Abstract
Background
Very little is known about healthcare resource utilization, including post-acute care use and hospital readmissions, following left ventricular assist device (LVAD) implantation.
Methods and Results
Administrative claims from a database of multiple U.S. health plans were used to identify patients that received an LVAD (ICD-9 code 37.66) and survived to hospital discharge from January 1, 2006 through September 30, 2013. Post-acute care use was defined as a skilled nursing facility or rehabilitation stay within 90 days after hospital discharge. Patients were censored at heart transplantation or end of coverage through December 31, 2013. Of 583 patients (mean age 55 years, 77% male), 223 (38.3%) utilized post-acute care services, which was more common in patients with diabetes, those who required hemodialysis, those who had LVADs implanted at hospitals in more populated areas, with more beds and in the Northeast region (p<0.05 for each). The most common reasons for readmission were device complications, heart failure, and arrhythmia. Readmission risk was higher in patients who had diabetes, peripheral vascular disease and longer hospital length of stay, but did not differ by post-acute care use.
Conclusions
Use of post-acute care services varies based on hospital characteristics. We found no association between post-acute care use and readmission risk after LVAD.
Keywords: left ventricular assist device, readmission, post-acute care
INTRODUCTION
Left ventricular assist devices (LVAD) are being increasingly utilized in patients with advanced heart failure (HF). While LVADs have been demonstrated to improve survival compared with medical therapy in patients with stage D HF, the care of the growing population of LVAD patients can be resource-intensive. Many patients will continue to struggle with the need for readmission after LVAD, both for factors related to their underlying heart failure and factors related to the LVAD such as device infection and gastrointestinal bleeding.
Recently, two separate analyses in elderly Medicare beneficiaries found that, while mortality after LVAD had improved over time, readmission risk either had not changed(1) or had increased(2). Few small single center studies have examined the risk of readmission after LVAD(3–5), and have reported the most common reasons for readmission include gastrointestinal bleeding(3, 4) and device infection(5). While important, single center studies fail to capture readmissions occurring outside of the implanting institution and results may be impacted by center-specific practices.
Furthermore, readmissions are just one component of the care that occurs in the early period after LVAD implantation. Patients often require admission to an acute inpatient rehabilitation or skilled nursing facility (SNF) following LVAD hospitalization to regain strength prior to returning home(6), but the use of these post-acute care services after LVAD has not been systematically examined.
Our goal was to address these gaps in knowledge, by describing use of post-acute care services, emergency department visits and readmissions after LVAD. Further, we aimed to examine the risk factors for readmission and to understand whether readmission risk differed by post-acute care use. We are uniquely positioned to address these issues using data from a large national administrative claims database.
METHODS
We conducted a retrospective analysis using the Optum Labs Data Warehouse, an administrative claims database of privately insured enrollees from throughout the United States(7, 8). This database includes claims for individuals enrolled in private health plans as well as in Medicare Advantage plans. The included plans provide claims for professional (e.g., physician), facility (e.g., hospital), and outpatient prescription medication services. Medical (professional, facility) claims include International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis codes, ICD-9 procedure codes, Current Procedural Terminology, Version 4 (CPT-4) procedure codes, Healthcare Common Procedure Coding System (HCPCS) procedure codes, site of service codes and provider specialty codes.
Study Population
We identified all patients that received an LVAD from January 1, 2006 through September 30, 2013 using the ICD-9-CM procedure code 37.66(2) at hospital discharge. To isolate LVADs placed for long-term therapy we excluded codes 37.62, 37.65 and 37.68 used for temporary non-implantable, or external or percutaneous external assist devices. As our primary focus was on readmissions and post-acute care use after hospital discharge, we excluded patients who subsequently had heart transplantation (procedure code 37.51) during the same hospitalization, died or changed insurance coverage prior to hospital discharge. We restricted the analysis to those enrollees who had at least 6 months of continuous health plan coverage prior to their LVAD implantation to capture comorbidities. If a patient had more than one LVAD implanted during the study period, we retained the first as the index procedure. Because an inpatient stay may consist of multiple claims and involve transfers between facilities, we considered inpatient claims ≤1 day apart to be part of a single continuous episode. No identifiable protected health information was accessed during the course of this study. Pursuant to the Health Insurance Portability and Accountability Act, the use of de-identified data does not require institutional review board approval or waiver.
