Abstract
Few interventions for Postnatal Depression (PND) have focused on parenting difficulties; the aim of this research was to investigate the feasibility and evaluate a parenting intervention (Baby Triple P) in women with PND. This was a pilot randomised controlled trial (RCT) to evaluate and determine the feasibility of the newly developed Baby Triple P compared with treatment as usual (TAU) in women with PND. In all, 27 female participants aged from 18 to 45 years (mean age = 28.4 years, standard deviation (SD) = 6.1), with a primary diagnosis of major depression and an infant under 12 months (mean age = 6.2 months, SD = 3.2 months), were recruited from primary care trusts in Greater Manchester, United Kingdom. Participants were randomly allocated to receive either eight Baby Triple P sessions in addition to TAU or TAU only. Outcomes were assessed at post-treatment (Time 2) and 3 months post-treatment (Time 3). Self-report outcomes were as follows: Beck Depression Inventory, Oxford Happiness Inventory, What Being the Parent of a New Baby is Like, Postpartum Bonding Questionnaire and the Brief Parenting Beliefs Scale–baby version. An assessor-rated observational measure of mother–infant interaction, the CARE Index and measure of intervention acceptability were also completed. Significant improvements from Time 1 to Time 2 and Time 1 to Time 3 were observed across both groups. Although women allocated to Baby Triple P showed more favourable improvements, the between-group differences were not significant. However, the intervention was highly acceptable to women with PND. A large-scale RCT is indicated.
Keywords: Mother–infant relationship, parenting, postnatal depression, feasibility, randomised controlled trial, baby, infant
Introduction
Postnatal depression (PND) affects approximately 10–15% of new mothers (Cooper & Murray, 1997). It is well documented that PND has an impact on maternal quality of life, and may increase vulnerability to subsequent episodes of depression. The infants of women with PND are at elevated risk of psychopathology (Goodman & Gotlib, 1999). The presence of psychosocial factors, including poverty, marital discord and life stressors (bereavement), also indicate increased risk of PND compared with biological or hormonal causes (Lee & Chung, 2007). However, antenatal depression and individual risk factors alone may not be sufficient to cause PND. The aetiology is likely influenced by a number of moderating risk variables, including demographic, economic, child age and timing of depression (Lovejoy, Graczyk, O’Hare, & Neuman, 2000). Biopsychosocial models of PND highlight multiple contributing factors at the biological, psychological and social levels (Milgrom, Martin & Negri, 1999). PND is similar to major depression occurring at other times in a woman’s life (Cooper, Campbell, Day, Kennerley, & Bond, 1988; O’Hara, 1994). However, the role of the primary caregiver (usually the mother) is central in promoting adaptive development in the infant and establishing positive foundations for continued social and emotional development and affect regulation (Tronick & Reck, 2009; Tronick & Weinberg, 1997). Therefore, the relationship between the mother and infant dyad and parenting behaviours are an important focus for interventions (O’Hara, 2009).
Considerable research has established the impact of parental psychopathology, particularly depression, on child development. PND may act as a risk factor for atypical socio-emotional and cognitive development in infants (Feldman et al., 2009; Hay, Pawlby, Angold, Harold, & Sharp, 2003; Kim-Cohen, Moffitt, Taylor, Pawlby, & Caspi, 2005; Stein, Malmberg, Sylva, Barnes, & Leach, 2008) as well as insecure attachment patterns (Martins & Gaffan, 2000). Cognitive deficits in infants have been significantly linked to the quality of the early mother–infant relationship, despite later remitting of maternal PND (Murray & Stein, 1991).
Problems may persist long after remission of maternal depressive symptoms. Indeed, longitudinal research has shown that children of women with depression remain vulnerable to parental psychopathology (Hay et al., 2003). Recent intergenerational research has also shown that the daughters of women with PND attain heightened scores on the Edinburgh Postnatal Depression Scale (EPDS; Cox, Holden, & Sagovsky, 1987) when they become parents themselves (Sejourne, Alba, Onorrus, Goutaudier & Chabrol, 2011).
The prevalence and pervasive impact of PND makes it a significant public health problem requiring early effective intervention. In two systematic reviews of interventions for PND, which assessed maternal mood and mother–infant outcomes and/or child developmental outcomes, it was noted that few studies had assessed child-related outcomes and there were discrepancies in maternal and child outcomes (Poobalan et al., 2007; Tsivos, Calam, Sanders, & Wittkowski, in press). This suggests that improvements in maternal mood do not necessarily translate into benefits to the mother–infant relationship and/or child development. In their review, Tsivos et al. (in press) also highlighted the unmet need for effective parenting interventions for women experiencing PND.
Poor parenting is a possible mechanism by which risk is transmitted from parent to child across the generational gap (Meaney, 2001). There is mounting evidence that women with PND may experience marked difficulties in practical care-giving tasks including breastfeeding (Dennis & McQueen, 2007; Field, 2010; Hart, Jackson, & Boylan, 2011; McLearn, Minkovitz, Strobino, Marks, & Hou, 2006a, 2006b), infant sleeping (Dennis & Ross, 2005; Field, 2010; Hatton, Harrison-Hohner, Dorato, Curen, & McCarron, 2005; Hiscock & Wake, 2001; McLearn et al., 2006a, 2006b), risky parenting behaviours (Zajicek-Farber, 2010), failing to attend well-child visits (Minkovitz et al., 2005; Zajicek-Farber, 2009), implementing household safety practices (McLearn et al., 2006a, 2006b; Zajicek-Farber, 2009) and difficulties bathing the infant (Righetti-Veltema, Conne-Perreard, Bousquet, & Manzano, 2002).
Further to the difficulties with parenting practices, PND is also associated with difficulties in responding to infants. Evidence exists for a positive association between prolonged infant crying and maternal depressive symptoms (Vik et al., 2009). Reck et al. (2011) reported that during interactions, infants and their depressed mothers were observed to display ‘less coordinations of positive matched states and took longer to move from mismatched states into positive matched states’ (p. 524).
There have also been notable differences in the interactive style between depressed dyads and non-depressed dyads. For example, mothers with PND have been observed to display more negative behaviours towards their babies, and their babies are less positive than babies of non-depressed mothers (Cohn, Campbell, Matias, & Hopkins, 1990; Tronick & Reck, 2009). Depressed mothers are also less likely to identify happy infant faces compared with their non-depressed peers (Arteche et al., 2011). An Australian comparative observational study of 48 ‘depressed’ and 40 ‘non-depressed’ mother–baby pairs found an association between poor maternal responsiveness and poorer developmental patterns (Milgrom, Westley, & Gemmill, 2004). Several studies have shown that cognitive outcomes in infants are related to the quality of the early mother–baby relationship, which were not reversed by later remittance of depression (Milgrom et al., 2004; Murray & Stein, 1991). Gerhardt (2004) outlined that responding inappropriately to a baby’s needs may lead to prolonged increase of cortisol, which may lead to neurodevelopmental changes and affect stress tolerance. Parenting practices, including communication and the formation of relationships between mother and infants, may, therefore, be an important target in protecting and promoting adaptive development (Craig, 2004; O’Hara, 2009).
The Triple P Positive Parenting Program is a system of interventions with impressive theoretical, scientific and clinical foundations (Sanders, 2012; Sanders, Markie-Dadds, & Turner, 2003; Turner & Sanders, 2006). Its aims include (1) enhancing parental knowledge and resourcefulness; (2) promoting nurturing, low-conflict environments for children; and (3) promoting children’s social, emotional and intellectual competencies through positive parenting practices (Sanders et al., 2003). The Triple P framework offers accessible, multi-level interventions increasing in intensity for parents with different needs, regardless of socio-cultural differences, age and gender (Sanders, Markie-Dadds, Tully, & Bor, 2000).
Early research which evaluated two types of behavioural family intervention (Triple P) in depressed mothers of children aged 3–9 years (M = 4.39 years) with behavioural difficulties demonstrated reductions in depressed mood and in frequency of difficult behaviour in their children (Sanders & McFarland, 2000).
Baby Triple P has been developed to enhance the knowledge, skills and confidence of new parents. The present is the first to examine the feasibility and acceptability of Baby Triple P compared with treatment as usual (TAU) in the treatment of women with PND. A secondary aim was to evaluate initial efficacy of Baby Triple P and explore whether it was sufficient to reduce the severity of depressive symptoms and improve the quality of the mother–infant relationship. In line with the above aims, it was hypothesised that compared with women receiving TAU only, women receiving Baby Triple P (in addition to TAU) would report (1) a significant reduction in depressed mood and improvements in positive mood, (2) that women in Baby Triple P would be observed to interact more sensitively with their infants compared with women receiving TAU only and (3) women receiving Baby Triple P would also report significant improvements in subjective bonding experience and increases in parental confidence. We hypothesised that these improvements would be sustained at 3-month follow-up.
As it has been suggested that parenting programmes function to improve self-regulatory skills (Sanders & Mazzucchelli, 2013), a further aim was to explore whether any reported improvements were associated with increases in self-regulation. Bandura (1991) theorised that dysfunctional self-regulation (i.e. parents’ belief in their ability to plan and execute goals successfully) was implicated in depressed mood. It was predicted that any improvements in the Baby Triple P arm would be associated with increases in parental self-regulation.
