboratory. Meta-analysis indicates that DB and ED measures are only modestly associated with one another in child and adult attention-deficit/hyperactivity disorder and in a heterogeneous group of neurologic patients, suggesting that they are measuring fairly distinct constructs,20,21 and could make unique contributions to neuropsychiatric disease. DB measures have also been shown to be predictive of poor antidepressant drug response. 7 It has been theorized that performance-based executive functions measure algorithmic processes, concerned with the efficiency and effectiveness of information processing, while the DB rating-based measures capture the more reflective dimension of goal-setting and decision-making.20 Both ED and DB have been associated with loss of autonomy in neurologic patients,21 indicative of their relevance to late-life depression.
Study Objectives
While ED and DB measures may predict poor response of late-life depression to antidepressants, less is known about how these diverse measures operate together, or how they are associated to late-life depression and the disability, which have been linked emprically.22 The study aim is to use a latent variable approach to assess the degree of association of all these variables, and the extent of the influence of ED and DB on late-life depression and disability.
METHODS
Sample
Participants were community-dwelling older adults (minimum age of 60), with an average age of 73 (M = 72.97, SD = 7.74) recruited primarily through radio station advertisements, senior center and healthcare provider referrals, community talks, and internet advertisements on ‘Craigslist’.
A total of 653 individuals were initially screened for eligibility with 220 participants randomly assigned to receive one of two forms of psychosocial treatment.23 Sixty-five percent of the sample were female, 87% were Caucasian, 7% were African American, 4% were Asian, and less than 1% were either American Indian, Pacific Islander, or “other”. Regarding ethnicity, 7% of participants were Hispanic. The average number of years of education was 15.25, the average age of depression onset was 55.8, and the average number of depressive episodes was 2.2.
Study procedures were approved and reviewed by the institutional review boards of Weill Cornell Medical College (Cornell) and the University of California at San Francisco.
Inclusion/Exclusion Criteria
Inclusion criteria for the study were: age (minimum age of 60 with no upper limit), DSM-IV diagnosis of major depressive disorder (as determined by the Structured Clinical Interview for DSM Disorders—SCID; and by a Hamilton Depression Rating Scale –HDRS;24 of 20 or higher corresponding to severe or very severe depression, a minimum score of 24/30 on the Mini Mental Status Exam (MMSE) (to assure lack of global cognitive impairment/dementia), raw scores below 33/37 on the Initiation/Perseveration subscale of the Mattis Dementia Rating Scale (DRS-IP),25 and raw scores below 25 on the Stroop Color Word Test (SCWT).26 DRS-IP and SCWT cutoff scores are indicative of executive dysfunction in this age group, and have been consistent with unfavorable response to anti-depressant medications in the study population. 4
Individuals were excluded from the study if they had a severe medical illness (e.g. metastatic cancer), were taking medications that may cause depression (e.g. steroids), were completely incapable of performing activities of daily living based on interview response to the Multilevel Assessment Instrument,28 were receiving psychological help and/or pharmacological interventions for depression, expressed active suicidal ideation, had a diagnosis of psychotic depression (based on the SCID), had a diagnosis of any other Axis I disorder, besides major depressive disorder or generalized anxiety disorder, were substance abusers, suffered from dementia (based on MMSE score <24 or DSM diagnosis), or had a history of head trauma; factors which, if present, would potentially interfere with study treatment and findings.