Patient Characteristics
We examined the demographic characteristics and prevalence of key comorbid conditions for patients who underwent an LVAD implantation. Demographic variables included age, gender, and race. As assignment of race in the Optum Labs Data Warehouse is performed by a third party and has not been validated, it was not included in any of the models. Comorbid conditions were identified by ICD-9 code in any position on claims during 6 months prior to LVAD implantation. The burden of comorbidity was assessed using the Charlson comorbidity index(9).
Hospital Characteristics
Characteristics of the hospitals where LVAD implantation took place were obtained using American Hospital Association data (8% of patients were missing these data). Hospital location is identified as rural if the population is <10,000, micro (10,000–50,000), metro (50,000–2.5 million), or division (>2.5 million). Regions (Northeast, Midwest, South, and West) were divided according to U.S. Census definitions. Teaching hospitals were defined as those that belong to the Council of Teaching Hospitals of the Association of American Medical Colleges.
Outcomes
We examined all-cause readmission and emergency department visits through December 31, 2013, and post-acute care use following hospital discharge. All readmissions were counted, up to censoring. Reasons for readmissions were categorized according to the Agency for Healthcare Research Quality Clinical Classifications Software. Post-acute care use included inpatient rehabilitation and skilled nursing facility use in the 90 days following hospital discharge after LVAD implantation and was identified using billing codes. Skilled nursing facility stays were identified using UB-04 Revenue Codes (0550, 0551, 0552, 0559, 0658), CPT-4 codes (99304–99313, 99315, 99316, 99318) and HCPCS code Q5004(10). Inpatient rehabilitation was identified using UB-04 Revenue Codes (0118, 0128, 0138, 0148, 0158, 0943). Patients were censored at the date of end of coverage, in-hospital death, orthotopic heart transplantation, or December 31, 2013, whichever came first.
Statistical Analysis
Baseline characteristics were summarized using N(%), median (25th, 75th percentile) or mean (standard deviation) as appropriate. We compared differences in baseline characteristics by post-acute care use using χ2 for categorical variables and t-tests for continuous variables. Multiple failure Cox regression models were used to identify patient and hospital factors associated with readmission. Length of stay was categorized by weeks based on distribution. When evaluating the association between post-acute care use and readmissions, post-acute care use was defined as whether it was used within the first 3 days post-hospital discharge after initial implant. Analyses were performed using SAS Version 9.3 and Stata 13.1. A p value of ≤0.05 was used to determine statistical significance.
RESULTS
In total, 695 patients received an LVAD, of whom 583 (83.9%) survived to hospital discharge without undergoing heart transplantation (n=16), ending insurance coverage (n=2), or dying (n=94) and were eligible for inclusion in analysis. LVADs were implanted at a total of 100 hospitals. The number of LVADs per center captured in this analysis ranged from 1–30 (25th-75th percentile 1–7). The mean age of the study population was 54.9 years, and 133 (22.8%) were women (Table 1). The median index hospital length of stay was 31 days (25th-75th percentile 21–48 days). After a mean follow-up of 1.0 (standard deviation 1.0) years, 170 (29.7%) patients had undergone heart transplantation. During that time, a total of 1,186 readmissions and 929 emergency department visits occurred.
Table 1.
