Abstract
Background
Intergenerational effects of child abuse have been documented, but it is unknown whether maternal childhood abuse influences offspring mental health in adolescence or adulthood.
Methods
To examine whether maternal experience of childhood abuse is associated with depressive symptoms in adolescent and young adult offspring, we linked data from two large longitudinal cohorts of women (N = 8,882) and their offspring (N = 11,402), and we examined three possible pathways by which maternal experience of abuse might be associated with offspring depressive symptoms: maternal mental health, family characteristics, and offspring’s own experience of abuse.
Results
Offspring of women who experienced severe versus no childhood abuse had greater likelihood of high depressive symptoms (RR = 1.78, 95% CI = 1.47, 2.16) and persistent high depressive symptoms (RR = 2.47, 95% CI = 1.37, 4.44). Maternal mental health accounted for 20.9% and offspring’s exposure to abuse accounted for 30.3% of the elevated risk of high depressive symptoms. Disparities in offspring depressive symptoms by maternal abuse exposure were evident at age 12 years and persisted through age 31 years.
Conclusions
Findings provide evidence that childhood abuse adversely affects the mental health of the victim’s offspring well into adulthood. As offspring exposure to abuse and maternal mental health accounted for more than 50% of the elevated risk of high depressive symptoms among offspring of women who experienced abuse, improving maternal mental health and parenting practices may reduce offspring risk for depressive symptoms in these families.
Keywords: child abuse, sexual abuse, depression, adult offspring, adolescent, maternal behavior
INTRODUCTION
Childhood abuse is common and is associated with poorer mental health across the lifespan.[1–4] Recent research has suggested that young children of women who experienced abuse may also be adversely affected.[5–9] However, it remains largely unknown whether mental health disparities in offspring of women who experienced abuse persist into adolescence and adulthood.
To date, few studies have examined maternal childhood abuse in association with offspring mental health in adolescence or beyond. These studies have been conducted in moderate-sized samples, often selected from clinics, with mixed findings. A study of 125 British families found that maternal exposure to abuse predicted antisocial behavior but not depressive symptoms in offspring.[10] A study of 318 children from a mental health clinic found externalizing and behavioral symptoms, but not internalizing symptoms, were higher in offspring of mothers who experienced abuse.[11] Studies in a sample of parents with mood disorders found anxiety and mood disorder[6, 12] and suicide risk[13] but not non-suicidal self-injury[14] higher in adult offspring of parents who experienced childhood abuse.
Maternal childhood abuse may increase risk for offspring depression through at least three interrelated mechanisms. First, women who experience childhood abuse are at risk of poor mental health, which has been linked through insensitive and inconsistent parenting behaviors[15] and insecure attachment[16] to depression in offspring.[17–20] Second, abuse is associated with adulthood family characteristics that have been linked to depression, including lower socioeconomic status (SES) and divorce.[21] Finally, women who have experienced abuse are more likely to have children who are themselves abused.[22, 23] However, it remains unknown which of these mechanisms, if any, links maternal experience of abuse with offspring risk of depression.
Depressive symptoms in adolescence have been associated prospectively with worse grades and poorer health-related quality of life in adolescence,[24] and increased risk of suicidality, major depression, anxiety disorders,[25] early childrearing, and dysfunctional parenting in adulthood.[26] If offspring of women who experienced abuse are at elevated risk for depressive symptoms, interventions could be targeted to this population.
In the present study, we link data from two large longitudinal cohorts of women (the Nurses’ Health Study II, NHSII) and their offspring (the Growing Up Today Study, GUTS) to examine whether maternal experience of abuse is associated with depressive symptoms in adolescent and young adult offspring. We hypothesize that maternal experience of abuse will increase risk of offspring’s depressive symptoms through three interrelated mechanisms: maternal mental health, family characteristics, and offspring exposure to abuse.
METHODS
SAMPLE
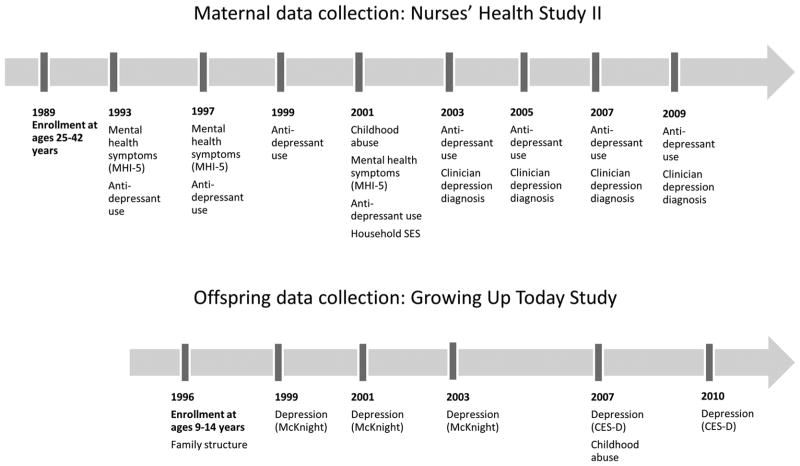
The NHSII comprises 116,430 nurses recruited in 1989 at ages 25–42 and followed biennially with mailed or web-based questionnaires. The Growing Up Today Study (GUTS) comprises 16,882 of their offspring, enrolled in 1996 and followed annually or biennially with mailed or web-based questionnaires. A total of 34,174 NHSII participants with children ages 9–14 were invited to enroll in GUTS, and 54% (n = 18,526) consented. Approximately 58% of boys (n = 7,843) and 68% of girls (n = 9,039) returned completed questionnaires. Participants were ages 12–19 in 1999, the first wave in which depressive symptoms were assessed, and ages 23–31 at the 2010 wave, the most recent wave in which depression was assessed. Figure 1 shows the data collection timeline for mothers (NHSII) and offspring (GUTS).
Figure 1.
Timeline of data collection in Nurses’ Health Study II (mothers) and the Growing Up Today Study (offspring).
MEASURES
Maternal Childhood Abuse
Maternal experience of childhood abuse was queried in NHSII in 2001. Physical/emotional abuse before age 11 years was assessed with the physical and emotional abuse sub-scale of the Childhood Trauma Questionnaire[27] and was coded in quartiles (0: lowest quartile to 3: highest quartile) to examine a possible dose–response association between abuse and offspring depressive symptoms. In a validation study, the scale had good internal consistency (Cronbach’s α = 0.94) and test-retest reliability (intraclass correlation = 0.82) over a 2- to 6-month interval.[27] The Childhood Trauma Questionnaire queries being punished with a hard object like a belt, receiving cruel punishments, being hit so hard that it left bruises, family members saying hurtful or insulting things, and family members yelling or screaming at the respondent. Women in the lowest quartile rarely or never had any of these experiences. Women in the highest quartile had all or nearly all these experiences sometimes, often or very often. Unwanted sexual experiences as a child (before age 11) and as a teenager (ages 11–17) were queried. For each time period, two questions from a national poll were asked: “Were you ever touched in a sexual way by an adult or older child or were you forced to touch an adult or older child in a sexual way when you did not want to?” and “Did an adult or older child ever force you or attempt to force you into any sexual activity by threatening you, holding you down, or hurting you in some way when you did not want to,” for a total of four questions on sexual abuse.[28, 29] Women were considered to have experience mild abuse if they responded “once” to one or two of these questions, or “more than once” to one of these questions. Women were considered to have experienced severe sexual abuse if they responded “once” or “more than once” to three or more of these questions with at least one response of “more than once.” Women with more than mild and less than severe abuse were considered to have experienced moderate abuse.