Method
Research design
This was a pilot randomised controlled trial (RCT) comparing the effectiveness of adding Baby Triple P to TAU in mothers with PND. This was a 2 (groups: intervention versus TAU) × 3 (assessment time points: pre- and post-treatment phase and 3-month follow-up) longitudinal design. Group assignment was by true block random allocation, stratified for severity of depression (i.e. low severity indicated by Beck Depression Inventory II (BDI-II) scores of ≤19 and high depression severity by BDI-II scores of ≥20). High and low severity were determined by BDI-II score categories in the BDI-II manual: scores from 0 to 13 indicate mild symptoms, 14 to 19 indicate mild, 20 to 28 indicate moderate and 29 to 63 indicate severe symptoms (Beck, Steer, & Brown, 1996). Average scores in similar studies (Milgrom, Negri, Gemmill, McNeil, & Martin, 2005; O’Hara, Stuart, Gorman, & Wenzel, 2000; Van Doesum, Riksen-Walraven, Hosman, & Hoefnagels, 2008) were also used to determine the cut-off point for severity.
Randomisation lists for low and high depression severity were computer generated by a statistician external to the research team. The process of randomisation was carried out using sealed opaque envelopes. Assignment to condition was concealed until group allocation (i.e. after baseline assessment). Eligibility screening, assessment and Baby Triple P sessions were conducted by the first author (Z.T.).
Measures
Clinical assessment measures
The Structured Clinical Interview for Diagnosing DSM-IV Disorders (SCID) was used to confirm a primary diagnosis of major depression. The SCID-PND is an adapted version of the SCID, which was developed for use with a PND population in a transcultural study (Gorman et al., 2004). A clinical diagnosis of depression was confirmed to ensure symptom severity was due to depression and not a general set of symptoms of psychological distress related to different psychopathology (Lovejoy, Graczyk, O’Hare, & Neuman, 2000).
The Family Background Questionnaire (FBQ; Sanders, Markie-Dadds, & Turner, 2001) is a self-report questionnaire used to collect demographic and psychosocial information (e.g. parent’s and infant’s age, onset of illness and duration). The FBQ is routinely used in Triple P research and clinical practice. It was modified for use with perinatal populations by accounting for factors associated with the perinatal context (e.g. antenatal complications, type of delivery, whether pregnancy was planned).
Outcome measures (all time-points)
Mood
The BDI-II (Beck et al., 1996) is a 21-item self-report measure of severity of depressive symptoms on a 4-point scale. Scores range from 0 to 63, with high scores indicating greater symptom severity. The BDI-II is valid for use in women experiencing PND and has been routinely used in perinatal research as a primary outcome measure (e.g. Boyd, Zayas, & McKee, 2006). It has high internal consistency (0.91) and test–retest reliability (0.93; Beck et al., 1996).
The Oxford Happiness Inventory (OHI; Argyle, Martin, & Crossland, 1989) is a 29-item self-report measure of broad personal happiness. It consists of a reversal of BDI-II items and eight additional items to cover aspects of subjective wellbeing not measured by the BDI-II. It has high internal consistency (0.92; Argyle et al., 1989).
Mother–infant relationship
The CARE Index (Crittenden, 2004) is a 3–5 minute, observer-rated video-taped interaction between mother–infant dyads. There are seven subscales, including maternal sensitivity, control, unresponsiveness and infant co-operation, compulsive/difficult responses or passivity. Scores range from 0 to 14, with high scores indicating greater sensitivity. It is suitable for infants up to the age of 15 months and is a robust indicator of current dyadic synchrony and future attachment behaviours (Crittenden, 2008). Rating of the CARE Index observations were conducted by an experienced qualified rater, external to the research team and double blind to depression diagnosis and treatment allocation.
The 25-item Postpartum Bonding Questionnaire (PBQ; Brockington et al., 2001) assesses maternal responses to her infant. It is scored on a 6-point scale (from 0 = always to 5 = never) where respondents indicate how true each statement is for them. High scores indicate greater psychopathology. It has good internal consistency (0.79; Wittkowski, Williams, & Wieck, 2010) and high test–retest reliability on total scale scores (0.95; Brockington et al., 2001).
Parenting competence, cognitions, attitudes and emotional responses
The What Being the Parent of a New Baby is Like (WPL; Pridham & Chang, 1989) is a 26-item self-report measure which assesses three major aspects of the parenting experience, including parenting evaluation, infant’s centrality in a parent’s thought and action and the life change the parent has experienced. The WPL contains 25 items scored on a 9-point scale and one open question prompting parents to describe what being a parent of a new baby is like for them. Internal consistency across the three subscales ranges from medium to high (0.77–0.90; Pridham & Chang, 1989).
The Brief Parenting Beliefs Scale–baby version (BPBS-b; Tsivos & Sanders, 2012) is a reliable 16-item self-report measure assessing self-regulation around parenting. Self-regulation is proposed to consist of four central concepts, including parental self-sufficiency, personal agency, parental self-efficacy and self-management. The BPBS-b was validated in a non-depressed sample of women and has good internal consistency (alpha = .80; Tsivos et al., in press).
Intervention arm specific measures
The Client Satisfaction Questionnaire (CSQ; Sanders et al., 2001) assesses the acceptability of the intervention. There are 13 items rated on a 7-point scale and three open-ended questions. Total scores range from 13 to 91 and higher scores represent higher acceptability.
Intervention protocol and therapist preparation
Baby Triple is a strengths-based intervention which aims to promote (1) healthy infant development, (2) reducing of family risk factors and (3) parental psychopathology. Baby Triple P consists of eight individual sessions delivered by a trained Triple P practitioner. The sessions include 1: positive parenting, 2: responding to your baby, 3: survival skills, 4: partner support, 5: implementing parenting routines (1), 6: implementing parenting routines (2), 7: implementing parenting routines (3), 8: implementing parenting routines (4) and maintenance and closure (see Table 1). The ‘implementing parenting routines’ sessions involve active skills practice between the mother–infant dyad. This involves implementing the Triple P strategies in vivo, during the session and in-between sessions through completion of homework tasks. The role of the practitioner is to provide feedback and prompt self-evaluation in the parent through identification of how the parent went with the strategy, asking them what they did well, what didn’t go well and what they might do differently in future. This same framework is used after every practice or parenting issue the parent undertakes, with the aim to promote an adaptive way of thinking about a parenting problem or issue.
Table 1.
Session content of Baby Positive Parenting Programme.
| Session title | Content | Baby Triple P strategies |
|---|---|---|
| Session 1: positive parenting | Introduces aims of the positive parenting programme as an approach to parenting | Spending time with baby |
| Communicating with baby | ||
| Overview of factors that impact baby development and strategies for promoting development and relationship with baby | Showing affection | |
| Set goals for relationship with baby and family | ||
| Session 2: responding to your baby | Introduces strategies for responding to baby and teaching new behaviours and skills through praise, attention, providing interesting activities and routines | Praise |
| Attention | ||
| Providing interesting activities | ||
| Covers why babies sleep and cry and strategies for managing infant distress and sleeping difficulties as well as strategies for promoting adaptive sleeping routines | Encouraging contentment | |
| Settling techniques | ||
| Diversion | ||
| Establishing limits | ||
| Session 3: survival skills | Common experiences of new parents when having a baby (i.e. parenting traps – unhelpful ways of thinking about parenting which make parenting more difficult and may lead to negative emotions)Covers what unpleasant emotions (i.e. anger, sadness, depression and anxiety) are and explores how they work and how they affect parentingSocialisation to ABC modelIdentification of negative automatic thoughtsCoping strategies are covered (i.e. catching unhelpful thoughts, abdominal breathing, positive self-talk, social support, developing personal coping plans) | Coping statements |
| Relaxation and stress management abdominal breathingFinding out what you need to knowSupportCoping plans for high-risk situationsCatching/challenging unhelpful thoughts | ||
| Session 4: partner support | Covers common experiences of couples during the transition to parenthood (i.e. partner traps – unhelpful ways of thinking about the partner relationship which lead to difficulties in the partner relationship)Also covers the importance of communication skills, maintaining relationship happiness, negotiating household and baby care tasks | Improving communicationGiving and receiving constructive feedbackHaving casual conversationsSupporting each other when problem behaviour occursProblem solvingImproving relationship happiness |
| Session 5–7: implementing parenting routines 1 | These sessions employ the use of the self-evaluation framework. The practitioner prompts self-evaluation in the parent to promote parental self-regulationThe practitioner aims to give little prompting to promote self-regulation. | As above |
| Session 8: implementing parenting routines 4 and maintenance and closure | Final implementing parenting routines session (as above)Client progress is reviewed and goals for future set | As above |
| Covers phasing out the programme and identifying obstacles (high-risk times) and strategies for maintaining change |
All sessions were delivered by a doctoral student who was a Triple P–accredited practitioner. Baby Triple P sessions took place in participants’ home on a weekly basis. The first four sessions lasted between 1 and 1.5 hours, and the remaining four sessions lasted between 40 minutes and 1 hour. A workbook (Spry, Morawska, & Sanders, 2009) detailing the session content was provided for the participant and a manual and session checklist were used by the practitioner during each session. The practitioner received weekly supervision from a clinical psychologist, who was also trained and accredited in Baby and Standard Triple P.
