Abstract
Introduction
Despite the known benefits of early treatment initiation for individual morbidity and mortality, as well as for reducing the risk of transmission, late presentation (LP) to HIV/AIDS services remains a major concern in many countries. There is little information on LP from middle and low-income countries and studies that do evaluate LP commonly disaggregate data by sex. It is rare, however, for researchers to further disaggregate the data by pregnancy status so it remains unclear if pregnancy status modifies the effects associated with sex.
Methods
The study was conducted at the only State Reference Center for HIV/AIDS in Salvador, Brazil’s third largest city. LP was defined as a patient accessing services with a CD4<350 cells/mm3. Data were abstracted from the electronic medical records of 1421 patients presenting between 2007 and 2009. CD4 counts and viral load (VL) information was validated with data from the National CD4/VL Database. Descriptive and bivariate statistics were conducted to inform the multivariate analysis. Adjusted prevalence ratios (APR) were estimated using generalized linear models due to the high frequency of the outcome.
Results
Half of the sample (52.5%; n=621) was classified as LP. Compared to the prevalence among pregnant women (21.1%), the prevalence of LP was more than twice as high among non-pregnant women (56.0%) and among men (55.4%). The multivariate analysis demonstrated no statistical difference between men and non-pregnant women (APR 1.04; 95%CI 0.92–1.19), but the APR of LP for non-pregnant women was 53% less than men (APR 0.47; 95%CI 0.33–0.68).
Conclusion
These results highlight the importance of analyzing data disaggregated not only by sex but also by pregnancy status to accurately identify the risk factors associated with LP so that programs and policies can effectively and efficiently address LP in Brazil and beyond.
Keywords: HIV/AIDS, late presentation, CD4 count, pregnancy, Brazil
INTRODUCTION
Despite increasing availability of antiretroviral therapy (ART) in many countries, studies have documented that HIV-positive individuals continue to access HIV/AIDS services at an advanced stage of infection (Althoff et al., 2010; Metallidis et al., 2012; O’Shea, Ebrahim, Egli, Redmond, & McConkey, 2013; Oliva et al., 2010; Wohlgemut, Lawes, & Laing, 2012). This late presentation (LP) to HIV/AIDS services is a substantial concern given the known benefits of early treatment initiation for individual morbidity and mortality, as well as for reducing the risk of transmission. However, the majority of studies on LP have been conducted in high-income countries, where the proportion of LP ranges from 30 to 67% (Bamford, Ehrenkranz, Eberhart, Shpaner, & Brady, 2010; Cevallos Garcia, Verdejo Ortes, Martinez Rodriguez, & Izarra Perez, 2012; d’Arminio Monforte et al., 2011; de Olalla et al., 2011; Dennis, Napravnik, Sena, & Eron, 2011; Dickson, McAllister, Sharples, & Paul, 2012; Diez et al., 2012; Helleberg et al., 2012; Leutscher et al., 2011; Mocroft et al., 2013; Ursini et al., 2012; Vincent et al., 2012; Wohlgemut et al., 2012; Zoufaly et al., 2012). In Brazil, a middle-income country were ART has been free and universally available since 1996 (Teixeira, Vitoria, & Barcarolo, 2004), three national studies estimated that between 33% (Fernandes, Acurcio Fde, Campos, & Guimaraes, 2009; Souza-Jr, Szwarcwald, & Castilho, 2007) and 43.6% of people living with HIV utilized HIV/AIDS services with CD4 cell counts <200 cells/mm3 or clinical symptoms of AIDS (Grangeiro, Escuder, Menezes, Alencar, & Ayres de Castilho, 2011). These studies suggest that even in Brazil, individuals living with HIV continue to utilize HIV/AIDS services at an advanced stage of HIV infection.
Increasingly, in Brazil and in other countries globally, the problem of LP is being recognized but issues impede the accurate analysisof LP in the peer-review literature. There is growing attention to the importance of controlling for sex as being male is commonly identified as a risk factor for LP. It is rare, however, for researchers to further control for pregnancy status as most studies examine LP among pregnant women in separate subgroup analyses (Fitzgerald et al., 2010; Izzo et al., 2011; Tariq, Elford, Cortina-Borja, & Tookey, 2012; Thayaparan, Balachandran, & Kawser, 2012). This potentially has major implications for the interpretation of results. Many women are tested during antenatal care and therefore are likely tested at an earlier stage of their disease progression. In comparison, non-pregnant women may be tested as a result of experiencing HIV/AIDS related symptoms and therefore are at a later stage of their disease progression and may be no different from men. It remains unclear if pregnancy status modifies the effects associated with sex, and despite controlling for sex, it is surprising that none of the studies in Brazil and only one of the studies outside of Brazil on LP controlled for pregnancy status (Krawczyk et al., 2006). Therefore the purpose of this study was to investigate the prevalence of LP in Brazil and determine if disaggregating the data based on sex and pregnancy status impacted our understanding of LP.