A combined score of physical, emotional, and sexual abuse was also created by summing physical/emotional abuse (in quartiles, 0–3) and sexual abuse (coded 0–3). Due to low prevalence of the most severe level of abuse, we combined the top two levels to create a score that ranged from 0 (no abuse) to 5 (severe abuse).[30, 31] Women in the no abuse group (a score of 0) had reported no unwanted sexual experiences and were in the lowest quartile of physical/emotional abuse. Women in the middle group (a score of 3) had typically reported mild or moderate sexual abuse and were in the second or third quartile of physical/emotional abuse, or had not experienced sexual abuse and were in the top quartile of physical/emotional abuse. Women in the severe abuse group (a score of 5) had experienced moderate or severe sexual abuse and 80% were in the top quartile of physical/emotional abuse, with the remainder in the third quartile of physical/emotional abuse.
Offspring Depressive Symptoms
Offspring depressive symptoms were assessed with the Depression Symptoms Scale of the McK-night Risk Factor Survey[32] in GUTS in 1999, 2001, and 2003 and with the Center for Epidemiological Studies Depression Scale–10 (CESD-10)[33] in 2007 and 2010. The McKnight Survey is comprised of six questions querying respondent’s past-year symptoms (response options, 0: never to 4: always). Responses were averaged, following scale recommendations.[32] The CESD-10 measures ten past-week depressive symptoms (response options, 0: rarely to 3: all of the time). Responses were summed to create a score ranging from 0 to 30. McK-night scores were highly correlated with CESD scores in a validation study.[32]
Two criteria have been used to select CESD cutoff values indicating high depressive symptoms/probable depression. Cutoffs have been selected: (1) so that the prevalence of scores above the cutoff matches the prevalence of depression in the relevant population;[34, 35] or (2) to identify a specific percentile of the sample (e.g., 20, 10, or 5%).[34, 36, 37] The estimated prevalence of major depression among adolescents and young adults in the US ranges from 5.3 to 11%.[38–40] We therefore created a cutoff score capturing the highest 10% of CESD scores (>14). To facilitate analyses using both measures, and as the McKnight scale does not provide a cutoff to indicate probable depression,[41] we similarly dichotomized the McKnight scale at the highest 10% of our sample (>2.0). For sensitivity analyses, we created a more stringent cutoff capturing the highest 5% of CESD (>16) and McKnight scores (>2.2) in our sample. We also separately z-scored CESD and McK-night scores to create a single continuous variable.
We considered respondents to have “persistent high depressive symptoms” if they were in the highest 10% of the sample at three or more waves. We conducted sensitivity analyses with persistent high depressive symptoms defined as having high symptoms at: (1) four or more waves and; (2) all five waves.
Potential Mediators
Maternal mental health
Information on maternal mental health was collected in a number of ways over the course of NHSII. Maternal past-4-week mental health symptoms were measured in NHSII in 1993, 1997, and 2001 with the Mental Health Index of the Medical Outcomes Study Short Form Health Survey (SF-36 MHI-5).[42] The MHI-5 has good psychometric properties in detecting affective disorders, including depression and anxiety,[43–47] and scores are strongly associated with the number of diagnoses met.[47] Maternal MHI-5 score at each of these three waves was included as a separate variable. Maternal past-2-year antidepressant use was assessed in eight waves in NHSII, 1993–2009. Although antidepressants have some non-mental-health indications, they are most commonly used to treat depressive and anxiety disorders.[48–50] Antidepressant use in 1993 and 1997, which were prior to the first assessment of offspring depressive symptoms, were coded as individual variables. An additional time-varying “recent antidepressant use” variable was created from reported antidepressant use at the wave most proximate to report of offspring depressive symptoms. Maternal lifetime history of clinician’s diagnosis of depression was by self-report in NHSII in 2003, updated in 2005, 2007, and 2009. Each maternal mental health indicator was entered as a separate variable.
Family characteristics
Maternal self-reported household income and subjective social standing in her community and in the US were assessed in NHSII in 2001.[51] US Census tract median income and percentage college educated were obtained from geocoded residential addresses. Offspring’s family structure was assessed in GUTS in 1996 by the question “Which adults do you live with most of the time?” and was coded as: both parents, one parent, or one parent and a stepparent.
Offspring experience of abuse
Offspring experience of physical, emotional, and sexual abuse before age 11 years was assessed in GUTS in 2007 at offspring ages 20–28 years, using four questions from the Childhood Trauma Questionnaire querying physical and emotional abuse,[27] two questions from the Conflict Tactic Scales querying threatened or actual physical assault,[52] and two questions querying forced touching or sexual activity by an adult or an older child.[28] Based on their distributions, physical/emotional abuse was coded in quintiles; physical assault was coded as none, moderate, or serious; and sexual abuse was coded as none, mild, moderate or severe. Child’s witness of violence before age 11 was queried with six items regarding frequency of seeing or hearing an adult use physical force (e.g., shove, punch) or verbally abuse (e.g., threaten, degrade) his/her mother, another adult, or a child. Each item was coded: never, once, a few times, or more than a few time and entered as separate variables.
ANALYSES
To examine offspring depressive symptoms across adolescence and young adulthood by maternal exposure to childhood abuse, we pooled data from all waves and computed cross-tabulations of high depressive symptoms by maternal childhood abuse at offspring ages 12–14, 15–17, 18–20, 21–24, and 25–31, using SAS PROC FREQ.
To investigate whether offspring of women exposed to abuse were at greater risk of high depressive symptoms adjusted for covariates, we calculated risk of offspring high depressive symptoms with maternal exposure to combined childhood abuse as the independent variable, using data from all waves in a repeated measures framework. We used a generalized estimating equation to account for the covariation of an individual’s depressive symptoms across multiple waves and covariation in depressive symptoms among siblings, as some women enrolled more than one child in GUTS. To estimate risk ratios, we used a log link and Poisson distribution in SAS PROC GENMOD.[53] The model was adjusted for maternal parents’ education, coded as high school or less, some college, or college or more, maternal parents’ home ownership in her infancy, coded as yes or no, and offspring’s sex, age, and race/ethnicity.
To determine whether offspring of women exposed versus unexposed to childhood abuse were at greater risk of persistent high depressive symptoms, we modeled persistent high depressive symptoms as the dependent variable with maternal exposure to childhood abuse as the independent variable, among offspring with three or more waves of data on depressive symptoms. In this model, we used a generalized estimating equation to account for covariation in depressive symptoms among siblings. To estimate risk ratios, we used a log link and Poisson distribution.[53] The model was adjusted for maternal parents’ education, coded as high school or less, some college, or college or more, maternal parents’ home ownership in her infancy, coded as yes or no, and offspring’s sex, age, race/ethnicity and the number of waves of data with depressive symptoms, ranging from 3 to 5, coded categorically. As strong sex differences in the prevalence of depression emerge in adolescence and persist into adulthood,[54] we investigated whether associations between maternal abuse and offspring depressive symptoms differed by offspring’s sex. We tested an offspring’s-sex-by-maternal-childhood-abuse interaction term in models of both high depressive symptoms and persistent high depressive symptoms.