Participants
Participants were eligible for inclusion if they met risk indicators for PND (i.e. scores of ≥ 10; Lee & Chung, 2007) on the EPDS (Cox et al., 1987) and a primary diagnosis of PND, based on confirmation of major depression on the SCID. Participants were excluded if they screened positive for psychotic symptoms or another mental health condition, which preceded the onset of their depressive episode. In addition, their infants had to be less than 12 months of age. They also had to live within the geographical recruitment area (Greater Manchester, UK) and read and write English (for the purposes of using the written workbook during intervention). Table 2 shows the major participant demographic and perinatal characteristics at baseline.
Table 2.
Socio demographics and characteristics of mothers and their infants in Baby Triple P and TAU at baseline (Time 1).
| TAU (n =13) | Baby Triple P (n = 14) | χ2 | t(df) | p | Total (n = 27) | |
|---|---|---|---|---|---|---|
| Maternal characteristics | ||||||
| Mean age (years) (SD) | 26.7 (SD = 6.2) | 30.7 (SD = 5.8) | −1.5 (25) | .16 | 28.4 (SD = 6.1) | |
| Partner mean age (years) (SD) | 28.15 (SD = 6.5) | 34 (SD = 5.0) | −2.6 (25) | .02a | 31.2 (SD = 6.4) | |
| Depression (BDI-II) | 32 (SD = 9.6) | 32.8 (SD = 9.7) | −0.21 (25) | .83 | 32.4 (SD = 9.5) | |
| EPDS | 19 (SD = 5.2) | 19.2 (SD = 4.8) | −0.11 (25) | .91 | 19.1 (SD = 4.9) | |
| History of depression (%) | 0.00 | 1.00 | ||||
| Yes | 53.8% (n = 7) | 57.1 (n = 8) | 56% (n = 15) | |||
| On antidepressant medication (%) | 0.32 | .57 | ||||
| Yes | 69.2% (n = 9) | 85% (n = 12) | 77.8% (n = 21) | |||
| Relationship status (%) | 0.47 | .79 | ||||
| Married | 53% (n = 7) | 42.9% (n = 6) | 48.1% (n = 13) | |||
| Living together | 38.5% (n = 5) | 42.9% (n = 6) | 40.7% (n = 11) | |||
| Separated/divorced | 7.7% (n = 1) | 14.3% (n = 2) | 11.1% (n = 3) | |||
| Ethnicity (%) | 8.3 | .14 | ||||
| British | 53.8% (n = 7) | 100% (n = 14) | 77% (n = 21) | |||
| Other White background | 7.7% (n = 1) | 3.7% (n = 1) | ||||
| Other Black background | 7.7% (n = 1) | 3.7% (n = 1) | ||||
| Other Mixed background | 7.7% (n = 1) | 3.7% (n = 1) | ||||
| Bangladeshi | 7.7% (n = 1) | 3.7% (n= 1) | ||||
| Other ethnic background | 15% (n = 2) | 7.4% (n = 2) | ||||
| Education level (%) | 2.4 | .79 | ||||
| No qualifications | 7.7% (n = 1) | 3.7% (n = 1) | ||||
| GCSEs, CSEs or O-levels | 15.4% (n = 2) | 21.4% (n = 3) | 18.5% (n = 5) | |||
| A levels/BTEC | 23.1% (n = 3) | 14.3% (n = 2) | 18.5% (n = 5) | |||
| Trade/apprenticeship | 7.7% (n = 1) | 7.1% (n = 1) | 7.4% (n = 2) | |||
| University Degree | 46.2% (n = 6) | 50% (n = 7) | 48.1 % (n = 13) | |||
| Family income (%) | 2.6 | .3 | ||||
| Low | 38.5 (n = 5) | 14.3% (n = 2) | 35.9% (n = 7) | |||
| Middle | 30.8 (n = 4) | 57.1 (n = 8) | 44.4% (n = 12) | |||
| High | 30.8 (n = 4) | 28.6% (n = 4) | 29.6% (n = 8) | |||
| Maternal employment (%) | 3.4 | .49 | ||||
| Full time | 7.1% (n = 1) | 3.7% (n = 1) | ||||
| Part time | 7.7 % (n = 1) | 14.3% (n = 2) | 11.1% (n = 3) | |||
| Home duties | 30.8% (n = 4) | 7.1% (n = 1) | 18.5% (n = 5) | |||
| On maternity leave | 46.2% (n = 6) | 50% (n = 7) | 48.1% (n = 13) | |||
| Unemployed | 15.4% (n = 2) | 21.4% (n = 3) | 18.5% (n = 5) | |||
| Infant characteristics | −0.81 (25) | .43 | ||||
| Mean age (months) at baseline | 5.7 (SD = 3.1) | 6.7 (SD = 3.4) | 6.2 (SD = 3.2) | |||
| Female (%) | 46.2% (n = 6) | 64.3% (n = 9) | .31 | .58 | 56 % (n = 15) | |
| Primiparous (%) | 76.9% (n = 10) | 71.4% (n = 10) | .00 | 1.0 | 74.1% (n = 20) | |
| Pregnancy characteristics (%) | 0.52 | .92 | ||||
| Delivery (%) | ||||||
| Vaginal | 61.5% (n = 8) | 71.4% (n = 10) | 67% (n = 18) | |||
| Assisted delivery (forceps) | 15.4% (n = 2) | 7.1% (n = 1) | 11.1% (n = 3) | |||
| Emergency caesarean | 15.4% (n = 1) | 14.3% (n = 2) | 15% (n = 4) | |||
| Planned caesarean | 7.7% (n = 1) | 7.1% (n = 1) | 7.4% (n = 2) | |||
| Perinatal complications (%) | 0.94 | .33 | ||||
| Yes | 38.5% (n = 5) | 57.1 (n = 8) | 48.1% (n = 13) | |||
| Planned pregnancy (%) | 0.00 | 1.0 | ||||
| Yes | 69.2% (n = 9) | 64.3% (n = 9) | 66.7% (n = 18) | |||
TAU: treatment as usual; EPDS: Edinburgh Postnatal Depression Scale; GCSE: General Certificate of Secondary Education; CSE: Certificate of Secondary Education; BDS: Beck Depression Inventory; SD: standard deviation; M: mean; BTEC: Business and Technology Education Council.
Fisher’s exact probability test.
Sampling procedures
Participants were from a convenience sample (i.e. referred by health visitors, general practitioners (GPs), midwives and self-referral through social media). The study team was only notified of individuals who opted-in to the study. As such, there is no information on the number of individuals approached but declining to take part in the research. Screening was done over the phone or directly with the participants. All baseline, post-treatment and 3-month follow-up assessments were done in the participants’ home or a place of their choice. No monetary incentive for taking part was offered; however, travel was reimbursed. Participants randomised to TAU received a copy of the Triple P: Every Parents Self-Help Workbook (Markie-Dadds, Sanders, & Turner, 1999) on completion of the study at the follow-up. The research was reviewed and approved by a National Health Service (NHS) research ethics committee (North West 6, ref: 10/H1003/73).
Sample size and power
The intended sample size was N = 60, as identified by a power analysis of previous studies in the psychological treatment of depression and PND, which used the BDI-II as an outcome measure. With 30 subjects in each group, the study would have 80% power to detect differences of 5.1 or more between the groups (with a simple t-test, estimated standard deviation (SD) of 7 and using the conventional 5% significance level).
Planned analyses
In order to test the hypotheses that Baby Triple P was associated with favourable outcomes compared with TAU, analysis of covariance (ANCOVA) was performed on each variable (BDI-II, OHI, BPBS-b, PBQ, etc.) from baseline to post-treatment (controlling for baseline scores of the given measure) and from baseline to 3-month follow-up. When data did not meet assumptions of parametric testing, changes from baseline to post-treatment and changes from baseline to 3-month follow-up were calculated for each group separately and then compared using Mann–Whitney U analysis (to compare changes between Baby Triple P and TAU, respectively).