METHODS
The data (n=1,564) were collected in a cross-sectional study conducted at the only State Reference Center (SRC) for HIV/AIDS in Bahia, a state in the northeastern region of Brazil. The study population was comprised of all individuals ≥15 years of age living with HIV who were enrolled in HIV care for the first time at the SRC between 2007 and 2009. Data were abstracted from the electronic medical records of 1,564 patients. These records were then supplemented with additional information reviewed by trained research assistantsfrom “SINAN” (Information System on Disease Notification), a database of registered AIDS cases and HIV-infected pregnant women. 143 records with missing CD4 cell count data were excluded resulting in review of 1,421 patient records (90.9%). Information was reviewed by trained research assistants from hand written clinical records and from the national database “SISCEL” (Laboratory Test Control System of the Brazilian National CD4+/CD8+T Lymphocyte Count and Viral Load Network).
The outcome variable LP was based on the consensus statement released by the European Late Presenter Group that defined LP as individuals with a CD4 cell count<350 cells per/mm3 and/or symptoms of AIDS-defining illnesses (Antinori et al., 2011; Antinori, Johnson, Moreno, Yazdanpanah, & Rockstroh, 2010). For our analysis, the outcome was restricted to individuals with available CD4 cell count.
We conducted a comprehensive review of the literature to identify variables of interest that should be included in the data analysis. Key descriptive statistics were generated for all study variables available in the electronic medical records. For the multivariate analysis, we included variables highlighted in the literature review and fromthe bivariate analysis if they had a p-value smaller than 0.20. Adjusted prevalence ratios (APR) were estimated using generalized linear models due to the high frequency of the outcome (McNutt, Wu, Xue, & Hafner, 2003) using STATA 10. This study was approved by the Ethics and Research Committee of the State Health Department of Bahia and written informed consent was given by all participants.
RESULTS
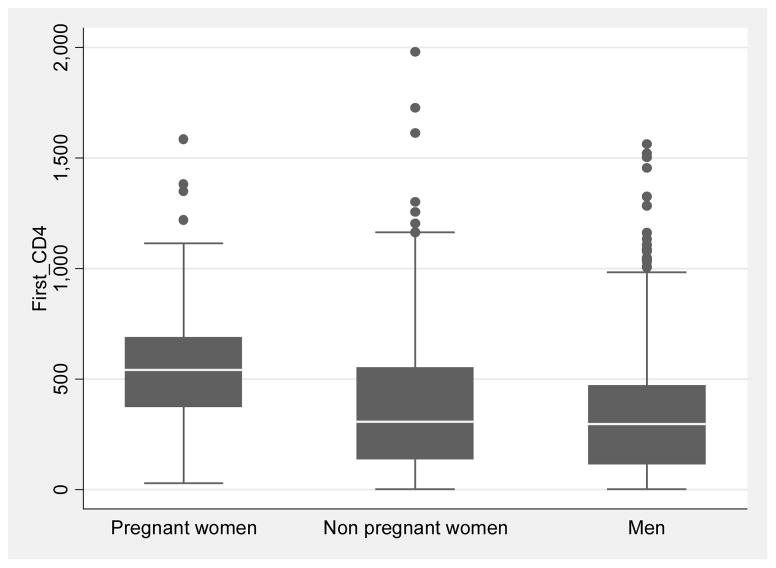
Of the 1,421 patients included in the study from 2007–2009, 54% were males (769) and among females (652), 21.3% were pregnant (139). While the prevalence of LP among men was 55.4% and 48.9% among all women, further analysis showed differences based on pregnancy status: The prevalence of LP (CD4<350 cells/mm3) was slightly higher among non-pregnant women (56.0%) as compared to men (55.4%), but was twice that compared to prevalence among pregnant women (22.1%). The proportion of non-pregnant women (32.5%) and men (37.5%) presented for HIV/AIDS care at an advanced stage of the infection (CD4<200 cells/mm3) was much higher compared to the proportion of pregnant women (7.1%). Complete descriptive statistics are provided in Table 1 and bivariate statistics are provided in Table 2. In terms of the distribution of CD4 counts, pregnant women had higher median CD4 counts (543 cells per mm3) than non-pregnant women (357 cells per mm3) and substantially higher than men (298 cells per mm3) (Figure 1). The differences in the median values were statistically significant (p-value=0.0001) and highlights that pregnancy statussubstantially confounds the effect of sex.