Mediation Analyses
Next, we examined whether an association between maternal exposure to childhood abuse and offspring’s risk of high depressive symptoms was accounted for by our hypothesized mediators. We first added maternal mental health indicators to the model (i.e., mental health symptoms, antidepressant use, and self-report of clinical diagnosis of depression). Next, we additionally adjusted for family characteristics. Last, we further adjusted for offspring’s exposure to abuse. To determine the proportion of the association accounted for by each set of mediators, we estimated a model with all mediators then compared coefficients from this model with coefficients from three models, each removing only one of the three sets of mediators (indicators of maternal mental health, family structure, and offspring’s exposure to abuse). The proportion of the association explained by a set of intermediaries was: 100 × [1- (exposure coefficient estimate with all three intermediary sets/exposure coefficient estimate without the intermediary set of interest)].
Sensitivity Analyses
We examined the association of maternal abuse and high depressive symptoms with high depressive symptoms dichotomized at the stricter 5% cutoff and with depressive symptoms as a continuous variable. We examined the association of maternal abuse and persistent high depressive symptoms with persistent high depressive symptoms alternatively defined as: (1) high depressive symptoms in four waves, restricted to offspring with at least four waves of data, N = 6,141; and (2) high depressive symptoms in all five waves, restricted to offspring with five waves of data, N = 3,837). To ascertain the association of maternal exposure to specific types of childhood abuse with offspring depression, we modeled offspring’s high depressive symptoms with maternal exposure to: (1) childhood physical/emotional abuse; and (2) sexual abuse as the independent variables in separate models; and (3) both physical/emotional and sexual abuse as separate independent variables in the same model. We also predicted offspring’s persistent high depressive symptoms in models with maternal exposure to either childhood physical/emotional abuse, sexual abuse, or both as the independent variables. To determine whether maternal childhood abuse was associated with offspring depressive symptoms even among offspring who did not experience childhood abuse, we restricted our sample to offspring who experienced no physical/emotional abuse, no threatened or actual physical assault, and no sexual abuse (N = 3,103, 27.2% of offspring). As the majority of our sample was white, we ascertained whether associations were similar among nonwhites by restricting our sample to nonwhites (N offspring = 720, 6.3% of offspring). Finally, we considered whether maternal grandparents’ depression might be a prior common cause of maternal experience of childhood abuse and offspring depression. In 2005, NHSII participants were asked whether their mother or father had major clinical depression before age 50 years. We adjusted for maternal grandmother’s clinical depression, coded yes or no, and maternal grandfather’s clinical depression, coded yes or no, in a sensitivity analysis.
Missing Data
In analyses of high depressive symptoms we included all offspring with report of maternal childhood abuse and at least one report of depressive symptoms (N = 11,402). In analyses of persistent high depressive symptoms we included offspring with report of maternal childhood abuse and with three or more reports of depressive symptoms (N = 8,108). For these included participants, fewer than 5% of values were missing for mediators and covariates except household income (14% missing) and offspring’s own abuse exposure, which was queried in the 12th year of GUTS (31% missing). For models examining mediation by offspring experience of childhood abuse, we restricted to offspring with data on childhood abuse. Association of maternal experience of abuse with offspring depressive symptoms was very similar in offspring with and without data on childhood abuse. For all other missing covariates and mediators, we used single imputation in the following order: (1) prior wave value carried forward, (2) subsequent wave value carried back, (3) mean value at each level of maternal abuse.
Included versus excluded offspring were similar in maternal exposure to childhood abuse (no abuse, 26.2 vs. 25.3%; severe abuse, 4.5 vs. 4.5%), prevalence of high depressive symptoms at baseline (6.5 vs. 7.6%), and offspring experience of sexual abuse (severe abuse, 1.3 vs. 1.6%, all P > .05). Included versus excluded offspring were more likely to be female (62.6 vs. 45.9%), more likely to be living with both parents in 1996 (76.2 vs. 55.7%), less likely to have a mother who used antidepressants regularly in the past 2 years (in 1993, 8.7 vs. 10.1%) and less likely to have experienced high levels of physical/emotional abuse (top quartile of CTQ, 15.5 vs. 20.6%, all P < .05).
To examine possible effects of missing data, we conducted sensitivity analyses using the statistical technique of inverse probability weighting.[55] Specifically, we created a variable indicating whether a given offspring in the GUTS cohort was included or not included in our multivariate analyses. We then estimated his or her probability of inclusion using as predictors: offspring race, sex, age, and childhood family structure, and maternal antidepressant use, depression diagnosis, mental health index (MHI-5), self-reported socioeconomic status, household income, Census tract median income, Census tract percentage college educated, maternal parental education in childhood, and maternal parental home ownership in her infancy. We then weighted the included respondents by the inverse of this probability. Probability of inclusion was calculated separately for analyses of high depressive symptoms and persistent high depressive symptoms.
RESULTS
One-fourth of offspring (26.1%, n=2,981) had mothers who reported no exposure to childhood physical, emotional, or sexual abuse, and approximately 5% of offspring (4.5%, n=517) had mothers who reported severe childhood abuse. Women who reported severe abuse versus those who reported no abuse were more likely to have recently taken antidepressants (27.7 vs. 11.6%), to have ever received a clinician’s diagnosis of depression (43.1 vs. 16.1%), and to have lower adulthood SES (Table 1). Offspring of women who experienced childhood abuse were less likely to live with both parents at GUTS baseline (1996) and more likely to themselves report experiences of childhood abuse than offspring of women who reported no abuse (Table 1).
TABLE 1.
Demographic characteristics and potential mediators by maternal experience of childhood abuse, Nurses’ Health Study II and Growing Up Today Study, N mothers = 8,882; N children = 11,402a
| Maternal experience of childhood abuseb
|
|||||||
|---|---|---|---|---|---|---|---|
| 0: no abuse (N = 2,981) | 1 (N = 2,618) | 2 (N = 2,204) | 3 (N = 2,179) | 4 (N = 903) | 5: severe abuse (N = 517) | ||
| Demographic characteristics | |||||||
| Maternal childhood SES | |||||||
