Abstract
Objective
No randomized controlled trials (RCTs) for adults have tested the effectiveness of a well-specified psychotherapy compared with a culturally adapted version of the same treatment. This study evaluates the effectiveness of cognitive behavioral therapy (CBT) and culturally adapted CBT (CA-CBT) in treating depressed Chinese American adults.
Methods
This was a RCT that treated 50 Chinese Americans who met criteria for major depression and sought treatment at community mental health clinics. Participants were screened beginning September 2008, with the last assessment conducted in March 2011. Participants were randomly assigned to 12 sessions of CBT or CA-CBT. Stratified randomization was used for patients who were on and not on antidepressants when they first came to the clinic, and the study did not influence regular prescription practices. The primary outcomes were dropout rates and the Hamilton Depression Rating Scale measured at baseline, session 4, session 8, and session 12.
Results
Participants in CA-CBT evidenced a greater overall decrease in depressive symptoms than those in CBT, but depression rates remained similarly high at week 12. Differences in dropout rates approached, but did not meet statistical significance (7% CA-CBT and 26% CBT).
Conclusions
Chinese Americans entered this study with very severe depression. Participants in both CBT and CA-CBT evidenced significant decreases in depressive symptoms, but the majority did not reach remission. Results suggest that these short-term treatments were not sufficient to address such severe depression and that more intensive and longer treatments may be needed. Results also indicate that cultural adaptations may confer additional treatment benefits.
Keywords: Asian American, Chinese American, culturally adapted treatment, ethnic minority, psychotherapy, culture, treatment, cognitive-behavioral therapy
Objective
Depression is a worldwide health problem that affects people from all cultural backgrounds. Empirically supported treatments such as cognitive behavioral therapy (CBT) have been shown to be effective for treating depression among African Americans and Latinos in the U.S.1–4 In addition, interpersonal psychotherapy has been found to be beneficial for perinatal depression among African American women, 5 and Africans in Uganda6. Some studies suggest that culturally adapted treatments may confer greater benefits than non-adapted treatments.7–10 Cultural adaptations refer to “the systematic modification of an evidence-based treatment or intervention protocol to consider language, culture, and context in such a way that it is compatible with the client’s cultural patterns, meanings, and values.” (p. 362).11 Among these studies, only one small study of children employed the most rigorous standard of comparing a well-defined intervention to the same intervention culturally adapted.12
Asian Americans have rarely been included in rigorous psychotherapy trials.13 Among the 3,860 participants enrolled in the clinical trials used to develop the evidence-based treatment guidelines for treating major depression, only 11 were Asian Americans.14 In addition, no randomized control trials have tested the effectiveness of a well-specified psychotherapy with Asian Americans. Dai et al. tested an 8-week cognitive-behavioral therapy program for a small sample of elderly Chinese Americans with minor depression, but did not use random assignment or psychiatric diagnoses.15 The goal of this study was to develop a culturally adapted CBT manual and to tests its effectiveness against non-adapted CBT for Chinese Americans with major depressive disorder.
Asian Americans are proportionately the fastest growing group in the US (over 17 million) and are projected to quadruple by 2050.16,17 Chinese Americans (2.7 million) are the largest Asian Americans group, and account for more than 1/5 of the world’s population. Mental illness and its treatment are highly stigmatized for Asians, resulting in lower help-seeking rates and delayed treatment,18–22 with greater psychiatric impairment at entry.21,23,24 Naturalistic outcome studies show that Asian Americans have lower treatment satisfaction, worse outcomes, and higher dropout rates than White Americans.21,25 main reason for seeking treatment.26–28 This study seeks to determine if a culturally adapted depression intervention can improve outcomes for Chinese Americans.
Methods
This RCT of adapted and standard CBT for Chinese Americans with major depression was conducted in community mental health clinics. This study was approved by the institutional review boards of Claremont McKenna College, Los Angeles Department of Mental Health, and the Community Behavioral Health Services City and County of San Francisco. Participants gave written informed consent for assessments and random assignment to treatment.
Sample Participants
Sixty-one adult Chinese American patients (between the ages of 18 and 65) who met criteria for DSM-IV major depression were randomly assigned to CBT versus Culturally Adapted CBT (CA-CBT). Patients were recruited from two mental health clinics, Richmond Area Multi-Services (RAMS) (n=47) in San Francisco and Asian Pacific Family Center (APFC) (n=14) in Los Angeles. Patients recruited from RAMS were seeking treatment from one of three subprograms, including the Adult Outpatient (AO) program (n=26), Asian Family Institute (AFI) (which contains Calworks, a federal welfare-to-work program) (n=15), or the Personal Assisted Employment Services (PAES) vocational program (n=6). Patients recruited from APFC were seeking treatment from one of two sub-programs, including the Older Adults (OA) program (n=5) and Calworks (C) (n=9).