Table 1.
Descriptive statistics of pregnant women, non-pregnant women and men (n=1421) receiving HIV/AIDS care at the State Reference Center in Salvador, Brazil between 2007 and 2009
| Variable | Pregnant women | Non-pregnant women | Men | p-value |
|---|---|---|---|---|
|
| ||||
| N (%) | N (%) | N (%) | ||
| CD4 cell at enrolment | 0.0001 | |||
| CD4 >=350 cells per mm3 | 88 (77.9) | 191 (44.0) | 284 (44.6) | |
| CD4<350 cell per mm3 | 25 (22.1) | 243 (56.0) | 353 (55.4) | |
| Presented with an advanced stage of thedisease | 0.0001 | |||
| CD4 >=200 cells per mm3 | 105 (92.9) | 293 (67.5) | 398 (62.5) | |
| CD4 <200 cells per mm3 | 8 (7.1) | 141 (32.5) | 239 (37.5) | |
| Age | 0.0001 | |||
| 15–24 | 50 (35.9) | 76 (14.1) | 95 (12.4) | |
| 25–34 | 69 (49.6) | 190 (37.0) | 322 (41.9) | |
| 35–44 | 20 (14.4) | 164 (31.2) | 216 (28.1) | |
| 45 or older | - | 83(16.2) | 136 (17.7) | |
| Education* | 0.008 | |||
| Greater than 8 years | 9 (33.3) | 40 (35.1) | 101 (51.8) | |
| Up to 8 years | 18 (67.7) | 74 (64.9) | 94 (48.2) | |
| Skin color | 0.001 | |||
| White | 9 (6.6) | 47 (9.3) | 116 (15.4) | |
| Black or brown | 128 (93.4) | 459 (90.7) | 638 (84.6) | |
| Sexual orientation | 0.0001 | |||
| Heterosexual | 135 (98.5) | 489 (97.4) | 397 (52.0) | |
| Homosexual or bisexual | 2 (1.5) | 13 (2.6) | 367 (48.0) | |
| Civil status | 0.001 | |||
| With a partner | 37 (27.0) | 111 (21.8) | 120 (15.8) | |
| Without a partner | 100 (73.0) | 398 (78.2) | 638 (84.2) | |
| Type of sexual partner | 0.0001 | |||
| Main partner** | 122 (91.0) | 330 (76.7) | 375 (53.6) | |
| Non-main partner | 12 (9.0) | 100 (23.3) | 325 (46.4) | |
| Condom use | 0.0001 | |||
| Always or sometimes | 79 (58.8) | 296 (59.2) | 572 (75.1) | |
| Never | 60 (47.2) | 204 (40.8) | 190 (24.9) | |
| Drug use | 0.0001 | |||
| Never | 128 (93.4) | 466 (91.6) | 636 (83.5) | |
| Frequently and/or sometimes | 9 (6.6) | 43 (8.4) | 126 (16.5 | |
| Alcohol use | 0.0001 | |||
| Never | 88 (66.2) | 310 (64.7) | 323 (46.9) | |
| Frequently and/or sometimes | 45 (33.8) | 169 (35.3) | 366 (53.1) | |
| Location | 0.003 | |||
| Metropolitan region of Salvador | 92 (66.2) | 347 (67.6) | 581 (75.6) | |
| Outside metropolitan region of Salvador | 47 (33.8) | 166 (32.4) | 188 (24.5) | |
Data on education only available for 24% of the participants;
To be with someone for more than a month
Table 2.
