Abstract
Background
Chronic pain can contribute to disability, depression, anxiety, sleep disturbances, poor quality of life and increased health care costs, with close to 20 % of the adult population in Europe reporting chronic pain. To empower the person to self-manage, it is advocated that education and training about the nature of pain and its effects and how to live with pain is provided. The objective of this review is to determine the level of evidence for education to facilitate knowledge about chronic pain, delivered as a stand-alone intervention for adults, to reduce pain and disability.
Methods
We identified randomised controlled trials of educational intervention for chronic pain by searching CENTRAL, MEDLINE, EMBASE and ongoing trials registries (inception to December 2013). Main inclusion criteria were (1) pain >3 months; (2) study design that allowed isolation of effects of education and (3) measures of pain or disability. Two reviewers independently screened and appraised each study.
Results
Nine studies were analysed. Pooled data from five studies, where the comparator group was usual care, showed no improvement in pain or disability. In the other four studies, comparing different types of education, there was no evidence for an improvement in pain; although, there was evidence (from one study) of a decrease in disability with a particular form of education—pain neurophysiology education (PNE). Post-hoc analysis of psychosocial outcomes reported in the studies showed evidence of a reduction in catastrophising and an increase of knowledge about pain following PNE.
Conclusions
The evidence base is limited by the small numbers of studies, their relatively small sample sizes, and the diversity in types of education studied. From that limited evidence, the only support for this type of education is for PNE, though it is insufficiently strong to recommend conclusively that PNE should be delivered as a stand-alone intervention.
It therefore remains sensible to recommend that education be delivered in conjunction with other pain management approaches as we cannot confidently conclude that education alone is effective in reducing pain intensity or related disability in chronic pain in adults.
Electronic supplementary material
The online version of this article (doi:10.1186/s13643-015-0120-5) contains supplementary material, which is available to authorized users.
Keywords: Education, Chronic pain, Physical function, Disability, Catastrophising
Background
Chronic pain can contribute to disability, depression and anxiety, sleep disturbances, poor quality of life, and increased health care costs, with close to 20 % of the adult population in Europe reporting chronic pain [1].
Chronic pain is recognised as a long-term condition in its own right or a major comorbidity of other long-term conditions. An aim of the management of all long-term conditions, embodied in the idea of self-management, is that the patient should be an active participant in the management of their own condition. In chronic pain management, such thinking is based on the assertion that “self-care and management underpins all activities in the care pathway and should be considered [at all stages]… pain management is most effective when it engages the patient in self-management” [2]. To empower the person to self-manage, it is advocated that education and training is provided about the nature of pain and its effects and how to live with pain. Responding to recommendations to establish what educational interventions in pain management work best and for whom [3] is complex not least because of the many different methods and combinations of methods of education and training that are available and in use.
The intervention being investigated in this study is education of the patient to facilitate their knowledge of chronic pain that does not include behaviour modification or training in skills of pain management.
Whilst the use of other non-pharmacological interventions can generally be informed by good quality systematic reviews of the literature (e.g. cognitive behavioural and behavioural therapy [4–6], TENS [7] and low-intensity movement therapy [6, 8]), that level of evidence is less readily available to inform the use of education to facilitate knowledge about chronic pain in adults.
Therefore, a systematic review of available studies that have evaluated the effectiveness of education to facilitate knowledge about chronic pain in adults was conducted to assess the current situation and inform future research and guidelines.
Review objectives
The primary objective was to determine the current level of evidence of the effect of education to facilitate knowledge about chronic pain for adults on pain and disability. A secondary objective was to determine (from the selected papers) the evidence of effect of the educational interventions on psychosocial outcomes.
Methods
Inclusion/exclusion criteria
Study type
Suitable for inclusion were randomised controlled trials (RCTs) and cluster-RCTs published and pre-published (electronically) in peer-reviewed journals; studies were accepted as randomised when described by the author as such. Studies were included if they were published in English. Studies were excluded if they were only available in abstract form.
Type of participants
Studies of adults (aged 18 years or older) reporting pain for at least 3 months (12 weeks) at any body-site(s) were included. Mixed age samples were included if data could be separated (adult/child). We excluded studies that were focused on specific diagnoses (e.g. osteoarthritis) and conditions where chronic pain is not necessarily the main symptom (e.g. irritable bowel syndrome), as the advice or guidance was likely to be based on the specific impact and management of the condition (e.g. joint stiffness, bowel dysfunction) at least as much as on the management of pain. We also excluded cancer-related pain.
We only included studies that focused on chronic pain, which is consistent with a strategy used in previous national guidelines [6].
Interventions
Studies were included where the effectiveness of education to facilitate knowledge about chronic pain could be assessed as a stand-alone intervention compared with usual care, or where different types of education could be compared with each other. Therefore, we excluded investigations of multi-disciplinary programmes (such as pain management programmes) which did not allow assessment of the effectiveness of the education component.
Outcome measures
Studies were included if they reported outcomes of pain severity and/or physical function.
Data collection and analysis
Electronic searches
We searched EBSCOhost [MEDLINE, CINAHL Plus, OmniFile (Full text), eBook Collection] and CENTRAL [Cochrane Central Register of Controlled Trials; MEDLINE, EMBASE, Cochrane Review Groups Specialist Registers] databases from inception to 31 December 2013. No language restrictions were imposed whilst searching; English language criterion was applied later in the process. The search strategy was developed for use in MEDLINE and adapted for each database (Additional file 1).
Other resources
Reference lists of reviews and the 22 articles reviewed in detail by all of the authors (see below) were checked for additional studies, and citation searches were performed on key articles to minimise publication bias.
Ongoing trials were searched using the World Health Organization International Clinical Trials Registry Platform (ICTRP) (http://apps.who.int/trialsearch/) and the metaRegister of Controlled Trials (mRCT) (http://www.controlledtrials.com/), which includes the ISRCTN Register (international), Action Medical Research (UK), NIH ClinicalTrials.gov Register (international), the Wellcome Trust (UK) and UK trials (UK).
Selection of studies
Following initial scanning of titles, abstracts and full papers by one author, two authors read the remaining full papers and assessed them separately. Authors independently selected studies that met the inclusion criteria using a purpose-designed checklist, limiting inclusion to studies that were randomised (or cluster-randomised) as a minimum. Further discussion was required when the authors could not reach a consensus on the studies to be included. Authors with psychological expertise reviewed the studies to remove those deemed to have formally implemented an underlying psychological therapy as part of, or including, education to facilitate knowledge about chronic pain. In this manner, 22 studies were included after screening and were then assessed by all authors. Finally, those studies that fulfilled all of the inclusion criteria were selected for analysis, a total of nine.
Data extraction and management
Data were extracted using a standardised form which included information regarding study design, participants, trial characteristics, intervention, comparison (control) and outcomes. Data were collected manually on paper extraction forms and entered into intermediate software (Microsoft Excel for Windows) before being entered in to RevMan 5.3 [9]. This intermediary stage allowed for any necessary statistical conversions. Only one pain measure was selected per study. When there were multiple measures of pain in a study, we used only the measure of average pain intensity. When there was more than one report of average pain intensity, then the mean of these was calculated. Results from visual analogues scores (VAS) were prioritised over measures such as the McGill Pain Questionnaire (MPQ) if both were reported.
Risk of bias assessment
Two authors independently assessed risk of bias for each study. Arbitration by a third author was not necessary as inconsistencies were resolved through discussion. The domain-based evaluation presented in the Cochrane Handbook for Systematic Reviews of Interventions (Chapter 8, version 5.1.0 [10]) was used to assess risk of bias. We assessed the following for each study: random sequence generation (checking for possible selection bias), allocation concealment (selection bias), blinding of patients and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias due to the amount, nature and handling of incomplete outcome data) and selective reporting (reporting bias). For “other” sources of bias, we included criteria to evaluate study sample size, where fewer than 50 participants per treatment arm was considered an increased risk of bias.
Risk of bias across all included studies was categorised according to the following:
Low risk of bias (✓) – plausible bias unlikely to seriously alter the results if most information was obtained from studies at low risk of bias
Unclear risk of bias (?) – plausible bias that raised some doubt about the results if most information was obtained from studies at low or unclear risk of bias
High risk of bias (X) – plausible bias that seriously weakens confidence in the results if the proportion of information was obtained from studies at high risk of bias sufficient to affect interpretation of results
Measurement of treatment effect
Data from included studies were reviewed separately and then, where possible, combined quantitatively by population, intervention, comparison and outcomes. Continuous data were expressed as mean difference (MD) or standardised mean difference (SMD) with 95 % confidence intervals (95 % CI); dichotomous data were reported by just one study [11] for a single outcome measure (session attendance), and this finding has been reported in the results of this review as text only.
Assessment of heterogeneity
We assessed heterogeneity according to the standard method using the Chi [2] test and the I [2] statistic, calculated for each comparison on each outcome. I [2] values above 50 % suggest high heterogeneity, 25–50 % medium heterogeneity and below 25 % low heterogeneity, though this is only used as a guide.