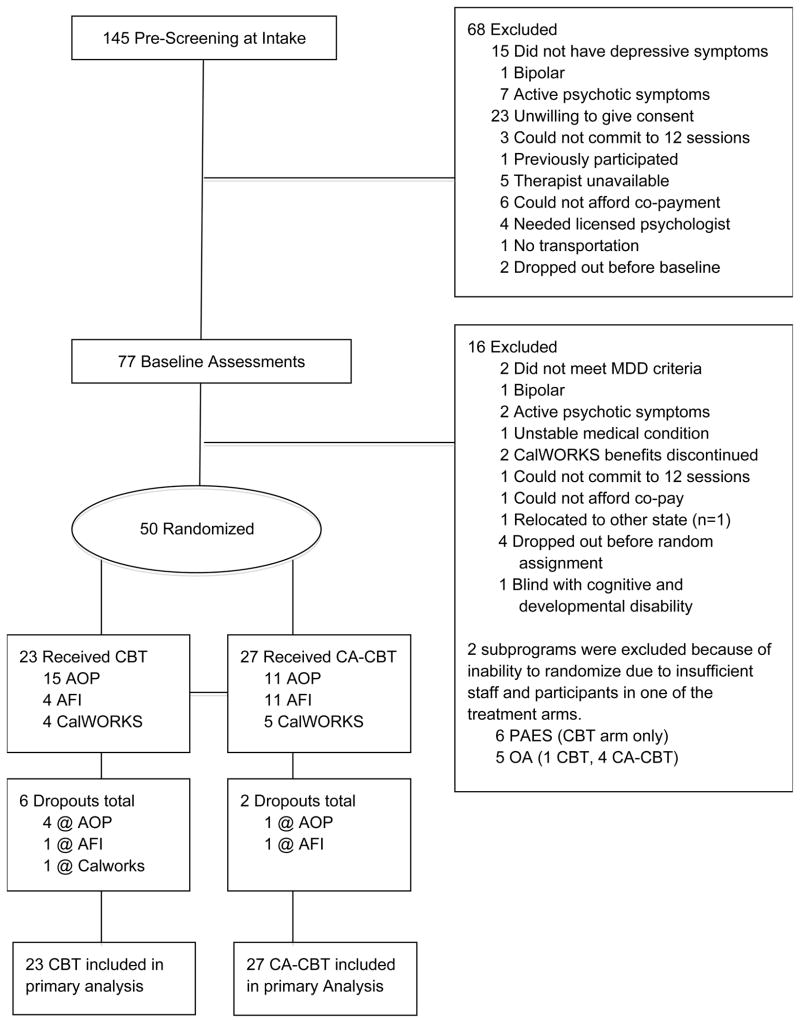
Figure 1 depicts study screening, enrollment, and exclusion criteria. Participants were screened into the study at RAMS and APFC starting September 2008 (last assessment conducted March 2011) and March 2009 (last assessment conducted January 2011), respectively. In order to be included in the study, participants had to be Chinese American, consent to treatment randomization, and meet criteria for major depression. Exclusion criteria included bipolar disorder, psychoses, unstable medical conditions, severe cognitive and developmental disabilities that prevented full participation in therapy, and a variety of real-world conditions that typically affect community-based clinical trials (e.g., unwilling to give consent and inability to afford treatment). At entry, a brief prescreening was conducted to assess for depression and obvious exclusion criteria. Participants completed an in-depth baseline screening to ensure they met study criteria.
Figure 1.
Flow of participants through each phase of the study
Randomization was implemented separately for each subprogram. Two subprograms (PAES and OA) were excluded from the primary analyses because of insufficient staffing in one of the treatment conditions, which led to inability to randomize and lack of participant variability (i.e., there were no participants in the CA-CBT arm for PAES and there was only 1 participant in the CBT arm for OA resulting in no variability). For the remaining three subprograms, 23 participants were computer randomized into CBT and 27 were randomized into CA-CBT, with stratified randomization implemented for those already taking versus not taking antidepressants at baseline screening. These 3 subprograms were collapsed (CBT=23; CA-CBT=27) in subsequent analyses because no differences were found in baseline HDRS severity. All participants agreed to come to therapy once a week. Because of real-world conditions (e.g., participant or therapist getting sick, problems scheduling, holidays, and vacations), the 12 sessions were not completed in 12 weeks, and there was no condition differences in mean number of days for completing the treatment (CBT: 102.53±20.08; CA-CBT: 100.32±2.29). Agency therapists were recruited and randomized into CBT or CA-CBT. All therapists were Chinese American and treated the patient using the patient’s language preference (i.e. Cantonese, Mandarin, or English). Psychiatrists were also blind to treatment conditions and continued with their regular prescription practices.
Interventions and Intervention Development
Participants randomized into the CBT condition were provided a widely used 12-session manualized treatment for depression,29 various versions of which have been shown to be effective in treating depression in African Americans and Latinos, as well as a variety of patients in different clinical settings.1–3,30,31 Participants randomized into the CA-CBT condition received a 12-session culturally adapted treatment32,33 that was developed using an integrative top-down and bottom-up approach called the Psychotherapy Adaptation and Modification Framework (PAMF)34 and the Formative Method for Adapting Psychotherapy (FMAP).35 The PAMF utilizes a three-tiered approach to understanding cultural adaptations (i.e., broader domains, more specific principles, and rationales for modifications). Domains include: understanding dynamic issues and cultural complexities, orienting clients to psychotherapy, understanding cultural beliefs about mental illness, improving the client-therapist relationship, understanding differences in the expression and communication of distress, and addressing culture-specific issues.