Bivariate statistics including the number, proportion, prevalence ratio (PR) and 95% confidence interval (CI) of late presentation among patients receiving HIV/AIDS care at the State Reference Center in Salvador, Brazil between 2007 and 2009
| Variable | Late Presentation | p-value | |||
|---|---|---|---|---|---|
| N | % | PR | 95% CI | ||
| Sex | 0.001 | ||||
| Men | 353 | 55.4 | 1.00 | ||
| Non-pregnant women | 434 | 56.0 | 1.01 | 0.91–1.13 | |
| Pregnant women | 113 | 22.1 | 0.40 | 0.28–0.57 | |
| Age | 0.001 | ||||
| 15–24 | 167 | 33.5 | 1.00 | ||
| 25–34 | 480 | 50.0 | 1.49 | 1.18–1.88 | |
| 35–44 | 343 | 57.1 | 1.70 | 1.35–2.15 | |
| 45 or older* | 194 | 66.5 | 1.98 | 1.57–2.51 | |
| Skin color | 0.84 | ||||
| White | 150 | 53.3 | 1.00 | ||
| Black | 1012 | 52.5 | 0.98 | 0.84–1.16 | |
| Education** | 0.32 | ||||
| Up to 8 years | 162 | 60.5 | 1.00 | ||
| Greater than 8 years | 137 | 54.7 | 1.11 | 0.91–1.35 | |
| Civil status | 0.510 | ||||
| With a partner | 223 | 50.8 | 1.00 | ||
| Without a partner | 945 | 53.1 | 1.05 | 0.91–1.21 | |
| Sexual orientation | 0.13 | ||||
| Heterosexual | 850 | 50.9 | 1.00 | ||
| Homosexual or bisexual | 320 | 55.9 | 1.10 | 0.98–1.24 | |
| Condom use | 0.290 | ||||
| Never | 381 | 54.6 | 1.00 | ||
| Always or sometimes | 786 | 51.3 | 0.83 | 0.84–1.05 | |
| Drug use | 0.090 | ||||
| Never | 1037 | 53.3 | 1.00 | ||
| Frequently and/or sometimes | 134 | 45.5 | 0.85 | 0.70–1.04 | |
| Alcohol use | 0.070 | ||||
| Never | 614 | 54.6 | 1.00 | ||
| Frequently and/or sometimes | 478 | 49.0 | 0.90 | 0.80–1.01 | |
| Location | 0.860 | ||||
| Metropolitan region of Salvador | 851 | 52.3 | 1.00 | ||
| Outside metropolitan region of Salvador | 333 | 52.9 | 0.99 | 0.88–1.11 | |
Pregnant women not included in this category as there was no pregnant women older than 44 years of age;
Data on education only available for 24% of the participants;
Figure 1.
Distribution and median CD4 count for pregnant women (543 cells per mm3), non-pregnant women (307 cells per mm3) and men (298 cells per mm3)
The multivariate analysis demonstrated no statistical difference between men and non-pregnant women (APR 1.04; 95%CI 0.92–1.19), but the APR of LP for non-pregnant women was 53% less than men (APR 0.47; 95%CI 0.33–0.68). Compared to individuals age 15–24, the APR of LP increased with each age category: from 1.46 (95%CI 1.13–1.87), to 1.59 (95%CI 1.24–2.04), to 1.77 (95%CI 1.37–2.29). Alcohol use seemed associated with lower prevalence of LP but only bordered statistical significance(Table 3).
Table 3.
Prevalence ratios and 95% confidence intervals of the association between late presentation among patients receiving HIV/AIDS care at the State Reference Center in Salvador, Brazil between 2007 and 2009
| Variable | Late Presentation | p-value | |
|---|---|---|---|
| * APR | **95%CI | ||
| Sex (men as reference) | 1.00 | ||
| Non-pregnant women | 1.04 | 0.92–1.19 | 0.510 |
| Pregnant women | 0.47 | 0.33–0.68 | 0.001 |
| Age (15–24 as reference) | 1.00 | ||
| 25–34 | 1.46 | 1.13–1.87 | 0.003 |
| 35–44 | 1.59 | 1.24–2.04 | 0.001 |
| 45 or older | 1.77 | 1.37–2.29 | 0.001 |
| Sexual orientation | |||
| Heterosexual | 1.00 | ||
| Homosexual or bisexual | 1.07 | 0.93–1.23 | 0.340 |
| Drug use | |||
| Never | 1.00 | ||
| Frequently and/or sometimes | 0.93 | 0.75–1.15 | 0.500 |
| Alcohol use | |||
| Never | 1.00 | ||
| Frequently and/or sometimes | 0.88 | 0.79–0.99 | 0.040 |
APR: adjusted prevalence ratios from GLM (generalized linear models) regression;
Pregnant women not included in this category as there was no pregnant woman older than 44 years of age;
DISCUSSION
In some respects, the findings of our study may appear simple, however the implications are significant. For example, there was no difference in the proportion of LP based on sex, but further disaggregating the data by pregnancy status showed that pregnant women, compared to non-pregnant women and men, were less likely to record a first CD4 count below 350 cells per mm3. Currently there is a strong assumption in the peer-reviewed literature that males delay in accessing care as several studies stated that men have a higher risk of LP than women (Choe et al., 2011; Cornell M, 2012; Dennis et al., 2011; Mocroft et al., 2013; Moreira et al., 2011). However, none of these studies accounted for pregnancy status in their analysis, nor did they compare non-pregnant women with men. Evidence from our study suggests that controlling for pregnancy status may minimize, if not eliminate, the difference among men and non-pregnant women. Thus, as the problem of LP is increasingly recognized among men, these results suggest that greater attention should also be given to LP among non-pregnant women.