| Parental education, college, or more | % (n) | 32.33 (900) | 27.56 (682) | 27.61 (569) | 24.47 (507) | 21.35 (180) | 19.35 (90) |
| Parents owned home in infancy | % (n) | 57.13 (1,582) | 56.47 (1,393) | 53.03 (1,084) | 52.46 (1,078) | 48.40 (409) | 51.92 (243) |
| Offspring’s race | |||||||
| Black | % (n) | 0.40 (12) | 0.65 (17) | 0.73 (16) | 0.55 (12) | 1.90 (17) | 0.97 (5) |
| Asian | % (n) | 1.21 (36) | 1.45 (38) | 1.73 (38) | 1.20 (26) | 1.79 (16) | 3.10 (16) |
| Hispanic | % (n) | 0.98 (29) | 1.11 (29) | 1.41 (31) | 2.12 (46) | 2.90 (26) | 1.94 (10) |
| White | % (n) | 95.45 (2,834) | 94.30 (2,466) | 93.18 (2,047) | 92.86 (2,017) | 90.51 (811) | 91.09 (470) |
| Others | % (n) | 1.95 (58) | 2.49 (65) | 2.96 (65) | 3.27 (71) | 2.90 (26) | 2.91 (15) |
| Sex | |||||||
| Male | % (n) | 45.22 (1,348) | 43.43 (1,137) | 42.74 (941) | 41.95 (914) | 42.86 (387) | 41.20 (213) |
| Potential mediator: maternal mental health | |||||||
| Maternal mental health (mental health inventory-5, higher is better health) | |||||||
| 1993 | Mean | 75.65 | 73.77 | 71.86 | 70.48 | 70.10 | 68.86 |
| 1997 | Mean | 77.56 | 75.38 | 73.70 | 71.87 | 71.76 | 70.82 |
| 2001 | Mean | 78.24 | 76.39 | 73.71 | 72.60 | 71.43 | 70.55 |
| Maternal recent antidepressant use (across all waves) | % (n) | 11.60 | 14.13 | 15.28 | 18.78 | 20.47 | 27.67 |
| Maternal lifetime depression diagnosis | |||||||
| 2003 | % (n) | 7.46 (220) | 9.93 (258) | 12.26 (268) | 15.78 (342) | 18.80 (169) | 25.98 (132) |
| 2009 | % (n) | 16.11 (461) | 20.67 (522) | 25.25 (535) | 30.84 (651) | 34.93 (307) | 43.09 (212) |
| Potential mediator: family characteristics | |||||||
| Maternal adulthood SES | |||||||
| US social standing (lower score indicates higher SES), 2001 | Mean | 3.73 | 3.82 | 3.85 | 3.93 | 3.93 | 4.19 |
| Community social standing (lower score indicates higher SES), 2001 | Mean | 3.80 | 3.87 | 3.99 | 4.16 | 4.01 | 4.39 |
| Household annual income category, 2001 (reported in nine levels, from <$15,000 to ≥$150,000) | Mean | 7.00 | 7.01 | 7.02 | 6.95 | 6.92 | 6.71 |
| US Census tract median household income, 1989–1995 ($) | Mean | 65,404 | 64,328 | 64,010 | 64,363 | 63,421 | 62,148 |
| US Census tract percentagecollege educated, 1989–1995 | Mean | 31.94 | 31.64 | 30.90 | 31.19 | 30.74 | 29.40 |
| Family structure, 1996 | |||||||
| Two parents | % (n) | 76.12 (2,269) | 75.63 (1,980) | 72.82 (1,605) | 70.67 (1,540) | 69.10 (624) | 69.63 (360) |
| Potential mediator: offspring’s experience of abuse | |||||||
| Child trauma questionnaire (physical and emotional abuse Subscale), top quintile | % (n) | 11.47 (236) | 14.02 (252) | 16.96 (261) | 19.07 (286) | 17.90 (111) | 21.45 (77) |
| Conflict tactics scale, top levelc | % (n) | 6.56 (135) | 8.07 (145) | 10.07 (155) | 11.47 (172) | 12.44 (77) | 12.53 (45) |
| Sexual abuse (any) | % (n) | 5.02 (107) | 5.05 (94) | 7.09 (114) | 6.99 (108) | 8.18 (53) | 11.61 (44) |
| Witness family physical violence (any) | % (n) | 9.04 (184) | 10.92 (194) | 13.76 (209) | 15.98 (237) | 19.61 (120) | 17.05 (60) |
| Witness family emotional abuse (any) | % (n) | 20.54 (418) | 21.34 (379) | 25.28 (384) | 30.61 (454) | 29.58 (181) | 34.09 (120) |
The unit of analysis in this table is offspring. Ns may not sum to column totals as missing values are not included.
Women in the no abuse group (a score of 0) had reported no unwanted sexual experiences and were in the lowest quartile of physical/emotional abuse. Women in the middle group (a score of 3) had typically reported mild or moderate sexual abuse and were in the second or third quartile of physical/emotional abuse, or had not experienced sexual abuse and were in the top quartile of physical/emotional abuse. Women in the severe abuse group (a score of 5) had experienced moderate or severe sexual abuse and 80% were in the top quartile of physical/emotional abuse, with the remainder in the third quartile of physical/emotional abuse.
Offspring at the highest level of the Conflict Tactics Scale reported an adult in the family threatened to kick, punch, hit with something, or physically attack sometimes or more often, or were actually kicked, punched, hit with something, or physically attacked sometimes or more often, or experienced both threats and actual events rarely or more often.
Offspring of women who experienced childhood abuse had higher prevalence of high depressive symptoms from age 12 through age 31 years. Greater maternal childhood abuse severity was associated with greater prevalence of offspring’s high depressive symptoms in an approximately monotonic fashion (Fig. 2).
Figure 2.
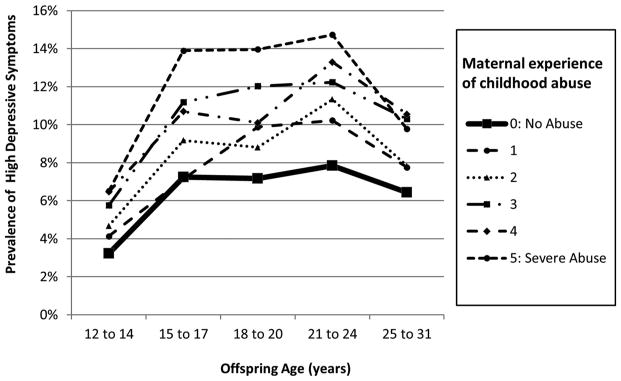
Highest decile of depressive symptoms across adolescence and young adulthood in offspring by maternal childhood experience of physical, emotional, and sexual abuse, N mothers = 8,882; N offspring = 11,402; N observations (offspring) = 39,213.
In models adjusted for maternal childhood SES and offspring’s age, sex, and race, offspring of women who experienced abuse had greater risk of high depressive symptoms than offspring of nonabused women (RR range = 1.20–1.78; RR severe abuse = 1.78, 95% CI = 1.47, 2.16; Table 2, Model 1). This association did not differ by offspring sex (P > .05). Adding maternal mental health indicators, family characteristics, and offspring’s exposure to abuse attenuated this association (Table 2, Models 2–4).
TABLE 2.
Maternal experience of childhood abuse and offspring’s age-adjusted high depressive symptoms across adolescence and young adulthood, Nurses’ Health Study II and Growing Up Today Study, N mothers = 8,882; N offspring = 11,402; N observations (offspring) = 39,213a
| N offspring | Risk ratio (95% CI)
|
||||
|---|---|---|---|---|---|
| Model 1: adjusted for demographic variables | Model 2: Model 1, further adjusted for maternal mental health indicators | Model 3: Model 2, further adjusted for adolescent SES and family structure | Model 4: Model 3, further adjusted for offspring’s experience of abuseb | ||
| Maternal experience of childhood abuse | |||||
| 0: no abuse | 2,981 | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| 1 | 2,618 | 1.20 (1.06, 1.36)c | 1.16 (1.02, 1.31)b | 1.16 (1.03, 1.32)b | 1.14 (0.99, 1.31) |
| 2 | 2,204 | 1.29 (1.13, 1.47)d | 1.20 (1.05, 1.37)c | 1.20 (1.05, 1.36)c | 1.13 (0.98, 1.30) |
| 3 | 2,179 | 1.56 (1.38, 1.77)d | 1.41 (1.25, 1.60)d | 1.40 (1.24, 1.59)d | 1.30 (1.13, 1.50)d |
| 4 | 903 | 1.52 (1.30, 1.79)d | 1.37 (1.16, 1.60)d | 1.36 (1.16, 1.60)d | 1.25 (1.04, 1.50)b |
| 5: severe abuse | 517 | 1.78 (1.47, 2.16)d | 1.53 (1.26, 1.87)d | 1.51 (1.24, 1.85)d | 1.30 (1.04, 1.63)b |
Models 1, 2, and 3 include the same participants; the stated N mothers, N offspring, and N observations applies. Model 4 is restricted to offspring with childhood abuse data; results for Model 1 in this subsample were similar to those in the whole sample (RR range = 1.22, 1.83, RR severe abuse = 1.83, 95% CI = 1.47, 2.29). All models adjusted for offspring’s age, sex, and race/ethnicity, and maternal childhood socioeconomic status. Risk ratios estimated using generalized estimating equations with log link and Poisson distributions, calculated using SAS PROC GENMOD.