A standard random effects analysis was used to avoid over-weighting large studies and potentially losing small study effects.
Assessment of reporting bias
We intended to use funnel plots to assess small-study effects, following the guidance of the Cochrane Handbook of Systematic Reviews for Interventions (Chapter 10) [10], but studies were insufficient in number (n = 9) to undertake this effectively.
Data synthesis
Data were entered into RevMan 5.3 [9] by one author and checked by a second. Data were largely presented as mean and standard deviation (SD); though one study [11] reported results as mean and standard error (SE), these data were converted to mean and standard deviation using the RevMan calculator, and results were checked by hand. One study reported only average (mean) results with no measure of variation [12], and we were unable to extract plausible data for inclusion in the meta-analyses or other form of data presentation within this review.
Analysis
Studies with a comparator group of usual care were analysed separately from the studies that compared different types of education. The issues with aging and pain are more complex than simply pain being a direct correlate of biological age, though there does appear to be justification for considering pain in older people as a distinct issue [13–16]. Therefore, where data on older people (>65 years) could be extracted, these were analysed separately. Sensitivity analysis was also planned to determine if the effect size was affected by the methodological quality of the study (risk of bias). However, these analyses were not possible due to the small number of included studies.
Using the same approach as above, we also carried out post-hoc analyses of the following psychosocial variables which were reported in these studies: catastrophising, mood, knowledge of chronic pain, self-efficacy, global health and social function.
Results
Search results
Results of the search are shown in Fig. 1. Summary information of the studies included in the review is shown in Table 1.
Fig. 1.
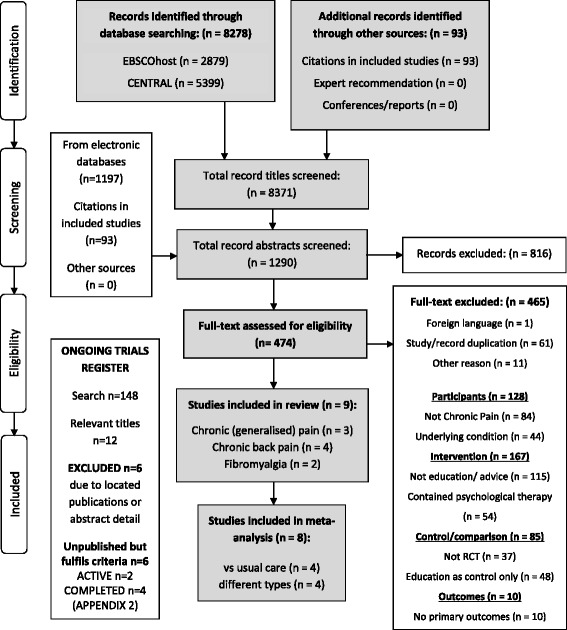
PRISMA [43] flow chart demonstrating database searches, identification, screening and selection of included studies
Table 1.
Characteristics of Included studies
| Author (year) in chronological order | Specialty | Patient eligibility and recruitment | Trial characteristics | Participant characteristics | Intervention and follow-up periods | Outcome measures reported |
|---|---|---|---|---|---|---|
| Studies assessing education versus usual care | ||||||
| Linton et al. 1997. Orebro (Sweden) | Chronic back pain | Age 18-60yrs old, accumulated sick leave for MSK pain of 2–24 weeks in the past year. Recruited via screening of insurance files, and through adverts in local newspaper | Parallel design, three arms (two interventions: “Educational support”, and “Professional support”, one control - we are not including “Professional support”). “Educational support”: patient-based support group with education, insight and empathy, used mastering pain self-help book. “Control”: regular treatment group, no additional effort to facilitate or prohibit. | “Educational support” n = 39 (74 % F), pain duration average 26 months; “Control” n = 25 (68 % F), pain duration average 26 months | “Educational support”: met for 180 min 15 times in 1 year; once/week for a month, every 2 weeks for 3 months, every other month for 5 months. Outcome measures at baseline and 1 year later | Sickness impact profile (SIP-pain), 50-item coping strategies questionnaire (CSQ), multidimensional pain inventory (MPI). Attendance, outcome evaluation questionnaire, sick leave from work. three pain beliefs and attitudes: pain and impairment relationship scale (PAIRS), Pain and discomfort scale (PADS), pain beliefs and perceptions inventory (PBPI) |
| Soares et al. 2002. Stockholm (Sweden) | Fibromyalgia | FM diagnosed in previous 2 years, female, 18–64 years, no other serious illness, no ongoing drug/alcohol abuse, not involved in other therapies. Recruited via GPs working in Stockholm area. | Parallel design, three arms (two interventions: “educational intervention” and “behavioural intervention”, one control - we are not including behavioural intervention). “educational intervention”: focus was on information about various health related topics inc the body, FM, pain, sleep hygiene, medication, managing crises, ergonomic education, self-management | All female, “educational intervention” n = 18, mean age 47 years, pain duration 50 months, “wait list control” n = 17 mean age 43 years, pain duration 37 months | “Education intervention”: two individual sessions (2 h each) and 15 group sessions (2 h each, 3–5 patients per group) for 10 weeks (total 102 h). Outcome measures at baseline, post-intervention, and 6 months later. | The pain questionnaire (PQ), the arthritis self-efficacy scale (ASES), The McGill Pain Questionnaire (MPQ), The coping strategies Questionnaire (CSQ), The Karolinska Sleep Questionnaire (KSQ), “The Diary” VAS-pain The Fibromyalgia Impact Questionnaire (FIQ), The symptom checklist - revised (SCL-90-R), The Interview Schedule of Social Support (ISSI), |
| Ruehlman et al. 2012. Arizona (USA) | Chronic pain | Over 18 yrs old, chronic pain for 6 months or more, access to computer with high speed internet, English language fluency. Recruitment via online pain sites. | Parallel design, two arms (intervention: online Chronic Pain Management Program, control: wait-list/usual care). “CPMP” has four learning modules of both online and offline activities (e.g. didactic and interactive material online, homework and self-monitoring offline), includes social networking component. | total n = 305 (196 F, 109 M), age 19–78 years mean 45 years, pain over 2 yrs in 90 % of sample, “CPMP” n = 162, “control” n = 143 | “CPMP” unsupervised access to website for 6 weeks i.e. self-directed and self-paced online program. Outcome measures at baseline, 7 weeks (i.e. post-intervention period), and at 14 weeks. | Profile of Pain: Screen (PCP-S), Centre for Epidemiological Studies Depression Scale (CES-D), Depression Anxiety and Stress Scale (DASS), pain knowledge, attitudes and beliefs: profile of pain extended assessment (PCP-EA), pain interference in functioning |
| Sparkes et al. 2012. Cardiff (UK) | Low back pain | Over 18yrs old, LBP with or without referral to the lower limbs, referred to spinal pain clinic by GP, English language fluency. Recruited via referrals sent to the spinal pain clinic. | Parallel design, two arms (intervention: The Back Book, control: usual care/wait list control). | “Back Book” n = 29 (13 M, 16 F) mean age 52 years, “control” n = 28 (11 M, 17 F) mean age 52 years | “Back Book” posted a copy of the book whilst waiting to be seen by specialist as part of referral process. Asked not to read until they had completed initial questionnaires. No follow-up letters sent which may have encourage compliance. Outcome measures at baseline (posted questionnaires after screening for inclusion/exclusion), and follow-up (at patients’ initial SPC consultation). | VAS-pain Back Beliefs Questionnaire (BBQ), Fear-avoidance beliefs questionnaire - physical activity (FABQ -PA), Roland Morris Disability Questionnaire (RMDQ), VAS-understanding of the back book |
| Excluded from analysis due to inability to extract data (Morrison et al. 1988) | ||||||
| Morrison et al. 1988. British Colombia (Canada) | chronic back pain | All (non-adolescent) patients routinely admitted to the back pain program between November 1981 and May 1982 participated. Referrals made by GPs and specialists. | Not a classic design—used sequential instead of concurrent assessment. Each group only assessed once. Attempted to strengthen study by repeated time sampling (collecting data for six different sets of patients, each with their own control group) | Mean age 45 years (range 17–74 years), n = 120 (63 % F), no individual group stats | six 3-h sessions over 2-, 3- or 6-week period: lectures and demonstrations of anatomy, physiology, body mechanics, posture, stress recognition and management, pain relief, physical exercise, and first aid techniques. Each group assessed only once; control at baseline, intervention group at the end. One year after completion, a random sample of intervention-ers (n = 28) re-assessed (physical function), and (n = 85) returned follow-up questionnaires | Oswestry Pain Scale (OPS), education - use of correct body mechanics, and patient knowledge (15-item quiz). State Anxiety Inventory (SAI). Function - strength and mobility, self-reported exercise, RAND physical abilities scale |
| Author (year) in chronological order | Specialty | Patient eligibility and recruitment | Trial characteristics | Participant characteristics | Intervention and follow-up periods | Outcome measures reported |
| Ferrell et al. 1997. California (USA) | chronic musculo-skeletal pain | Over 65 years old, presence of lower extremity pain, use of analgesics, ambulatory without assistance, English language fluency. Recruited from a Veterans Admin Medical Centre in response to info brochure mailed to home address | Parallel design, three arms (two intervention: “physical methods” and “walkers”, one control - we are not including the “walkers” intervention). “physical methods”: 90minute education session of non-drug interventions. “control”: attention control, received printed material with general info about pain and management | Mean age 73 years, “physical methods” n = 10 (3 F, 7 M), pain duration 1–53 years; “control” n = 10 (10M), pain duration 10 months–53 years | Two orientation sessions prior to intervention to educate about pain. ”physical methods” one-off education session. Outcomes measures at baseline (pre-randomisation; t1), following the two orientation sessions (t2), and 6 weeks later (t3) | Patient Pain Questionnaire (PPQ), RAND 36-item health Survey (SF-36). three performance tests: 6 min walk test, sit to stand 30, sit and reach test |