Measurement Procedures
Participants underwent an extensive pre-treatment evaluation conducted by trained research assistants (RAs) that included ED, DB, depression and disability measures. Performance-based ED measures included the response inhibition condition of the Color Word Interference Stroop Test27, the Trail Making Test part B29 involving cognitive flexibility, and the Hopkins Verbal Learning Test-Trial One,30 involving learning strategy. The executive dysfunction subscale of the FrSBe,18 both self and other-rated (by the RA) served as the ratings-based measure of DB and has a Cronbach’s alpha of .92.18 Indicators of depression included The Hamilton Depression Rating Scale (21-item),24 Beck Depression Inventory (BDI)31 and the Neuroticism Extroversion Openness- Five Factor Inventory neuroticism subscale (NEO-N).32 The World Health Organization Disability Assessment Scale II (WHODAS II) seven subscale scores were used to assess functional status. The Social Problem-Solving Inventory-Revised (SPSI-R), demonstrated to correlate with self-report of depression, was included in the event that follow-up analyses of related aspects of depression were needed.33
Analysis
Latent variable analyses were conducted using AMOS 20.0.34 Chi-square goodness of fit adjusted for degrees of freedom (CMIN and CMIN/DF), comparative-fit index (CFI), and root-mean-square error of approximation (RMSEA) were used to assess model fit.35 Conclusions about model fit were derived from consideration of all measures; no single measure was considered a “gold standard.”36 To assess the significance of individual and unique associations of latent variables to late-life depression or disability the maximum likelihood estimates were used at or below statistical threshold (p < .05), and the standardized regression weights at or below statistical threshold (p< .05) were used to compare degree of association.
The study aims to use confirmatory factor analysis with structural equation modeling to better understand the inter-relationship of the latent variables of ED, DB, late-life depression and disability. The ED latent variable will consist of measures of mental switching, response inhibition and memory updating to robustly represent the factor common to ED measures.13-15 First, a measurement model was evaluated to assess the degree to which indicators loaded on their respective constructs, and, the degree to which latent variables were related to each other and represented distinct, but, perhaps related constructs. Second, a structural model evaluated the influence of the ED and DB latent variables on late-life depression and disability, interpreted by the standardized regression weights.
RESULTS
Pre-analysis
ED, DB, late-life depression and disability variables were all normally distributed (see Table 1).
Table 1.
Descriptive Statistics for the major measures
| Measure Name | N | M | SD | Min | Max | Skewness | Kurtosis |
|---|---|---|---|---|---|---|---|
| Trails B | 190 | 137.58 | 63.49 | 44 | 300 | .93 | .15 |
| HVLT-Trial 1 | 211 | 5.24 | 1.906 | 0 | 10 | -.042 | -.105 |
| Stroop Interference | 217 | 22.03 | 8.21 | 0 | 49 | -.083 | .97 |
| FRSBE-RA | 172 | 39.89 | 9.04 | 20 | 64 | .08 | -.31 |
| FRSBE-PT | 185 | 38.78 | 8.34 | 19 | 64 | -.268 | -.34 |
| NEO-neuroticism | 213 | 14.98 | 5.13 | 4 | 27 | .137 | -.59 |
| HDRS | 220 | 24.04 | 4.43 | 18 | 41 | 1.19 | 1.29 |
| BDI | 219 | 13.80 | 3.20 | 7 | 22 | .206 | -.271 |
| WHODAS-II Total | 205 | 26.55 | 7.33 | 12 | 49 | .42 | .095 |
Aim One. The Measurement Model
To understand the inter-relationship of ED, DB, latelife depression, and disability a measurement model was created in which all four latent variables were set as related to one another (see Figure One). To set the metric of latent variables, the first factor loading of each variable was set to 1. Model fit was good (χ2(df =84) = 151.72, Cmin/df = 1.8, CFI = .89, RMSEA = .06). All indicators were significantly associated to their latent variable (ps <.001; factor loadings of above .4, with the exception of WHODAS-2 with a factor loading of .33 for getting around). The estimated correlation coefficients for the latent variables displayed a range of associations from nil (disability and ED) to modest to moderate (late-life depression and disability)(see Table Two).
Figure One.