P < .05.
P < .01.
P < .001
Among offspring with complete data on childhood abuse, associations with maternal abuse and depressive symptoms were very similar to those found among all offspring (RR range = 1.22, 1.83, RR severe abuse = 1.83, 95% CI = 1.47, 2.29). In the fully adjusted model (restricted to offspring with data on their own exposure to abuse), including maternal mental health indicators, family characteristics, and offspring’s exposure to abuse, maternal mental health accounted for 20.9%, family characteristics 0.3%, and offspring’s exposure to abuse 30.3% of the association between maternal experience of abuse and offspring’s risk of high depressive symptoms.
Offspring of women exposed to childhood abuse, versus those not exposed, were also at greater risk of persistent high depressive symptoms across adolescence and young adulthood (RR range = 1.42,2.47; RR severe abuse = 2.47, 95% CI = 1.37, 4.44; Table 3, Model 1). This association did not differ by offspring’s sex (sex-by-mother’s-abuse interaction term, P > .05). Maternal mental health indicators, family characteristics, and offspring’s exposure to abuse each attenuated this association (Table 3, Models 2–4). In the fully adjusted model including maternal mental health indicators, family characteristics, and offspring’s exposure to abuse, maternal mental health indicators accounted for 12.2%, family characteristics 0.3%, and offspring’s exposure to abuse 27.6% of the association between women’s experience of abuse and offspring’s risk of persistent high depressive symptoms.
TABLE 3.
Maternal experience of childhood abuse and offspring’s persistent high depressive symptoms across adolescence and young adulthood, Nurses’ Health Study II and Growing Up Today Study, N mothers = 6,692 N offspring = 8,108 N observations (offspring) = 34,302a
| N offspring | Risk ratio (95% CI)
|
||||
|---|---|---|---|---|---|
| Model 1: adjusted for demographic variables | Model 2: Model 1, further adjusted for maternal mental health indicators | Model 3: Model 2, further adjusted for adolescent socioeconomic status and family structure | Model 4: Model 3, further adjusted for offspring’s experience of abuse | ||
| Maternal experience of childhood abuse | |||||
| 0: no abuse | 2,102 | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) | 1.00 (Reference) |
| 1 | 1,850 | 1.42 (0.90, 2.23) | 1.33 (0.85, 2.10) | 1.34 (0.85, 2.12) | 1.36 (0.85, 2.17) |
| 2 | 1,591 | 1.80 (1.16, 2.78)c | 1.59 (1.03, 2.47)b | 1.60 (1.03, 2.48)b | 1.41 (0.90, 2.23) |
| 3 | 1,553 | 2.43 (1.60, 3.69)d | 2.07 (1.36, 3.15)d | 2.04 (1.33, 3.11)d | 1.85(1.18, 2.90)c |
| 4 | 635 | 2.04 (1.22, 3.44)c | 1.72 (1.01, 2.91)b | 1.73 (1.02, 2.92)b | 1.28 (0.71, 2.29) |
| 5: severe abuse | 377 | 2.47 (1.37, 4.44)c | 1.92 (1.05, 3.54)b | 1.85 (0.99, 3.43)b | 1.44 (0.76, 2.70) |
Models 1, 2, and 3 include the same participants; the stated N mothers, N offspring, and N observations applies. Model 4 is restricted to offspring with childhood abuse data; results for Model 1 in this subsample were similar to those in the whole sample (RR range = 1.51, 2.55, RR severe abuse = 2.55, 95% CI = 1.37, 4.76). All models adjusted for offspring’s age, sex, and race/ethnicity, and maternal childhood socioeconomic status. Risk ratios were estimated using generalized estimating equations with a log link and a Poisson distribution, using SAS PROC GENMOD. The sample for this table was restricted to offspring with three or more waves of data on depressive symptoms.
P < .05.
P < .01.
P < .001.
In sensitivity analyses separately examining maternal exposure to childhood physical/emotional and sexual abuse, offspring risk of high depressive symptoms was strongly associated with both maternal physical/emotional (RR range = 1.21, 1.51, Table 4, Model 1a) and sexual abuse (RR range = 1.11, 1.69; Table 4, Model 1b). Risk of high depressive symptoms increased monotonically with the severity of maternal experience of abuse. There was also a strong dose–response relationship between maternal exposure to physical/emotional abuse and her offspring’s risk of persistent high depressive symptoms (RR range = 1.37, 2.13; Table 4, Model 2a). Maternal exposure to sexual abuse was associated with her offspring’s risk of persistent high depressive symptoms (RR range = 0.95, 2.14; Table 4, Model 2b). In models with maternal sexual and physical/emotional abuse entered simultaneously as separate variables, both types of abuse were associated with offspring’s high depressive symptoms (RR top quartile physical abuse = 1.44; RR severe sexual abuse = 1.51).
TABLE 4.
Maternal childhood experience of physical/emotional or sexual abuse and offspring’s risk of high depressive symptoms and persistent high depressive symptoms across adolescence and young adulthood, Nurses’ Health Study II and Growing Up Today Study, N mothers = 8,882 N offspring = 11,402 N observations (offspring) = 39,213d
| Offspring’s high depressive symptoms
|
Offspring’s persistent high depressive symptoms
|
|||
|---|---|---|---|---|
| N offspring | Risk ratio (95% CI) | N offspring | Risk ratio (95% CI) | |
| Model 1a | Model 2a | |||
| Maternal childhood experience of physical/emotional abuse | ||||
| First quartile | 3,945 | 1.00 (Reference) | 2,783 | 1.00 (Reference) |
| Second quartile | 2,519 | 1.21 (1.08, 1.36)c | 1,768 | 1.38 (0.92, 2.07) |
| Third quartile | 2,382 | 1.32 (1.17, 1.48)c | 1,726 | 1.94 (1.34, 2.81)c |
| Fourth quartile | 2,556 | 1.51 (1.35, 1.69)c | 1,831 | 2.15 (1.51, 3.07)c |
| Model 1b | Model 2b | |||
| Maternal childhood experience of sexual abuse | ||||
| None | 7,726 | 1.00 (Reference) | 5,500 | 1.00 (Reference) |
| Mild | 2,665 | 1.12 (1.01, 1.23)a | 1,896 | 0.95 (0.70, 1.30) |
| Moderate | 685 | 1.19 (1.01, 1.40)a | 483 | 1.09 (0.65, 1.84) |
| Severe | 326 | 1.69 (1.37, 2.10)c | 229 | 2.11 (1.25, 3.57)b |
Wald χ2 P < .05.
Wald χ2 P < .01.
Wald χ2 P < .001.
All models were adjusted for sex, and race, and maternal childhood socioeconomic status. Risk ratios were estimated using generalized estimating equations with a log link and Poisson distributions, using SAS PROC GENMOD.
Sensitivity analyses using a more stringent cutoff for high depressive symptoms in offspring (highest 5% of depressive symptoms) showed an even stronger association between maternal exposure to combined childhood abuse and her offspring’s risk of high depressive symptoms (RR range = 1.26, 1.94; RR severe abuse = 1.94, 95% CI = 1.52, 2.47). In sensitivity analyses with offspring’s depressive symptoms coded continuously, maternal childhood abuse was significantly associated with offspring depressive symptoms in an approximately monotonically increasing fashion (severe abuse, B = 0.26, 95% CI = 0.18, 0.34, P < .0001). In analyses defining persistent high depressive symptoms as high depressive symptoms in four or more waves, the association between maternal childhood abuse and persistent high depressive symptoms was stronger (RR severe abuse = 12.38, 95% CI =3.25, 47.16, P < .001). Models examining persistent high depressive symptoms defined as high depressive symptoms in all five waves did not converge, as only 11 offspring had high depressive symptoms in all five waves.