Patient Baseline Characteristics
| Characteristic | Overall(N=583) | Used Post-Acute Care (N=223) |
No Post-Acute Care (N=360) |
P value |
|---|---|---|---|---|
| Age, years, mean (standard deviation) | 54.9 (12.1) | 56.1 (12.5) | 54.2 (11.8) | 0.052 |
| Female | 133 (22.8) | 59 (44.4) | 74 (55.6) | 0.10 |
| Race/ethnicity | --- | |||
| White | 300 (51.5) | 114 (38.0) | 186 (62.0) | |
| Black | 86 (14.8) | 38 (44.2) | 48 (55.8) | |
| Other | 36 (6.2) | 15 (41.7) | 21 (58.3) | |
| Unknown/missing | 161 (27.6) | 56 (34.8) | 105 (65.2) | |
| LVAD hospitalization length of stay (median, IQR) | 31 (21, 48) | 32 (20, 50) | 31 (21, 47) | 0.61 |
| Charlson comorbidity index (median, IQR) | 4 (2, 5) | 4 (2, 6) | 4 (2, 5) | 0.55 |
| Comorbidities | ||||
| Diabetes | 216 (37.0) | 95 (44.0) | 121 (56.0) | 0.03 |
| Stroke | 45 (7.7) | 18 (40.0) | 27 (60.0) | 0.80 |
| Cerebrovascular Disease | 159 (27.3) | 59 (37.1) | 100 (62.9) | 0.73 |
| Moderate/Severe Renal Disease | 198 (34.0) | 74 (37.4) | 124 (62.6) | 0.75 |
| Chronic Pulmonary Disease | 298 (51.1) | 113 (37.9) | 185 (62.1) | 0.87 |
| Use of Hemodialysis pre-LVAD | 15 (2.6) | 11 (73.3) | 4 (26.7) | 0.005 |
| Depression | 51 (8.7) | 21 (41.2) | 30 (58.8) | 0.65 |
| Peripheral Vascular Disease | 124 (21.3) | 54 (43.5) | 70 (56.5) | 0.17 |
| Hospital bed size* | 0.002 | |||
| 1–49 | 186 (34.8) | 58 (31.2) | 128 (68.8) | |
| 50–199 | 216 (40.4) | 90 (41.7) | 126 (58.3) | |
| 200–399 | 96 (17.9) | 33 (34.4) | 63 (65.6) | |
| 400+ | 37 (6.9) | 23 (62.2) | 14 (37.8) | |
| Hospital location* | 0.003 | |||
| Rural | 129 (24.1) | 32 (24.8) | 97 (75.2) | |
| Micro | 46 (8.6) | 17 (37.0) | 29 (63.0) | |
| Metro | 265 (49.5) | 112 (42.3) | 153 (57.7) | |
| Division | 95 (17.8) | 43 (45.3) | 52 (54.7) | |
| Hospital region* | 0.011 | |||
| Northeast | 54 (10.1) | 27 (50.0) | 27 (50.0) | |
| Midwest | 189 (35.3) | 80 (42.3) | 109 (57.7) | |
| South | 211 (39.4) | 77 (36.5) | 134 (63.5) | |
| West | 81 (15.1) | 20 (24.7) | 61 (75.3) | |
| Hospital ownership* | 0.15 | |||
| Public | 131 (24.5) | 59 (45.0) | 72 (55.0) | |
| Private Nonprofit | 288 (53.8) | 101 (35.1) | 187 (64.9) | |
| For Profit | 116 (21.7) | 44 (37.9) | 72 (62.1) |
All values shown are N(%) unless otherwise noted. Row percentages are shown.
In total, 47 (8.2%) of patients were missing AHA hospital characteristics.
Post-Acute Care Use
Within 90 days of hospital discharge, 223 (38.3%) patients utilized post-acute care services following LVAD implantation, including 179 (30.7%) who were cared for in a SNF, 24 (4.1%) who participated in rehabilitation in a non-skilled nursing setting, and 20 (3.4%) who used both. Of the 223 patients who utilized post-acute care within 90 days post-LVAD hospital discharge, 61 had a readmission before utilization, and 162 did not. Post-acute care use was more common in patients who had LVADs implanted at hospitals in more populated areas, in the Northeast region and in hospitals with a greater number of beds (Table 1). Post-acute care use was also more common in patients who were diabetic and required hemodialysis prior to LVAD. There was a trend toward higher post-acute care use in older patients (p=0.052). The proportion of patients utilizing post-acute care was 50% in the Northeast, 42% in the Midwest, 37% in the South, and 25% in the West.
Emergency Department Visits
The number of emergency department visits varied from 0 to 28 per person (median 1, 25th-75th percentile 0–2). In total, 50% (461 of 929) of emergency department visits led to hospital admissions. Of the remaining 467 emergency department visits that did not result in hospital admission, the most common reasons for visits were epistaxis (82 visits in 38 patients), chest pain (29 visits in 22 patients), and device complication (23 visits in 21 patients, Table 2).
Table 2.
