Abstract
Anticoagulant use, such as heparin, is usually contraindicated in acute stroke patients. We present a study of patients, who were treated with intravenous heparin after a stroke that were also found to have an intraluminal thrombus. Prior studies imply that recanalization is achieved with heparin; however heparin should only prevent thrombus propagation. Therefore it is unclear whether and how IV heparin can achieve recanalization of intraluminal thrombi in acute stroke patients. A retrospective review of all acute stroke patients from a single stroke center who received a therapeutic IV heparin infusion from 5/2006 to 9/2011 were included in the study. We compared patients who had complete/partial recanalization and/or improved flow versus those that did not, with both these groups on a standard intravenous heparin infusion protocol. Demographic data was compared between the groups. Average partial thromboplastin time (PTT) during heparin infusion, time between computed tomography angiographies (CTAs), time from stroke onset to receiving IV heparin, and vessel occluded were also compared between groups. Forty-one patients (19 female, 22 male) were included in the study with a total of 55 vessels (either carotid, middle cerebral artery, anterior cerebral artery, posterior cerebral artery/posterior circulation) having intraluminal thrombi; 31 patients had 41 vessels with either partial or complete recanalization of effected vessels, while 10 patients had 14 vessels that did not have at least one vessel recanalize while on heparin. Using t-test we noted that the average PTT between the vessels that had partial/complete recanalization group (61.74) and nonrecanalization group (66.30) was not statistical significantly different (P=0.37).The average time in days on heparin between vascular imaging studies (CTA/conventional angiogram) in the group of vessels with partial/complete recanalization (7.12 days) and the ones with no change (6.11 days) was not significantly different between the two groups (P=0.59). Patient’s vessels receiving heparin for <24 hours versus those >24 hours did not significantly differ either (P=0.17). This study compares patient characteristics associated with recanalization of intraluminal thrombi in acute stroke patients on heparin. Recanalization of intraluminal thrombi are not associated with average PTT or duration on heparin.
Key words: Heparin, stroke, thrombus, recanalization
Introduction
Meyer and Struzziero described the use of heparin in acute stroke models in 1958.1 They administered heparin to monkeys and cats and observed differences in ischemia and cerebral circulation. The heparin treated animals showed that an increase of collateral blood flow produced more rapid resumption of normal flow in ischemic areas than in untreated animals although resulting perivascular hemorrhages might be extensive. Although heparin was likely used in circulation experiments prior to this study, it was clear that reperfusion and improved collateral circulation sometimes came at the cost of reperfusion injury and bleeding. However, due to the morbidity and mortality of stroke, heparin and anticoagulants continued to be an option for acute stroke treatment from the 1950’s,2 until the development and confirmation of efficacy of tissue plasminogen activator. However, it did not completely negate the use of anticoagulants in stroke. The Trial of ORG 10172 (danaparoid) in Acute Ischemic Stroke Treatment (TOAST) delineated the need to subtype stroke etiology, but it was not successful in showing clinical benefit of a heparinoid in clinical outcomes of acute stroke patients.3 This study did not include imaging data including computed tomography angiography (CTA) or magnetic resonance angiography (MRA) data as a guide to determine which patients may benefit from anticoagulation therapy and advocated these modalities be used in future studies.3
As mentioned, hemorrhage remains the primary adverse event that limits heparin use in acute stroke.4-7 Hemorrhagic conversion of ischemic brain in stroke patients can be difficult to manage, especially in stroke patients who received thrombolytics like intravenous tissue plasminogen activators.8 Reversing anticoagulation after intracranial hemorrhage can also be a clinical challenge.
A Cochrane Collaborative Review demonstrated additional lack of evidence of anticoagulation use in acute stroke patients. This meta-analysis showed that anticoagulation lowered the chance of recurrent ischemic stroke but also increased the risk of hemorrhage. Subgroup analysis was not performed, but the authors of this study state that …it is unclear whether a subgroup of patients who have strokes in progression with intraluminal thrombi might benefit from the use of anticoagulation like IV heparin in the acute period following an ischemic stroke. Again, they contend that the increased risk of hemorrhage precludes the effective use of anticoagulation in all acute stroke patients.9 Multiple small studies and case series have shown utility and improved outcome as well as recanalization when using heparin or other anticoagulants in stroke patients.10-12 But there remain several questions as to how heparin is able to improve recanalization.