In analyses restricted to offspring not exposed to childhood abuse, maternal abuse remained associated with offspring high depressive symptoms (RR severe abuse = 1.70, 95% CI = 1.08, 2.68). In analyses restricted to nonwhites, offspring’s high depressive symptoms were also associated with maternal abuse (RR severe abuse = 2.31, 95% CI = 1.24, 4.30). Results in models using inverse probability weighting were similar (top 10% depressive symptoms, RR severe abuse = 1.87, 95% CI = 1.46, 2.39). Estimates were nearly identical in models further adjusted for maternal grandmother and grandfather’s clinical depression.
DISCUSSION
We document for the first time in a large population-based sample an association between maternal childhood abuse and depressive symptoms in her adolescent and young adult offspring. Offspring of women severely abused were at more than 1.5 times the risk of high depressive symptoms and nearly 2.5 times the risk of persistent depressive symptoms than offspring of women who did not experience abuse. Disparities in depressive symptoms by maternal abuse exposure were evident at age 12 and persisted through the end of our study period, age 31. Disparities in depressive symptoms were remarkably consistent across adolescence and early adulthood, suggesting that the effects of maternal childhood abuse on the mental health of offspring may be tenacious.
We found larger disparities by maternal abuse when we examined risk of persistent high depressive symptoms and when we used a more stringent cutoff for high depressive symptoms. These results suggest that maternal abuse may be associated not only with higher risk of depressive symptoms but also with more problematic depressive symptoms, as higher scores on the CESD correlate with depression severity[56, 57] and suicidal ideation.[58] Persistent versus episodic depression in emerging adulthood has been linked to more social withdrawal, anxiety, somatic complaints, externalizing behavior and aggression.[59] In mothers, chronic versus brief depression is associated with worse infant cognitive and psychomotor development,[60] findings particularly relevant to our study, as we found elevated depression in the offspring across peak childbearing years, which include ages 20–34.[61]
We found that offspring’s own exposure to abuse accounted for a large part of their increased risk of depressive symptoms. Although it is well known that children of abused versus nonabused parents are themselves at elevated risk of abuse and that abuse harms mental and physical health across the lifecourse, little empirical evidence exists to support the logical consequence that offspring of abused versus nonabused parents are at risk of worse physical and mental health. The present findings contribute to an emerging literature suggesting that effects of childhood abuse cross generations and impact multiple health domains.[5, 7, 11, 14, 30, 31, 62]
Maternal mental health also explained a moderate portion of the association we found. Studies have indicated that maternal mental health is associated with offspring depression independently of shared genetics.[17, 18] Maternal depression and anxiety have been linked to less parenting satisfaction, more controlling and less affectionate parenting, parenting dysfunction, and more interpersonal stress,[26, 63, 64] which may increase offspring risk of depression through offspring exposure to stress, greater physiological response to stress,[65] and diminished social competence.[66]
Our findings should be considered in light of several limitations. Our sample is comprised mostly of white women, reflecting the racial composition of the nursing profession at the time of study enrollment. However, among nonwhites the association between maternal abuse and offspring depressive symptoms was similar to that of the whole sample. Because our sample is comprised of professional nurses, women who were most profoundly affected by their experiences of abuse (e.g., women who were unable to complete their education) may not be represented. Such sampling bias may result in underestimation of the true association of maternal abuse with offspring depression. Maternal childhood abuse was by retrospective self-report, which, like all measures of childhood abuse, is subject to error.[67] If, for example, women’s current mental health affected recall of childhood abuse, our estimates may be biased. Our study also has important strengths. Depressive symptoms were assessed directly in the offspring at five waves. We assessed maternal childhood abuse by her own report and assessed potential mediators repeatedly and prospectively. The large sample enabled us to examine possible differences by offspring sex in the effects of abuse.
Our findings suggest important avenues for preventing depressive symptoms in offspring of women who experienced abuse. Several interventions have been found to be effective in improving parenting and preventing child abuse.[68–70] Because these interventions affect multiple domains of maternal and family functioning, they are cost effective even strictly in terms of reducing net government expenditure.[68] The present study contributes to a growing literature indicating that pregnant women and mothers of young children should be screened for history of childhood abuse and offered interventions to improve their own well-being and to prevent potentially serious long-term health disparities in their offspring.
Acknowledgments
This study was funded by NIH R01HD057368 (to SBA) and K01MH092526 (to KAM). The Nurses’ Health Study II is funded in part by NIH CA50385. We thank the Channing Division of Network Medicine of Brigham and Women’s Hospital and Harvard Medical School, Boston, for its supervision of the Nurses’ Health Study II and the Growing Up Today Study. The funders played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Contract grant sponsor: NIH; Contract grant numbers: R01HD057368, K01MH092526, and CA50385.
Footnotes
Conflict of interest. The authors report no conflicts of interest
References
- 1.Anda RF, Felitti VJ, Bremner JD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. 2006;256(3):174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anda RF, Brown DW, Felitti VJ, Dube SR, Giles WH. Adverse childhood experiences and prescription drug use in a cohort study of adult HMO patients. BMC Public Health. 2008;8:198–206. doi: 10.1186/1471-2458-8-198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anda RF, Croft JB, Felitti VJ, et al. Adverse childhood experiences and smoking during adolescence and adulthood. JAMA. 1999;282(17):1652–1658. doi: 10.1001/jama.282.17.1652. [DOI] [PubMed] [Google Scholar]
- 4.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Am JPrev Med. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 5.Bailey JA, Hill KG, Oesterle S, Hawkins JD. Parenting practices and problem behavior across three generations: monitoring, harsh discipline, and drug use in the intergenerational transmission of externalizing behavior. Dev Psychol. 2009;45(5):1214–1226. doi: 10.1037/a0016129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oquendo MA, Ellis SP, Chesin MS, et al. Familial transmission of parental mood disorders: unipolar and bipolar disorders in offspring. Bipolar Disord. 2013;15(7):764–773. doi: 10.1111/bdi.12107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Collishaw S, Dunn J, O’Connor TG, et al. Maternal childhood abuse and offspring adjustment over time. Dev Psychopathol. 2007;19(2):367–383. doi: 10.1017/S0954579407070186. [DOI] [PubMed] [Google Scholar]