Additional research should disentangle the role of pregnancy status in defining health-seeking behaviors. Doing so would enable programs and policies to more effectively ensure that all individuals who test positive are then successfully linked to sustained HIV/AIDS care, whether male, female, pregnant, or not. If the current status quo persists then individuals who are not traditionally considered at increased risk for HIV, such as non-pregnant women, may continue to be overlooked which has severe implications for individual health, as well as the risk of transmission to sexual partners.
LP was also associated with age among men and non-pregnant women. This is consistent with the findings from other studies (Adler, Mounier-Jack, & Coker, 2009; Helleberg et al., 2012; Metallidis et al., 2012; Tey et al., 2012; Vincent et al., 2012; Vives et al., 2012). Studies suggest that the progression of infection may be more rapid in older individuals (Kirk & Goetz, 2009; Manfredi, 2002, 2004). It is also possible that providers do not perceive their older age patients to be at risk for HIV infection, nor do older age individuals themselves feel at risk, and therefore are less likely to be tested for HIV. Even among individuals who may be aware their risk for HIV, other physical barriers (such as access to testing sites) or social barriers (such as HIV-related stigma) (Mussini, 2012)may prevent them from utilizingavailable services.
Limitations of our study should be acknowledged. The cross-sectional study design limited our ability to assess temporal association and to adjust for time. Incompleteness of documentation in the patient’s electronic database and charts for education, income and occupation limited our ability to assess these variables. Finally, the outcome defines patients as late presenters based on their CD4 count so it is unclear if individuals were late in their diagnosis of HIV or late in their subsequent linkage to care (Kozak, Zinski, Leeper, Willig, & Mugavero, 2013; Maccarthy, Bangsberg, Fink, Reich, & Gruskin, 2013). Importantly, thisstudy highlights the need to controlfor pregnancy status, and although this seems relatively straightforward, it is not consistently done in studies on LP.
CONCLUSIONS
This study underscores the need for the risk factors of LP to be accurately identified. Specifically, it is critical that the role of pregnancy status be addressed in analyses to ensure results can be translated into programmatic and policy action for all populations who need them. Only in so doing can we begin to reduce and eventually eliminate LP to testing, treatment and care in Brazil and beyond.
Acknowledgments
Funding
This article was supported by UNAIDS, UNIFEM, Brazilian National Department of STD/AIDS and Viral Hepatitis/Ministry of Health, the Foundation for Research Support of the State of Bahia (FAPESB), The HIV/AIDS Reference Center of the Bahia Department of Health (CEDAP/SESAB), The Pathfinder Foundation and the “HIV and Other Infectious Consequences of Substance Abuse” under Grant T32DA13911-12; the Lifespan/Tufts/Brown Center for AIDS Research under grant P30AI042853.
Footnotes
The authors would like to express their gratitude to Dr. Pedro Chequer who inspired us to investigate late presentation, to Joselina Soeiro, Lucília Nascimento and Rafaela Santos for the field work coordination, and Cristiane Mercês and Sandra Brignol for the database organization.
Competing interests
None of the authors have any conflicts of interest (including financial and other relationships) to declare.
Authors’ contributions
This manuscript has not been submitted or accepted for publication elsewhere. All authors contributed to the concept of the paper and data analysis. ID, SM and SG were responsible for the writing of the final version of the manuscript. All authors have read and approved the paper, have met the criteria for authorship as established by the International Committee of Medical Journal Editors, believe that the paper represents honest work, and are able to verify the validity of the results reported.
Disclosure of funding for this work from relevant institutions: n/a
Contributor Information
Inês Dourado, Email: ines.dourado@gmail.com.
Sarah MacCarthy, Email: sarah_maccarthy@brown.edu.
Carlos Lima, Email: carlosls@carlosls.com.br.
Maria Amélia Veras, Email: maria.veras@gmail.com.
Ligia Kerr, Email: ligiakerr@gmail.com.
Ana Maria de Brito, Email: anabrito1009@gmail.com.
Sofia Gruskin, Email: Gruskin@med.usc.edu.