Results
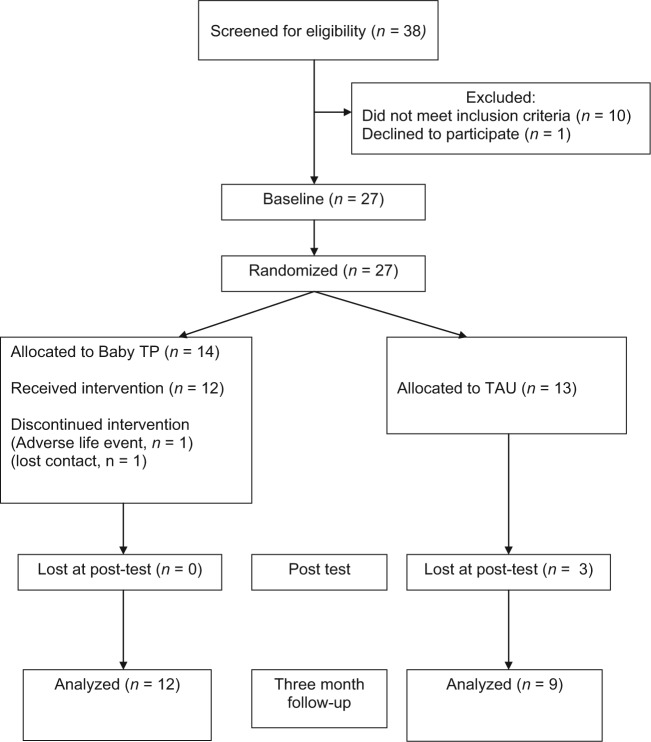
In all, 27 women met inclusion criteria for the present study and completed baseline assessments and were subsequently randomised to condition (see Figure 1 for CONSORT diagram detailing flow of participants through the study). Participants were recruited on a rolling basis between December 2010 and May 2012. A total of 13 women were randomised to Baby Triple P + TAU and 14 to TAU only. Two women dropped out of Baby Triple P after sessions 2 and 3, respectively. They could not be contacted, and therefore, were not assessed at post-treatment and 3-month follow-up. Of the drop-outs from the Baby Triple P condition, one participant reported an adverse life event and the other lost contact. Treatment completers received all sessions detailed in the treatment protocol. Three participants from the TAU group dropped out before post-treatment assessment and contact was lost with one further participant before the 3-month follow-up assessment. With respect to the TAU drop-outs, one participant moved and the other three could not be contacted. At post-treatment, data were analysed from Baby Triple P (n = 12) and TAU (n = 10). Following the 3-month follow-up, data were analysed from Baby Triple P (n = 12) and TAU (n = 9). Participant characteristics and demographics are presented in Table 2.
Figure 1.
CONSORT diagram detailing participant involvement through study progress.
TAU: treatment as usual; TP: triple P.
TAU
Of the 27 women in this study, a total of 21 women (TAU = 9; Baby Triple P + TAU = 12) were receiving antidepressant medication (i.e. sertraline, fluoxetine, citalopram). Four women (TAU = 2; Baby Triple P = 2) were receiving additional psychological support focusing on depression (Cognitive Behaviour Therapy (CBT), counselling) in addition. A total of 11 participants (TAU = 5; Baby Triple P = 6) had been referred by a specialist health visitor following the completion of a 6-session postnatal support group. The content of the support group sessions were unstructured and flexible. General session topics included, establishing group rules and ice breaking; psycho-education around medication, stress, anxiety, depression and cross-sectional formulations; relaxation and coping and meeting own needs; debriefing on birth and hospital experience, postnatal period, physical recovery, breastfeeding, experience of PND, support, role of partners and parenting challenges; self-care, food, diet, sleep and alternative therapies and discussion of goals and summary of previous sessions.
Baby Triple P acceptability ratings
Baby Triple P was rated as highly acceptable. Table 3 shows means and SDs for each of the 13 items on the CSQ. Scores ranged from 1 (least satisfied) to 7 (most satisfied). The mean total score was 85.83 (SD = 4.47), from a maximum score of 91.
Table 3.
Client satisfaction ratings for women allocated to Baby Triple P.
| Item | Client satisfaction questionnaire (n = 10) |
|
|---|---|---|
| M | SD | |
| Quality of service | 6.75 | 0.62 |
| Baby Triple P provided the help sought | 6.67 | 0.65 |
| Baby Triple P met child’s needs | 6.83 | 0.39 |
| Baby Triple P met parental needs | 6.83 | 0.39 |
| Satisfied with amount of help | 7.00 | 0.00 |
| Programme has helped with child behaviour | 6.75 | 0.62 |
| Programme has helped deal with family problems | 6.58 | 0.52 |
| Programme has helped with partner relationship | 5.64 | 1.86 |
| Overall satisfaction with programme | 7.00 | 0.00 |
| Would do Triple P again if needed | 6.92 | 0.29 |
| Programme skills can be applied to other family members | 6.42 | 0.79 |
| Child’s development at this point | 6.25 | 0.62 |
| Satisfaction with child progress | 6.67 | 0.49 |
M: mean; SD: standard deviation.
Statistical analysis
Preliminary investigation of the data indicated skewness and kurtosis on some outcome measures. Log (ln) transformations were performed on data, which violated the assumptions of non-parametric testing. Where data could not be transformed successfully, non-parametric tests (Mann–Whitney U) were used to compare group differences on change scores. Preliminary analysis of baseline characteristics revealed no differences on any variables except for age of partner: therefore, only baseline scores were entered as covariates for ANCOVA analyses due to the small sample size.
Individual missing data points on self-report items were calculated by averaging available responses and multiplying by the number of items in the questionnaire. Analyses followed intention-to-treat (ITT) protocol and included all participants as randomised. It was only possible to include participants who had been assessed at least at two time-points. Complete data from baseline to post-treatment were available for 22 participants (TAU = 10, Baby Triple P = 12). Complete datasets from baseline to follow-up were available for 21 participants (TAU = 9, Baby Triple P = 12). It was not possible to perform multiple imputations on the data given the small sample size. Sensitivity analyses were carried out using the Last Observation Carried Forward (LOCF) method for handling missing data.
Maternal mood
There were no significant differences between conditions on depressed mood (BDI scores) at post-treatment (Baby Triple P: M = 9.39, confidence interval (CI) = 5.5–16.1; TAU: M = 11.23, CI = 6.3–20.3), F(1, 19) = 1.9, p = 0.18, partial eta square = 0.09, or from baseline to follow-up, F(1, 18) = .25, p = .65, partial eta square = 0.12, between the groups (Baby Triple P, M = 9.49, CI = 5.2–17.5; TAU, M = 7.77, CI = 3.9–15.5) (see Table 4).
Table 4.
Adjusted means and confidence intervals for all outcome measures at all time points.
| Measure and condition | Baselinea |
Post-test |
3 month follow-up |
Baseline to post-test |
Baseline to 3-month follow-up |
||
|---|---|---|---|---|---|---|---|
| M (SD) | M (CI) | M (CI) | F(df) | p | F(df) | p | |
| BDI-IIb | |||||||
| Baby TP | 31.50c | 9.39 (5.5–16.1) | 9.49 (5.2–17.5) | 1.9 (1) | 0.18 | 0.25 (1) | .65 |
| TAU | 30.56c | 11.23 (6.3–20.3) | 7.77 (3.9–15.5) | ||||
| OHI | |||||||
| Baby TP | 68.23 (15.23) | 117.80 (101.75–133.85) | 118.30 (101.11–135.57) | 2.89 (1) | 0.11 | 1.5 (1) | .23 |
| TAU | 83.99 (19.97) | 98.20 (80.57–115.83) | 102.70 (82.70–122.62) | ||||
| WPL | |||||||
| Baby TP | 155.52 (30.63) | 171.73 (160.97–182.02) | 176.30 (165.76–186.87) | 0.28 (1) | 0.60 | 0.22 (1) | .65 |
| TAU | 175.15 (20.55) | 175.00 (165.63–184.77) | 172.70 (160.42–184.92) | ||||
| PBS-b | |||||||
| Baby TP | 54.71 (9.63) | 65.09 (61.04–69.15) | 62.32 (57.65–66.99) | 1.19 (1) | 0.29 | 0.16 (1) | .69 |
| TAU | 56.25 (10.82) | 61.88 (57.20–66.56) | 60.90 (55.18–66.62) | ||||
| PBQd | U(z) | p | U(z) | p | |||
| Baby TP | 20.62 (8.65–75.96) | 9.5 (0–67.0) | 7.0 (0–48.0) | 54.0 (−0.40) | 0.69 | 40.0 (−1) | .32 |
| TAU | 18.9 (1.92–56.73) | 9.75 (1.0–38.0) | 16.0 (0-31.0) | ||||
SD: standard deviation; BDI-II: Beck Depression Inventory-II; OHI: Oxford Happiness Inventory; PBQ-b: Postpartum Bonding Questionnaire–baby version; WPL: What Being the Parent of a Baby is Like; PBS: Parenting Beliefs Scale; TP: triple P; TAU: treatment as usual.
p-value from Mann–Whitney test.
Raw data mean (SD).
Adjusted geometric mean (95% confidence intervals).
Geometric mean (range).
Median (range).
There was a significant effect of time across both groups on happiness (OHI scores) from baseline to post-treatment, F(1, 19) = 8.19, p = .01, and from baseline to 3-month follow-up, F(1, 18) = 5.89, p = .03. There were no significant group differences when controlling for happiness (OHI) scores at baseline from baseline to post-treatment, F(1, 19) = 2.89, p = .11, partial eta square = 0.13, and from baseline to 3-month follow-up, F(1, 18) = 1.5, p = .23, partial eta square = 0.08. There was a non-significant trend with respect to happiness scores in the predicted direction at post post-treatment (Baby Triple P: M = 117.80, CI = 101.75–133.85; TAU: M = 98.20, CI = 80.57–115.83) and at follow-up (Baby Triple P, M = 118.30, CI = 101.11–135.57; TAU, M = 102.70, CI = 82.70–122.62).
Self-regulation
There was a significant effect of time across both groups on self-regulation (BPBS-b) scores from baseline to post-treatment, F(1, 18) = 6.88, p = .02. Women allocated to Baby Triple P group (M = 65.09, CI = 61.04–69.15) obtained non-significant, F(1, 18) = 1.19, p = .29, favourable scores at post-treatment compared with women allocated to TAU (M = 61.88, CI = 57.20–66.56). The same pattern was observed for self-regulation scores from baseline to 3-month follow-up, F(1, 17) = 5.32, p = .03. Women receiving Baby Triple P (M = 62.32, CI = 57.65–66.99) obtained non-significant, F(1, 17) = 0.16, p = .69, higher self-regulation scores compared with those receiving TAU (M = 60.90, CI = 55.18–66.62).