Top 10 Reasons for Readmission and Emergency Room Visits
| Primary Diagnosis | Readmissions (N) | Patients (N, %) |
|---|---|---|
| Device Complication | 266 | 156 (26.8) |
| Heart Failure | 136 | 89 (15.3) |
| Arrhythmia | 71 | 52 (8.9) |
| Gastrointestinal bleeding | 65 | 44 (7.5) |
| Complication of procedure | 44 | 32 (5.5) |
| Anemia | 34 | 28 (4.8) |
| Septicemia | 31 | 25 (4.3) |
| Other gastrointestinal diagnosis | 30 | 27 (4.6) |
| Acute cerebrovascular disease | 29 | 26 (4.5) |
| Other upper respiratory | 27 | 21 (3.6) |
| Primary Diagnosis |
Emergency Room Visits (N) |
Patients (N, %) |
| Epistaxis | 82 | 38 (6.5) |
| Chest pain | 29 | 22 (3.8) |
| Device complication | 23 | 21 (3.6) |
| Arrhythmia | 20 | 19 (3.3) |
| Other lower respiratory | 17 | 15 (2.6) |
| Heart Failure | 16 | 14 (2.4) |
| Other aftercare | 13 | 9 (1.5) |
| Superficial injury | 11 | 11 (1.9) |
| Abdominal pain | 10 | 9 (1.5) |
| Dizziness | 10 | 10 (1.7) |
Readmissions
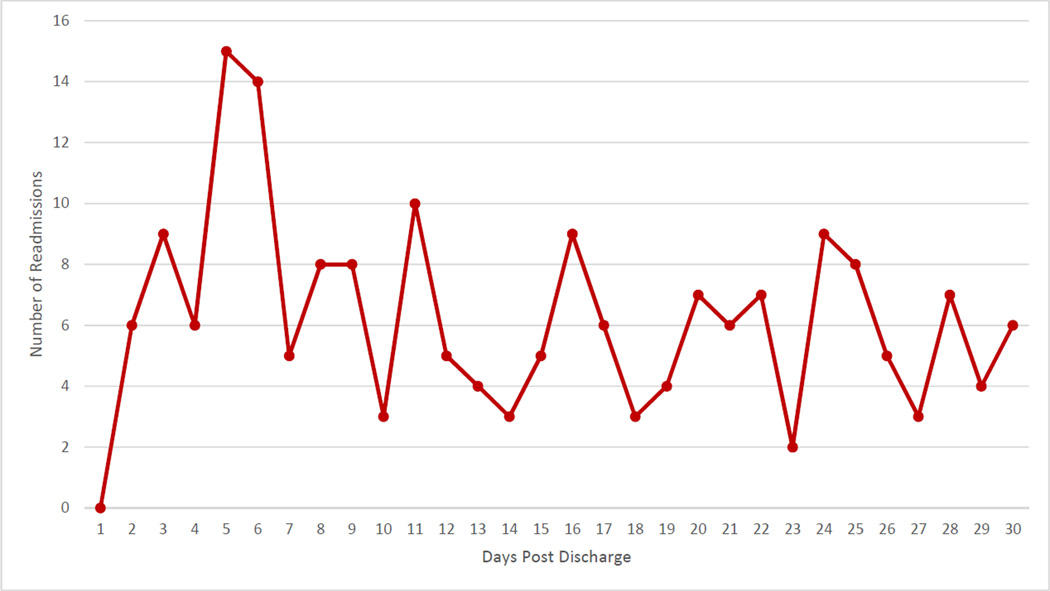
The number of readmissions per patient varied widely (0 to 18 per person), with 199 (34.0%) patients experiencing no readmissions, while 74 (12.7%) had 5 or more readmissions during follow-up. Of the patients with no readmissions, most (78.9%) had a heart transplant within 90 days and 26% had an emergency department visit but were not hospitalized. On average, the rate of readmissions was 2.0 per person year of follow-up, but was higher early after LVAD implantation (Figure 1A). The most common reasons for readmission were device complications (266 readmissions in 156 patients), heart failure (136 readmissions in 89 patients), and arrhythmia (71 readmissions in 52 patients, Table 2). Readmissions for device complication included those for LVAD-related infection (n=136 of 266, 51.1%, ICD-996.61) and mechanical complication of cardiac device (ICD-9 996.72 and 996.09, N=128, 48.1%), which often includes patients with suspected or confirmed LVAD thrombus and other mechanical issues such as driveline fracture. GI bleeding was a more frequent reason for readmission among older patients (12% of readmissions in patients ≥65 years old vs. 4% in patients <65). There were no other age-related differences in reasons for readmission observed. Multiple readmissions per patient for a single reason were common. In total, 86.1% (934 of 1085 with known hospital location) of readmissions were at the same facility as the initial LVAD implantation. The 30-day readmission rate was 27.6% (161 of 583 patients, Figure 1B). The total number of readmissions occurring within 30 days was 187, as some patients were readmitted multiple times. In total, 55 (29.4%) readmissions were in the first week after hospital discharge. The most common reasons for 30-day readmissions were device complications (32 admissions in 31 patients), heart failure (20 admissions in 20 patients) and arrhythmia (15 admissions in 12 patients). When patients were categorized by whether they used post-acute care services within the first 3 days after hospitalization, we saw no difference in the rates of 30 day readmissions between groups (28% in those who used post-acute care compared with 23% in those who did not, p=0.30). There was no difference in the association between age and post-acute care use in predicting 30-day readmission (interaction age*post-acute care use p=0.80).