- 8.Roberts R, O’Connor T, Dunn J, Golding J. The effects of child sexual abuse in later family life; mental health, parenting and adjustment of offspring. Child Abuse Negl. 2004;28(5):525–545. doi: 10.1016/j.chiabu.2003.07.006. [DOI] [PubMed] [Google Scholar]
- 9.Burkett LP. Parenting behaviors of women who were sexually abused as children in their families of origin. Fam Process. 1991;30(4):421–434. doi: 10.1111/j.1545-5300.1991.00421.x. [DOI] [PubMed] [Google Scholar]
- 10.Plant D, Barker ED, Waters C, Pawlby S, Pariante C. Intergenerational transmission of maltreatment and psychopathology: the role of antenatal depression. Psychol Med. 2013;43(03):519–528. doi: 10.1017/S0033291712001298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miranda JK, dela Osa N, Granero R, Ezpeleta L. Multiple mediators of the relationships among maternal childhood abuse, intimate partner violence, and offspring psychopathology. J Interpers Violence. 2013;28(14):2941–2965. doi: 10.1177/0886260513488686. [DOI] [PubMed] [Google Scholar]
- 12.Brent DA, Oquendo M, Birmaher B, et al. Familial transmission of mood disorders: convergence and divergence with transmission of suicidal behavior. J Am Acad Child Adolesc Psychiatry. 2004;43(10):1259–1266. doi: 10.1097/01.chi.0000135619.38392.78. [DOI] [PubMed] [Google Scholar]
- 13.Melhem NM, Brent DA, Ziegler M, et al. Familial pathways to early-onset suicidal behavior: familial and individual antecedents of suicidal behavior. Am J Psychiatry. 2007;164(9):1364–1370. doi: 10.1176/appi.ajp.2007.06091522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cox LJ, Stanley BH, Melhem NM, et al. Familial and individual correlates of nonsuicidal self-injury in the offspring of mood-disordered parents. J Clin Psychiatry. 2012;73(6):813–820. doi: 10.4088/JCP.11m07196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martins C, Gaffan EA. Effects of early maternal depression on patterns of infant-mother attachment: a meta-analytic investigation. J Child Psychol Psychiatry. 2000;41:737–746. [PubMed] [Google Scholar]
- 16.Atkinson L, Paglia A, Coolbear J, Niccols A, Parker KCH, Guger S. Attachment security: a meta-analysis of maternal mental health correlates. Clin Psychol Rev. 2000;20(8):1019–1040. doi: 10.1016/s0272-7358(99)00023-9. [DOI] [PubMed] [Google Scholar]
- 17.Lewis G, Rice F, Harold GT, Collishaw S, Thapar A. Investigating environmental links between parent depression and child depressive/anxiety symptoms using an assisted conception design. J Am Acad Child Adolesc Psychiatry. 2011;50(5):451–459. doi: 10.1016/j.jaac.2011.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh AL, D’Onofrio BM, Slutske WS, et al. Parental depression and offspring psychopathology: a Children of Twins study. Psychol Med. 2011;41(7):1385–1395. doi: 10.1017/S0033291710002059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barker ED, Jaffee SR, Uher R, Maughan B. The contribution of prenatal and postnatal maternal anxiety and depression to child maladjustment. Depress Anxiety. 2011;28(8):696–702. doi: 10.1002/da.20856. [DOI] [PubMed] [Google Scholar]
- 20.Starr LR, Conway CC, Hammen CL, Brennan PA. Transdiagnostic and disorder-specific models of intergenerational transmission of internalizing pathology. Psychol Med. 2014;44(01):161–172. doi: 10.1017/S003329171300055X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Everson SA, Maty SC, Lynch JW, Kaplan GA. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity, and diabetes. J Psychosom Res. 2002;53(4):891–895. doi: 10.1016/s0022-3999(02)00303-3. [DOI] [PubMed] [Google Scholar]
- 22.Pawlby S, Hay D, Sharp D, Waters CS, Pariante CM. Antenatal depression and offspring psychopathology: the influence of childhood maltreatment. Br J Psychiatry 2011. 2011;199(2):106–112. doi: 10.1192/bjp.bp.110.087734. [DOI] [PubMed] [Google Scholar]
- 23.Berlin LJ, Appleyard K, Dodge KA. Intergenerational continuity in child maltreatment: mediating mechanisms and implications for prevention. Child Dev. 2011;82(1):162–176. doi: 10.1111/j.1467-8624.2010.01547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jaycox LH, Stein BD, Paddock S, et al. Impact of teen depression on academic, social, and physical functioning. Pediatrics. 2009;124(4):e596–e605. doi: 10.1542/peds.2008-3348. [DOI] [PubMed] [Google Scholar]
- 25.Fergusson D, Horwood L, Ridder E, Beautrais A. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch Gen Psychiatry. 2005;62(1):66–72. doi: 10.1001/archpsyc.62.1.66. [DOI] [PubMed] [Google Scholar]
- 26.Hammen C, Brennan PA, LeBrocque R. Youth depression and early childrearing: stress generation and intergenerational transmission of depression. J Consult Clin Psychol. 2011;79(3):353–363. doi: 10.1037/a0023536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bernstein DP, Fink L, Handelsman L, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151(8):1132–1136. doi: 10.1176/ajp.151.8.1132. [DOI] [PubMed] [Google Scholar]
- 28.Moore D, Gallup G, Schussel R. Disciplining children in America: A Gallup poll report. Princeton, NJ: The Gallup Organization; 1995. [Google Scholar]
- 29.Finkelhor D, Moore D, Hamby SL, Straus MA. Sexually abused children in a national survey of parents: methodological issues. Child Abuse Negl. 1997;21(1):1–9. doi: 10.1016/s0145-2134(96)00127-5. [DOI] [PubMed] [Google Scholar]
- 30.Roberts AL, Galea S, Austin SB, Corliss HL, Williams MA, Koenen KC. Women’s experience of abuse in childhood and their children’s smoking and overweight. Am J Prev Med. 2014;46(3):249–258. doi: 10.1016/j.amepre.2013.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Roberts AL, Lyall K, Rich-Edwards JW, Ascherio A, Weisskopf MG. Association of maternal exposure to childhood abuse with elevated risk for autism in offspring. JAMA Psychiatry. 2013;70(5):508–515. doi: 10.1001/jamapsychiatry.2013.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shisslak CM, Renger R, Sharpe T, et al. Development and evaluation of the McKnight Risk Factor Survey for assessing potential risk and protective factors for disordered eating in preadolescent and adolescent girls. Int J Eat Disord. 1999;25(2):195–214. doi: 10.1002/(sici)1098-108x(199903)25:2<195::aid-eat9>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 33.Radloff LS. The CES-D scale: a self report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 34.Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. J Youth Adolesc. 1991;20(2):149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- 35.Chabrol H, Montovany A, Chouicha K, Duconge E. Study of the CES-D on a sample of 1953 adolescent students. L’Encephale. 2001;28(5 Pt 1):429–432. [PubMed] [Google Scholar]
- 36.Doerfler LA, Felner RD, Rowlison RT, Raley PA, Evans E. Depression in children and adolescents: a comparative analysis of the utility and construct validity of two assessment measures. J Consult Clin Psychol. 1988;56(5):769–772. doi: 10.1037//0022-006x.56.5.769. [DOI] [PubMed] [Google Scholar]