Although, recanalization does not necessarily mean clinical improvement, prior studies imply recanalization is achieved with heparin.10-12 But, based on its physiology, heparin should only prevent thrombus propagation. However, it appears to be doing more than preventing propagation of thrombus.
This study investigates ischemic stroke patients who presented with identifiable intra-arterial thrombi who were administered heparin and determine if duration of heparin treatment, partial thromboplastin time (PTT), location of occlusion, or a particular demographic of patients was associated with recanalization.
Materials and Methods
Institutional review board approval was granted for a retrospective review of all patient admissions to a high volume stroke center where we collected the patient information including demographic data, of all patients who were admitted for stroke between May 2006 and September 2011 and were treated with heparin or heparinoids for intraluminal thrombi of the carotids or intracranial vessels. In addition to clinical diagnosis by a neurologist, imaging studies, either magnetic resonance imaging (MRI) or computed tomography perfusion (CTP), computer were used to confirm that these patients had a stroke, and CTA or conventional cerebral angiogram was used to confirm the presence of intraluminal thrombi by a radiologist. Those patients who had serial CT angiograms or conventional angiograms of the carotid and intracranial large vessels were included in the study for comparison after heparin administration. Time between stroke onset and start of heparin was recorded in hours. A standard IV heparin protocol was used in all cases and mean PTT during the heparin administration was noted. All but one patient was concurrently on aspirin and/or Plavix. Duration on heparin and duration between imaging studies were noted. Radiologists reviewed images for changes to the intraluminal thrombi of internal carotids, vertebral, basilar, middle, anterior, and posterior cerebral arteries. These changes were noted as either complete, partial, or no recanalization by the radiologists. A neurologist also confirmed these findings. In order to reduce potential confounding factors associated with demographic data, vessels were compared rather than individuals.
Results
A total of 41 patients (22 males, 19 females) were included in the study, with a total of 55 vessels (28 male vessels, 27 female vessels) involved (either middle cerebral artery, anterior cerebral artery, posterior cerebral artery/posterior circulation, or carotids). While 14 patients (7 males, 7 females) had 14 vessels (7 from male, 7 from female) that had no recanalization or no change in the intraluminal thrombus of at least one vessel, 31 patients with 41 vessels (as some patients had multi-vessel involvement) had complete or partial recanalization with 20 of those vessels belonging to female patients and 21 belonging to male patients. However using the Pearson Chi-Square test, this difference was not statistically significant between male and female with at least some recanalization versus no recanalization (Figure 1).
Figure 1.
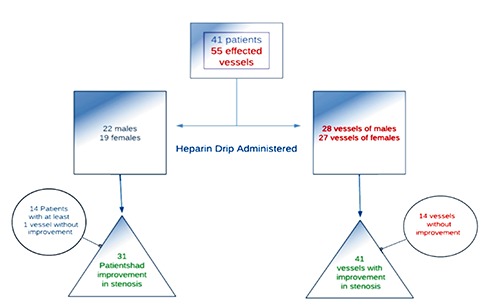
Flowchart summarizing the result of the study.
The mean age between the partial/complete recanalization group (63.65 years old) and non-recanalization group (67.8 years old) was not statistically different using the t-test (P=0.46). The mean duration on heparin/heparinoids was 7.12 days for the partial/complete recanalization group (41 vessels) and 6.11 days for the non-recanalization group (14 vessels), but there was no statistical difference between them, using the t-test (P=0.38). The mean PTT was 61.7 for the partial/complete recanalization group and 66.3 for the non-recanalization group but again with no statistical difference between them, again, using the t-test (P=0.395). Additionally, comparing patient’s vessels that were on heparin for >24 hours versus those <24 hours did not show a statistical difference in recanalization (P=0.129) using the Pearson Chi-square test (Table 1). Although the number of patients who partially to completely recanalize versus those that did not was not significant, when individual locations of vessels were compared (carotid, MCA, PCA, ACA, and posterior circulation or multi-vessel involvement), the number of MCA thrombi that partially or completely recanalized (19 MCA vessels) was significantly higher than those that did not (2 MCA vessels) when compared to carotid, while on heparin, using the Pearson Chi-square test (P=0.014). However, the other vessels (MCA, ACA, PCA, basilar, vertebral, and AICA/PICA) were not statistically significant (Table 2).