| Moseley et al. 2004. Brisbane and Sydney (Australia) | Chronic low back pain | Primary reason for presentation at pain clinic was LBP longer than 6 months. Recruited by A note advertising the project was included in the material given to patients at three private rehab clinics. | Parallel design, two arms (intervention: neurophysiology education, control: back education) | Intervention: “neurophysiology education” n = 31 (13 M, 18 F), mean age 42 years, pain duration average 29 months. Control “back education” n = 27 (12 M, 15 F), mean age 45 years, pain duration average 30 months | Both groups same format: took part in a one-off education session in 1-to-1 seminar format, each session was 3 h long with a 20 min break. Homework was a workbook in ten sections - read one section, answer three questions each weekday for 2 weeks. | Compliance. Roland Morris Disability Questionnaire (RMDQ). Survey of Pain Attitudes, revised (SOPA-R). Three physical performance measures - straight leg raise (SLR), forward bending range, abdominal drawing in task (ADIT), Pain Catastrophising Scale (PCS) |
| Gallagher et al. 2013. Adelaide and Sydney (Australia) | Chronic pain | Age 18–75 years, pain that disrupts ADLs for more than previous 3 months, English language fluency. Recruited from waiting list for multidisciplinary pain management program. | Partial (control group) cross-over design, two arms (intervention: “book of metaphors to help understand the biology of pain”, control: “advice about managing pain”, then crossed over to intervention). “book of metaphors” each section was a short story, followed by interpretation. “control/ advice booklet” each section focussed on a concept of pain management and drew heavily from the back book and manage your pain. | “metaphors” n = 40 (26 F, 14 M), age = 42 years, pain duration =25 months. “advice/control” n = 39 (22 F, 17 M), age = 45 years, pain duration = 31 months | Both groups received information in the same format—booklet of 80 pages in 11 sections. Outcome measures at baseline, and emailed questionnaires 3 weeks later, and two months after that (“12 weeks”). | Pain assessed on 11-point numerical rating scale (NRS), pain biology questionnaire (PBQ), pain catastrophising scale (PCS), disability/function—Five tasks assessed on 11-point numerical rating scale (NRS) |
| Van Oosterwijck et al. 2013. Brussels (Belgium) and Glasgow (UK) | Fibromyalgia | Age 18–65 years, FM defined by the criteria of the 1990ACR, have Dutch as native language | Parallel design, two arms (intervention: neurophysiology education, control: activity management education) | Intervention “neurophysiology” n = 15 (3 M, 12 F) age = 46 years, symptom duration = 156 months. Control “activity management” n = 15 (1 M, 14 F) age = 46 years, symptom onset = 116 months | 2 one-on-one education sessions. Intervention and control differed in content only. First session used powerpoint presentation of 30 min. Leaflet handed out. Second session 1 week later delivered by telephone. Outcome measures at baseline (pre), 2 weeks (post), and 3 months (follow-up). Additional outcome measure (PPT and neurophysiology questionnaire) also tested after first education session. | Spatial summation procedure (SSP), Health status survey (SF36), pain coping inventory (PCI), Pain Vigilance and Awareness Questionnaire (PVAQ), Tampa Scale Kinaesiophobia (TSK), pressure pain threshold (PPT) pain catastrophising scale (PCS), fibromyalgia impact questionnaire (FIQ), Neurophysiology of pain test |
Searches for ongoing trials revealed 148 trials, of which twelve titles fulfilled the inclusion criteria. From these, six were excluded after further examination of the abstract/trial registration detail or due to duplication with previously located studies. The remaining six studies have potential to be included in future updates but are currently unavailable to this review (Additional file 2).
Description of studies
Nine studies were included (Ferrell et al. 1997 [17], Gallagher et al. 2013 [18]; Linton et al. 1997 [11], Morrison et al. 1988 [12], Moseley et al. 2004 [19], Ruehlman et al. 2012 [20], Soares et al. 2002 [21], Sparkes et al. 2012 [22] and van Oosterwijck et al. 2013 [23]). In each study, all of the participants reported pain for at least 3 months. Two studies were conducted on people with fibromyalgia [21, 23], three were on people with chronic pain or chronic musculoskeletal pain [17–19], and four studies specifically examined back pain [11, 12, 19, 22]. Individual study sample size ranged from 20 [17] to 305 [20]. Participants were over the age of 18 years in all studies, though one did not specify this in the criterion [19]. There was no upper age limit in five studies [12, 17, 19, 20, 22], one of which used a sample that was exclusively over 65 years old [17]. Others excluded individuals over the age of 60 [11], 65 [21, 23] and 75 years [18].
All studies except one [23] reported the process of recruiting, which was largely through a general practitioner (GP) or specialist referrals and pain programme waiting lists. Trials were conducted in Canada [12], USA [17, 20], Sweden [11, 21], Australia [18, 19], UK [22] and in both Belgium and the UK [23].
Education to facilitate knowledge about chronic pain was in the form of lectures [12, 17, 19, 23], individual or group discussions [11, 21], written text [18, 22] or website interaction [20]. These interventions took place during a single session [17, 19, 23], numerous interactions (multiple sessions of the same format [11, 12], individual and then group sessions [21]) or with no direct contact [18, 20, 22]. Education varied in focus from understanding the neurophysiology and biology of pain [18, 19, 23] to management of symptoms through accessing physical help, such as medication, hot/cold packs, ergonomics [17, 21] and a combination of these and other topics (e.g. anatomy, physiology, body mechanics, posture, pain relief and first aid techniques [11, 12, 20, 22]).
The comparator group was usual care in five studies [11, 12, 20–22], and the other four studies compared different methods of education [17–19, 23].
The nine studies included in this review reported at least one of the primary outcome measures (Table 4). All studies except one [19] reported an assessment of pain, although there was a variety of measures used for the assessment. Physical function or disability was measured objectively in two studies using validated performance tests [17] and standardised tests for the study [12]. It was also measured subjectively (patient-reported) in a further four studies using a validated disability questionnaire (Roland Morris Disability Questionnaire) [19, 22] and validated assessment of interference or impact on daily life [11, 20].
Table 4.
Pain and disability outcome measures - post-intervention
| Outcome measure | Study | Sample size | Statistic used | Heterogeneity | Effect size | Test for overall effect | Notes | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Total | I 2 (%) | [95 % CI] | Z-value | p-value | |||||
| PAIN INTENSITY | |||||||||||
| Education versus usual care | |||||||||||
| “average pain” | Linton 1997; Soares 2002; Sparkes 2012; Ruehlman 2013 | 248 | 213 | 461 | SMD random | 0 | −0.01 | [−0.19, 0.17] | 0.12 | 0.90 | Figure 2 |
| PPQ - pain in the last week | Ferrell 1997 | 10 | 10 | 20 | MD random | n/a | −2.80 | [−21.09, 15.49] | 0.30 | 0.76 | Sample >65 years |
| Comparison of different types of education | |||||||||||
| SF36 - bodily pain | van Oosterwijck 2013 | 15 | 15 | 30 | MD random | n/a | −3.40 | [19.98, 13.18] | 0.40 | 0.69 | |
| DISABILITY | |||||||||||
| Education versus usual care | |||||||||||
| Disability or interference | Linton 1997; Ruehlman 2012; Sparkes 2012 | 230 | 196 | 426 | SMD random | 49 | 0.02 | [−0.31, 0.34] | 0.11 | 0.91 | Figure 4 |
| Comparison of different types of education | |||||||||||
| SF36 - physical function | van Oosterwijck 2013 | 15 | 15 | 30 | MD random | n/a | 5.30 | [−8.64, 19.24] | 0.75 | 0.46 | |
| Roland Morris Disability Questionnaire | Moseley 2004 | 31 | 27 | 58 | MD random | n/a | −2.00 | [−3.55, −0.45] | 2.53 | 0.01 | Favours education |
| Function and Disability (pooled data using negative RMDQ score for direct comparison) | van Oosterwijck 2013; Moseley 2004 | 46 | 42 | 88 | SMD random | 0 | 0.52 | [0.09, 0.95] | 2.38 | 0.02 | Figure 6; favours education |
| SF36 - physical function | Ferrell 1997 | 10 | 10 | 20 | MD random | n/a | 6.70 | [−9.11, 22.51] | 0.83 | 0.41 | Sample >65 years |
PPQ patient pain questionnaire, SF-36 RAND 36-item health survey, 95 % CI 95 % confidence interval, effect size represented as standardised mean difference (SMD) or mean difference (MD) depending on statistic used; Random = random effects model; heterogeneity is not applicable (n/a) when reported as single study
Excluded studies
Thirteen studies were excluded (Table 2). Three of these were excluded due to their multi-disciplinary intervention, where the effect of education alone could not be assessed [24–26]; five were excluded after assessment as having a psychological, rather than an educational content [27–31]; and three more were excluded due to inconsistency with the study design criteria [32–34].