- 37.Opoliner A, Carwile JL, Blacker D, Fitzmaurice GM, Austin SB. Early and late menarche and risk of depressive symptoms in young adulthood. Arch Womens Ment Health. 2014;17:1–8. doi: 10.1007/s00737-014-0435-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rushton JL, Forcier M, Schectman RM. Epidemiology of depressive symptoms in the national longitudinal study of adolescent health. J Am Acad Child Adolesc Psychiatry. 2002;41(2):199–205. doi: 10.1097/00004583-200202000-00014. [DOI] [PubMed] [Google Scholar]
- 39.CDC. Current Depression Among Adults — United States, 2006 and 2008. Morbidity and Mortality Weekly Report. 2010 Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5938a2.htm. [PubMed]
- 40.Saluja G, Iachan R, Scheidt PC, Overpeck MD, Sun W, Giedd JN. Prevalence of and risk factors for depressive symptoms among young adolescents. Arch Pediatrics Adolesc Med. 2004;158(8):760–765. doi: 10.1001/archpedi.158.8.760. [DOI] [PubMed] [Google Scholar]
- 41.Laboratory for the Study of Behavioral Medicine. [Accessed November 5, 2014];Scoring guide for the McKnight Risk Factor Survey. Available at: http://bml.stanford.edu/resources/
- 42.Ware J, Snow K, Kosinski M, Gandek B. SF-36 Health Survey: Manual & Interpretation Guide. Boston: The Health Institute, New England Medical Center; 1993. [Google Scholar]
- 43.Berwick DM, Murphy JM, Goldman PA, Ware JE, Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991;29(2):169–176. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- 44.Strand BH, Dalgard OS, Tambs K, Rognerud M. Measuring the mental health status of the Norwegian population: a comparison of the instruments SCL-25, SCL-10, SCL-5 and MHI-5 (SF-36) Nord J Psychiatry. 2003;57(2):113–118. doi: 10.1080/08039480310000932. [DOI] [PubMed] [Google Scholar]
- 45.Rumpf H-J, Meyer C, Hapke U, John U. Screening for mental health: validity of the MHI-5 using DSM-IV Axis I psychiatric disorders as gold standard. Psychiatry Res. 2001;105(3):243–253. doi: 10.1016/s0165-1781(01)00329-8. [DOI] [PubMed] [Google Scholar]
- 46.Means-Christensen AJ, Arnau RC, Tonidandel AM, Bramson R, Meagher MW. An efficient method of identifying major depression and panic disorder in primary care. J Behav Med. 2005;28(6):565–572. doi: 10.1007/s10865-005-9023-6. [DOI] [PubMed] [Google Scholar]
- 47.Cuijpers P, Smits N, Donker T, ten Have M, deGraaf R. Screening for mood and anxiety disorders with the five-item, the three-item, and the two-item Mental Health Inventory. Psychiatry Res. 2009;168(3):250–255. doi: 10.1016/j.psychres.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 48.Hollingworth SA, Burgess PM, Whiteford HA. Affective and anxiety disorders: prevalence, treatment and antidepressant medication use. Aust N Z J Psychiatry. 2010;44(6):513–519. doi: 10.3109/00048670903555138. [DOI] [PubMed] [Google Scholar]
- 49.Harris MG, Burgess PM, Pirkis J, Siskind D, Slade T, Whiteford HA. Correlates of antidepressant and anxiolytic, hypnotic or sedative medication use in an Australian community sample. Aust N Z J Psychiatry. 2011;45(3):249–260. doi: 10.3109/00048674.2010.531459. [DOI] [PubMed] [Google Scholar]
- 50.Patten SB, Esposito E, Carter B. Reasons for antidepressant prescriptions in Canada. Pharmacoepidemiol Drug Saf. 2007;16(7):746–752. doi: 10.1002/pds.1385. [DOI] [PubMed] [Google Scholar]
- 51.Giatti L, do Camelo LV, Rodrigues JF, Barreto SM. Reliability of the MacArthur scale of subjective social status - Brazilian Longitudinal Study of Adult Health (ELSA-Brasil) BMC Public Health. 2012;12:1096–1102. doi: 10.1186/1471-2458-12-1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Straus MA, Hamby SL, Boney-McCoy SUE, Sugarman DB. The Revised Conflict Tactics Scales (CTS2) J Fam Issues. 1996;17(3):283–316. [Google Scholar]
- 53.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 54.Cyranowski JM, Frank E, Young E, Shear MK. Adolescent onset of the gender difference in lifetime rates of major depression: a theoretical model. Arch Gen Psychiatry. 2000;57(1):21–27. doi: 10.1001/archpsyc.57.1.21. [DOI] [PubMed] [Google Scholar]
- 55.Hogan JW, Lancaster T. Instrumental variables and inverse probability weighting for causal inference from longitudinal observational studies. Stat Methods Med Res. 2004;13(1):17–48. doi: 10.1191/0962280204sm351ra. [DOI] [PubMed] [Google Scholar]
- 56.Santor DA, Zuroff DC, Ramsay J, Cervantes P, Palacios J. Examining scale discriminability in the BDI and CES-D as a function of depressive severity. Psychol Assess. 1995;7(2):131–139. [Google Scholar]
- 57.Husaini BA, Neff JA, Harrington JB, Hughes MD, Stone RH. Depression in rural communities: validating the CES-D scale. J Community Psychol. 1980;8(1):20–27. [Google Scholar]
- 58.Allison S, Roeger L, Martin G, Keeves J. Gender differences in the relationship between depression and suicidal ideation in young adolescents. Aust N Z J Psychiatry. 2001;35(4):498–503. doi: 10.1046/j.1440-1614.2001.00927.x. [DOI] [PubMed] [Google Scholar]
- 59.Barrett AE, Turner RJ. Family structure and mental health: the mediating effects of socioeconomic status, family process, and social stress. J Health Soc Behavior. 2005;46(2):156–169. doi: 10.1177/002214650504600203. [DOI] [PubMed] [Google Scholar]
- 60.Cornish A, McMahon C, Ungerer J, Barnett B, Kowalenko N, Tennant C. Postnatal depression and infant cognitive and motor development in the second postnatal year: the impact of depression chronicity and infant gender. Infant Behav Dev. 2005;28(4):407–417. [Google Scholar]
- 61.Dye JL. US Census Bureau, editor. Fertility of American women: June 2008. Washington, DC: US Department of Commerce; 2010. [Google Scholar]
- 62.Mahedy L, Heron J, Stapinski LA, et al. Mothers’ own recollections of being parented and risk of offspring depression 18 years later: a prospective cohort study. Depress Anxiety. 2014;31(1):38–43. doi: 10.1002/da.22174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gerlsma C, Emmelkamp PMG, Arrindell WA. Anxiety, depression, and perception of early parenting: a meta-analysis. Clin Psychol Rev. 1990;10(3):251–277. [Google Scholar]
- 64.Berz JB, Taft CT, Watkins LE, Monson CM. Associations between PTSD symptoms and parenting satisfaction in a female veteran sample. J Psychol Trauma. 2008;7(1):37–45. [Google Scholar]
- 65.Essex MJ, Klein MH, Cho E, Kalin NH. Maternal stress beginning in infancy may sensitize children to later stress exposure: effects on cortisol and behavior. Biol Psychiatry. 2002;52(8):776–784. doi: 10.1016/s0006-3223(02)01553-6. [DOI] [PubMed] [Google Scholar]
- 66.Hammen C, Shih JH, Brennan PA. Intergenerational transmission of depression: test of an interpersonal stress model in a community sample. J Consult Clin Psychol. 2004;72(3):511–522. doi: 10.1037/0022-006X.72.3.511. [DOI] [PubMed] [Google Scholar]
- 67.Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry. 2004;45(2):260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- 68.Olds DL, Kitzman HJ, Cole RE, et al. Enduring effects of prenatal and infancy home visiting by nurses on maternal life course and government spending: follow-up of a randomized trial among children at age 12 years. Arch Pediatr Adolesc Med. 2010;164(5):419–424. doi: 10.1001/archpediatrics.2010.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Olds DL, Eckenrode J, Henderson CR, Jr, et al. Long-term effects of home visitation on maternal life course and child abuse and neglect. Fifteen-year follow-up of a randomized trial. JAMA. 1997;278(8):637–643. [PubMed] [Google Scholar]
- 70.Olds DL, Henderson CR, Chamberlin R, Tatelbaum R. Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics. 1986;78(1):65–78. [PubMed] [Google Scholar]