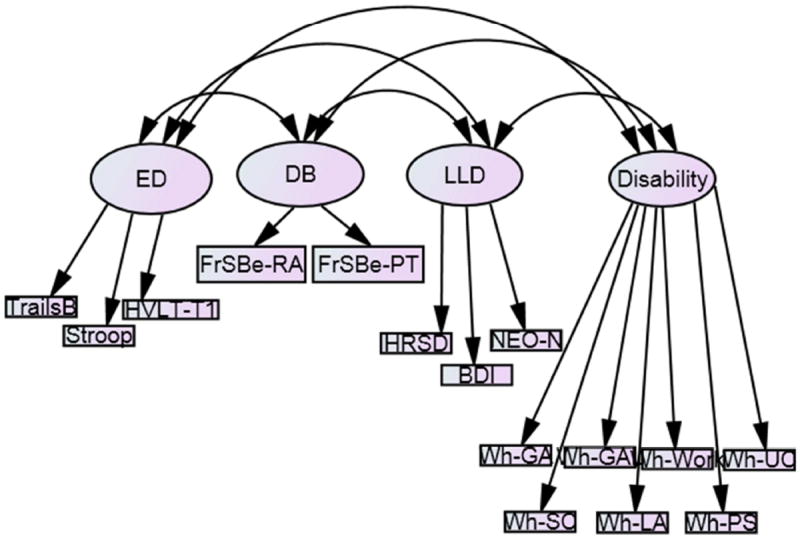
Measurement model of Executive Dysfunction, Dysexecutive Behavior, Late-Life Depression, and Disability.
ED- executive dysfunction: Trail Making Test B; Stroop Color Word Interference
Condition; Hopkings Verbal Learning Test Trial 1
DB- dysexecutive behavior: Frontal Systems Behavior Scale- research assistant and patient rating of executive dysfunction
LLD- late-life depression: Hamilton Rating Scale for Depression; Beck Depression Inventory, Neuroticism Extroversion and Openness Five Factor Inventory neuroticism subscale
Disability: WHODAS-II getting around, getting along with others, work, understanding and communicating, self-care, life activities, participating socially
Table 2.
Estimated Correlation Coefficients (r) of the Latent Variables
| Variable Name | Executive Dysfunction | Dysexecutive Behavior | Late-life depression | Disability |
|---|---|---|---|---|
| Executive Dysfunction | -- | .22* | .26* | .04* |
| Dysexecutive Behavior | -- | -- | .48** | .35** |
| Late-life depression | -- | -- | -- | .56** |
| Disability | -- | -- | -- | -- |
Correlation coefficients estimated by structural equation model, degrees of freedom=84.
p < .05.
p < .05.
Aim Two. The Structural Model: The influence of DB and ED on late-life depression and disability
Directional paths from DB and ED to late-life depression and disability were specified to evaluate the influence of each variable on late-life depression and disability while controlling for the level of the other variable.
Both DB and ED remained significantly associated with late-life depression when controlling for the other (DB: b = .13, 95%CI = .07 to .19, CR1 = 4.19, β = .61, p <.001; ED: b = -.02, 95%CI = .00 to .04, CR= -.272, β = .43, p <.01,). When both DB and ED were set to be associated with late-life depression more variance was explained in that latent variable (multiple squared correlation = .43).
With both latent variables predicting disability, only DB exhibited a significant association (DB: b = .05, 95%CI = .03 to .07, CR = 3.98, β = .42, p <.001; ED: b = .00, 95%CI = 0 to 0, CR = -.272, β=.16 ns,). When disability was set to be associated only with DB the variance explained declined slightly (.15), and variance was unexplained when set to be associated only with ED (.00).
Post-hoc evaluation of the associations between DB and ED and association to latelife depression: Social problem solving as an intervening variable
As both DB and ED demonstrated unique associations to late-life depression, the hypothesis that they were not related to late-life depression in the same way was explored. It was hypothesized that the variance in late-life depression associated with DB would be accounted for by social problem solving, while the variance in late-life depression associated with ED would not.
