Abstract
Congenital dyserythropoietic anemias (CDA) represent a heterogeneous group of disorders characterized by morphological abnormalities of erythroid precursor cells and various degrees of hemolysis. Iron overload is a result of continuous hemolysis and recurrent transfusions. It is treated with iron chelators, including deferasirox. We present here a case of acute liver failure in a 12 years old girl with CDA type I treated with deferasirox and discuss the approach to treatment.
Key words: Congenital dyserythropoietic anemia, deferasirox, acute liver failure, N-acetylcysteine
Introduction
Congenital dyserythropoietic anemias (CDA) represent a heterogeneous group of disorders characterized by morphological abnormalities of erythroid precursor cells and various degrees of hemolysis. Three classical types of CDAs are distinguished by differences in bone marrow morphology.1 CDA type I results from mutation of CDAN1 gene encoding a codanin-1 protein which plays a role in regulation of chromatin structure and cell cycle transition.2 CDA type II stems from mutation of SEC23B gene with resultant defect in glycosylation of intracellular vesicle proteins and accumulation of endoplasmatic reticulum remnants in the cytoplasm of erythroid precursors.3,4 CDA type III has been recently attributed to mutation of a KIF23 gene, that encodes a kinesin family protein MKLP1, endowed with crucial role in cytokinesis.5 CDA type I is rare, with less than 200 cases from 143 families reported worldwide.6 The cumulative incidence of CDA type I in Europe is estimated to be 0.24 cases/million [ibid]. It is particularly prevalent in Israeli Bedouin population, being reported in 70 consanguineous Bedouin families.7
Congenital dyserythropoietic anemias should be suspected in patients with symptoms and signs of mild hemolysis, namely jaundice, low haptoglobin and high reticulocyte count that does not match the severity of anemia.6 Iron overload, cholelithiasis and splenomegaly are the most important complications of CDA. Most CDA patients suffer from mild to moderate anemia and usually do not require blood transfusions. In patients with iron overload, as judged by elevated ferritin concentration in peripheral blood, iron chelation should be administered.
Iron chelators are agents that bind iron and excrete it in a non-toxic form. Deferasirox is once-daily oral iron chelating agent with good bio-availability and long half-life of 8-16 hours. It is a generally well tolerated drug with side-effects of mild to moderate severity. The most common side effects are skin eruptions, elevation of serum creatinine, and gastrointestinal adverse ones.8,9 The most common gastrointestinal side effects of deferasirox are diarrhea (33%), nausea and vomiting (21%), abdominal pain (8%) and constipation (6%). Hepatic adverse effects of deferasirox are usually mild (elevated transaminases), but several cases of liver failure in adult patients have been observed in clinical trials (EX-JADE® prescribing information, Novartis, Stein, Switzerland) and in clinical practice.9,10
We present here a case of acute liver failure in a 12 years old girl with CDA type I treated with deferasirox and discuss the approach to treatment.
Case Report
Twelve-year old girl of Bedouin origin with CDA type I (missense R1042W mutation of the CDAN1 gene) was admitted due to vomiting, progressing jaundice and abdominal pain for several days. The patient was afebrile. Three months prior to the admission the deferasirox treatment (26 mg/kg/day) was initiated by the hematologist because of iron overload – significantly elevated serum ferritin concentration of 537.6 ng/mL (<8-142) and decreased transferring level – 187 mg/dL (240-360). The patient has not received any other medication prior to appearance of symptoms. On admission the patient was alert and oriented with normal vital signs. The physical examination was remarkable for jaundice. The abdomen was soft, without hepatosplenomegaly. Laboratory investigations revealed evidence of normocytic normochromic anemia (hemoglobin 7.2 g/dL, otherwise normal blood count), direct hyperbilirunemia with total and direct bilirubin concentrations of 11.3 (0.3-1.2) mg/dL and 5.9 (0-0.3) mg/dL, respectively. Serum concentrations of GOT, GPT and GGT were elevated: 329 (0-47), 345 (0-49) and 376 (0-17) U/L, respectively. INR was elevated (2.03), clotting factors V and VII levels were low, 43 (62-139%) and 21 (66-143%), respectively, but serum albumin and glucose were normal. Serum concentrations of iron was of 319 ug/mL (43-184), ferritin of 218.5 ng/mL (<8-142), transferrin of 280 mg/dL (240-360), and transferrin saturation of 89.8% (15-50), respectively. Deferasirox treatment was discontinued, intravenous fluids, cefotaxime, vitamin K and intravenous ranitidine were initiated. Despite the treatment, patient’s condition continued to deteriorate with progression of direct hyperbilirubinemia, with the highest total and direct bilirubin concentrations of 21 and 14.2 mg/dL, respectively. Serum transaminases elevated in a similar fashion with peak levels of GOT, GPT and GGT of 414, 541 and 72 U/L, respectively. Blood ammonia concentration remained normal. N-acetyl cysteine (NAC, 100 mg/kg/day) treatment was initiated on the second day of hospitalization. Liver biopsy was performed after exclusion of other etiologies: serological tests for hepatitis A, B and C, EBV and CMV did not reveal evidence of acute infection, metabolic screen, including serum ceruloplasmin, and 1-antithrypsine was normal, antinuclear antibody was negative, anti-smooth muscle and antimitochondrial antibodies were within normal range, Doppler-ultrasound examination of liver was normal. Canalicular cholestasis was observed without evidence of fibrosis, inflammation, hemosiderosis, necrosis, fatty changes or ductal reaction. Copper liver content was of 50 µg/g dry liver weight (normal range 10-50). A possibility of acute liver failure due to deferasirox treatment was considered. NAC treatment, that was initiated on 2nd admission day and resulted in rapid return of bilirubin, transaminases and INR to baseline values, was discontinued after five days (Figure 1). The patient’s clinical condition and laboratory parameters remained normal.