The FMAP is a community-participatory, bottom-up approach for culturally adapting psychotherapy.35,36. The FMAP approach consists of five phases: generating knowledge and collaborating with stakeholders integrating generated information with empirical and clinical knowledge, reviewing initial adaptations with stakeholders and further revision, testing the culturally adapted intervention, and finalizing the treatment. Two sets of 4-hour focus groups (14 total) were conducted with therapists at ethnic focused community mental health clinics (Asian Americans for Community Involvement, Asian Community Mental Health Services, Asian Pacific Counseling and Treatment Center, Asian Pacific Mental Health Services, and Chinatown North Beach Service Center. The first 4-hours involved discussions of how therapists culturally adapt therapy, challenges in working with Asian Americans, and reviewing a nonadapted CBT manual.29 Interviews were also conducted with Buddhist monks and nuns, spiritual and religious Taoist masters, and Traditional Chinese Medicine practitioners to understand Chinese notions of mental illness. After the PI wrote the culturally adapted manual, another set of 4-hour therapist focus groups were conducted to further improve the manual. Adaptations include providing a comprehensive therapy orientation, reducing stigma, discussing somatic aspects of depression, a greater focus on goal setting and problem solving, integrating cultural metaphors and symbols, using cultural and philosophical teachings, understanding cultural differences in communication, and addressing culturally salient issues.
The CBT and CA-CBT manuals were translated and back-translated by a translation team and the PI to ensure semantic, linguistic, and conceptual equivalence. Because written Chinese may have regional differences that is influenced by regional and linguistic variability of expression, translated materials were reviewed by lay community participants from different Chinese regions (e.g., Mainland China, Taiwan, and Hong Kong) to ensure comprehensibility of materials. Therapists in both conditions received 12-hours of training followed by weekly group supervision. As therapists treated each participant, they were asked to rate their ability to effectively present session materials, and adhere to session protocol on a Likert scale ranging from 1 (not at all) to 5 (totally). These 2 items were assessed at every session and an overall mean score for adherence across 12 sessions was calculated. There were no mean treatment condition differences regarding therapist ability to effectively adhere to the manuals (CBT: 3.59±0.61; CA-CBT: 3.57±0.68).
Diagnostic and Outcome Measures
Clinical assessors blind to treatment condition conducted an in person baseline assessment and phone assessments after sessions 4, 8, and 12. Participants were paid $150 for completing all assessments. Diagnostic screenings were conducted using a modified version of the Structured Clinical Interview for DSM-IV.37 The Chinese version of the SCID has demonstrated good psychometric properties and evidences good validity when used with Chinese and Chinese Americans.38–40 The 17-item Hamilton Depression Rating Scale was used to diagnose depression (HDRS>14) and assess depression symptoms.41,42 The HDRS has been successfully translated, validated, and used with Chinese and Chinese Americans.43–46 Inter-rater reliability in this study was high for SCID diagnoses (Kappa=100%) and HDRS scores (Intraclass correlation=.99).
Statistical analysis
We conducted linear growth models in SAS 9.2 Proc Mixed.47 The base model treated number of therapy sessions since beginning therapy as the unit of time, which included baseline, 4 sessions after baseline, 8 sessions after baseline, and 12 sessions after baseline (coded 0, 4, 8, & 12, respectively). The intercept represented depression at baseline and the time effect (i.e., session number) as the change in depression per therapy session. A treatment (CBT vs. CA-CBT) main effect and treatment by time interaction were also included representing treatment differences at baseline (the main effect) and treatment differences in the rate of change in depression (treatment X time). Missing HDRS scores were treated as missing at random and automatically accommodated in the growth model. All models treated the intercept and time as random (with the two random parameters freely covarying), and the parameters were estimated using restricted maximum likelihood. An alpha of .05 two-tailed was adopted for all analyses.
Results
Differences in drop-out rates were not statistically significant between CBT and CA-CBT, but approached significance (χ2=3.22, df=1, p=.073), with CBT evidencing 6 dropouts, (23%) and CA-CBT two (6%). Two CBT participants dropped out at session 6, and the remainder dropped out at sessions 1, 2, 4, and 5. Both CA-CBT participants dropped out at session 1. For CBT and CA-CBT, 53% and 47% evidenced no improvement, 41% and 36% evidenced partial improvement, 0% and 20% evidenced partial remission, and 12% and 16% evidenced full remission according to NIMH cut-offs, respectively However, these findings were not statistically significant. No adverse events were reported.
Depression Outcome
Table 2 shows each of the predictor effect estimates (i.e., the intercept represents HDRS level at baseline). An interaction effect between therapy sessions and CBT treatment type was observed. Specifically, the CBT group displayed a statistically significant decrease in depression (HDRS reduction of 5.53) over 12 sessions, t= 3.07, df=44, p=.004, effect size of r2=.45 (within group variance explained), and the CA-CBT group displayed approximately twice the decrease in depression (HDRS reduction of 10.62) over 12 sessions, t= 2.16, df=84, p=.033, effect size of r2=.02 (see Figure 2). The therapy session effect size was 1.54 and 2.96 for CBT and CA-CBT, respectively (difference in HDRS scores divided by within group standard deviation). However, this did not result in significantly different adjusted HDRS at the twelfth therapy session (assessed by rescaling time to −12, −8, −4, & 0 and examining the main effect of condition). The difference in the rate of change was influenced by group differences in HDRS scores at baseline (i.e., a 3.0 unit difference in adjusted HDRS scores between the two groups was statistically significant, t= 3.39, df=48, p=.001). See Table 3 for adjusted mean difference of HDRS scores across assessment time points. To verify that treatment differences in the rates of change were not being primarily driven by the baseline difference, we also tested a loglinear growth model [using time coded as ln(1), ln(5), ln(9), ln(13). The loglinear growth model also detected an interaction effect between time and treatment condition, suggesting that the difference in the rate of change held, t= 2.01, df=84, p=.047.