References
- Adler A, Mounier-Jack S, Coker RJ. Late diagnosis of HIV in Europe: definitional and public health challenges. [Research Support, Non-U.S. Gov’t] AIDS Care. 2009;21(3):284–293. doi: 10.1080/09540120802183537. [DOI] [PubMed] [Google Scholar]
- Althoff KN, Gange SJ, Klein MB, Brooks JT, Hogg RS, Bosch RJ, Moore RD. Late presentation for human immunodeficiency virus care in the United States and Canada. Clin Infect Dis. 2010;50(11):1512–1520. doi: 10.1086/652650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antinori A, Coenen T, Costagiola D, Dedes N, Ellefson M, Gatell J, De Wolf F. Late presentation of HIV infection: a consensus definition. [Research Support, Non-U.S. Gov’t] HIV Med. 2011;12(1):61–64. doi: 10.1111/j.1468-1293.2010.00857.x. [DOI] [PubMed] [Google Scholar]
- Antinori A, Johnson M, Moreno S, Yazdanpanah Y, Rockstroh JK. Report of a European Working Group on late presentation with HIV infection: recommendations and regional variation. [Congresses Research Support, Non-U.S. Gov’t] Antivir Ther. 2010;15(Suppl 1):31–35. doi: 10.3851/IMP1525. [DOI] [PubMed] [Google Scholar]
- Bamford LP, Ehrenkranz PD, Eberhart MG, Shpaner M, Brady KA. Factors associated with delayed entry into primary HIV medical care after HIV diagnosis. AIDS. 2010;24(6):928–930. doi: 10.1097/QAD.0b013e328337b116. [DOI] [PubMed] [Google Scholar]
- Cevallos Garcia C, Verdejo Ortes J, Martinez Rodriguez S, Izarra Perez C. Late diagnosis of human immuno deficiency virus infection in the Madrid region (2007–2011) Rev Esp Salud Publica. 2012;86(1):37–47. doi: 10.1590/S1135-57272012000100004. [DOI] [PubMed] [Google Scholar]
- Choe PG, Park WB, Song JS, Kim NH, Park JY, Song KH, Oh MD. Late presentation of HIV disease and its associated factors among newly diagnosed patients before and after abolition of a government policy of mass mandatory screening. [Research Support, Non-U.S. Gov’t] J Infect. 2011;63(1):60–65. doi: 10.1016/j.jinf.2011.05.002. [DOI] [PubMed] [Google Scholar]
- Cornell MSM, Garone DB, Giddy J, Hoffmann CJ, Lessells R, Maskew M, Prozesky H, Wood R, Johnson LF, Egger M, Boulle A, Myer L for the International Epidemiologic Databases to Evaluate AIDS Southern Africa (IeDEA-SA) Collaboration. Gender Differences in Survival among Adult Patients Starting Antiretroviral Therapy in South Africa: A Multicentre Cohort Study. PLOS Med. 2012;9(9):e1001304. doi: 10.1371/journal.pmed.1001304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- d’Arminio Monforte A, Cozzi-Lepri A, Girardi E, Castagna A, Mussini C, Di Giambenedetto S, Antinori A. Late presenters in new HIV diagnoses from an Italian cohort of HIV-infected patients: prevalence and clinical outcome. Antivir Ther. 2011;16(7):1103–1112. doi: 10.3851/IMP1883. [DOI] [PubMed] [Google Scholar]
- de Olalla PG, Mazardo C, Sambeat MA, Ocana I, Knobel H, Humet V, Cayla JA. Epidemiological characteristics and predictors of late presentation of HIV infection in Barcelona (Spain) during the period 2001–2009. AIDS Res Ther. 2011;8(1):22. doi: 10.1186/1742-6405-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis AM, Napravnik S, Sena AC, Eron JJ. Late entry to HIV care among Latinos compared with non-Latinos in a southeastern US cohort. [Research Support, N.I.H., Extramural] Clin Infect Dis. 2011;53(5):480–487. doi: 10.1093/cid/cir434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickson N, McAllister S, Sharples K, Paul C. Late presentation of HIV infection among adults in New Zealand: 2005–2010. [Research Support, Non-U.S. Gov’t] HIV Med. 2012;13(3):182–189. doi: 10.1111/j.1468-1293.2011.00959.x. [DOI] [PubMed] [Google Scholar]
- Diez M, Oliva J, Sanchez F, Vives N, Cevallos C, Izquierdo A. Incidence of new HIV diagnoses in Spain, 2004–2009. Gac Sanit. 2012;26(2):107–115. doi: 10.1016/j.gaceta.2011.07.023. [DOI] [PubMed] [Google Scholar]