Figure 1.
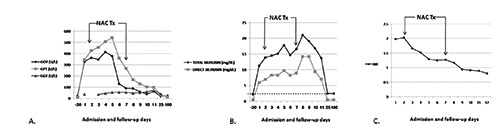
Changes of selected laboratory parameters during the course of the disease and follow-up. Intitiation and termination of N-acetylcysteine (NAC) treatment is indicated by arrows. A) Liver enzymes. B) Total and direct bilirubin. Dashed line indicates patient's baseline level of total bilirubin. C) International normalized ratio.
Discussion
We report a case of deferasirox-induced liver failure in a child with CDA type I and discuss an approach to treatment based on use of N-acetyl cysteine. To the best of our knowledge, this is the first case of deferasirox-induced acute liver failure in the pediatric practice.
Drug-induced liver injury accounts for more than 50% of the cases of acute liver failure in the USA, has an annual incidence of 1 in 10,000-100,000, and is reported after use of more than 1000 medications.11,12 Several mechanisms have been implicated in its pathogenesis, including drug-induced direct hepatotoxicity and secondary activation of innate and adaptive immune responses by damaged hepatocyte. Direct drug-induced hepatotoxicity probably results from enhanced apoptosis of hepatocytes following exposure to offending drug.13 Indeed, given the relatively low serum ferritin level of 218.5 (<8-142) ng/mL at the time of admission, a possibility of direct deferasirox toxicity in the setting of low iron overload should be considered.
Albeit the precise mechanism of deferasirox-induced liver damage remains obscure, one is tempted to consider its ability to induce apoptosis of hepatocytes with resultant liver damage. Recent evidence clearly demonstrates pro-apoptotic activity of deferasirox. Kim et al. have shown the ability of the drug to induce caspase-dependent apoptosis of myeloid leukemia cell line.14 Messa et al. demonstrated its ability to inhibit NF-κB with resultant enhancement of apoptotic rate of leukemia cell lines.15 Cumulatively, these observations, if extrapolated, might provide a plausible explanation of direct hepatotoxicity mechanism of deferasirox.
Codanin-1 is important for controlling cell-cycle transition in S-phase by means of regulating chromatin assembly.16 Disruption of cell cycle regulating protein’s function might result in increased sensitivity of cells to apoptosis. Indeed, silencing of the Drosophila discs lost gene, homologous to human CDAN1, resulted in increased rate of apoptosis, probably caspase-independent.17
In this context, of particular interest is ability of N-acetylcysteine to protect hepatocytes from apoptotic death in an animal model of fulminant hepatic failure by modulation of Bcl-2 and Bax genes.18 This effect of N-acetylcysteine differs from canonical hepatoprotective mechanism of the medication, which is based on its ability to replenish cellular glutathion stores and to reverse oxidative damage and might explain its efficacy in our case.19 Of note, Bcl-2 protein in known to protect the cells from both caspase-dependent and caspase-independent apoptosis.20
Conclusions
We described here a case of acute liver failure in deferasirox treated child with CDA type I, attribute the direct hepatotoxicity of the drug to its possible pro-apoptotic effect and describe the beneficial effect of N-acetylcysteine treatment. Given the theoretical possibility of increased sensitivity of hepatocytes to apoptosis in CDA type I patients and the possibility of increased toxicity risk at the setting of low iron load, we suggest using deferasirox in these patients with frequent liver function testing and immediate discontinuation of the medicine following drop of serum ferritin concentration below 300 ng/mL threshold.