Parenting attitudes
With regard to experience of parenthood (WPL), there was a significant effect of time, F(1, 19) = 14.13, p = .001. However, no significant group differences were found (when controlling for baseline WPL scores) from baseline to post-treatment, F(1, 19) = 0.28, p = .60, partial eta square = 0.02 (Baby Triple P: M = 171.73, CI = 160.97–182.02; TAU: M = 175.00, CI = 165.63–184.77). A significant effect of time was observed across both groups on experience of parenthood from baseline to 3-month follow-up, F(1, 18) = 6.45, p = .02. However, the groups did not differ significantly (when controlling for baseline WPL scores) from baseline to follow-up, F(1, 18) = 0.22, p = .65, partial eta square = 0.01 (Baby Triple P: M = 176.30, CI = 165.76–182.87; TAU: M = 172.72, CI = 160.42–184.92).
Subjective bonding
Since subjective bonding (PBQ) scores could not be transformed successfully, change scores were calculated from baseline to post-treatment and again from baseline to 3-month follow-up; groups were then compared using Mann–Whitney U. There were non-significant, U = 54.0, z = −0.40, p = .69, improvements to subjective bonding scores from baseline to post-treatment for women receiving Baby Triple P (median = 9.5, range = 0–67.0) compared with those receiving TAU (median = 9.75, range = 1.0–38.0). A similar non-significant, U = 48.0, p = .67, z = −0.42, pattern of change was observed from baseline to 3-month follow-up, Baby Triple P (median = 7.0, range = 0–48.0) reported greater improvements compared with women allocated to TAU (median = 16.0, range = 0–31.0); however, the difference was not statistically significant, U = 40.0, z = −1.00, p = .32.
Dyad relationship
With respect to maternal sensitivity, although it increased from baseline to post-treatment in women receiving Baby Triple P compared with those receiving TAU, group differences were not significant, U = 51.5, p = .57, z = −0.57 (see Table 5). Changes in maternal controlling behaviour decreased for women receiving Baby Triple P, and increased for the TAU group from baseline to post-treatment. However, these differences did not reach significance, U = 39, p = .16, z = −1.39. Again, changes in maternal unresponsiveness were not significant between the two groups from baseline to post-treatment, U =39.5, p = .17, z = −1.36. The infants across both groups were observed to be more cooperative from baseline to post-treatment; however, these differences were non-significant, U = 51.5, p = .57, z = −0.56. All infants were observed to display more difficult behaviour from baseline to post-treatment, but this change in difficult behaviour was non-significant, U = 53, p = .64, z = −0.47. Infant compulsivity also did not appear to non-significantly increase for infants of mothers receiving Baby Triple P compared with infants of TAU mothers from baseline to post-treatment, U = 53, p = .64, z = −0.47. Non-significant decreases in infant passivity were also observed across both groups, U = 50, p = .51, z = −0.67.
Table 5.
Medians and ranges for care index variables for Baby Triple P group and TAU at baseline (Time 1), post-treatment (Time 2) and 3-month follow-up (Time 3).
| Care index variable |
Baby TP, median (range) |
TAU, median (range) |
Baby TP, median (range) |
TAU, median (range) |
Baby TP, median (range) |
TAU, median (range) |
Baseline to post-treatment |
Baseline to follow-up |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Post-treatment | Follow-up |
delta |
U | z | p |
delta |
U | z | p | ||||||
| Baby Triple P | TAU | Baby Triple P | TAU | |||||||||||||
| Mother | ||||||||||||||||
| Sensitive | 4.0 (2–11) | 5.0 (2–12) | 4.5 (1–9) | 6.0 (2–12) | 5.0 (2–8) | 6.0 (2–11) | 0.5 (−4.0 to 4.0) | .5 (−6.0 to 5.0) | 51.5 | −0.57 | 0.57 | 1.0 (−5.0–4.0) | −1.0 (−5.0–6.0) | 43.5 | −0.75 | 0.45 |
| Controlling | 6.0 (1–9) | 5.0 (1–12) | 5.0 (3–13) | 7.0 (1–10) | 6.0 (2–11) | 7.0 (1–12) | −0.5 (−4.0 to 5.0) | 2.0 (−2.0 to 7.0) | 39.0 | −1.39 | 0.16 | 1.5 (−4 to 6.0) | 4.0 (−2.0 to 6.0) | 43.0 | −0.79 | 0.43 |
| Unresponsiveness | 2.0 (0–11) | 3.0 (0–10) | 2.0 (0–8) | 0.5 (0–2) | 2.0 (0–5) | 2.0 (0–4) | −0.5 (−6.0 to 4.0) | −2.5 (−9.0 to 2.0) | 39.5 | −1.36 | 0.17 | −1.0 (−8.0 to 3) | −3.0 (−7.0 to 2) | 43.0 | −0.79 | 0.43 |
| Infant | ||||||||||||||||
| Cooperativeness | 4.5 (1–10) | 4.0 (0–12) | 5.0 (1–9) | 7.0 (1–12) | 5.0 (2–9) | 7.0 (3–12) | 0.5 (−3.0 to 4.0) | 1.0 (−5.0 to 6.0) | 51.5 | −.56 | 0.57 | 0.5 (−5.0 to 5.0) | −1.0 (−6.0 to 7.0) | 48.0 | −0.42 | 0.67 |
| Difficult behaviour | 2.0 (0–7) | 2.0 (0–7) | 3.5 (0–12) | 4.0 (0–13) | 3.5 (0–11) | 3.0 (0–8) | 0.5 (−10.0 to 12) | 0.0 (−5.0 to 7.0) | 53.0 | −.47 | 0.64 | 1.0 (−9.0 to 11.0) | 0.0 (−9.0 to 5.0) | 52.0 | −0.14 | 0.89 |
| Compulsivity | 1.0 (0–10) | 1.0 (0–12) | 1.5 (0–12) | 0.0 (0–9) | 3.0 (0–7) | 4.0 (1–7) | 0 (−6.0 to 12.0) | 1.5 (−2.0 to 8) | 53.0 | −.47 | 0.64 | 1.5 (−6.0 to 5.0) | 3.0 (−3.0 to 5.0) | 41.0 | −0.93 | 0.35 |
| Passivity | 1.0 (0–11) | 1.0 (0–9) | 0.5 (0–5) | 0.5 (0–5) | 0 (0–5) | 0.0 (0–3) | −1.0 (−11.0 to 4.0) | −1.0 (−7.0 to 2.0) | 50.0 | −.67 | 0.51 | 0.0 (−11.0 to 2.0) | −1.0 (−8.0 to 0.0) | 41.0 | −0.94 | 0.35 |
TAU: treatment as usual.
Maternal sensitivity increased although the change from baseline to 3-month follow-up was not statistically significant, U = 43.5, p = .45, z = −0.75. Changes in maternal controlling did not reach significance, U = 43, p = .43, z = −0.79. Again, changes in maternal unresponsiveness were not significant between the two groups from baseline to post-test, U = 43, p = .43, z = −0.79. This non-significant pattern was the same for change in infant difficult behaviour, U = 52.0, p = .89, z = −0.14, and infant compulsivity, U = 41.0, p = .35, z = −0.93. A non-significant decrease in infant passivity was found in both groups, U = 41.0, p = .35, z = −0.94.
Reliable change index
At post-treatment, women allocated to the Baby Triple P group had lower BDI-II scores. Although the ANCOVA analysis indicated that the difference between the groups was not significant, there was a significant effect of time. Therefore, individual scores were assessed using Jacobson and Truax’s (1991) reliable change index (RCI). From baseline to post-treatment, 75% of women in Baby Triple P had a clinically significant improvement to depressed mood compared with 70% of women allocated to TAU. From baseline to 3-month follow-up, 75% of women in Baby Triple P had clinically significant improvements compared with 80% of the TAU group (see Table 6).
Table 6.