Table 2.
Slope Estimates, Standard Error, Degrees of Freedom (df), t-statistic, and Significance Level from the Analysis of the Hamilton Depression Scale Scores
| Predictor | Estimate | Standard Error | t | df | p |
|---|---|---|---|---|---|
| Fixed Effects | |||||
| Intercepta | 23.40 | 1.15 | 20.40 | 48 | <.001 |
| Time | −0.46 | 0.15 | −3.07 | 44 | .004 |
| Tx Condition | 3.00 | 1.56 | 1.93 | 84 | .057 |
| Time by Tx Condition | −0.42 | 0.20 | −2.16 | 84 | .033 |
The intercept represents the mean predicted Hamilton Depression score at baseline while controlling for all other predictors. The variance for the random intercept was 12.83±6.58 and the random time trend was 0.10±0.10, with the covariance between the two random effects being 1.02±0.60.
Figure 2.
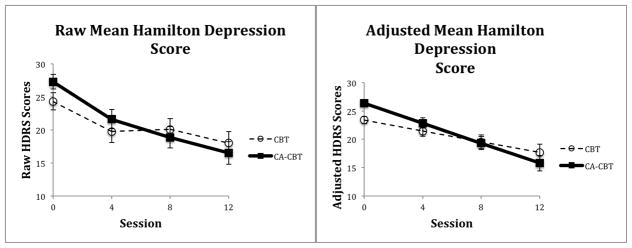
Raw and Adjusted Mean (SE) for Patients as a Function of Treatment Condition
Table 3.
Adjusted Mean Differences of HDRS for CBT Treatment Group (Covariate Antidepressant)
| CBT | CA-CBT | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Session | N | Adjusted Mean | 95% CI | N | Adjusted Mean | 95% CI | t | df | p |
| Baseline | 23 | 23.4 | 22.1–24.7 | 27 | 26.4 | 25.1–27.7 | −3.39 | 48 | .001 |
| 4 | 21 | 21 | 19.6–23.3 | 25 | 22.9 | 21.0–24.7 | −1.12 | 44 | .270 |
| 8 | 17 | 19.6 | 17.0–22.1 | 25 | 19.3 | 17.0–21.7 | 0.12 | 40 | .902 |
| 12 | 17 | 17.7 | 14.6–20.7 | 25 | 15.8 | 13.0–18.6 | 0.92 | 40 | .362 |
To examine the sensitivity of our results to missing data, we replicated the primary analysis using five data files generated using multiple imputation with MCMC estimation. This recovered a total of twenty one instances across all individuals modeled as a function of the depression values at the other time points, the condition and all possible two way interactions. The pooled results evidenced 97% efficiency for the worst parameter, indicating very good recovery. The parameters and significance tests were nearly identical with the only change being that the main effect of condition at baseline now reached statistical significance.
Conclusion
This study is unique in that it is the first RCT of a nonadapted versus culturally adapted well-defined treatment comparison for psychiatrically diagnosed adults.9,13 It is also the first RCT to be conducted with Asian Americans for a specific psychiatric outcome using evidence-based research methods recommended for clinical trials.48 This study also addresses the efficacy-effectiveness gap by directly treating patients in real-world community mental health settings.49 Chinese Americans in both the CBT and CA-CBT evidenced decreases in depressive symptoms, as well as low premature dropout. Participants in CA-CBT evidenced approximately twice the depressive symptom reduction than those in CBT, indicating that cultural adaptations may be beneficial. However, the majority in both treatment conditions remained depressed.
Participants in this study benefited from both CBT and CA-CBT. Dropout rates in this study were particularly low (i.e., 7% for the CA-CBT group and 26% for the CBT group) for a community mental health setting. A meta-analysis that examined psychotherapy dropout rates across 125 studies reported a mean rate of 47%,50 and other studies report dropout rates ranging between 30 to 60%.51–55 Minority racial status, low social economic status, and low education, all of which characterize the participants in this study, have been consistently found to be associated with premature treatment failure.50,51,53 On average, therapists in this study were less experienced (4 therapists were in graduate school and the 10 employed therapists averaged a mean post-degree clinical experience of 2.36±3.31 years), suggesting that relatively less experienced therapists can be effectively trained to provide culturally adapted treatments that engage Asian Americans.
Participants in this study were more severely depressed than many other studies, confirming that Asian Americans may delay help-seeking because of stigma.34 The adjusted mean HDRS baseline score for participants in this study was 23 and 26 for CBT and CA-CBT, respectively. By session 12, CBT and CA-CBT adjusted HDRS scores decreased to 18 and 16, respectively. In contrast, outpatients in the National Institute of Mental Health Treatment of Depression Collaborative Research Program started with a mean HDRS pretreatment score of 19.2±3.6 and after 16 weeks of treatment evidenced an adjusted mean score of 7.6±5.8.52 African American women and Latinas in the Miranda et al. study started with a baseline adjusted mean HDRS of 14.2, and after 6-months of treatment obtained an adjusted mean of 7.2.1 Both studies referenced above implemented longer treatments than this one. Although, the effect sizes for CBT and CA-CBT were quite large for a short-term treatment, results suggest that longer or more intensive treatments may be needed in order to better address the severity of depression among Chinese Americans.