Figure. Readmissions in First Year Post-LVAD.
The rate of readmissions per 100 person*months for the first year post-LVAD are shown in Panel A. In panel B, the number of readmissions per day in the first 30 days post-LVAD hospital discharge are shown.
The bivariate and multivariate predictors of readmission are shown in Table 3. Longer index length of stay and peripheral vascular disease were each associated with an increased risk of readmission. There was a trend toward lower readmission risk in older patients and higher readmission risk in patients with diabetes. We found no association between hospital characteristics and readmission risk. In a sensitivity analysis, addition of the hospital characteristics to the multivariate model did not appreciably change the results observed. In the multivariate model, diabetes, peripheral vascular disease, and longer length of stay were associated with higher risk of readmission. When evaluating the association between length of stay and readmission, patients who had hospital stays of >6 weeks at the time of LVAD implantation were at particular high risk for readmission. A non-significant trend toward lower readmission risk in older patients persisted. We found no association between use of post-acute care services within 3 days of index hospital discharge and readmission risk.
Table 3.
Predictors of All-Cause Readmission
| Bivariate Models | Multivariate Model | |||
|---|---|---|---|---|
| Characteristic | Hazard Ratio (95% CI) | P-value | Hazard Ratio | Wald P-value |
| Age | 0.091 | 0.069 | ||
| <=45 | 1 (referent) | 1 (referent) | ||
| 46–55 | 0.806 (0.513, 1.266) | 0.703 (0.473, 1.045) | ||
| 56–65 | 1.321 (0.855, 2.040) | 1.071 (0.730, 1.571) | ||
| 66–75 | 0.919 (0.538, 1.569) | 0.703 (0.416, 1.188) | ||
| 75+ | 0.552 (0.188, 1.623) | 0.45 (0.160, 1.261) | ||
| Female | 0.876 (0.603, 1.273) | 0.487 | 1.019 (0.726, 1.431) | 0.911 |
| Length of Stay | 0.003 | 0.009 | ||
| <15 days | 1 (referent) | 1 (referent) | ||
| 15–21 days | 1.847 (0.941, 3.626) | 1.705 (0.862, 3.372) | ||
| 22–42 days | 1.497 (0.852, 2.632) | 1.662 (0.938, 2.942) | ||
| 43–56 days | 2.766 (1.479, 5.173) | 2.851 (1.517, 5.358) | ||
| 57+ days | 2.455 (1.325, 4.549) | 2.267 (1.215, 4.230) | ||
| Charlson comorbidity index | 0.203 | --- | ||
| 0 | 1 (referent) | |||
| 1–2 | 2.137 (0.764, 5.979) | |||
| 3–5 | 2.046 (0.752, 5.569) | |||
| 6+ | 2.68 (0.963, 7.464) | |||
| Moderate/Severe Renal Disease | 1.091 (0.790, 1.507) | 0.596 | 0.956 (0.703, 1.299) | 0.773 |
| Chronic Obstructive Pulmonary Disease | 0.944 (0.691, 1.290) | 0.716 | 0.894 (0.675, 1.184) | 0.433 |
| Peripheral Vascular Disease | 1.853 (1.302, 2.639) | 0.001 | 2.035 (1.473, 2.811) | <0.001 |
| Cerebrovascular Disease | 1.005 (0.703, 1.437) | 0.978 | 0.97 (0.692, 1.359) | 0.860 |
| Diabetes | 1.323 (0.959, 1.826) | 0.088 | 1.321 (1.000, 1.746) | 0.050 |
| Depression | 1.083 (0.705, 1.662) | 0.716 | 0.97 (0.615, 1.530) | 0.896 |
| Post-Acute Care Use within 3 days | 0.834 (0.528, 1.317) | 0.436 | 0.79 (0.531, 1.176) | 0.246 |
| Hospital Control | 0.887 | --- | ||
| Public | 1 (referent) | |||
| Public Non-Profit | 1.149 (0.745, 1.772) | |||
| For Profit | 1.016 (0.611, 1.691) | |||
| Unknown | 1.132 (0.544, 2.356) | |||
| Hospital Region | 0.438 | --- | ||
| Northeast | 1 (referent) | |||
| Midwest | 1.323 (0.723, 2.422) | |||
| South | 1.682 (0.932, 3.037) | |||
| West | 1.52 (0.778, 2.968) | |||
| Unknown | 1.505 (0.660, 3.428) | |||
| Hospital Teaching Status | 0.605 | --- | ||
| No | 1 (referent) | |||
| Residency | 0.994 (0.683, 1.447) | |||
| COTH | 0.639 (0.333, 1.225) | |||
| Unknown | 0.999 (0.519, 1.921) | |||
| Hospital Beds | 0.766 | ---- | ||
| 1–49 | 1 (referent) | |||