Individual BDI-II scores and RCI value.
| Participant | BDI-II scores |
Statistically and clinically significant change (RCI)a |
||||
|---|---|---|---|---|---|---|
| Baseline | Post-intervention | 3-month follow-up | Baseline to post-intervention | Baseline to 3-month follow-up | ||
| Baby TP | 1 | 18 | 16 | 13 | No (0.52) | No (1.31) |
| 2 | 30 | 30 | 23 | No (0) | No (1.84) | |
| 3 | 22 | 2 | 8 | Yes (5.24) | Yes (3.67) | |
| 4 | 29 | 3 | 2 | Yes (6.82) | Yes (7.08) | |
| 5 | 45 | 13 | 16 | Yes (8.39) | Yes (7.60) | |
| 6 | 40 | 13 | 17 | Yes (7.08) | Yes (6.03) | |
| 7 | 37 | 39 | 39 | No (−0.52) | No (−0.52) | |
| 8 | 33 | 13 | 20 | Yes (5.24) | Yes (3.41) | |
| 9 | 29 | 10 | 8 | Yes (4.98) | Yes (5.51) | |
| 10 | 30 | 2 | 4 | Yes (7.34) | Yes (6.82) | |
| 11 | 24 | 13 | 4 | Yes (2.88) | Yes (5.24) | |
| 12 | 26 | 7 | 4 | Yes (4.98) | Yes (5.77) | |
| TAU | 13 | 14 | 13 | 5 | No (0.26) | Yes (2.36) |
| 14 | 36 | 11 | 1 | Yes (6.55) | Yes (9.18) | |
| 15 | 28 | 26 | – | No (0.52) | – | |
| 16 | 26 | 5 | 4 | Yes (5.51) | Yes (5.77) | |
| 17 | 48 | 29 | 36 | Yes (4.98) | Yes (3.15) | |
| 18 | 45 | 38 | 42 | No (1.84) | No (0.79) | |
| 19 | 21 | 5 | 13 | Yes (4.91) | Yes (2.10) | |
| 20 | 23 | 10 | 7 | Yes (3.41) | Yes (4.19) | |
| 21 | 36 | 3 | 3 | Yes (8.65) | Yes (8.65) | |
| 22 | 36 | 11 | 13 | Yes (6.55) | Yes (6.03) | |
RCI: Reliable Change Index; BDI-II: Beck Depression Inventory-II.
RCI is clinically significant when RCI > 1.96.
Discussion
Acceptability and feasibility
The primary aim of this study was to investigate the acceptability and feasibility of the newly developed Baby Positive Parenting Programme (Baby Triple P) compared with TAU in women with PND. High scores on the CSQ suggest that Baby Triple P was highly acceptable to women with PND. Although the sample size was modest (N = 27), the drop out was low (N = 2/14), which supports the notion that the intervention was acceptable. The present study may offer important information relating to the methodological decisions of future (large-scale) trials. Lancaster, Dodd and Williamson (2004) have highlighted that pilot studies can lead to higher quality RCTs. The feasibility of the current study is outlined in relation to their framework.
The study protocols have been developed and may require further refinement. These include an intake interview schedule designed to assess initial eligibility criteria and provide further information about randomisation and Baby Triple P session content. Future studies may consider including a session to debrief about the birth experience to promote engagement. Additionally, the research was conducted in participants’ home, with an aim to increase participation, reduce drop-out and facilitate attendance at sessions. Clinical observations suggest that, having the baby present during sessions was generally not obstructive and promoted practising of skills in situ, although there was no formal measure of this.
In relation to data collection, it took approximately 30–45 minutes to complete all questionnaires. Some participants reported that this was too long. In future, assessment batteries could be conveniently completed by participants online. This approach could reduce response biases, although it may result in reduced response rates.
With respect to outcome measures, all measures in the present study were validated, reliable measures. The primary outcome measure (the BDI-II) is a very robust indicator of depression severity. The inclusion of the BDI-II in future studies would allow comparisons between studies with respect to changes in depression symptoms. Responses on the CSQ indicated that Baby Triple P had a positive effect on the marital relationship. Although the marital relationship and paternal wellbeing were not formally assessed, future studies could include indexes of marital adjustment and paternal wellbeing since these may be affected by PND. The variables could be potential mediators in recovery from PND and infant wellbeing. Future studies should also collect detailed information on participants’ psychiatric histories (including chronicity and severity of symptoms), their socio-economic status, age of infant, factors around their pregnancy and the nature of the experience since these variables may play an important part in their engagement as well as their recovery.
There are further considerations for recruitment. Women with PND have historically been a very difficult population to recruit successfully to research trials (Appleby & Whitton, 1993). Literature on help-seeking behaviour has highlighted several factors, which influence disclosure of their experiences and help-seeking support (Dennis & Chung-Lee, 2006; Shakespeare, Blake, & Garcia, 2006).
The recruitment strategy of the present study involved contacting all GPs, community pharmacists, health visitors, community midwives, charitable organisations in the local area and public advertising. Following contact, individual visits were made to teams to present what the research involved, what the potential benefits to clients might be and how it might help support the service. Brief information leaflets were provided to all teams. Social media was also used to promote the research. Despite high prevalence rates in the geographical area, referral rates were by comparison extremely low. The teams that did refer clients had a great deal of interest in parenting and reported a need for continued support of their clients.
Given the difficulties with recruitment, there are important implications concerning this process. For example, in the present study, the researcher was only able to make contact with participants once they had agreed. It is likely that future studies could maximise their recruitment figures by employing a research nurse or health visitor who has detailed knowledge of the study integrated within services to recruit women. It should also be noted for future research that those who self-referred (i.e. via public advertisement), had fewer difficulties and less severe symptoms compared with those referred via a primary healthcare professional.
Experimental hypotheses
The experimental hypothesis that Baby Triple P would be associated with greater decreases in depressed maternal mood compared with TAU was not supported. The hypothesis that women receiving Baby Triple P would be observed to be more sensitive in their interaction with their infants was also not supported, as demonstrated by the non-significant findings across the sensitivity scale and all other CARE-Index subscales. There were no significant group differences on any of the other secondary outcome measures, including happiness, subjective bonding, the parenting experience and self-regulation.
Our additional experimental hypothesis that any significant changes would be maintained at 3-month follow-up was also not supported. However, Baby Triple P was rated highly acceptable by the women receiving it. This finding is comparable to CSQ scores obtained in other Triple P trials (i.e. Hoath & Sanders, 2002).
Women receiving Baby Triple P had non-significantly greater improvements in their self-regulation scores compared with TAU. Although non-significant, it provides some support for the theorised relationship between depression and dysfunctional self-regulation posed by Bandura (1991). Indeed, the effect of time on self-regulation was significant across both groups, with, self-regulation increasing for both groups. This finding may be related to decreases in depression, or that women became more confident in their parenting skills over time. This lends some support for self-regulation as a possible mechanism of change. Improvements following Triple P treatment and long-term maintenance of effects are thought to be associated with increased parental self-regulation (Sanders, Mazzucchelli & Ralph, 2012b). Specifically, increases in self-regulation are thought to arise through parents modifying their parenting behaviours. Adaptive self-regulation is thought to involve operationalising of four concepts (Sanders et al., 2001, p. 6), including (1) self-sufficiency: having resilience, resourcefulness, knowledge and skills to parent with confidence; (2) parental self-efficacy: the belief that one can overcome and deal with problem behaviours; (3) self-management: tools and skills that parents can use to become more self-sufficient, including self-monitoring, self-determination of goals and performance standards, self-evaluation of their own performance against performance criterion and self-selection of change strategies; and (4) personal agency: attribution of changes or improvements in their child’s behaviour or their own rather than to chance, age, maturational factors or other uncontrollable events. It is hypothesised that parents generalise skills and knowledge acquired in the programme beyond context of the intervention itself. Furthermore, this generalisation of skills and knowledge is associated with long-term maintenance of intervention effects.
The pattern of findings reported is best explained by insufficient power to detect differences between the groups. While speculative, we acknowledge further explanations for the non-significant findings. First, the present sample was more severely depressed compared with previous studies (Milgrom et al., 2005; O’Hara et al., 2000; Van Doesum et al., 2008). The increased severity of depressive symptoms experienced by women in the present study may have elicited a greater degree of support, including more careful monitoring by health visitors and stronger medication prescription by GPs. Additionally, the health visitors who made referrals to this study represent a minority of individuals especially interested in PND and the research. The level of motivation of these health visitors may have had an added impact on recovery rates in the TAU group compared with the quality of health visiting services in other areas.
Second, the high prevalence of those taking antidepressant medication (21/27) may have further contributed to improvement in symptoms. Previous studies which compared anti-depressant medication with Interpersonal Psychotherapy (IPT; Pearlstein et al., 2006) or with CBT (Misri, Reebye, Corral, & Mills, 2004) reported a similar pattern of results to the present study. Third, there may have been improvements in the intervention group, which our measures were not sensitive to, for example, marital relationship and parenting stress.
Finally, while the data suggest that the intervention content was acceptable to the sample, there remains some uncertainty around whether it is a sufficient target for PND. The focus of interventions for this population is a prevalent issue within the literature as evidence for the specificity of intervention targets is mixed (for a review, see Bennett et al., 2007). The suitability of the Baby Triple P intervention content for PND should therefore be considered as a focus of further research.
Limitations
Despite encouraging findings, some limitations need to be considered. Notably, the sample size was small, which prevented the detection of significant group differences. This is a common limitation of pilot studies, but does not necessarily imply a negative result (Altman & Bland, 1995). A further limitation was that all assessments and the delivery of Baby Triple P sessions were undertaken by the same person. Although this decision potentially introduced a response bias, it promoted engagement and contributed to low attrition. Indeed, several participants had expressed concerns over having to deal with multiple researchers.
Conclusion
This pilot RCT represents one of the first applications of parenting interventions in the context of PND and is the first to examine the feasibility and acceptability of Baby Triple P to PND. We have presented several important observations that could inform future research. Our findings suggest that this intervention with a parenting focus is highly acceptable to women with PND. Although the present study failed to demonstrate an additive effect of Baby Triple P, the pattern of results, albeit non-significant, were in the predicted direction with regard to level of happiness, self-regulation, subjective bonding and depression (at post-treatment only). These results should be taken as preliminary. However, on the basis of establishing feasibility and high acceptability in the present study, a larger scale RCT is warranted.