References
- 1.Iolascon A, Russo R, Delaunay J. Congenital dyserythropoietic anemias. Curr Opin Hematol 2011;18:146-51. [DOI] [PubMed] [Google Scholar]
- 2.Dgany O, Avidan N, Delaunay J, et al. Congenital dyserythropoietic anemia type I is caused by mutations in codanin-1. Am J Hum Genet 2002;71:1467-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bianchi P, Fermo E, Vercellati C, et al. Congenital dyserythropoietic anemia type II (CDA II) is caused by mutation in the SEC23B gene. Hum Mut 2009;30:1292-8. [DOI] [PubMed] [Google Scholar]
- 4.Schwarz K, Iolascon A, Verissimo F, et al. Mutations affecting the secretory COPII coat component SEC23B cause congenital dyserythropoietic anemia type II. Nat Genet 2009;41:936-40. [DOI] [PubMed] [Google Scholar]
- 5.Liljeholm M, Irvine A, Vikberg AL, et al. Congenital dyserythropoetic anemia type III (CDA III) is caused by a mutation in kinesin family member, KIF23. Blood 2013;121:4791-9. [DOI] [PubMed] [Google Scholar]
- 6.Iolascon A, Esposita M, Russo R. Clinical aspects and pathogenesis of congenital dyseryhtropoietic anemias: from morphology to molecular approach. Haematologica 2012;97:1786-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tamary H, Dgany O. Congenital dyserythropoietic anemia type I. Pagon R, Adam M, Ardinger H, et al., eds. Source: GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2015. [Google Scholar]
- 8.Adams R, Bird R. Safety and efficacy of deferasirox in the management of transfusion-dependent patients with myelodysplastic syndrome and aplastic anemia: a perspective review. Ther Adv Hematol 2013;4:93-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nolte F, Angelucci E, Beris P, et al. Clinical management of gastrointestinal disturbances in patients with myelodysplastic syndromes receiving iron chelation treatment with deferasirox. Leuk Res 2011;35:1131-5. [DOI] [PubMed] [Google Scholar]
- 10.Aslam N, Mettu P, Marsano-Obando L, Martin A. Deferasinox induced liver injury in haemochromatosis. J Coll Physicians Surg Pak 2010;20:551-3. [PubMed] [Google Scholar]
- 11.Ostapowicz G, Fontana RJ, Schiødt FV, et al. Results of a prospective study of acute liver failure and 17 tertiary care centers in the United States. Ann Intern Med 2002;137:947-54. [DOI] [PubMed] [Google Scholar]
- 12.Grant M, Rockey D. Drug-induced liver injury. Curr Opin Gastroentrol 2012;28:198-202. [DOI] [PubMed] [Google Scholar]
- 13.Kaplowitz N. Drug-induced liver injury. Clin Inf Dis 2004;38:S44-8. [DOI] [PubMed] [Google Scholar]
- 14.Kim JL, Kang HN, Kang MH, et al. The oral iron chelator deferasirox induces apoptosis in myeloid leukemia cells by targeting caspase. Acta Haematol 2011;126:241-5. [DOI] [PubMed] [Google Scholar]
- 15.Messa E, Carturan S, Maffè C, et al. Deferasirox is a powerful NF-κB inhibitor in myelodysplactic cells and in leukemia cell lines acting independently from cell iron deprivation by chelation and reactive oxygen species scavenging. Haematologica 2010;95:1308-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ask K, Jasencakova Z, Menard P, et al. Codanin-1, mutated in the anaemic disease CDAI, regulates Asf1 function in S-phase histone supply. EMBO J 2012;31:2013-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pielage J, Stork T, Bunse I, Klämbt C. The Drosophila cell survival gene discs lost encodes a cytoplasmic codanin-1-like protein, not a homolog of tight junction PDZ protein Patj. Dev Cell 2003;5:841-5. [DOI] [PubMed] [Google Scholar]
- 18.San-Miguel B, Alvarez M, Culebras J, et al. N-acetyl-cysteine protects liver from apoptotic death in an animal model of fulminant hepatic failure. Apoptosis 2006;11:1945-57. [DOI] [PubMed] [Google Scholar]
- 19.Rushworth G, Megson I. Existing and potential therapeutic uses for N-acetylcysteine: The need for conversion to intracellular glutathione for antioxidant benefits. Pharmacol Therapeutics 2014;141:150-9. [DOI] [PubMed] [Google Scholar]
- 20.Okuno S, Shimizu S, Ito T, et al. Bcl-2 prevents caspase-independent cell death. J Biol Chem 1998;273:34272-7. [DOI] [PubMed] [Google Scholar]