A social problem solving latent variable, consisting of the five SPSI-R subscales as indicators was added to the measurement model. All SPSI-R indicators were significantly associated to their latent variable (ps <.001; factor loadings ranged from .46 to .75). Overall model fit for the measurement model when adding the social problem solving latent variable was adequate (χ2(df =160)=299.67. Cmin/df = 1.87, CFI = .87. RMSEA = .06, AIC = 439.665). Next, a structural model estimating both direct paths from DB (path c’DB) and ED (path c’ED) to late-life depression and indirect paths from these variables through social problem solving (path b) was evaluated. Model fit declined slightly (χ2(df=162)= 321.58, Cmin/df = 1.98, CFI = .85, RMSEA = .07, AIC = 457.58). Regarding paths from the predictors (DB and ED, paths aDB and aED, respectively) to the intervening variable (social problem solving), DB (β= -.63, p <.001), but not ED (β = .14, ns) was meaningfully associated with social problem solving. In this model social problem solving was meaningfully associated with late-life depression (path b, β = -.44, p<.01).
While controlling for social problem solving both DB and ED continued to be meaningfully directly associated with late-life depression (bc’EF = -.02, 95%CI = -.04 to -.0004, CR = -2.48, β = -.36, p = .01; ; bc’DB = .05, 95%CI = .01 to .09, CR = 2.24, β = .29, p = .03). We estimated the indirect paths by computing the product of the coefficients for path a and path b (ab). We evaluated the statistical significance of these indirect paths using the on-line software program RMediation37 to compute the 95% confidence intervals (CIs) for the ab estimates. As estimates of the strength of the indirect paths, we computed the ratio of the total effect from each predictor to the outcome (c’ +ab) that was accounted for by the indirect effect (ab).38 The indirect path from DB to late-life depression through social problem solving was statistically significant (abDB = .05, 95%CI = .02 to .092), which accounted for 49% of the relationship between DB and late-life depression. The indirect path from ED to late-life depression through social problem solving was not statistically significant (abED = -.003, 95%CI = -.009 to .001) and accounted for 14% of the relationship between ED and late-life depression. This suggests that the association between DB and late-life depression was partly accounted for by social problem solving, while the association between ED and late-life depression was not.
DISCUSSION
The principal finding of this study is that dysexecutive behavior and executive dysfunction are distinct constructs, each associated with severity of late-life depression, but only dysexecutive behavior is associated with disability. Social problem-solving capacity accounted for nearly half of the variance in the association of dysexecutive behavior with late-life depressive symptoms. To our knowledge, this is the first report of an association of dysexecutive behavior to disability in patients with late-life depression and executive dysfunction (estimated r of .35).
The finding that DB predicts disability has intuitive appeal. The measures of DB (FrSBe) and disability (WHODAS-II) are both reports of abnormal or undesirable behavior. So it is plausible to expect that one predicts the other. Despite its ecological and predictive validity,21,39 ED was not significantly associated with disability in this study. At least two reasons may explain the lack of association. First, all subjects had executive dysfunction. The lack of subjects with intact executive function performance at a normal level may have obscured the relationship of ED measures to disability. Second, ED as assessed in this study was based on performance in paper and pencil and computer tests designed to test the function of circumscribed neural networks. Such tests may not account for betweennetwork compensatory mechanisms. Unlike ED (as measured here), DB describes complex behaviors, which are the final product of dysfunction in individual networks plus the overall compensatory coordination by the brain. Taken together, these findings suggest that patients with late-life depression and executive dysfunction may be more likely to develop disability when they exhibit dysexecutive behavior.
The latent variables of ED and DB appeared to represent distinct constructs with a modest association with each other (estimated correlation coefficient of .22).19 This observation is consistent with the conclusions of a recent meta-analysis of 20 samples of adults and children, and in a heterogeneous group of neurologic patients.20,21 Amongst neurologic patients ED and DB were both independently related to disability (loss of autonomy). 21 ED represents computational resources, including the efficiency and accuracy of mental processes. In contrast, DB is a measure of impairment in higher order functions such as motivated behavior, inhibition of inappropriate behavior, decisionmaking, goal-setting, and prioritizing. These processes support the expression of the individual’s values and approach to life.40 The association of DB to social problem-solving is consistent with this conceptualization of DB.