Table 2.
Excluded studies
| Author (year) | Reason for exclusion |
|---|---|
| Burckhardt et al. 1994 | Refers to “a contract for individual behaviour change”, suggesting CBT/BT |
| Chiauzzi et al. 2010 | Second main component of website “CBT to improve self-efficacy” |
| Dirmaier et al. 2013 | Protocol only |
| Dush et al. 2006 | Mentions “psychotherapy components were tailored to patient’s needs”, suggesting psychotherapy in addition to education |
| Dworkin et al. 2002 | Involves relaxation and coping skills training |
| Haas et al. 2005 | Uses Stanford Self-management model (multi-disciplinary, unable to assess educational component alone) |
| Harpole et al. 2003 | Includes detailed clinical assessment and tailored treatment plan |
| Jerjes et al. 2007 | Pilot study, non-randomised |
| LeFort et al. 1998 | Uses Stanford Self-management model (multi-disciplinary, unable to assess educational component alone) |
| Matchar et al. 2008 | Includes diagnosis and treatment as part of the programme |
| Michelotti et al. 2012 | Focus on “habit reversal” (psychological intervention) and includes a large physiotherapy (exercise) component (multi-disciplinary, unable to assess educational component alone) |
| Van Ittersum et al. 2011 | No control group |
| Vlaeyen et al. 1996 | Includes physical exercise at the end of each session, therefore, cannot distinguish effect of education or exercise |
Risk of bias in included studies
Low or unclear/uncertain risk was identified across the majority of the six domains. Risk of bias for each included study is shown in Table 3.
Table 3.
Risk of bias summary showing the review authors’ judgements about each methodological quality item for each included study
| Selection bias | Performance bias | Detection bias | Attrition bias | Reporting bias | Other bias | Total | ||
|---|---|---|---|---|---|---|---|---|
| Author (year) In chronological order |
Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | Other (eg. sample size) | No. of low risk of bias (✓) |
| Morrison et al. 1988 | ? | ? | ? | X | ? | ? | ? | 0 |
| Ferrell et al. 1997 | ? | ? | ? | ✓ | ✓ | ? | x | 2 |
| Linton et al. 1997 | ✓ | ✓ | ? | ? | ✓ | ? | ? | 3 |
| Soares et al. 2002 | x | x | ✓ | ✓ | ✓ | ? | x | 3 |
| Moseley et al. 2004 | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ? | 5 |
| Ruehlman et al. 2012 | ? | ? | ✓ | ✓ | ✓ | ? | ✓ | 4 |
| Sparkes et al. 2012 | ✓ | ? | ✓ | ✓ | ✓ | ? | ? | 4 |
| Gallagher et al. 2013 | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✓ | 6 |
| Van Oosterwijck et al. 2013 | ✓ | ✓ | ✓ | ✓ | ✓ | ? | X | 5 |
| No. of studies with low risk of bias - ✓ | 5 | 4 | 6 | 7 | 8 | 0 | 2 | |
| No. of studies with uncertain/unclear - ? | 3 | 4 | 3 | 1 | 1 | 9 | 4 | |
| No. of studies with high risk of bias—X | 1 | 1 | 0 | 1 | 0 | 0 | 3 | |
(✓) is low risk of bias, (X) high risk of bias, (?) unclear or uncertain
Selection bias (random sequence generation and allocation concealment)
Four studies fulfilled both criteria for low risk of bias [28, 32, 33, 35], and one fulfilled one of the two criteria [36]. Three studies mentioned that the participants were randomised and allocation-concealed but did not specify the method constituting an unclear risk of bias [29, 31, 34]. One study described itself as randomised, but patients were “consecutively allocated” to each group and so held a high risk of bias [37].
Performance bias (blinding of participants and personnel)
All of the most recent studies [32–37] showed low risk of bias and reported blinding of participants and personnel where necessary. Earlier publications [28, 29, 31] did not mention blinding.
Detection bias (blinding of outcome assessment)
In five studies, there was no blinding of outcome assessments [31–34, 36], but the review authors judged that the outcome measure was unlikely to be influenced by this knowledge as questionnaires were completed alone by the participant. Two studies reported blinding for outcome measures [35, 37], only one of which reported assessing the success of blinding of both the participants and personnel [35]. The study by Morrison et al. [29] was labelled high risk of bias as each group was only assessed once (the control group at pre-intervention, and treatment group post-intervention only).
Attrition bias (incomplete outcome data)
Dropouts and withdrawals were noted and explained in all studies (low risk of bias) except one where there was no mention of incomplete data [29].
Reporting bias (selective reporting)
No published protocols were found, and so we cannot say with absolute certainty that all outcome measures were reported, and all included studies were therefore awarded an unclear/uncertain risk of bias.
Other potential sources of bias
Study size was assessed as an additional risk of bias, as a small study size could bias the results. The methods specified that fewer than 50 participants per treatment arm would be an increased risk of bias as seen in all but two studies (low risk of bias n = 79 after crossover from control [32], n = 162 [34]). The remaining seven studies were further separated into those with fewer than 20 participants in the treatment group as high risk of bias in three studies (n = 10 [31], n = 18 [37], n = 15 [35]), uncertain risk for those where n ~ 30 in the treatment group [28, 33, 36] and unclear risk for one study [29] that reported no separate treatment/control sample size.
Intervention effect
Table 5.
Pain and disability outcome measures - follow-up
| Outcome measure | Study | Sample size | Statistic used | Heterogeneity | Effect size | Test for overall effect | Notes | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Total | I 2 (%) | [95 % CI] | Z-value | p-value | |||||
| PAIN INTENSITY | |||||||||||
| Education versus usual care | |||||||||||
| “average pain” | Soares 2002; Ruehlman 2013 | 18 | 17 | 35 | SMD random | 0 | 0.02 | [−0.19, 0.24] | 0.21 | 0.83 | Figure 3 |
| Comparison of different types of education | |||||||||||
| SF36 - bodily pain | van Oosterwijck 2013 | 15 | 15 | 30 | MD random | n/a | −9.90 | [−24.73, 4.93] | 1.31 | 0.19 | |
| PPQ - pain in the last week | Ferrell 1997 | 10 | 10 | 20 | MD random | n/a | −6.50 | [−22.94, 9.94] | 0.78 | 0.44 | Sample >65 years |
| DISABILITY | |||||||||||
| Education versus usual care | |||||||||||
| PCP-S - interference | Ruehlman 2012 | 162 | 143 | 305 | MD random | n/a | 0.46 | [−1.46, 2.38] | 0.47 | 0.64 | Figure 5 |
| comparison of different types of education | |||||||||||
| SF36 - physical function | van Oosterwijck 2013 | 15 | 15 | 30 | MD random | n/a | 8.40 | [−4.27, 21.07] | 1.30 | 0.19 | Figure 7 |
| SF36 - physical function | Ferrell 1997 | 10 | 10 | 20 | MD random | n/a | −1.80 | [−15.71, 12.11] | 0.25 | 0.80 | Sample >65 years |
PCP-S profile of chronic pain-screening, PPQ patient pain questionnaire, SF-36 RAND 36-item health survey, 95 % CI 95 % confidence interval; Effect size represented as standardised mean difference (SMD) or mean difference (MD) depending on statistic used; Random = random effects model; heterogeneity is not applicable (n/a) when reported as single study
Education versus usual care
Adults >18 years: All four studies measured pain at the post-intervention measurement point [11, 20–22], and two of these studies also reported follow-up assessments [20, 21].
None of the studies showed significant effects post-intervention. Pooling the data of all four studies showed low heterogeneity (I [2] = 0 %), and the effect size was small and statistically non-significant (Fig. 2). In neither of the two studies reporting results around 3 months after the end of the intervention was there a significant effect. Again, pooling of the data showed a small effect size that was not statistically significant (Fig. 3).
Fig. 2.