Despite the strengths and unique contributions of this study, a number of limitations deserve mentioned. Results are based on a small sample size spread across two cities and multiple subprograms (2 of which were dropped due to insufficient staffing which led to inability to randomize). Although there were no differences in depression severity across subprograms, it is unclear how the results might have been different if the sample size was larger or if we were able to include additional programs. Future studies should also use more rigorous methods for assessing treatment fidelity.
Although randomly assigned, the CA-CBT participants were more severely depressed at baseline than the CBT group. Although the rate of depression change was steeper for the CA-CBT group, severity of depression was similar by session 12 and it is unclear whether this greater rate of improvement was affected by differences in initial depression severity. A larger study is needed to definitively document the impact of culturally adapting interventions for Chinese Americans. Given the severity of depression in this community mental health sample, it may be beneficial to screen and test treatments in less stigmatized settings such as primary care where depression severity may be lower.
Finally, the PI supervised therapists in CBT and CA-CBT. This was a better option than having separate supervisors, which would have led to inseparable supervisor effects. Although strictures were put in place to not systematically adapt the CBT condition (e.g., therapists were not allowed to look at the CA-CBT manual), the therapists as well the supervisor may have inherently made some modifications to CBT (e.g., they had experience working in ethnic specific clinics that are known for providing culturally sensitive or competent care). This is an ethical dilemma because by telling therapist not to make any adaptations, we are essentially telling therapists not to individualize therapy for their patients, which is essential to good therapy and violates their professional responsibility.56–58
In spite of these limitations, this is the first psychotherapy RCT conducted with an Asian American group. Results suggest that Chinese Americans may benefit from CBT and that systematic cultural adaptations may help retain Chinese Americans in treatment and improve rates of symptom reduction. Longer or more intense treatments may be needed to address the greater clinical severity that depressed Chinese American patients exhibit when they seek help. Larger and longer-term clinical trials that reaffirm the benefits and mechanisms of cultural adaptation are needed if they are to be widely implemented into care.
Supplementary Material
Table 1.
Participant demographic information
| Total (N=50) | CA-CBT (N = 27) | CBT (N = 23) | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Characteristic | N | % | N | % | N | % | Value | df | pa |
| Female | 36 | 72 | 19 | 70 | 17 | 74 | .08 | 1 | .781 |
| Age in years (M±SD) | 45.2±11.5 | 44.8±10.7 | 45.7±12.6 | .26 | 48 | .795 | |||
| Family annual income (M±SD) | 11123±17656 | 12605±21730 | 9994±12471 | .51 | 46 | .616 | |||
| Unemployed/SSDI | 24 | 48 | 14 | 52 | 10 | 44 | .35 | 1 | .555 |
| No H.S. Diploma | 22 | 44 | 11 | 41 | 11 | 48 | .25 | 1 | .615 |
| Marital status | .87 | 2 | .650 | ||||||
| Never Married | 6 | 12 | 4 | 15 | 2 | 9 | |||
| Married & live with partner | 19 | 38 | 11 | 41 | 8 | 35 | |||
| Divorced or separated or widowed | 25 | 50 | 12 | 44 | 13 | 57 | |||
| Foreign Born | 48 | 96 | 25 | 93 | 23 | 100 | b | ||
| Generational status | b | ||||||||
| 1st Generation | 48 | 96 | 25 | 93 | 23 | 100 | |||
| 2nd Generation | 1 | 2 | 1 | 4 | 0 | 0 | |||
| 3rd Generation | 1 | 2 | 1 | 4 | 0 | 0 | |||
| Years in US (M±SD) | 15.5±9.2 | 17.7±9.1 | 12.9±8.8 | 1.89 | 48 | .065 | |||
| Age of immigration (M±SD) | 29.4±10.0 | 27.3±10.3 | 32.0±9.1 | 1.69 | 48 | .097 | |||
| Language used in therapy | b | ||||||||
| Cantonese | 36 | 72 | 22 | 82 | 14 | 61 | |||
| English | 2 | 4 | 2 | 7 | 0 | 0 | |||
| Mandarin | 12 | 24 | 3 | 11 | 9 | 39 | |||
| On antidepressant at baseline | 7 | 14 | 3 | 11 | 4 | 17 | .41 | 1 | .542 |
| On antidepressant during study | 23 | 46 | 12 | 44 | 11 | 48 | .06 | 1 | .811 |
| Baseline HDRS (M±SD) | 25.9±6.1 | 27.3±5.7 | 24.3±6.3 | 1.76 | 48 | .084 | |||
| Clinic | 3.70 | 2 | .157 | ||||||
| RAMS AFI | 15 | 30 | 11 | 17 | 4 | 41 | |||
| RAMS Outpatient | 26 | 52 | 11 | 65 | 15 | 51 | |||
| APFC Calworks | 9 | 18 | 5 | 17 | 4 | 19 | |||
Based on chi-square or t-test depending on whether the variable was continuous our categorical.