Both the DB and ED latent variables were distinctly associated with the latent variable of late-life depression (βs of .61 and .43, respectively, while controlling for each other). A greater part of the variance in the depression latent variable was accounted for when it was associated with both DB and ED (multiple squared correlation of .43). Severity of DB and ED deficits both predict poor response of late-life depression to antidepressants.4,6,7 These observations suggests that severity of late-life depression, ED and DB are part of a distinct clinical complex with unique prognostic significance.
Our findings should be viewed in the context of their limitations. All participants in this analysis had major depression and executive dysfunction. Therefore, our findings cannot be generalized to a broader population of depressed or non-depressed older adults. Further, the restricted range of both depression and ED measures, and that there were no participants without some degree of ED, could lead to under-estimation of strength of associations and the relative robustness of DB measures. Nevertheless, the cut-offs were such that there was variability, perhaps more than could be found in a dementia sample, lending credence to utility. In addition, the cross-sectional nature of the design precludes us from drawing causal conclusions. However, the findings of this analysis set the stage for longitudinal research to evaluate the temporal dynamics in the relationships among depression, dysexecutive behavior, executive dysfunction and disability.
In conclusion, DB and ED measures can contribute distinct and complementary information in the assessment and the treatment of the older depressed patient. DB emerged as a more predictive behavioral measure, relating to both severity of depression and disability, while ED related only to depression. These findings underscore the clinical value of assessing dysexecutive behavior, because some dysexecutive behaviors can be targeted with appropriate behavioral interventions.
Acknowledgments
Funding/Support:
This study was supported by grants R01 MH064099, R01MH063982, K2 MH074717, and P30 MH 085943 from the National Institute of Mental Health and by the Sanchez Foundation.
Footnotes
Financial Disclosure
Dr. Alexopoulos has received grant support from Forest Pharmaceuticals; has served as a consultant to the scientific advisory board of Jannsen; and, has been a member of speakers’ bureaus sponsored by Forest, Novartis, Sunovion, Astra Zeneca, Takeda, and Hoffman LaRoche.
CR = Critical Ratio, which is computed by dividing the estimate, or b, by the standard error of the estimate. With large samples, the critical ratio follows the standard normal distribution with +/- 1.96 setting the critical regions to evaluate statistical significance.41
The distribution of product terms (e.g., a*b indirect effect) often do not follow a normal distribution. Therefore, the confidence interval of estimates for indirect effects are asymmetric. The recommended manner for determining statistical significance is to compute the 95% confidence interval if adopting an alpha of .05. A confidence interval for and indirect effect that does not include zero indicates statistical significance.38
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Alexopoulos GS, Kiosses DN, Klimstra S, et al. Clinical presentation of the “depressionexecutive dysfunction syndrome” of late life. Am J of Geriatric Psychiatr. 2002;10:98–106. [PubMed] [Google Scholar]
- 2.Elderkin-Thompson V, Kumar A, Bilker WB, et al. Neuropsychological deficits among patients with late-onset minor and major depression. Archives of Clinical Neuropsychology. 2003;18:529–549. doi: 10.1016/s0887-6177(03)00022-2. [DOI] [PubMed] [Google Scholar]