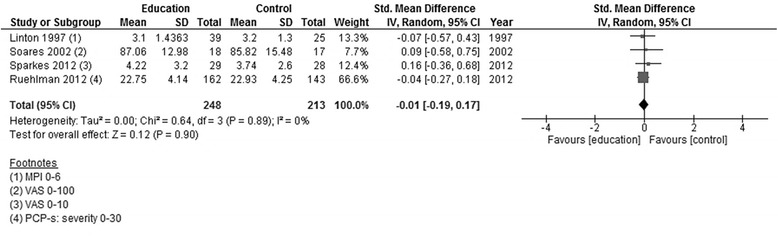
Forest plot showing pain intensity (education versus usual care)—post-intervention
Fig. 3.
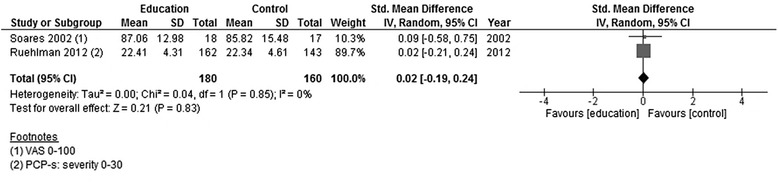
Forest plot showing pain intensity (education versus usual care)—follow-up (3 months)
Adults >65 years: No specific data were available.
Comparison of different types of education
Adults >18 years: Measures of average pain could only be extracted from one study [23]. In this study, which used a very small sample size to compare pain neurophysiology education (PNE) with another form of information provision, there were no statistically significant differences in average pain intensity between the two forms of information provision 2 weeks after the intervention period or 3 months after the intervention ended.
Adults >65 years: One study exclusively investigated adults aged >65 years [17]. The study, which had a very small sample size, found no significant differences between information provision about pain and information provision about physical methods to reduce pain immediately after the intervention period or 6 weeks after completion.
Education versus usual care
Adults >18 years: Disability was assessed in three out of the four studies post-intervention [11, 20, 22]. Only one of the studies had a follow-up assessment, reporting results at 3 months from the end of the intervention [20].
There were no significant effects on disability in any of the studies immediately after the end of the intervention. When data were pooled, heterogeneity was high amongst these studies (I [2] = 49 %), and the overall effect size was low (Z = 0.11) and statistically non-significant (Fig. 4). The single study that assessed disability at 3 months following the end of the intervention showed no significant differences in disability between groups (Fig. 5).
Fig. 4.

Forest plot showing disability (education versus usual care)—post-intervention
Fig. 5.

Forest plot showing disability (education versus usual care)—follow-up (3 months)
Adults >65 years: No specific data were available.
Comparison of different types of education
Adults >18 years: Disability was assessed in two studies, both of which compared pain neurophysiological education (PNE) with other information provision types [19, 23]. Only one study contained a follow-up assessment at 3 months following the end of the intervention; this study used a very small sample size [23].
PNE showed a significantly better effect than its comparator on the Roland Morris Disability Questionnaire (RMDQ) scores immediately after the intervention in one study [19]. In the other study, which had a very small sample size [23], the mean difference in favour of PNE (5.3 points on the SF36 physical function subscale 2 weeks after the intervention had ended) was not statistically significant. Pooling the data from both studies showed low heterogeneity (I [2] = 0 %), and there was a statistically significant difference in favour of PNE (Fig. 6).
Fig. 6.
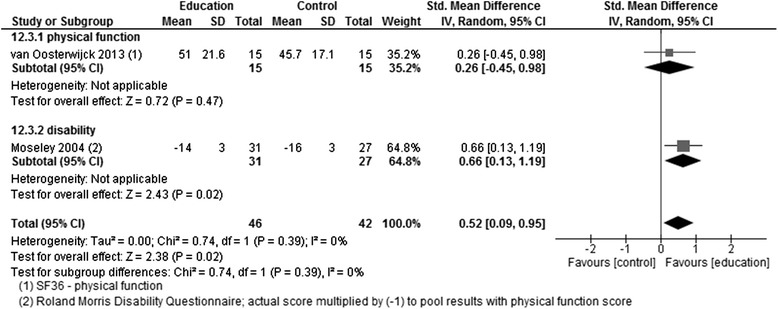
Forest plot showing disability and physical function (comparison of different types of education)—post-intervention
In the study [23] that contained a follow-up assessment (3 months after the intervention had ended), there was a mean difference of 8.4 points on the SF36 physical function subscale (range 0–100) in favour of PNE, which was not statistically significant (Fig. 7).
Fig. 7.
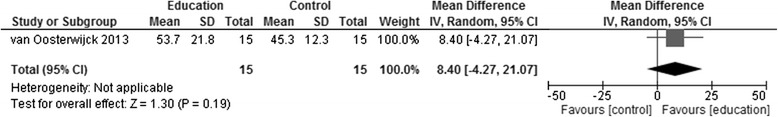
Forest plot showing disability (comparison of different types of education)—follow-up (3 months)
Adults >65 years: The one study exclusively investigating older adults (>65 years) used a very small sample size [17]. There were no significant differences between education about pain and education about physical methods to reduce pain either immediately after the intervention period or 6 weeks from its end.
Table 6.
Psychosocial outcome measures - post-intervention
| Outcome measure | Study | Sample size | Statistic used | Heterogeneity | Effect size | Test for overall effect | Notes | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Total | I 2 (%) | [95 % CI] | Z-value | p-value | |||||
| CATASTROPHISING | |||||||||||
| Education versus usual care | |||||||||||
| CSQ – catastrophising PCP (EA) - catastrophising |
Linton 1997; Soares 2002; Ruehlman 2012 | 219 | 185 | 404 | SMD random | 0 | −0.08 | [−0.28, 0.12] | 0.79 | 0.43 | Figure 8 |
| Comparison of different types of education | |||||||||||
| Pain catastrophising scale (PCS) | Moseley 2004; van Oosterwijck 2013; Gallagher 2013 | 86 | 81 | 167 | SMD random | 48 | −0.81 | [−1.27, −0.35] | 3.47 | 0.0005 | Figure 10; favours education |
| SELF-EFFICACY | |||||||||||
| Education versus usual care | |||||||||||
| CSQ - self efficacy | Soares 2002 | 18 | 17 | 35 | MD random | n/a | 0.47 | [−0.83, 1.77] | 0.71 | 0.48 | |
| KNOWLEDGE OF PAIN | |||||||||||
| Comparison of different types of education | |||||||||||
| Pain biology/neuro-physiology knowledge | Gallagher 2013; van Oosterwijck 2013 | 55 | 54 | 109 | MD random | 0 | 3.86 | [2.44, 5.28] | 5.34 | <0.00001 | Figure 12; favours education |
| Knowledge and attitude score | Ferrell 1997 | 9 | 9 | 18 | MD random | n/a | 34.10 | [23.22, 44.98] | 6.14 | <0.00001 | Sample >65 years |
| GLOBAL HEALTH | |||||||||||
| Comparison of different types of education | |||||||||||
| SF36 - general health perceptions | van Oosterwijck 2013 | 15 | 15 | 30 | MD random | n/a | −0.50 | [−11.07, 10.07] | 0.09 | 0.93 | |
| SF36 - overall health rating | Ferrell 1997 | 10 | 10 | 20 | MD random | n/a | −16.20 | [−31.56, −0.84] | 2.07 | 0.04 | Favours control |
| MOOD | |||||||||||
| Education versus usual care | |||||||||||
| DASS – depression | Ruehlman 2012 | 162 | 143 | 305 | MD random | n/a | −0.26 | [−1.51, 0.99] | 0.41 | 0.68 | |
| Comparison of different types of education | |||||||||||
| SF36 - mental health | van Oosterwijck 2013 | 15 | 15 | 30 | MD random | n/a | 13.40 | [−1.24, 28.04] | 1.79 | 0.07 | |
| SOCIAL FUNCTION | |||||||||||
| Comparison of different types of education | |||||||||||
| SF36 – social function | van Oosterwijck 2013 | 15 | 15 | 30 | MD random | n/a | 8.90 | [−8.16, 25.96] | 1.02 | 0.31 | |
SF-36 RAND 36-item health survey, DASS depression, anxiety and stress scale, CSQ coping strategies questionnaire, PCS pain catastrophising scale, CSQ coping strategies questionnaire, PCP (EA) profile of chronic pain (Extended Assessment), 95 % CI 95 % confidence interval; Effect size represented as standardised mean difference (SMD) or mean difference (MD) depending on statistic used; Random = random effects model; heterogeneity is not applicable (n/a) when reported as single study
Table 7.