All variables did not show any statistically significant difference between CA-CBT and CBT.
Language used in therapy, place of birth, and generational status could not be tested because of the minimal variability in frequencies (i.e., a value of zero in some cells).
Footnotes
Conflicts of Interest/Financial Disclosures: None reported.
Contributor Information
Wei-Chin Hwang, Email: whwang@cmc.edu, Claremont McKenna College - Psychology, 850 Columbia Ave., Claremont, California 91711.
Hector Myers, UCLA - Psychology, Los Angeles, California.
Eddie Chiu, Alliant University - Psychology, San Francisco, California.
Elsie Mak, Palo Alto University - Psychology, Palo Alto, California.
Jonathan Butner, University of Utah - Psychology, Salt Lake City, Utah.
Ken Fujimoto, University of Illinois, Chicago - Education, Chicago, Illinois.
Jeff Wood, UCLA - Education, Los Angeles, California.
Jeanne Miranda, UCLA - Psychiatry, Los Angeles, California.
References
- 1.Miranda J, Chung JY, Green BL, et al. Treating depression in predominantly low-income young minority women: A randomized controlled trial. JAMA. 2003;290(1):57–65. doi: 10.1001/jama.290.1.57. [DOI] [PubMed] [Google Scholar]
- 2.Miranda J, Duan N, Sherbourne C, et al. Improving care for minorities: can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized, controlled trial. Health Serv Res. 2003;38(2):613–630. doi: 10.1111/1475-6773.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miranda J, Azocar F, Organista KC, Dwyer E, Areane P. Treatment of depression among impoverished primary care patients from ethnic minority groups. Psychiatr Serv. 2003;54(2):219–225. doi: 10.1176/appi.ps.54.2.219. [DOI] [PubMed] [Google Scholar]
- 4.Miranda J, Shoenbaum M, Sherbourne C, Duan N, Wells KB. Effects of primary care depression treatment on minority patients’ clinnical status and employment. Arch Gen Psychiatry. 2004;61(8):827–834. doi: 10.1001/archpsyc.61.8.827. [DOI] [PubMed] [Google Scholar]
- 5.Grote NK, Swartz HA, Geibel SL, Zuckoff A, Houck PR, Frank E. A randomized controlled trial of culturally relevant, brief interpersonal psychotherapy for perinatal depression. Psychiatr Serv. 2009;60(3):313–321. doi: 10.1176/appi.ps.60.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bolton P, Bass J, Neugebauer R, et al. Group interpersonal psychotherapy for depression in the rural Uganda: A randomized controlled trail. JAMA. 2003;289(23):3117–3124. doi: 10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- 7.Griner D, Smith TB. Culturally adapted mental health interventions: A meta-analytic review. Prof Psychol Res Pr. 2006;43(4):531–548. doi: 10.1037/0033-3204.43.4.531. [DOI] [PubMed] [Google Scholar]
- 8.Smith TB, Domenech Rodríguez MM, Bernal G. Culture. J Clin Psycholol. 2011;67:166–175. doi: 10.1002/jclp.20757. [DOI] [PubMed] [Google Scholar]
- 9.Benish SG, Quintana S, Wampold BE. Culturally adapted psychotherapy and the legitimacy of myth: A direct-comparison meta-analysis. J Couns Psychol. 2011;58:279–289. doi: 10.1037/a0023626. [DOI] [PubMed] [Google Scholar]
- 10.van Loon A, van Schaik A, Dekker J, Beekman A. Bridging the gap for ethnic minority adult outpatients with depression and anxiety disorders by culturally adapted treatments. J Affect Disord. 2013;147:9–16. doi: 10.1016/j.jad.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 11.Bernal G, Jimenez-Chafey MI, Domenech Rodríguez MM. Cultural adaptation of treatments: A resource for considering culture in evidence-based practice. Prof Psychol Res Pr. 2009;40(4):361–368. [Google Scholar]
- 12.McCabe K, Yeh M. Parent– child interaction therapy for Mexican Americans: A randomized clinical trial. J Clin Child Adolesc Psychol. 2009;38:753–759. doi: 10.1080/15374410903103544. [DOI] [PubMed] [Google Scholar]
- 13.Miranda J, Bernal G, Lau A, Kohn L, Hwang W, La Flamboise T. State of the Science on Psychosocial Interventions for Ethnic Minorities. Annu Rev Clin Psychol. 2005;1(1):113–142. doi: 10.1146/annurev.clinpsy.1.102803.143822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.U. S. Department of Health and Human Services. Mental Health: Culture, Race, and Ethnicity - Supplement to Mental Health: A Report of the Surgeon General. Washington, DC: Government Printing Office; 2001. [Google Scholar]
- 15.Dai Y, Zhang S, Yamamoto J, et al. Cognitive behavioral therapy of minor depressive symptoms in elderly Chinese Americans: A pilot sstudy. Community Ment Hlt J. 1999;35(6):537–542. doi: 10.1023/a:1018763302198. [DOI] [PubMed] [Google Scholar]
- 16.Humes KR, Jones NA, Ramirez RR. Overview of race and Hispanic origin: 2010. US Department of Commerce, Economics and Statistics Administration, US Census Bureau; 2011. [Google Scholar]