- Fernandes JR, de Acurcio FA, Campos LN, Guimaraes MD. Initiation of antiretroviral therapy in HIV-infected patients with severe immunodeficiency in Belo Horizonte, Minas Gerais State, Brazil. Cad Saude Publica. 2009;25(6):1369–1380. doi: 10.1590/s0102-311x2009000600019. [DOI] [PubMed] [Google Scholar]
- Fitzgerald FC, Bekker LG, Kaplan R, Myer L, Lawn SD, Wood R. Mother-to-child transmission of HIV in a community-based antiretroviral clinic in South Africa. [Comparative Study Research Support, N.I.H., Extramural] S Afr Med J. 2010;100(12):827–831. doi: 10.7196/samj.4045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grangeiro A, Escuder MM, Menezes PR, Alencar R, Ayres de Castilho E. Late entry into HIV care: estimated impact on AIDS mortality rates in Brazil, 2003–2006. [Research Support, Non-U.S. Gov’t] PLoS One. 2011;6(1):e14585. doi: 10.1371/journal.pone.0014585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helleberg M, Engsig FN, Kronborg G, Laursen AL, Pedersen G, Larsen O, Obel N. Late presenters, repeated testing, and missed opportunities in a Danish nationwide HIV cohort. Scand J Infect Dis. 2012;44(4):282–288. doi: 10.3109/00365548.2011.626440. [DOI] [PubMed] [Google Scholar]
- Izzo I, Forleo MA, Casari S, Quiros-Roldan E, Magoni M, Carosi G, Torti C. Maternal characteristics during pregnancy and risk factors for positive HIV RNA at delivery: a single-cohort observational study (Brescia, Northern Italy). [Research Support, Non-U.S. Gov’t] BMC Public Health. 2011;11:124. doi: 10.1186/1471-2458-11-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk JB, Goetz MB. Human immunodeficiency virus in an aging population, a complication of success. [Review] J Am Geriatr Soc. 2009;57(11):2129–2138. doi: 10.1111/j.1532-5415.2009.02494.x. [DOI] [PubMed] [Google Scholar]
- Kozak M, Zinski A, Leeper C, Willig JH, Mugavero MJ. Late diagnosis, delayed presentation and late presentation in HIV: proposed definitions, methodological considerations and health implications. Antivir Ther. 2013 doi: 10.3851/IMP2534. [DOI] [PubMed] [Google Scholar]
- Krawczyk CS, Funkhouser E, Kilby JM, Kaslow RA, Bey AK, Vermund SH. Factors associated with delayed initiation of HIV medical care among infected persons attending a southern HIV/AIDS clinic. [Research Support, N.I.H., Extramural] South Med J. 2006;99(5):472–481. doi: 10.1097/01.smj.0000215639.59563.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leutscher PD, Laursen T, Andersen B, Ostergaard L, Laursen A, Larsen CS. HIV late presenters in Denmark: need for increased diagnostic awareness among general practitioners. Dan Med Bull. 2011;58(4):A4253. [PubMed] [Google Scholar]
- Maccarthy S, Bangsberg D, Fink G, Reich M, Gruskin S. Late presentation to HIV/AIDS testing, treatment or continued care: clarifying the use of CD4 evaluation in the consensus definition. HIV Med. 2013 doi: 10.1111/hiv.12088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manfredi R. HIV disease and advanced age: an increasing therapeutic challenge. [Review] Drugs Aging. 2002;19(9):647–669. doi: 10.2165/00002512-200219090-00003. [DOI] [PubMed] [Google Scholar]
- Manfredi R. HIV infection and advanced age emerging epidemiological, clinical, and management issues. [Review] Ageing Res Rev. 2004;3(1):31–54. doi: 10.1016/j.arr.2003.07.001. [DOI] [PubMed] [Google Scholar]
- McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157(10):940–943. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- Metallidis S, Pilalas D, Skoura L, Haidich AB, Tsachouridou O, Papaioannou M, Nikolaidis P. Time trends and correlates of late presentation for HIV care in Northern Greece during the decade 2000 to 2010. J Int AIDS Soc. 2012;15(2):17395. doi: 10.7448/IAS.15.2.17395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mocroft A, Lundgren JD, Sabin ML, Monforte A, Brockmeyer N, Casabona J, Kirk O. Risk factors and outcomes for late presentation for HIV-positive persons in europe: results from the collaboration of observational HIV epidemiological research europe study (COHERE). [Research Support, Non-U.S. Gov’t] PLOS Med. 2013;10(9):e1001510. doi: 10.1371/journal.pmed.1001510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreira RI, Luz PM, Struchiner CJ, Morgado M, Veloso VG, Keruly JC, Moore RD. Immune status at presentation for HIV clinical care in Rio de Janeiro and Baltimore. [Comparative Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t,] J Acquir Immune Defic Syndr. 2011;57(Suppl 3):S171–178. doi: 10.1097/QAI.0b013e31821e9d59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mussini C. Late presenters: what can we do? J Int AIDS Soc. 2012;15(Suppl 4):18072. doi: 10.7448/IAS.15.6.18072. [DOI] [Google Scholar]
- O’Shea D, Ebrahim M, Egli A, Redmond D, McConkey S. Late presentation of HIV despite earlier opportunities for detection, experience from an Irish Tertiary Referral Institution. Ir J Med Sci. 2013 doi: 10.1007/s11845-012-0898-2. [DOI] [PubMed] [Google Scholar]
- Oliva J, Galindo S, Vives N, Arrillaga A, Izquierdo A, Nicolau A, Diez M. Delayed diagnosis of HIV infection in Spain. Enferm Infecc Microbiol Clin. 2010;28(9):583–589. doi: 10.1016/j.eimc.2010.02.013. [DOI] [PubMed] [Google Scholar]
- Souza PR, Jr, Szwarcwald CL, Castilho EA. Delay in introducing antiretroviral therapy in patients infected by HIV in Brazil, 2003–2006. Clinics (Sao Paulo) 2007;62(5):579–584. [PubMed] [Google Scholar]
- Tariq S, Elford J, Cortina-Borja M, Tookey PA. The association between ethnicity and late presentation to antenatal care among pregnant women living with HIV in the UK and Ireland. [Research Support, Non-U.S. Gov’t] AIDS Care. 2012;24(8):978–985. doi: 10.1080/09540121.2012.668284. [DOI] [PubMed] [Google Scholar]
- Teixeira PR, Vitoria MA, Barcarolo J. Antiretroviral treatment in resource-poor settings: the Brazilian experience. AIDS. 2004;18(Suppl 3):S5–7. doi: 10.1097/00002030-200406003-00002. [DOI] [PubMed] [Google Scholar]
- Tey JS, Ang LW, Tay J, Cutter JL, James L, Chew SK, Goh KT. Determinants of late-stage HIV disease at diagnosis in Singapore, 1996 to 2009. Ann Acad Med Singapore. 2012;41(5):194–199. [PubMed] [Google Scholar]
- Thayaparan P, Balachandran T, Kawser M. Adverse outcomes of pregnancy in HIV-positive women in the era of HAART: a perspective from an outer London centre in the UK. J Int AIDS Soc. 2012;15(6):18238. doi: 10.7448/IAS.15.6.18238. [DOI] [Google Scholar]
- Ursini T, Polilli E, Sozio F, Mazzotta E, Tontodonati M, Di Stefano P, Parruti G. Retrospective evaluation of late presentation and retention in care in a monocentric cohort of HIV-patients in 2006–2011. J Int AIDS Soc. 2012;15(6):18301. doi: 10.7448/IAS.15.6.18301. [DOI] [Google Scholar]
- Vincent A, Jonckheere S, Wilmes D, Belkhir L, Vandercam B, Yombi J. Late presentation for HIV diagnosis: a single-centre experience. J Int AIDS Soc. 2012;15(6):18368. doi: 10.7448/IAS.15.6.18368. [DOI] [Google Scholar]
- Vives N, Carnicer-Pont D, Garcia de Olalla P, Camps N, Esteve A, Casabona J. Factors associated with late presentation of HIV infection in Catalonia, Spain. Int J STD AIDS. 2012;23(7):475–480. doi: 10.1258/ijsa.2011.011280. [DOI] [PubMed] [Google Scholar]
- Wohlgemut J, Lawes T, Laing RB. Trends in missed presentations and lateHIV diagnosis in a UK teaching hospital: a retrospective comparative cohort study. BMC Infect Dis. 2012;12:72. doi: 10.1186/1471-2334-12-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zoufaly A, an der Heiden M, Marcus U, Hoffmann C, Stellbrink H, Voss L, Hamouda O. Late presentation for HIV diagnosis and care in Germany. [Multicenter Study] HIV Med. 2012;13(3):172–181. doi: 10.1111/j.1468-1293.2011.00958.x. [DOI] [PubMed] [Google Scholar]