Psychosocial outcome measures - follow-up
| Outcome measure | Study | sample size | Statistic used | Heterogeneity | Effect size | Test for overall effect | Notes | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | Total |
I
2
(%) |
[95 % CI] | Z-value | p-value | |||||
| CATASTROPHISING | |||||||||||
| Education versus usual care | |||||||||||
| CSQ – catastrophising PCP (EA) - catastrophising |
Soares 2002; Ruehlman 2012 | 177 | 160 | 337 | SMD random | 0 | −0.09 | [−0.30, 0.13] | 0.79 | 0.43 | Figure 9 |
| Comparison of different types of education | |||||||||||
| Pain catastrophising scale (PCS) | van Oosterwijck 2013; Gallagher 2013 | 55 | 54 | 109 | SMD random | 0 | −0.87 | [−1.26, −0.47] | 4.31 | <0.0001 | Figure 11; favours education |
| KNOWLEDGE OF PAIN | |||||||||||
| comparison of different types of education | |||||||||||
| Pain biology/neuro-physiology knowledge | Gallagher 2013; van Oosterwijck 2013 | 55 | 54 | 109 | MD random | 0 | 3.69 | [2.22, 5.17] | 4.90 | <0.00001 | Figure 13; favours education |
| knowledge and attitude score | Ferrell 1997 | 9 | 9 | 18 | MD random | n/a | 24.10 | [9.15, 39.05] | 3.16 | 0.002 | Sample >65 years |
| GLOBAL HEALTH | |||||||||||
| Comparison of different types of education | |||||||||||
| SF36 - general health perceptions | van Oosterwijck 2013 | 15 | 15 | 30 | MD random | n/a | 9.10 | [−1.07, 19.27] | 1.75 | 0.08 | |
| SF36 - overall health rating | Ferrell 1997 | 10 | 10 | 20 | MD random | n/a | 5.60 | [−9.73, 20.93] | 0.72 | 0.47 | Sample >65 years |
| MOOD | |||||||||||
| Education versus usual care | |||||||||||
| DASS – depression | Ruehlman 2012 | 162 | 143 | 305 | MD random | n/a | 0.36 | [−0.99, 1.71] | 0.52 | 0.60 | |
| Comparison of different types of education | |||||||||||
| SF36 - mental health | van Oosterwijck 2013 | 15 | 15 | 30 | MD random | n/a | 18.20 | [5.39, 31.01] | 2.78 | 0.005 | Favours education |
| SOCIAL FUNCTION | |||||||||||
| Comparison of different types of education | |||||||||||
| SF36 – social function | van Oosterwijck 2013 | 15 | 15 | 30 | MD random | n/a | −3.10 | [−19.13, 12.93] | 0.38 | 0.70 | |
SF-36 RAND 36-item health survey, DASS depression, anxiety and stress scale, CSQ coping strategies questionnaire, PCS pain catastrophising scale, CSQ coping strategies questionnaire, PCP (EA) profile of chronic pain (Extended Assessment); 95 % CI 95 % confidence interval; Effect size represented as standardised mean difference (SMD) or mean difference (MD) depending on statistic used; Random = random effects model; heterogeneity is not applicable (n/a) when reported as single study
Education versus usual care
Adults >18 years: Catastrophising was assessed in three of the four studies post-intervention [11, 20, 21]. Two had a follow-up assessment at 3 months from the end of the intervention [20, 21]. There was no effect, post-intervention, in any of the studies individually or when the data were pooled (Fig. 8), nor was there an effect at follow-up (Fig. 9). One study measured self-efficacy, only at post-intervention, and showed no effect [21]. Depression was measured in one study, and there were no changes post-intervention or at follow-up [20].
Fig. 10.

Forest plot showing catastrophising (comparison of different types of education)—post-intervention
Fig. 11.
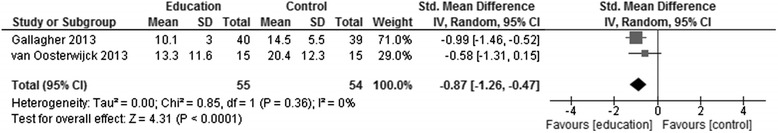
Forest plot showing catastrophising (comparison of different types of education)—follow-up (3 months)
Fig. 12.
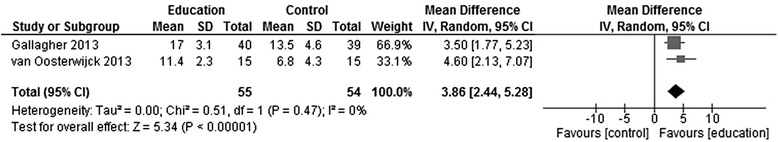
Forest plot showing knowledge of pain (comparison of different types of education)—post-intervention
Fig. 13.
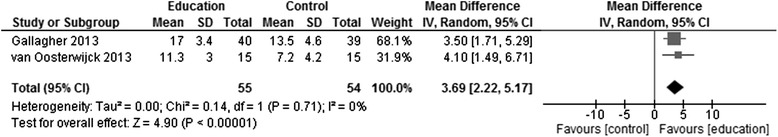
Forest plot showing knowledge of pain (comparison of different types of education)—follow-up (3 months)
Fig. 8.
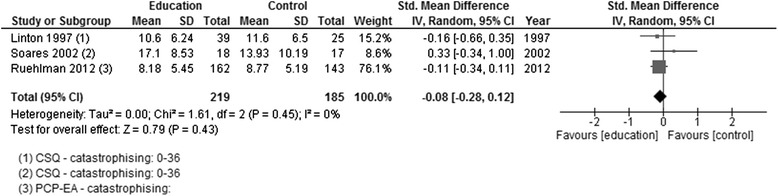
Forest plot showing catastrophising (education versus usual care)—post-intervention
Fig. 9.
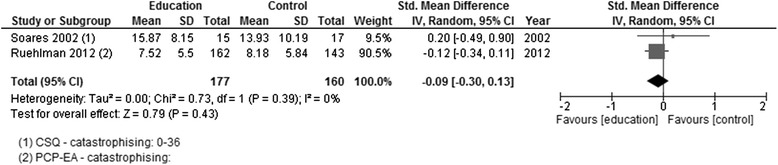
Forest plot showing catastrophising (education versus usual care)—follow-up (3 months)
Adults >65 years: One study carried out a bespoke measure of participants’ knowledge about pain and reported a significant improvement, post-intervention and at follow-up, in favour of the intervention [17].
Comparison of different types of education
Adults >18 years: Catastrophising was assessed in each of the three studies post-intervention [18, 19, 23], with two providing follow-up data [18, 23]. In each study and in the pooled data, there was a positive effect in favour of PNE at both assessment times (Fig. 6a, b). Two of the three studies assessed knowledge of pain post-intervention and at follow-up [18, 23]. A positive effect in pooled data in favour of PNE reflected the positive effects in both studies post-intervention and at follow-up (Fig. 7a, b). Only one of the studies assessed other relevant outcomes—mood, global health and social function [23]. For mood, there were positive effects post-intervention in favour of PNE, which did not reach statistical significance (p > 0.05) but did so at follow-up. There were no significant effects in global health or social function at either measurement point.
Adults >65 years: No specific data were available.
Discussion
We systematically reviewed RCTs that investigated the effects of education to facilitate knowledge of chronic pain in adults on pain intensity and disability. Our analysis of the nine studies that fit the inclusion criteria found no evidence of an effect on pain intensity. However, for disability, there was evidence of a significant improvement immediately following a course of a particular type of education—pain neurophysiology education (PNE). Such an effect was not seen for the other types of education investigated in the studies.
Only one study specifically looked at people over 65 years old, also showing no significant effect on pain or disability.
Other reviews have been published in the past 5 years examining education for cancer pain [37], PNE for chronic musculoskeletal pain [36], PNE for chronic low back pain [35], education for neck pain [38, 39], educational interventions by pharmacists for chronic pain [40] and knowledge translation for chronic non-cancer pain management [41]. This last review included interventions aimed at health professionals, patients and a combination of target groups. Of these reviews, only three were able to combine studies to perform some meta-analyses within their reviews [35, 38, 40], whilst others reported results in the narrative.
Pain severity/intensity
As in the current review, educational interventions had no significant impact on pain severity or intensity in whiplash-associated disorders (neck pain [38]) and no clinical significance in chronic low back pain [35], though it was shown to be significantly effective in reviews of education in cancer pain [37] and chronic musculoskeletal pain [38]. The variation in results with regards to the change (or lack thereof) in pain intensity may largely be due to the nature of the patient population (cancer patients [37]) or the intervention itself (multi-disciplinary approach combining education with physiotherapy or cognition-targeted motor control training [38]).
Disability/physical function
Other reviews [35, 38] have not revealed significant change in levels of disability and function, consistent with the present review.
Conversely, Louw et al. [38] described a significant effect from education in those with musculoskeletal pain. Included in that review [38] was the one study in the present review that showed a significant improvement in disability as a result of the intervention [19], and others by the same research team (five out of eight trials), potentially skewing the results of the review to reflect this one intervention. The review of knowledge translations targeting patients showed short-term improvements in patient function with chronic low back pain, but no change in migraine-related complaints [41], suggesting as we have in the inclusion and exclusion criteria of the present review that underlying conditions (such as migraine) should be treated and analysed separately to other manifestations of chronic pain.