- 17.Barnes JS. Current Populaton Reports C2KBR/01-16. Washington, DC: U.S. Census Bureau; 2002. The Asian Population: 2000. [Google Scholar]
- 18.Bui KV, Takeuchi DT. Ethnic minority adolescents and the use of community mental health care services. Am J Community Psychol. 1992;20(4):403–417. doi: 10.1007/BF00937752. [DOI] [PubMed] [Google Scholar]
- 19.Hu TW, Snowden LR, Jerrell JM, Nguyen TD. Ethnic populations in public mental health: Services choice and level of use. Am J Public Health. 1991;81(11):1429–1434. doi: 10.2105/ajph.81.11.1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Snowden LR, Cheung FK. Use of inpatient mental health services by members of ethnic minority groups. Am Psychol. 1990;45(3):347–355. doi: 10.1037//0003-066x.45.3.347. [DOI] [PubMed] [Google Scholar]
- 21.Sue S. Community mental health services to minority groups: Some optimism, some pessimism. Am Psychol. 1977;32(8):616–624. doi: 10.1037//0003-066x.32.8.616. [DOI] [PubMed] [Google Scholar]
- 22.Sue S, Fujino DC, Hu LT, Takeuchi DT, Zane NW. Community mental health services for ethnic minority groups: A test of the cultural responsiveness hypothesis. J Consult Clin Psychol. 1991;59(4):533–540. doi: 10.1037//0022-006x.59.4.533. [DOI] [PubMed] [Google Scholar]
- 23.Sue D, Sue S. Cultural factors in the clinical assessment of Asian Americans. J Consult Clin Psychol. 1987;55(4):479–487. doi: 10.1037/0022-006X.55.4.479. [DOI] [PubMed] [Google Scholar]
- 24.Lin TY, Lin MC. Service delivery issues in Asian-North American communities. Am J Psychiatry. 1978;135(4):454–456. doi: 10.1176/ajp.135.4.454. [DOI] [PubMed] [Google Scholar]
- 25.Zane N, Enomoto K, Chun CA. Treatment outcomes of Asian- and White-American clients in outpatient therapy. Am J Community Psychol. 1994;22(2):177–191. [Google Scholar]
- 26.Altshuler LL, Wang XD, Qi HQ, Wang WQ, et al. Who seeks mental health care in China? Diagnoses of Chinese outpatients according to DSM-III criteria and the Chinese classification system. Am J Psychiatry. 1988;145(7):872–875. doi: 10.1176/ajp.145.7.872. [DOI] [PubMed] [Google Scholar]
- 27.Flaskerud JH, Hu LT. Participation in and outcome of treatment for major depression among low income Asian-Americans. Psychiatry Res. 1994;53(3):289–300. doi: 10.1016/0165-1781(94)90056-6. [DOI] [PubMed] [Google Scholar]
- 28.Nakane Y, Ohta Y, Radford M, Yan H, et al. Comparative study of affective disorders in three Asian countries: II. Differences in prevalence rates and symptom presentation. Acta Psychiatr Scand. 1991;84(4):313–319. doi: 10.1111/j.1600-0447.1991.tb03151.x. [DOI] [PubMed] [Google Scholar]
- 29.Miranda J, Woo S, Lagomasino I, Hepner KA, Wiseman S, Munoz R. Manual for group cognitive-behavioral therapy of major depressions. San Francisco, CA: San Francisco General Hospital; 2006. Group cognitive behavioral therapy for depression - Thoughts, actions, people and your mood. [Google Scholar]
- 30.Munoz RF, Mendelson T. Toward evidence-based interventions for diverse populations: The San Francisco General Hospital prevention and treatment manuals. J Consult Clin Psychol. 2005;73(5):790–799. doi: 10.1037/0022-006X.73.5.790. [DOI] [PubMed] [Google Scholar]
- 31.Sherbourne CD, Wells KB, Duan N, et al. Long-term effectiveness of disseminating quality improvement for depression in primary care. Arch Gen Psychiatry. 2001;58(7):696–703. doi: 10.1001/archpsyc.58.7.696. [DOI] [PubMed] [Google Scholar]
- 32.Hwang W. Improving your mood: A culturally responsive and holistic approach to treating depression in Chinese Americans. 2008. (Client Manual - Chinese and English versions) [Google Scholar]
- 33.Hwang W. Improving your mood: A culturally responsive and holistic approach to treating depression in Chinese Americans. 2008. (Therapist Manual - Chinese and English versions) [Google Scholar]
- 34.Hwang W. The Psychotherapy Adaptation and Modification Framework: Application to Asian Americans. Am Psychol. 2006;61(7):702–715. doi: 10.1037/0003-066X.61.7.702. [DOI] [PubMed] [Google Scholar]
- 35.Hwang W. The Formative Method for Adapting Psychotherapy (FMAP): A community-based developmental approach to culturally adapting therapy. Prof Psychol Res Pr. 2009;40(4):369–377. doi: 10.1037/a0016240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hwang W. Integrating top-down and bottom-up approaches to culturally adapting psychotherapy: Application to Chinese Americans. In: Bernal G, Rodríguez MMD, editors. Cultural Adaptations: Tools for Evidence-Based Practice with Diverse Populations. Washington, DC: American Psychological Association; 2012. pp. 179–198. [Google Scholar]