- 3.Bonelli KM, Cummings JL. Fronto-subcortical circuitry and behavior. Dialogues in Clinical Neuroscience. 2007;9:141–151. doi: 10.31887/DCNS.2007.9.2/rbonelli. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alexopoulos GS, Kiosses D, Moonseong H, et al. Executive dysfunction and the course of geriatric depression. Biol Psychiatr. 2005;58:204–210. doi: 10.1016/j.biopsych.2005.04.024. [DOI] [PubMed] [Google Scholar]
- 5.Pimontel MA, Culang-Reinlieb ME, Morimoto SS, et al. Executive dysfunction and treatment response in late-life depression. Int J Geriatric Psychiatr. 2012;27:893–899. doi: 10.1002/gps.2808. [DOI] [PubMed] [Google Scholar]
- 6.Sneed JR, Roose SP, Keilp JG, et al. Response Inhibition predicts poor antidepressant treatment response in very old depressed patients. Am J Geriatric Psychiatr. 2007;15(7):553–563. doi: 10.1097/JGP.0b013e3180302513. [DOI] [PubMed] [Google Scholar]
- 7.Manning KJ, Alexopoulos GS, Banerjee S, et al. Executive Functioning Complaints and Escitalopram Treatment Response in Late-life depression. Am J Geriatric Psychiatr. doi: 10.1016/j.jagp.2013.11.005. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gunning-Dixon FM, Hoptman MJ, Lim KO, et al. Macromolecular white matter abnormalities in geriatric depression: a magnetization transfer imaging study. Am J Geriatric Psychiatr. 2008;16(4):255–262. doi: 10.1097/JGP.0b013e3181602a66. [DOI] [PubMed] [Google Scholar]
- 9.Schaefer LA, Hebben N. Domains of Neuropsychological Function and Related Neurobehavioral Disorders. In: Stucky KJ, Kirkwood MW, Donders J, editors. Neuropsychology Study Guide & Board Review. New York: Oxford University Press; 2014. [Google Scholar]
- 10.Anderson V, Jacobs R, Anderson PJ, editors. Executive functions and the frontal lobes. New York: Taylor and Francis Group; 2008. [Google Scholar]
- 11.Eslinger PJ, Chakara F. Frontal Lobe and Executive Functions. In: Rizzo M, Eslinger PJ, editors. Principles and Practice of Behavioral Neurology and Neuropsychology. Elsevier, Inc.; USA: 2004. [Google Scholar]
- 12.Gioia GA, Isquith PK, Retzlaff PD, et al. Confirmatory factor analysis of Behavior Rating Inventory of Executive Function (BRIEF) in a clinical sample. Child Neuropsych. 2002;8:249–257. doi: 10.1076/chin.8.4.249.13513. [DOI] [PubMed] [Google Scholar]
- 13.Miyake A, Friedman NP, Emerson MJ, et al. The Unity and Diversity of Executive Functions and Their Contributions to Complex “Frontal Lobe” Tasks: A Latent Variable Analysis. Cogn Psych. 2000;41:49–100. doi: 10.1006/cogp.1999.0734. [DOI] [PubMed] [Google Scholar]
- 14.Collette F, Van der Linden M, Laureys S, et al. Exploring the Unity and Diversity of the Neural Substrates of Executive Functioning. Human Bain Mapping. 2005;25:409–423. doi: 10.1002/hbm.20118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barbey AK, Colom R, Solomon J. An integrative architecture for general intelligence and executive function revealed by lesion mapping. Brain. 2012;135:1154–1164. doi: 10.1093/brain/aws021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nho K, Risacher SL, Crone PK, et al. Voxel and Surface-based topography of memory and executive deficits in mild cognitive impairment and Alzheimer’s disease. Brain Img and Behav. 2012;6:551–567. doi: 10.1007/s11682-012-9203-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gioia GA, Isquith PK, Guy SC, et al. Behavior Rating of Executive Function. Lutz, FL: Psychological Assessment Resources; 2000. [Google Scholar]
- 18.Carvalho JO, Ready RE, Malloy P, et al. Confirmatory Factor Analysis of the Frontal Systems Behavior Scale (FrSBe) Assessment. 2013;20(5):632–641. doi: 10.1177/1073191113492845. [DOI] [PubMed] [Google Scholar]
- 19.Grace J, Malloy P. Frontal Systems Behavior Scale (FrSBe): Professional Manual. Lutz, Fl.: Psychological Assessment Resources; 2001. [Google Scholar]