Psychosocial outcomes
The most interesting findings were the significant improvements in catastrophising and knowledge of pain. The improvements in catastrophising were only found in those studies that utilised pain neurophysiological education (PNE) in the intervention. This fits with one of the primary aims of PNE, to reconceptualise thinking about pain, away from the belief that “hurt” always equates to “physical harm”. The change in knowledge about pain, which were also seen with PNE, also point towards achievement of this primary aim. However, the design of the studies and reliance on questionnaire findings do not allow the depth of investigation needed to fully explore this suggestion, and appropriate qualitative investigation is called for. Interestingly, knowledge of pain was found to increase in the single study on older people exclusively [17] (not using PNE). This suggests that such an aim (to reconceptualise thinking) is not limited by older age. However, the measurement used in the study was very superficial, and again, the most appropriate action would be to explore this in more depth.
This review was conducted using the most robust techniques available. Electronic searches included full access to four databases (MEDLINE, CINAHL Plus, EMBASE and CENTRAL [Cochrane Central Register of Controlled Trials]), alongside international trial registries and author personal libraries. In total, 8519 titles were assessed for inclusion (8371 of published papers, 148 from ongoing trial registry). The review summarises the highest quality evidence available using RCTs of reasonable quality. The use of meta-analytical methods to pool data from different studies, which had relatively small individual sample sizes, maximised the strength of the findings.
The search was undertaken from database inception until 31 December 2013, and all data were extracted and analysed within 6 months of this date. The resources available prevent us from updating and re-analysing the search, and we are unable to examine the effect that any subsequent studies may have on our findings. This is an area for ongoing research, which will be supported by our included list of ongoing trials noted at the time of our analysis.
The review was limited by the small number of studies suitable for analysis, reflecting the availability of relevant published studies. This meant that findings were based on relatively low sample sizes, although this was overcome to an extent by pooling of data where appropriate. Because of the small numbers available, we were not able to carry out subgroup analyses to assess the influence of study quality on outcomes nor were we able to comprehensively assess the influence of older age.
The scope of the review was deliberately restricted to investigate education in isolation from other interventions, and care should therefore be taken when extrapolating the findings to the use of education delivered in combination with other interventions. However, there is room for future study of the additive effects of education in combination with other approaches to pain management.
We also used outcomes of pain intensity and disability as inclusion criteria. Therefore, in our post-hoc analysis of psychosocial outcomes, it is likely that we have excluded evidence from studies that used such measures but did not measure pain or disability; other sources of evidence should be used to make judgement on the effect of education on other outcomes such as mood, coping strategies and pain beliefs, all of which can be important in pain management.
We did not contact authors for further information and excluded papers that were not available in English at the full-text stage only. Both of these decisions were largely made as a result of the resources available to us. However, the need to contact authors only occurred in the case of a single paper [12], where details were lacking regarding group sample sizes, and no variation around the mean was reported. We decided we were unlikely to receive a response due to the considerable time period since publication (1988), and as a result, the paper was excluded from the meta-analyses. Only one paper [42] was excluded due to the language (Fig. 1), and we are unable to judge the effect of this exclusion on our results.
As highlighted by the small number of studies and the diverse range of educational methods that have been used in the current literature base, there is a general need for more high quality trials in this area. The specific findings for PNE, in this review and in others, should stimulate research to see how its promise can be optimised to further improve its effects, perhaps by comparing different methods of delivery and tailoring its content to specific populations including older people.
One study [28] compared two different modes of delivery (website versus written material), though it was excluded due to the large cognitive behavioural therapy (CBT) component delivered through the website. Equivalent research examining mode of delivery would be of interest to further examine whether online delivery of an educational intervention, for example, is equally effective across all age groups or whether it is the group element compared to individual learning that has the greatest influence on effect size.
The wide variety of assessments available for this review meant that a great deal of analysis was not possible due to the variability of the focus of the assessments or when subscales were not reported. Future meta-analyses could be improved through the standardisation of outcome measures.
Further, the effect of education on psychosocial variables as mediators of pain and disability remains to be elucidated. Research to investigate the effect of education upon knowledge and its relationship to psychosocial mediators is warranted.
Finally, a long-term follow-up should be implemented for all studies, as short-term results whilst promising, do not necessarily suggest long-term effect.
Conclusions
Of the different forms of education reported in RCTs, only PNE appears to be effective (by reducing disability) as a sole intervention for adults with chronic pain and only immediately after the intervention. However, the evidence is too limited to conclusively rule out other options.
Practical implications
Education to facilitate knowledge of chronic pain in adults remains a potentially important part of patient activation. Certainly, for people with established chronic pain (as represented by the studies reviewed here), it would be sensible to include education along with other interventions as there is little evidence to support education as a stand-alone intervention. Whilst research findings continue to emerge, clinicians should consider incorporating PNE, though it would be premature to discard other options. However, we cannot confidently conclude that education alone is effective in reducing pain intensity or related disability in chronic pain in adults.
Acknowledgements
This review was supported through wider project funding from the MRC, Lifelong Health and Wellbeing Grant, ID 91029, UK.
Abbreviations
- CBT
cognitive behavioural therapy
- CI
confidence interval
- GP
general practitioner
- ICTRP
International Clinical Trial Registry Platform
- MD
mean difference
- MPQ
McGill Pain Questionnaire
- PNE
pain neurophysiology education
- RCT
randomised controlled trial
- RMDQ
Roland Morris Disability Questionnaire
- SD
standard deviation
- SE
standard error
- SMD
standardised mean difference
- TENS
transcutaneous electrical nerve stimulation
- VAS
visual analogue scores
- WHO
World Health Organisation
Additional files
Search strategy. (DOCX 13 kb)
Ongoing (unpublished) trials. (DOCX 16 kb)
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
LJG developed the research question, definition of participants, intervention, comparisons and outcomes; developed and implemented search strategy in various databases; undertook hand-searching of reference lists, conference proceedings, ongoing trials; assessed titles; located and assessed abstracts; located and accessed full papers of potential studies; assessed full papers for inclusion (participants, intervention, comparison, outcomes); quality assessed included reviews; extracted data in included reviews; performed necessary statistical conversions; analysed the data; interpreted the results; wrote draft review and is the main contact person. DM developed research question; developed definition of participants, intervention, comparisons and outcomes; assessed full papers for correct intervention (education only); performed necessary statistical conversions; analysed the data; interpreted the results and helped re-draft the review. NA assessed full papers for the correct intervention (to exclude psychological therapies only) and approved the final draft of the review. CC developed the research question; assessed full papers for inclusion (participants, intervention, comparison, outcomes); quality assessed included reviews and approved the final draft of the review. MD developed the research question; developed definition of participants, intervention, comparisons and outcomes; assessed full papers for correct intervention (to exclude psychological therapies only); analysed the data; interpreted the results and approved final draft of review. BHS initiated concept of the review; developed the research question; developed definition of participants, intervention, comparisons and outcomes; assessed full papers for inclusion (participants, intervention, comparison, outcomes); interpreted the results and approved the final draft of the review. DJ, PMcN, PS approved the final draft of the review. All authors read and approved the final manuscript.
Contributor Information
Louise J. Geneen, Phone: (+44) 01382 383191, Email: l.geneen@dundee.ac.uk
Denis J. Martin, Email: d.martin@tees.ac.uk
Nicola Adams, Email: Nicola.adams@northumbria.ac.uk.
Clare Clarke, Email: c.z.clarke@dundee.ac.uk.
Martin Dunbar, Email: martin.dunbar@ggc.scot.nhs.uk.
Derek Jones, Email: derek.jones45@yahoo.co.uk.
Paul McNamee, Email: p.mcnamee@abdn.ac.uk.
Pat Schofield, Email: p.a.schofield@greenwich.ac.uk.
Blair H. Smith, Email: b.h.smith@dundee.ac.uk
References
- 1.Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10(4):287–333. doi: 10.1016/j.ejpain.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 2.British Pain Society Map of Medicine. 2013. Available at: http://www.cambsphn.nhs.uk/Libraries/Pain_Management_-_Pthwys_Gdnce/neuropathic_pain_British_pain_society_1.sflb.ashx. Accessed September 20, 2014.
- 3.NICE. Low back pain | 4-research-recommendations | Guidance and guidelines. Natl Inst Heal Care Excell. 2009;CG88. Available at: https://www.nice.org.uk/guidance/cg88/chapter/4-research-recommendations#delivery-of-patient-education. Accessed October 15, 2014.
- 4.Williams A, Eccleston C, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults (Review). Cochrane Database Syst Rev. 2013;(2). doi:10.1002/14651858.CD007407.pub3. [DOI] [PMC free article] [PubMed]
- 5.Eccleston C, Fisher E, Craig L, Duggan R, Keogh E. Psychological therapies (internet delivered) for the management of chronic pain in adults (Protocol). Cochrane Database Syst Rev. 2013;7. [DOI] [PMC free article] [PubMed]
- 6.SIGN 136: Management of chronic pain. 2013.