- 37.First MB, Gibbon M. User’s guide for the Structured Clinical Interview for DSM-IV Axis I Disorders - Clinician Version( SCID-CV) Amer Psychiatric Pub Incorporated; 1997. [Google Scholar]
- 38.So E, Kam II, Leung CM, Chung DD, Liu ZZ, Fong SS. The Chinese-bilingual SCID-I/P Project: Stage 1--Reliability for mood disorders and schizophrenia. Hong Kong Journal Of Psychiatry. 2003;13(1):7–18. [Google Scholar]
- 39.Hsu GK, Wan YM, Adler DD, Rand WW, Choi EE, Tsang BP. Detection of Major Depressive Disorder in Chinese Americans in primary care. Hong Kong Journal Of Psychiatry. 2005;15(3):71–76. [Google Scholar]
- 40.Yeung A, Fung F, Yu S, et al. Validation of the Patient Health Questionnaire-9 for depression screening among Chinese Americans. Compr Psychiatry. 2008;49(2):211–217. doi: 10.1016/j.comppsych.2006.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Williams JB. A structured interview guide for the Hamilton Depression Rating Scale. Arch Gen Psychiatry. 1988;45(8):742–747. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- 43.Zheng Y, Zhao J, Phillips M, et al. Validity and reliability of the Chinese Hamilton Depression Rating Scale. Br J Psychiatry. 1988;152:660–664. doi: 10.1192/bjp.152.5.660. [DOI] [PubMed] [Google Scholar]
- 44.Leung CM, Wing YK, Kwong PK, Lo AA, Shum KK. Validation of the Chinese-Cantonese version of the Hospital Anxiety and Depression Scale and comparison with the Hamilton Rating Scale of Depression. Acta Psychiatr Scand. 1999;100(6):456–461. doi: 10.1111/j.1600-0447.1999.tb10897.x. [DOI] [PubMed] [Google Scholar]
- 45.Hwang WC, Wood JJ, Fujimoto K. Acculturative family distancing (AFD) and depression in Chinese American families. J Consult Clin Psychol. 2010;78(5):655–667. doi: 10.1037/a0020542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yeung A, Shyu I, Fisher L, Wu S, Yang H, Fava M. Culturally sensitive collaborative treatment for depressed Chinese Americans in primary care. Am J Public Health. 2010;100(12):2397–2402. doi: 10.2105/AJPH.2009.184911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hedeker D, Gibbons RD. Longitudinal data analysis. Hoboken, NJ: John Wiley & Sons, Inc; 2006. [Google Scholar]
- 48.Chambless DL, Hollon SD. Defining empirically supported therapies. J Consult Clin Psychol. 1998;66(1):7. doi: 10.1037//0022-006x.66.1.7. [DOI] [PubMed] [Google Scholar]
- 49.Weisz JR, Donenberg GR, Han SS, Kauneckis D. Child and adolescent pscyhotherapy outcomes in experiments versus clinics: Why the disparity? J Abnorm Child Psychol. 1995;23:83–106. doi: 10.1007/BF01447046. [DOI] [PubMed] [Google Scholar]
- 50.Wierzbicki M, Pekarik G. A meta-analysis of psychotherapy dropout. Prof Psychol Res Pr. 1993;24(2):190–195. [Google Scholar]
- 51.Baekeland F, Lundwall L. Dropping out of treatment: A critical review. Psychol Bull. 1975;82(5):738–783. doi: 10.1037/h0077132. [DOI] [PubMed] [Google Scholar]
- 52.Elkin I, Shea MT, Watkins JT National Institute of Mental Health Treatment of Depression Collaborative Research Program. General effectiveness of treatments. Arch Gen Psychiatry. 1989;46(11):971–982. doi: 10.1001/archpsyc.1989.01810110013002. [DOI] [PubMed] [Google Scholar]
- 53.National Institute of Mental Health. Report prepared by the Survey and Reports Branch, Division of Biometry and Epidemiology. Washington, DC: U.S. Government Printing Office; 1981. Provisional data on federally funded community mental health centers, 1978–89. [Google Scholar]
- 54.Sledge WH, Moras K, Hartley D, Levine M. Effect of time-limited psychotherapy on patient dropout rates. Am J Psychiatry. 1990;147(10):1341–1347. doi: 10.1176/ajp.147.10.1341. [DOI] [PubMed] [Google Scholar]
- 55.Persons JB, Burns DD, Perloff JM. Predictors of dropout and outcome in cognitive therapy for depression in a private practice setting. Cognit Ther Res. 1988;12(6):557–575. [Google Scholar]
- 56.Domenech Rodríguez MM, Bernal G. Bridging the gap between research and practice in a multicultural world. In: Bernal G, Domenech Rodríguez MM, editors. Cultural Adaptations: Tools for Evidence-Based Practice with Diverse Populations. Washington, DC: American Psychological Association; 2012. pp. 265–287. [Google Scholar]
- 57.American Psychological Association. [Accessed January 2010];Ethical principles of psychologists and code of conduct: 2010 Amendments. Available at http://www.apa.org/ethics/code/index.asp.aspx.
- 58.American Psychological Association Presidential Task Force on Evidence-Based Practice. Evidence-based practice in psychology. Am Psychol. 2006;61(4):271–285. doi: 10.1037/0003-066X.61.4.271. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.