Table 1.
Patient age and patient associated heparin infusion data.
| Recanalization | No recanalization | P-value | |
|---|---|---|---|
| Average age (years) | 63.65 | 67.80 | 0.46 |
| Mean duration on heparin drip (days) | 7.12 | 6.11 | 0.68 |
| Mean partial thromboplastin time while on heparin (sec) | 61.8 | 66.3 | 0.18 |
| Number of patients >24 hrs on heparin | 8 | 3 | 0.17 |
Table 2.
Vessel data: median coronary artery recanalization significant compared to carotid recanalization.
| Vessels recanalized | Vessels without change | Total vessels | P-value (Chi-square) | |
|---|---|---|---|---|
| MCA | 19 | 2 | 21 | 0.014 |
| ACA | 4 | 0 | 4 | 0.091 |
| Posterior circulation (PCA, basilar, vertebral, AICA, PICA) | 11 | 6 | 17 | 0.547 |
| Carotids | 7 | 6 | 13 | NA |
MCA, median coronary artery; ACA, anterior coronary artery; PCA, posterior coronary artery; AICA, anterior inferior cerebellar artery; PICA;
In a logistic regression model comparing the carotid vessels with the other vessels (i.e. MCA, ACA, and posterior circulation), showed an odds ratio (OR) of 3.64 (P=0.058, 95%CI: 0.959 to 13.843) for likelihood of at least some recanalization with heparin; unfortunately this was not statistically significant but may indicate a trend. Additional logistic regression model comparing the MCA vessels with the carotids, showed an OR=8.14 (P=0.024, 95%CI: 1.32 to 50.25); suggesting heparin may improve recanalization in MCA vessels better than in the carotids. The anterior circulation (MCA and ACA) in comparison to the posterior circulation (PCA, basilar, vertebral, and AICA/PICA), demonstrated an OR=6.273 (P=0.04, 95%CI: 1.085 to 36.249) in our logistic regression model. Of course this data must be taken in light of a univariate analysis that may have associated confounding factors that were able to be accounted for in these models.
Discussion
As mentioned above, the idea of heparin improving intracranial stenosis and thrombosis is not new. A study from 1978 showed resolution of cerebral vessel thrombosis after heparin was given on conventional cerebral angiogram.10 However, our study does suggest that intracranial vessels and associated clot burdens respond to heparin administration differently. Recanalization leads to improved outcomes in stroke patients. With large trials, like CREST and SAMPRIS, showing non-superiority to medical management, it remains controversial whether mechanical recanalization leads to better outcomes than medical recanalization, especially in patients with large vessel thrombi.
Use of any anticoagulation and antiplatelet agents, are contraindicated in acute stroke patients receiving TPA in the first 24 hours, but antiplatelets are initiated after the first 24 hours if no hemorrhage is noted on follow-up imaging after the first 24 hours. Despite guideline contra-indicating it, the use of anticoagulation in strokes in progression has been suggested for the last few decades.11-13 Recently there have been reports of use of antiplatelet agents along with or within the first 24 hours of giving thrombolytics in stroke patients.14,15 This remains a controversial topic but it appears that a select group of patients may see benefit from earlier initiation of antiplatelet agents.
This study demonstrates that for most stroke patients, anticoagulation is not an efficient mechanism to achieve recanalization. Duration on heparin, PTT, or demographic data, did not significantly associate with complete or partial recanalization. There may appear to be a difference in heparin’s effect on recanalization based on the type of vessel involved, but more likely related to thrombus characters which was not part of our analysis.