- 7.Nnoaham K, Kumbang J. Transcutaneous electrical nerve stimulation (TENS) for chronic pain. Cochrane Database Syst Rev. 2008;(3):Art. No.: CD003222. doi:10.1002/14651858.CD003222.pub2. [DOI] [PubMed]
- 8.Wieland L, Skoetz N, Manheimer E, Pilkington K, Vempati R, Berman B. Yoga treatment for chronic non-specific low-back pain [Protocol]. Cochrane Database Syst Rev. 2013;(7):Art. No.: CD010671. doi:10.1002/14651858.CD010671. [DOI] [PMC free article] [PubMed]
- 9.Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration; 2014. [Google Scholar]
- 10.Higgins J, Green S. The Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0 edition. The Cochrane Collaboration, 2011; 2011.
- 11.Linton S, Hellsing A, Larsson I. Bridging the Gap: support groups do not enhance long-term outcome in chronic back pain. Clin J Pain. 1997;13(3):221–8. doi: 10.1097/00002508-199709000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Morrison G, Chase W, Young V, Roberts W. Back pain: treatment and prevention in a community hospital. Arch Phys Med Rehabil. 1988;69:605–9. [PubMed] [Google Scholar]
- 13.Gagliese L. Pain and aging: the emergence of a new subfield of pain research. Pain. 2009;10(4):243–53. doi: 10.1016/j.jpain.2008.10.013. [DOI] [PubMed] [Google Scholar]
- 14.Elliott AM, Smith BH, Penny KI, Smith WC, Chambers WA. The epidemiology of chronic pain in the community. Lancet. 1999;354(9186):1248–52. Available at: http://www.ncbi.nlm.nih.gov/pubmed/10520633. Accessed November 14, 2013. [DOI] [PubMed]
- 15.Abdulla A, Adams N, Bone M, et al. Guidance on the management of pain in older people. Age Ageing. 2013;42(Suppl 1):i1–57. doi: 10.1093/ageing/afs200. [DOI] [PubMed] [Google Scholar]
- 16.Schofield P, Clarke A, Jones D, Martin D, McNamee P, Smith B. Chronic pain in later life: a review of current issues and challenges. Ageing Heal. 2011;7(4):1–7. [Google Scholar]
- 17.Ferrell B, Josephson K, Pollan A, Ferrell B. A randomised trial of walking versus physical methods for chronic pain management. Aging Clin Exp Res. 1997;9(1/2):99–105. doi: 10.1007/BF03340134. [DOI] [PubMed] [Google Scholar]
- 18.Gallagher L, McAuley J, Moseley GL. A randomized-controlled trial of using a book of metaphors to reconceptualize pain and decrease catastrophizing in people with chronic pain. Clin J Pain. 2013;29(1):20–5. doi: 10.1097/AJP.0b013e3182465cf7. [DOI] [PubMed] [Google Scholar]
- 19.Moseley GL, Nicholas MK, Hodges PW. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin J Pain. 2004;20(5):324–30. doi: 10.1097/00002508-200409000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Ruehlman L, Karoly P, Enders C. A randomized controlled evaluation of an online chronic pain self management program. Pain. 2012;153(2):319–30. doi: 10.1016/j.pain.2011.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Soares JJF, Grossi G. A randomized, controlled comparison of educational and behavioural interventions for women with fibromyalgia. Scand J Occup Ther. 2002;9:35–45. doi: 10.1080/110381202753505845. [DOI] [Google Scholar]
- 22.Sparkes V, Chidwick N, Coales P. Effect of The Back Book on fear-avoidance beliefs, disability, and pain levels in subjects with low back pain. Int J Ther Rehabil. 2012;19(2):79–86. doi: 10.12968/ijtr.2012.19.2.79. [DOI] [Google Scholar]
- 23.Van Oosterwijck J, Meeus M, Paul L, et al. Pain physiology education improves health status and endogenous pain inhibition in fibromyalgia. Clin. 2013;29(10):873–82. doi: 10.1097/AJP.0b013e31827c7a7d. [DOI] [PubMed] [Google Scholar]
- 24.Haas M, Groupp E, Muench J, et al. Chronic disease self-management program for low back pain in the elderly. J Manipulative Physiol Ther. 2005;28(4):228–37. doi: 10.1016/j.jmpt.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 25.Lefort SM, Gray-donald K, Rowat KM, Ellen M. Randomized controlled trial of a community-based psychoeducation program for the self-management of chronic pain. Pain. 1998;74:297–306. doi: 10.1016/S0304-3959(97)00190-5. [DOI] [PubMed] [Google Scholar]
- 26.Vlaeyen J, Teeken-Gruben N, Goossens M, et al. Cognitive-educational treatment of fibromyalgia: a randomized clinical trial. I Clin Effects J Rheumatol. 1996;23(7):1237–45. [PubMed] [Google Scholar]
- 27.Burckhardt C, Mannerkorpi K, Hedenberg L, Bjelle A. A randomized, controlled clinical trial of education and physical training for women with Fibromyalgia. J Rheumatol. 1994;21:714–20. [PubMed] [Google Scholar]
- 28.Chiauzzi E, Pujol LA, Wood M, et al. painACTION-back pain: a self-management website for people with chronic back pain. Pain Med. 2010;11(7):1044–58. doi: 10.1111/j.1526-4637.2010.00879.x. [DOI] [PubMed] [Google Scholar]
- 29.Michelotti A, Voilaro S, Steenks MH, Fareiia M. Evaluation of the short-term effectiveness of education versus an occlusal splint for the treatment of myofascial pain of the jaw muscles. J Orofacial Pain J Am Dental Assoc JADA. 2012;143:47–53. doi: 10.14219/jada.archive.2012.0018. [DOI] [PubMed] [Google Scholar]
- 30.Dush D. Effectiveness of home-study extended patient education for chronic pain. Am J Pain Manag. 2006;16(1):5–11. [Google Scholar]
- 31.Dworkin SF, State W, Foundation D, et al. A randomized clinical trial using research diagnostic criteria for temporomandibular disorders-axis II to target clinic cases for a tailored self-care TMD treatment program. J Orofac Pain. 2002;16(1):48–63. [PubMed] [Google Scholar]
- 32.Dirmaier J, Härter M, Weymann N. A tailored, dialogue-based health communication application for patients with chronic low back pain : study protocol of a randomised controlled trial. BMC Med Inform Decis Mak. 2013;13(66). doi:10.1186/1472-6947-13-66. [DOI] [PMC free article] [PubMed]
- 33.Jerjes W, Madland G, Feinmann C, et al. Psycho-education programme for temporomandibular disorders: a pilot study. J Negat Results Biomed. 2007;6:4. doi: 10.1186/1477-5751-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van Ittersum MW, van Wilgen CP, Groothoff JW, van der Schans CP. Is appreciation of written education about pain neurophysiology related to changes in illness perceptions and health status in patients with fibromyalgia? Patient Educ Couns. 2011;85(2):269–74. doi: 10.1016/j.pec.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 35.Clarke CL, Ryan CG, Martin DJ. Pain neurophysiology education for the management of individuals with chronic low back pain : A systematic review and meta-analysis. Man Ther. 2011;16(6):544–9. doi: 10.1016/j.math.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 36.Louw A, Diener I, Butler DS, Puentedura EJ. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. YAPMR. 2011;92(12):2041–56. doi: 10.1016/j.apmr.2011.07.198. [DOI] [PubMed] [Google Scholar]
- 37.Ling C, Lui LYY, So WKW. Do educational interventions improve cancer patients’ quality of life and reduce pain intensity? Quantitative systematic review. J Adv Nurs. 2011;68(3):511–20. doi: 10.1111/j.1365-2648.2011.05841.x. [DOI] [PubMed] [Google Scholar]
- 38.Gross A, Forget M, St George K, et al. Patient education for neck pain (Review) Cochrane Database Syst Rev. 2012;3 doi: 10.1002/14651858.CD005106.pub4. [DOI] [PubMed] [Google Scholar]
- 39.Yu H, Cote P, Southerst D, et al. Does structured patient education improve the recovery and clinical outcomes of patients with neck pain ? A systematic review from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Spine J. 2014;(in press). doi:10.1016/j.spinee.2014.03.039. [DOI] [PubMed]
- 40.Bennett MI, Bagnall A, Raine G, et al. Educational interventions by pharmacists to patients with chronic pain. Clin J Pain. 2011;27(7):623–30. doi: 10.1097/AJP.0b013e31821b6be4. [DOI] [PubMed] [Google Scholar]
- 41.Ospina MB, Taenzer P, Rashiq S, et al. A systematic review of the effectiveness of knowledge translation interventions for chronic noncancer pain management. Pain Res Manag. 2013;18(6):129–41. doi: 10.1155/2013/120784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Andrade SC, Araújo AGR, Vilar MJ. Escola de coluna para pacientes com lombalgia cronica inespecifica: Beneficios da associacao de exercicios e educacao ao paciente. Acta Reumatol Port. 2008;33:443–50. [PubMed] [Google Scholar]
- 43.Moher D, Liberati A, Tetzlaff J, Altman D, Group TP. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med. 2009;6(6) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]