| 50–199 | 0.789 (0.546, 1.139) | |||
| 200–399 | 0.858 (0.554, 1.330) | |||
| 400+ | 0.759 (0.371, 1.552) | |||
| Unknown | 0.911 (0.464, 1.786) | |||
| Hospital location type | 0.998 | --- | ||
| Division (>2.5 million) | 1 (referent) | |||
| Metro (50,000 to 2.5 million) | 0.96 (0.595, 1.549) | |||
| Micro (10,000–50,000) | 1.027 (0.473, 2.230) | |||
| Rural (<10,000) | 1.019 (0.578, 1.794) | |||
| Unknown | 1.037 (0.480, 2.240) | |||
Individual comorbidites rather than Charlson were included in the multivariate model.
DISCUSSION
There are several important findings from this study. First, more than one-third of patients utilized post-acute care services following LVAD, and hospital characteristics were associated with differential use. Second, readmissions are common post-LVAD, frequently recurrent, and the majority of readmissions occur at the implanting hospital rather than a new hospital. Patients at highest risk for subsequent hospitalizations include those who are diabetic, have peripheral vascular disease and experience longer hospital stays at the time of the LVAD implantation.
Post-acute care use is common after an acute hospitalization, and represents a substantial burden to the healthcare system(11). Medicare and private insurers pay for post-acute care, including short-term skilled nursing and therapy for patients recovering from an acute illness or surgery. After LVAD implantation, patients often have decreased strength from prolonged immobility or other skilled needs, such that post-acute care is often used, but until now, has not been quantified. We found that over one-third of individuals utilized either skilled nursing or inpatient rehabilitation services in the 90 days after LVAD hospital discharge. Most care was performed in a skilled setting, whereas inpatient rehabilitation services in a non-skilled setting were used less often. The largest driver of differences in utilization of post-acute care services were hospital characteristics, as use was more common in patients who had LVADs implanted in larger hospitals in more populated areas and in the Northeast, possibly reflecting differences in availability of these services. Inpatient rehabilitation, in particular, is available on-site at some large academic centers(6, 12), and in those circumstances can be utilized in as many as half of patients after LVAD. Patients participating in inpatient rehabilitation programs after LVAD have been demonstrated to have substantial improvements in their functional ability by discharge(6, 12), though the benefits of rehabilitation in this setting have not been assessed in a controlled or randomized fashion.
Overall, we found no association between use of post-acute care services and readmission risk. Differences in patient characteristics and hospital patterns of post-acute care use limit our ability to draw conclusions about causality in this setting. However, this information may be of utility for programs that are considering routine use of post-acute care as a way to decrease early readmission rates, which were quite high regardless of use of post-acute care services.
Readmissions remain a common problem after LVAD. Heart failure has the highest 30-day readmission rate at 24.8% for any discharge diagnosis among elderly Medicare beneficiaries(13). By comparison, we found that the 30-day readmission rate after initial LVAD implantation was 28%, which was similar to that reported in Medicare LVAD recipients(2), underscoring that the burden of early readmissions is very high in this population. Similar to others(4), we saw that the readmission rate is highest early post-LVAD, declines over the first 6 months, and then appears to stabilize.