With any study of this size, there is additional unknown confounding data such as prior use of anti-platelets or anti-coagulation, which was not collected and multivariate analysis was not performed. But this was a small study from a single center using a single IV heparin protocol. It is noted that almost all patients in this study were concurrently on antiplatelet agents, which may improve the efficacy of heparin effects. Additionally, this study did not review clinical outcomes of patients, but did include parameters of heparin administration and efficacy including average PTT.
Conclusions
Heparin use in acute stroke patients remains contraindicated, but there may be a population of stroke patients who may benefit from its ability to recanalize intracerebral vessels. Heparin may not work equally or as efficiently to improve stenosis or occlusions in all intracranial vessels. Continued study of heparin or heparinoids in acute stroke patients should be considered in specific cases.
References
- 1.Meyer JS. Localized changes in properties of the blood and effects of anticoagulant drugs in experimental cerebral infarction. N Engl J Med 1958;258:151-9. [DOI] [PubMed] [Google Scholar]
- 2.Fisher CM. Cerebrovascular diseases: pathophysiology, diagnosis, and treatment. J Chron Dis 1958;8:419-47. [DOI] [PubMed] [Google Scholar]
- 3.The Publications Committee for the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) Investigators. Low molecular weight heparinoid, ORG 10172 (danaparoid), and outcome after acute ischemic stroke: a randomized controlled trial. JAMA 1998;279:1265-72. [PubMed] [Google Scholar]
- 4.Benatar M. Heparin use in acute ischaemic stroke: does evidence change practice? QJM 2005;98:147-52. [DOI] [PubMed] [Google Scholar]
- 5.Babikian VL, Kase CS, Pessin MS, et al. Intracerebral hemorrhage in stroke patients anticoagulated with heparin. Stroke 1989;20:1500-3. [DOI] [PubMed] [Google Scholar]
- 6.Sandercock PAG, Counsell C, Tseng MC. Low-molecular-weight heparins or heparinoids versus standard unfractionated heparin for acute ischaemic stroke (Review). Available from: http://www.update-software.com/pdf/CD000119.pdf. [Google Scholar]
- 7.Sandercock PAG, Counsell C, Kamal AK. Anticoagulants for acute ischaemic stroke (Review). Available from: http://www.bibliotecacochrane.com/PDF/CD000024.pdf [DOI] [PubMed] [Google Scholar]
- 8.Brunner F, Tomandl B, Schröter A, et al. Hemorrhagic complications after systemic thrombolysis in acute stroke patients with abnormal baseline coagulation. Eur J Neurol 2011;18:1407-11. [DOI] [PubMed] [Google Scholar]
- 9.Sandercock PA, Gibson LM, Liu M. Anticoagulants for preventing recurrence following presumed non-cardioembolic ischaemic stroke or transient ischaemic attack. Cochrane Database Syst Rev 2009:CD000248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yarnell P, Earnest M, Kelly G, Sanders B. Disappearing carotid defects. Stroke 1978;9:258-62. [DOI] [PubMed] [Google Scholar]
- 11.Dobkin BH. Heparin for lacunar stroke in progression. Stroke 1983;14:421-3. [DOI] [PubMed] [Google Scholar]
- 12.Mokin M, Kass-Hout T, Kass-Hout O, et al. Intravenous heparin for the treatment of intraluminal thrombus in patients with acute ischemic stroke: a case series. J Neurointerv Surg 2013;5:144-50. [DOI] [PubMed] [Google Scholar]
- 13.Yatsu FM. Acute medical therapy of strokes. Stroke 1982;13:524-6. [DOI] [PubMed] [Google Scholar]
- 14.Zinkstok SM, Roos YB. ARTIS investigators. Early administration of aspirin in patients treated with alteplase for acute ischaemic stroke: a randomised controlled trial. Lancet 2012;380:731-7. [DOI] [PubMed] [Google Scholar]
- 15.Zinkstok SM, Vermeulen M, Stam J, et al. A randomised controlled trial of antiplatelet therapy in combination with Rt-PA thrombolysis in ischemic stroke: rationale and design of the ARTIS-Trial. Trials 2010;11:51. [DOI] [PMC free article] [PubMed] [Google Scholar]