Author biographies
Zoe-Lydia Tsivos is a Trainee Clinical Psychologist at the University of Manchester. This research was completed as part of her PhD in Clinical Psychology at the University of Manchester (2012).
Rachel Calam is Professor of Child and Family Psychology and Head of the School of Psychological Sciences at The University of Manchester. She has a particular interest in increasing the reach of evidence-based parenting interventions.
Matthew R Sanders is a Professor of Clinical Psychology and Director of the Parenting and Family Support Centre at the University of Queensland. As the founder of the Triple P-Positive Parenting Program, Professor Sanders is considered a world leader in the development, implementation, evaluation and dissemination of population based approaches to parenting and family interventions.
Anja Wittkowski is a Senior Lecturer in Clinical Psychology at the University of Manchester. She also works as a clinical psychologist on a Mother and Baby Unit. She is interested in perinatal psychology and in particular in the mental health of mothers.
Footnotes
Declaration of conflicting interests: Rachel Calam has long standing research collaborations with staff at the Parenting and Family Support Centre, School of Psychology, University of Queensland. She has been a board member of the Triple P Research Network and is currently on the Triple P International Scientific Advisory Committee in a research capacity. The Parenting and Family Research Group at The University of Manchester and its members have no share in, ownership of, or formal relationship with, Triple P International Pty Ltd and derive no funding or royalty from it.
Funding: This research was funded through grants from the University of Manchester, the Manchester Statistical Society and the Medical Research Council (MRC).
Standard Disclosure Statement: The Triple P-Positive Parenting Program is owned by the University of Queensland (UQ). The University through its main technology transfer company UniQuest Pty Limited, has licensed Triple P International Pty Ltd to disseminate the program worldwide. Royalties stemming from this dissemination activity are distributed to the Parenting and Family Support Centre, School of Psychology, UQ; Faculty of Health and Behavioural Sciences at UQ; and contributory authors. No author has any share or ownership in Triple P International Pty Ltd. Matthew Sanders is the founder and an author on various Triple P programs and a consultant to Triple P International.
References
- Altman D. G., Bland J. M. (1995). Statistics notes – Absence of evidence is not evidence of absence. BMJ, 311, 485–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appleby L., Whitton A. (1993). Recruitment for post-natal depression studies. British Journal of Psychiatry, 163, 691. [DOI] [PubMed] [Google Scholar]
- Argyle M., Martin M., Crossland J. (1989). Happiness as a function of personality and social encounters. In Forgas J. P., Innes J. M. (Eds.), Recent advances in social psychology: An international perspective (1st ed, pp. 189–203). North-Holland, The Netherlands: Elsevier. [Google Scholar]
- Arteche A., Joormann J., Harvey A., Craske M., Gotlib I. H., Lehtonen A., . . . Stein A. (2011). The effects of postnatal maternal depression and anxiety on the processing of infant faces. Journal of Affective Disorders, 133, 197–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. (1991). Social cognitive theory of self-regulation. Organizational Behavior and Human Decision Processes, 50, 248–287. [Google Scholar]
- Beck A., Steer R., Brown G. (1996). Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Bennett C., Macdonald G. M., Dennis J., Coren E., Patterson J., Astin M., Abbott J. (2007). Home-based support for disadvantaged adult mothers. The Cochrane Database of Systematic Reviews, 3, CD003759. [DOI] [PubMed] [Google Scholar]
- Boyd R. C., Zayas L. H., McKee M. D. (2006). Mother-infant interaction, life events and prenatal and postpartum depressive symptoms among urban minority women in primary care. Maternal and Child Health Journal, 10, 139–148. [DOI] [PubMed] [Google Scholar]
- Brockington I. F., Oates J., George S., Turner D., Vostanis P., Sullivan M., . . . Murdoch C. (2001). A screening questionnaire for mother-infant bonding disorders. Archives of Women’s Mental Health, 3, 133–140. [Google Scholar]
- Cohn J. F., Campbell S. B., Matias R., Hopkins J. (1990). Face-to-face interactions of postpartum depressed and nondepressed mother-infant pairs at 2 months. Developmental Psychology, 26(1), 15–23. [Google Scholar]
- Cooper P., Campbell E. A., Day A., Kennerley H., Bond A. (1988). Non-psychotic psychiatric disorder after childbirth: A prospective study of prevalence, incidence, course and nature. British Journal of Psychiatry, 152, 799–806. [DOI] [PubMed] [Google Scholar]
- Cooper P., Murray L. (1997). The impact of psychological treatments of postpartum depression on maternal mood and infant development. 1997. In Murray L. C. P. J. (Ed.), Postpartum depression and child development (pp. 201–220). New York, NY: Guilford Press. [Google Scholar]
- Cox J. L., Holden J. M., Sagovsky R. (1987). Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry, 150, 782–786. [DOI] [PubMed] [Google Scholar]
- Craig E. A. (2004). Parenting programs for women with mental illness who have young children: A review. Australian and New Zealand Journal of Psychiatry, 38, 923–928. [DOI] [PubMed] [Google Scholar]
- Crittenden P. M. (2004). CARE-Index: Coding manual. Unpublished manuscript. Miami, Florida. [Google Scholar]
- Crittenden P. M. (2008). Raising parents: Attachment, parenting and child safety. Devon, UK: Willan. [Google Scholar]
- Dennis C. L., Chung-Lee L. (2006). Postpartum depression help-seeking barriers and maternal treatment preferences: A qualitative systematic review. Birth, 33, 323–331. [DOI] [PubMed] [Google Scholar]
- Dennis C. L., McQueen K. (2007). Does maternal postpartum depressive symptomatology influence infant feeding outcomes? Acta Paediatrica, 96, 590–594. [DOI] [PubMed] [Google Scholar]
- Dennis C. L., Ross L. (2005). Relationships among infant sleep patterns, maternal fatigue, and development depressive symptomatology. Birth, 32, 187–193. [DOI] [PubMed] [Google Scholar]
- Feldman R., Granat A., Pariente C., Kanety H., Kuint J., Gilboa-Schechtman E. (2009). Maternal depression and anxiety across the postpartum year and infant social engagement, fear regulation, and stress reactivity. Journal of the American Academy of Child & Adolescent Psychiatry, 48, 919–927. [DOI] [PubMed] [Google Scholar]
- Field T. (2010). Postpartum depression effects on early interactions, parenting, and safety practices: A review. Infant Behavior & Development, 33(1), 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerhardt S. (2004). Why love matters: How affection shapes a baby’s brain. New York, NY: Routledge/Taylor & Francis Group. [Google Scholar]
- Goodman S. H., Gotlib I. H. (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106, 458–490. [DOI] [PubMed] [Google Scholar]
- Gorman L. L., O’Hara M. W., Figueiredo B., Hayes S., Jacquemain F., Kammerer M. H. (2004). Adaptation of the Structured Clinical Interview for DSM-IV disorders for assessing depression in women during pregnancy and post-partum across countries and cultures. British Journal of Psychiatry, 184(Suppl. 46), s17–s23. [DOI] [PubMed] [Google Scholar]
- Hart S. L., Jackson C., Boylan L. (2011). Compromised weight gain, milk intake, and feeding behavior in breastfed newborns of depressive mothers. Journal of Pediatric Psychology, 36, 942–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatton D. C., Harrison-Hohner J., Dorato V., Curen L. B., McCarron D. A. (2005). Symptoms of postpartum depression and breastfeeding. Journal of Human Lactation, 21, 444–449. [DOI] [PubMed] [Google Scholar]
- Hay D. F., Pawlby S., Angold A., Harold G. T., Sharp D. (2003). Pathways to violence in the children of mothers who were depressed postpartum. Developmental Psychology, 39, 1083–1094. [DOI] [PubMed] [Google Scholar]
- Hiscock H., Wake M. (2001). Infant sleep problems and postnatal depression: A community-based study. Pediatrics, 107, 1317–1322. [DOI] [PubMed] [Google Scholar]
- Hoath F. E., Sanders M. R. (2002). A feasibility study of enhanced group triple p-positive parenting program for parents of children with attention-deficit/hyperactivity disorder. Behaviour Change, 19, 191–206. [Google Scholar]
- Jacobson N. S., Truax P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J., Moffitt T. E., Taylor A., Pawlby S. J., Caspi A. (2005). Maternal depression and child antisocial behaviour: Nature and nurture effects. Archives of General Psychiatry, 62, 173–181. [DOI] [PubMed] [Google Scholar]
- Lancaster G. A., Dodd S., Williamson P. R. (2004). Design and analysis of pilot studies: Recommendations for good practice. Journal of Evaluation in Clinical Practice, 10, 307–312. [DOI] [PubMed] [Google Scholar]