The top reasons for readmission observed herein were device complications such as infection and thrombosis, heart failure, and arrhythmias. A similar pattern was reported among Medicare beneficiaries(2), though single-center studies have often reported a heavier burden of gastrointestinal bleeding(3, 4). These differences could be related to variations in the way that the reasons for readmissions were categorized, based on manual record review in single-center studies compared with billing codes. Overall, we found that 14% of readmissions over time were to hospitals other than the implanting hospital. Therefore, studies that rely solely upon counting readmissions to their own hospital may modestly underestimate the total burden of readmissions after LVAD.
While readmissions after LVAD are common, some patient populations are at particularly high risk, including those who are diabetic, have peripheral vascular disease, and have longer hospital length of stay at the time of LVAD implantation. Finding that readmission risk was higher in patients with very prolonged index hospital length of stay was not surprising, as this association has been reported in other populations of patients after myocardial infarction(14) and coronary artery bypass grafting(15), and likely reflects a complicated hospital course with the potential for ongoing issues at the time of hospital discharge. Similarly, patients with diabetes are known to have higher readmission risk after hospitalization for cardiovascular reasons(14, 15). Finally, we saw a higher risk for readmission in patients with peripheral vascular disease, which has also been reported as a risk factor for 30-day readmission after coronary artery bypass grafting(15). It is important to note that while our population was large compared to single center studies in LVAD recipients on the same topic(3–5), the number of patients and total readmissions are still relatively modest, which limits our ability to detect small differences in risk of readmission by patient or hospital factors that may exist.
Strengths and Limitations
There are several important factors to consider in interpreting these findings. First, this is a retrospective observational study, so no causal inferences can be made. Second, these data are from an insured population, and include only a subset of insured patients in the US; the findings from other patient populations may differ. We were able to capture utilization occurring while patients remained enrolled in the health plan, but could not capture utilization after end of coverage. To accurately capture comorbidity burden and baseline risk we required patients to have 6 months continuous coverage prior to LVAD to be included in the analysis, and these patients may differ than those who recently acquired coverage. Furthermore, when health plan coverage ended, we do not know whether it was because the patient died or changed insurance coverage. As such, we are unable to capture the impact that the competing risk of death, particularly outpatient death that does not result in a readmission, has on factors associated with readmission risk in this study. We also do not have details about the model of device that was implanted or whether it was implanted as a bridge to transplant or destination therapy. This study also has the limitations of any study based on claims data: while commonly used and validated in health services research, reliance upon billing codes for identification of comorbidities and reasons for readmissions may result in misclassification. However, there are several notable strengths. We were able to comprehensively capture all post-acute care use, emergency department visits, and hospitalizations in a large population of patients with LVADs. Our study included patients from geographically diverse areas across the United States. Our findings are complementary to those reported among elderly Medicare beneficiaries(1, 2), and would be applicable to privately insured individuals undergoing LVAD implantation. Based on previous publications using INTERMACS and Medicare data(1, 16), we would estimate that 51.7% of the 4850 patients receiving LVADs from 2006–11 were Medicare fee-for-service beneficiaries. In a similar time frame, 1,044 patients in the Optum Labs Data Warehouse received LVADs, such that approximately 44.6% of non-Medicare fee-for-service beneficiaries receiving LVADs can be captured using this data source.
Conclusions
There is variability in use of post-acute care services after LVAD. Patients who have LVADs implanted in larger hospitals in more populated areas are more likely to utilize post-acute care services, though we found no association between its use and subsequent readmissions. Readmissions after LVAD implantation are high, particularly in the early period post-implantation. While mortality has improved after LVAD implantation in recent years, readmissions and their associated morbidity remain common and are an area in need of further progress and improvement.
HIGHLIGHTS.
More than one-third of patients utilize post-acute care services after LVAD surgery
Patients cared for in larger hospitals, in more populated areas, and in the Northeastern United States are more likely to use post-acute care after LVAD
Patients with diabetes, peripheral vascular disease, and those with longer hospital length of stay for LVAD surgery are at highest risk for readmission, but post-acute care use is not associated with differential readmission risk
Acknowledgments
FUNDING SOURCES: Dr. Dunlay is supported by a NIH Career Development Award (K23 HL116643).