- 20.Toplak ME, West RF, Stanovich KE. Practitioner Review: Do performance-based measures and ratings of executive function assess the same construct? J Child Psychol Psychiatr. 2013;54(2):131–143. doi: 10.1111/jcpp.12001. [DOI] [PubMed] [Google Scholar]
- 21.Godefroy O, Azouvi P, Robert P, et al. Dysexecutive Syndrome: Diagnostic Criteria and Validation Study. Ann Neurol. 2010;68:855–864.22. doi: 10.1002/ana.22117. [DOI] [PubMed] [Google Scholar]
- 22.Alexopoulos G, Vrontou C, Kakuma T, et al. Disability in geriatric depression. Am J Psychiatr. 1996;153(7):877–885. doi: 10.1176/ajp.153.7.877. [DOI] [PubMed] [Google Scholar]
- 23.Arean PA, Raue P, Mackin S, et al. Problem Solving therapy and supportive therapy in older adults with major depression and executive dysfunction. Am J Psychiatr. 2010;167(11):1391–1398. doi: 10.1176/appi.ajp.2010.09091327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamilton MA. A rating scale for depression. J Neurol Neurosurg Psychiatr. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mattis S. Dementia Rating Scale Professional Manual. Odessa: Psychological Assessment Resources; 1988. [Google Scholar]
- 26.Perret E. The left frontal lobe of man and the suppression of habitual responses in verbal categorical behaviour. Neuropsychologia. 1974;12(3):323–330. doi: 10.1016/0028-3932(74)90047-5. [DOI] [PubMed] [Google Scholar]
- 27.Stroop JR. Studies of interference in serial verbal reactions. J Exp Psychol. 1935;18(6):643–662. [Google Scholar]
- 28.Lawton MP, Moss M, Fulcomer M, et al. A Research and Service Oriented Multilevel Assessment Instrument. J Gerontol. 1982;37(1):91–99. doi: 10.1093/geronj/37.1.91. [DOI] [PubMed] [Google Scholar]
- 29.Reitan RM. Validity of the Trail Making Test as an indicator of organic brain damage. Percept and Mot Skills. 1958;8:271–276. [Google Scholar]
- 30.Brandt J, Benedict HRB. Hopkins Verbal Learning Test-Revised professional manual. Odessa, FL: Psychological Assessment Resources, Inc; 2001. [Google Scholar]
- 31.Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatr. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 32.McCrae RR, Costa PT. NEO Inventories: Professional manual. Lutz, FL: Psychological Assessment Resources, Inc; 2010. [Google Scholar]
- 33.Dreer LE, Berry J, Rivera P, et al. Efficient Assessment of Social Problem-Solving Abilities in Medical and Rehabilitation Settings: A Rasch Analysis of the Social Problem-Solving Inventory-Revised. J Clin Psychol. 2009;65(7):653–669. doi: 10.1002/jclp.20573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arbuckle J. Amos 7.0 user’s guide. Chicago: SPSS; 2006. [Google Scholar]
- 35.Burnham KP, Anderson DR. Model selection and multi-model inference: a practical information-theoretic approach. 2. Secaucus, NJ: Springer; 2002. [Google Scholar]
- 36.Brown TA. Confirmatory Factor Analysis for Applied Research. New York: Guilford Press; 2006. [Google Scholar]
- 37.Tofighi D, MacKinnon DP. RMediation: An R package for mediation analysis confidence intervals. Behav Research Methods. 2011;43(3):692–700. doi: 10.3758/s13428-011-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.MacKinnon DP. Introduction to statistical mediation analysis. Routledge; 2008. [Google Scholar]
- 39.Leahy BJ, Lam CS. Neuropsychological testing and functional outcome for individuals with traumatic brain injury. Brain Injury. 1998;12(12):1025–1035. doi: 10.1080/026990598121936. [DOI] [PubMed] [Google Scholar]
- 40.Stanovich KE. Distinguishing the reflective, algorithmic, and autonomous minds: It is time for a tri-pocess theory? In: Evans BT, Frankish K, editors. In two minds: Dual processes and beyond. New York: Oxford University Press; 2009. pp. 55–88. [Google Scholar]
- 41.Hox JJ, Bechger TM. An introduction to structural equation modelling. Family Science Review. 1998;11:354–373. [Google Scholar]