- Lee D. T. S., Chung T. H. K. (2007). Postnatal depression: an update. Best Practice & Research Clinical Obstetrics and Gynaecology, 21(2), 183–191. [DOI] [PubMed] [Google Scholar]
- Lovejoy M. C., Graczyk P. A., O’Hare E., Neuman G. (2000). Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review, 20, 561–592. [DOI] [PubMed] [Google Scholar]
- Markie-Dadds C., Sanders M. R., Turner K. M. T. (1999). Every parent’s self-help workbook. Brisbane, Queensland, Australia: Families International Publishing. [Google Scholar]
- Martins C., Gaffan E. A. (2000). Effects of early maternal depression on patterns of infant-mother attachment: A meta-analytic investigation. Journal of Child Psychology and Psychiatry, 41, 737–746. [PubMed] [Google Scholar]
- McLearn K. T., Minkovitz C. S., Strobino D. M., Marks E., Hou W. (2006a). Maternal depressive symptoms at 2 to 4 months postpartum and early parenting practices. Archives of Pediatric & Adolescent Medicine, 160, 279–284. [DOI] [PubMed] [Google Scholar]
- McLearn K. T., Minkovitz C. S., Strobino D. M., Marks E., Hou W. (2006b). The timing of maternal depressive symptoms and mothers’ parenting practices with your children: Implications for pediatric practice. Pediatrics, 118, e174–e182. [DOI] [PubMed] [Google Scholar]
- Meaney M. J. (2001). Maternal care, gene expression, and the transmission of individual differences in stress reactivity across generations. Annual Review of Neuroscience, 24, 1161–1192. [DOI] [PubMed] [Google Scholar]
- Milgrom J., Martin P. R., Negri L. M. (1999). Treating postnatal depression: a psychological approach for health care practitioners. London: Wiley. [Google Scholar]
- Milgrom J., Negri L. M., Gemmill A. W., McNeil M., Martin P. R. (2005). A randomized controlled trial of psychological interventions for postnatal depression. British Journal of Clinical Psychology, 44, 529–542. [DOI] [PubMed] [Google Scholar]
- Milgrom J., Westley D., Gemmill A. (2004). The mediating role of maternal responsiveness in some longer term effects of postnatal depression on infant development. Infant Behavior & Development, 27, 443–454. [Google Scholar]
- Minkovitz C. S., Strobino D., Charfstein D., Hou W., Miller T., Mistry K. B. (2005). Maternal depressive symptoms and children’s receipt of healthcare in the first 3 years of life. Pediatrics, 115, 306–314. [DOI] [PubMed] [Google Scholar]
- Misri S., Reebye P., Corral M., Mills L. (2004). The use of paroxetine and cognitive-behavioral therapy in postpartum depression and anxiety: A randomized controlled trial. Journal of Clinical Psychiatry, 65, 1236–1241. [DOI] [PubMed] [Google Scholar]
- Murray L., Stein A. (1991). The effects of postnatal depression on mother-infant relations and infant development. In Woodhead M., Carr R., Light P. (Eds.), Becoming a person (pp. 144–166). Florence, KY: Taylor & Frances/Routledge. [Google Scholar]
- O’Hara M. W. (1994). Postpartum depression: Causes and consequences (Series in psychopathology). New York, NY: Springer-Verlag. [Google Scholar]
- O’Hara M. W. (2009). Postpartum depression: What we know. Journal of Clinical Psychology, 65, 1258–1269. [DOI] [PubMed] [Google Scholar]
- O’Hara M. W., Stuart S., Gorman L. L., Wenzel A. (2000). Efficacy of interpersonal psychotherapy for postpartum depression. Archives of General Psychiatry, 57, 1039–1045. [DOI] [PubMed] [Google Scholar]
- Pearlstein T., Zlotnick C., Battle C., Stuart S., O’Hara M., Price A., . . . Howard M. (2006). Patient choice of treatment for postpartum depression: A pilot study. Archives of Women’s Mental Health, 9, 303–308. [DOI] [PubMed] [Google Scholar]
- Poobalan A., Aucott L., Ross L., Smith W., Helms P., Williams J. (2007). Effects of treating postnatal depression on mother-infant interaction and child development: Systematic review. British Journal of Psychiatry, 191, 378–386. [DOI] [PubMed] [Google Scholar]
- Pridham K. F., Chang A. S. (1989). What being the parent of a baby is like: Revision of an instrument. Research in Nursing and Health, 12, 323–329. [DOI] [PubMed] [Google Scholar]
- Reck C., Noe D., Stefenelli U., Fuchs T., Cenciotti F., Stehle E., . . . Tronick E. Z. (2011). Interactive coordination of currently depressed inpatient mothers and their infants during the postpartum period. Infant Mental Health Journal, 32, 542–562. [DOI] [PubMed] [Google Scholar]
- Righetti-Veltema M., Conne-Perreard E., Bousquet A., Manzano J. (2002). Postpartum depression and mother-infant relationship at 3 months old. Journal of Affective Disorders, 70, 291–306. [DOI] [PubMed] [Google Scholar]
- Sanders M. R. (2012). Development, evaluation and multinational dissemination of the triple P-positive parenting program. Annual Review of Clinical Psychology, 8, 345–379. [DOI] [PubMed] [Google Scholar]
- Sanders M. R., Markie-Dadds C., Tully L., Bor W. (2000). The Triple P Positive Parenting Program: A comparison of enhanced, standard, and self-directed behavioral family intervention for parents of children with early onset conduct problems. Journal of Consulting and Clinical Psychology, 68, 624–640. [PubMed] [Google Scholar]
- Sanders M. R., Markie-Dadds C., Turner K. M. T. (2001). Practitioner’s manual for Standard Triple P. Brisbane, Queensland, Australia: Triple P International Pty Ltd. [Google Scholar]
- Sanders M. R., Markie-Dadds C., Turner K. M. T. (2003). Theoretical, scientific and clinical foundations of the Triple P-Positive Parenting Program: A populations approach to promotion of parenting competence. Parenting Research and Practice Monograph, 1, 1–25. [Google Scholar]
- Sanders M. R., Mazzucchelli T. G. (2013). The promotion of self-regulation through parenting interventions. Clinical Child and Family Psychology Review, 16(1), 1–17. [DOI] [PubMed] [Google Scholar]
- Sanders M. R., Mazzucchelli T. G., Ralph A. (2012b). Promoting parenting competence through a self-regulation approach to feedback. In Sutton R. M., Hornsey M. J., Douglas K. M. (Eds.), Feedback: The communication of praise, criticism, and advice (pp. 305–321). New York, NY: Peter Lang. [Google Scholar]
- Sanders M. R., McFarland M. (2000). Treatment of depressed mothers with disruptive children: A controlled evaluation of cognitive behavioral family intervention. Behaviour Therapy, 31(1), 89–112. [Google Scholar]
- Sejourne N., Alba J., Onorrus M., Goutaudier N., Chabrol H. (2011). Intergenerational transmission of postpartum depression. Journal of Reproductive and Infant Psychology, 29, 115–124. [Google Scholar]
- Shakespeare J., Blake F., Garcia J. (2006). How do women with postnatal depression experience listening visits in primary care? A qualitative interview study. Journal of Reproductive and Infant Psychology, 24, 149–162. [Google Scholar]
- Spry C., Morawska A., Sanders M. R. (2009). Baby Triple P. Brisbane, Queensland, Australia: Triple P International. [Google Scholar]
- Stein A., Malmberg L., Sylva K., Barnes J., Leach P. (2008). The influence of maternal depression, caregiving, and socioeconomic status in the post-natal year on children’s language development. Child: Care, Health and Development, 34, 603–612. [DOI] [PubMed] [Google Scholar]
- Tronick E., Reck C. (2009). Infants of depressed mothers. Harvard Review of Psychiatry, 17, 147–156. [DOI] [PubMed] [Google Scholar]
- Tronick E., Weinberg M. K. (1997). Depressed mothers and infants: Failure to form dyadic states of consciousness. In Murray L., Cooper P. (Eds.), Postpartum depression and child development (pp. 54–81). New York, NY: Guilford Press. [Google Scholar]
- Tsivos Z. L., Sanders M. R. (2012). Brief Parenting Beliefs Scale – Baby version. Brisbane, Queensland, Australia: Parenting and Family Support Centre, University of Queensland. [Google Scholar]
- Turner K. M., Sanders M. R. (2006). Help when it’s needed first: A controlled evaluation of brief, preventative behavioral family intervention in a primary care setting. Behavior Therapy, 37(2), 131–142. [DOI] [PubMed] [Google Scholar]
- Van Doesum K., Riksen-Walraven J., Hosman C., Hoefnagels C. (2008). A randomized controlled trial of a home-visiting intervention aimed at preventing relationship problems in depressed mothers and their infants. Child Development, 79, 547–561. [DOI] [PubMed] [Google Scholar]
- Vik T., Grote V., Escribano J., Socha J., Verduci E., Fritsch M., . . . Koletzko B. (2009). Infantile colic, prolonged crying and maternal postnatal depression. Acta Paediatrica, 98, 1344–1348. [DOI] [PubMed] [Google Scholar]
- Wittkowski A., Williams J., Wieck A. (2010). An examination of the psychometric properties and factor structure of the post-partum bonding questionnaire in a clinical impatient sample. British Journal of Clinical Psychology, 49, 163–172. [DOI] [PubMed] [Google Scholar]
- Zajicek-Farber M. L. (2009). Postnatal depression and infant health practices among high-risk women. Journal of Child and Family Studies, 18, 236–245. [Google Scholar]
- Zajicek-Farber M. L. (2010). The contributions of parenting and postnatal depression on emergent language of children in low-income families. Journal of Child and Family Studies, 19, 257–269. [Google Scholar]