ABBREVIATIONS
- CPT-4
Current Procedural Terminology, Version 4
- HCPCS
Healthcare Common Procedure Coding System
- HF
heart failure
- ICD-9-CM
International Classification of Diseases, 9th revision
- LVAD
left ventricular assist device
- SNF
skilled nursing facility
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
DISCLOSURES: None
REFERENCES
- 1.Khazanie P, Hammill BG, Patel CB, Eapen ZJ, Peterson ED, Rogers JG, et al. Trends in the use and outcomes of ventricular assist devices among medicare beneficiaries, 2006 through 2011. J Am Coll Cardiol. 2014;63:1395–1404. doi: 10.1016/j.jacc.2013.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lampropulos JF, Kim N, Wang Y, Desai MM, Barreto-Filho JA, Dodson JA, et al. Trends in left ventricular assist device use and outcomes among Medicare beneficiaries, 2004–2011. Open Heart. 2014;1:e000109. doi: 10.1136/openhrt-2014-000109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Forest SJ, Bello R, Friedmann P, Casazza D, Nucci C, Shin JJ, et al. Readmissions after ventricular assist device: etiologies, patterns, and days out of hospital. Ann Thorac Surg. 2013;95:1276–1281. doi: 10.1016/j.athoracsur.2012.12.039. [DOI] [PubMed] [Google Scholar]
- 4.Hasin T, Marmor Y, Kremers W, Topilsky Y, Severson CJ, Schirger JA, et al. Readmissions after implantation of axial flow left ventricular assist device. J Am Coll Cardiol. 2013;61:153–163. doi: 10.1016/j.jacc.2012.09.041. [DOI] [PubMed] [Google Scholar]
- 5.Smedira NG, Hoercher KJ, Lima B, Mountis MM, Starling RC, Thuita L, et al. Unplanned hospital readmissions after HeartMate II implantation: frequency, risk factors, and impact on resource use and survival. JACC Heart Fail. 2013;1:31–39. doi: 10.1016/j.jchf.2012.11.001. [DOI] [PubMed] [Google Scholar]
- 6.English ML, Speed J. Effectiveness of acute inpatient rehabilitation after left ventricular assist device placement. Am J Phys Med Rehabil. 2013;92:621–626. doi: 10.1097/PHM.0b013e31827442a4. [DOI] [PubMed] [Google Scholar]
- 7.Lipska KJ, Ross JS, Van Houten HK, Beran D, Yudkin JS, Shah ND. Use and out-of-pocket costs of insulin for type 2 diabetes mellitus from 2000 through 2010. JAMA. 2014;311:2331–2333. doi: 10.1001/jama.2014.6316. Research Support, U.S. Gov't, PHS.]. 2014 Jun 11;311(22):2331-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wallace PJ, Shah ND, Dennen T, Bleicher PA, Crown WH. Optum Labs: building a novel node in the learning health care system. Health Aff (Millwood) 2014;33:1187–1194. doi: 10.1377/hlthaff.2014.0038. [DOI] [PubMed] [Google Scholar]
- 9.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 10.Koroukian SM, Xu F, Murray P. Ability of Medicare claims data to identify nursing home patients: a validation study. Med Care. 2008;46:1184–1187. doi: 10.1097/MLR.0b013e31817925d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mechanic R. Post-acute care--the next frontier for controlling Medicare spending. N Engl J Med. 2014;370:692–694. doi: 10.1056/NEJMp1315607. [DOI] [PubMed] [Google Scholar]
- 12.Alsara O, Reeves RK, Pyfferoen MD, Trenary TL, Englan DJ, Vitse ML, et al. Inpatient rehabilitation improves outcomes for patients receiving left ventricular assist device. Inpatient Rehab and Functional Improvement. 2014;93:860–868. doi: 10.1097/PHM.0000000000000101. [DOI] [PubMed] [Google Scholar]
- 13.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 14.Dunlay SM, Weston SA, Killian JM, Bell MR, Jaffe AS, Roger VL. Thirty-day rehospitalizations after acute myocardial infarction: a cohort study. Ann Intern Med. 2012;157:11–18. doi: 10.7326/0003-4819-157-1-201207030-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hannan EL, Zhong Y, Lahey SJ, Culliford AT, Gold JP, Smith CR, et al. 30-day readmissions after coronary artery bypass graft surgery in New York State. JACC Cardiovasc Interv. 2011;4:569–576. doi: 10.1016/j.jcin.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 16.Kirklin JK, Naftel DC, Pagani FD, Kormos RL, Stevenson LW, Blume ED, et al. Sixth INTERMACS annual report: a 10,000-patient database. J Heart Lung Transplant. 2014;33:555–564. doi: 10.1016/j.healun.2014.04.010. [DOI] [PubMed] [Google Scholar]