Introduction
I like to tell my residents and fellows that one of the benefits of working in the field of epilepsy is that you're rarely ever wrong: ask four different attending physicians the same question and you're likely to get four different answers; so whatever you propose to do for a patient, there's probably someone who will back you up.
I could scarcely come up with a better illustration of my aphorism than the results of a recent Quantitative Practical Use-Driven Learning Survey in epilepsy (Q-PULSE) regarding driving. We asked respondents their practice vis-à-vis driving in four different situations: 1) a patient on a monotherapy regimen who is tapering off the sole antiepileptic drug (AED), 2) a patient on a polytherapy regimen who is tapering off one of two AEDs, 3) a patient who is switching from one monotherapy AED to another. and 4) a patient who has psychogenic seizures.
FIGURE 1.
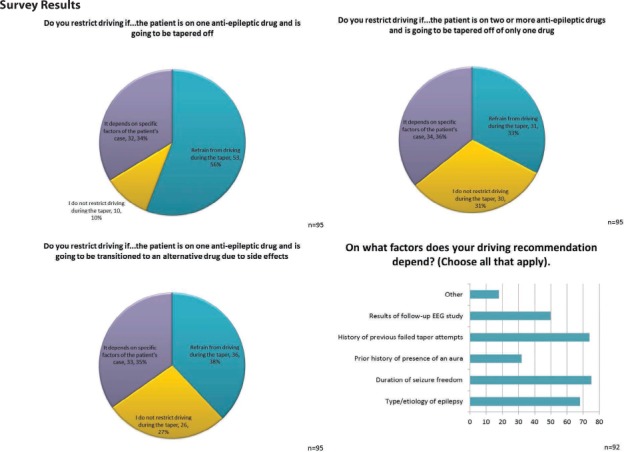
FIGURE 2.
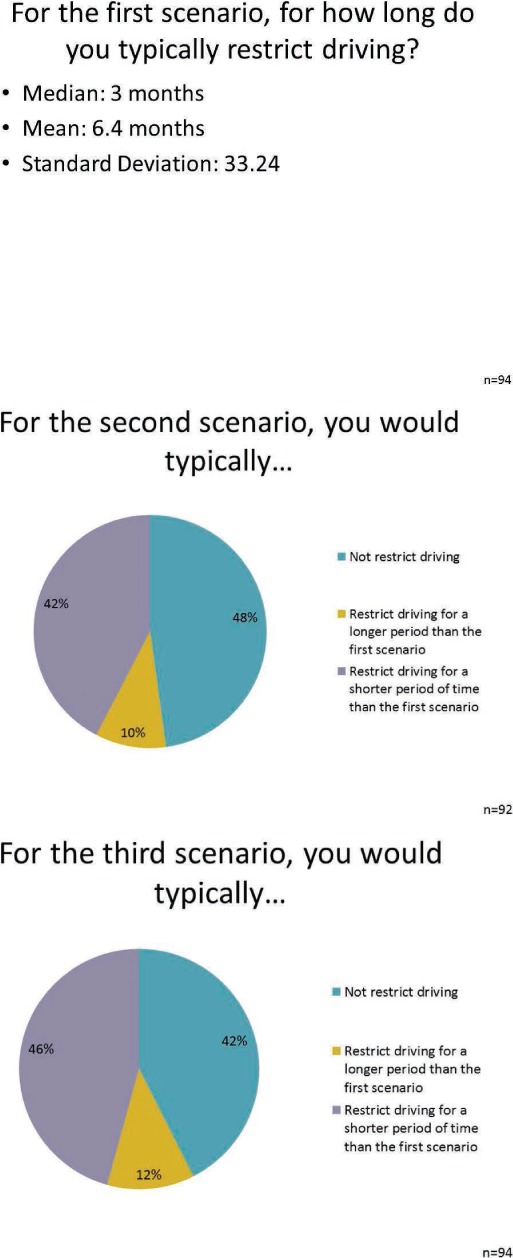
FIGURE 3.
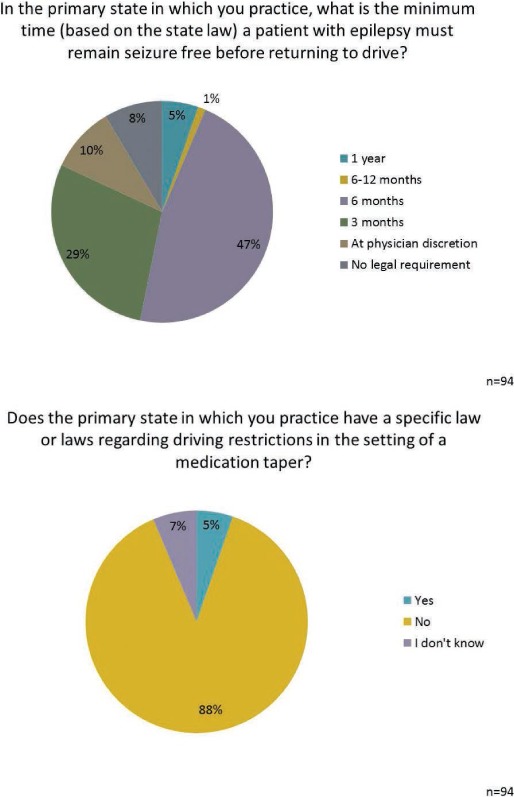
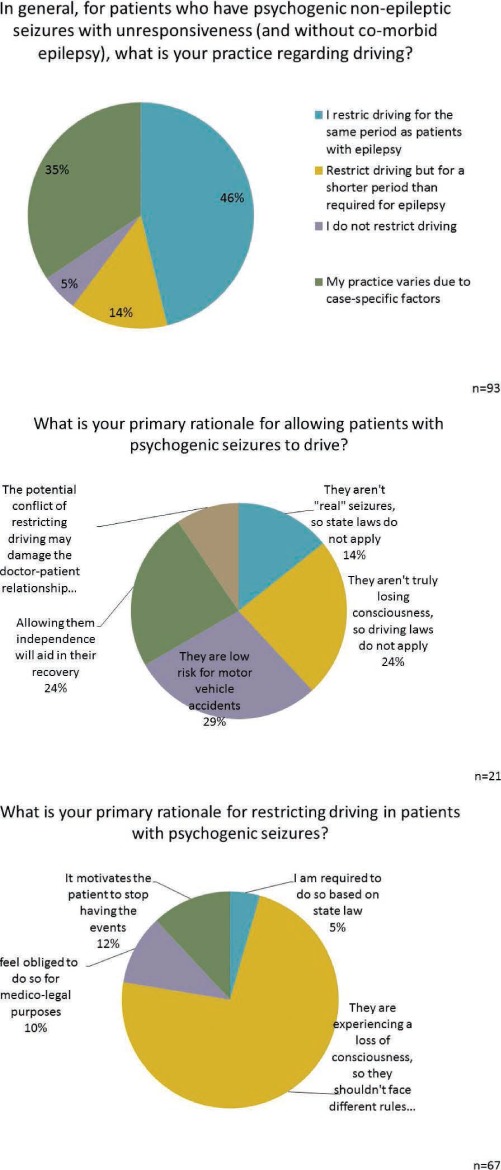
FIGURE 4.
Discussion
On this fundamental clinical issue, which we face on a weekly basis, there is no other way to characterize the responses than to say they demonstrate a spectacular lack of consensus. Regarding the most basic question, about half of the respondents restrict driving when tapering a patient off their only AED, and most of the remainder decide whether or not to restrict driving based on factors related to the patient's specific case, among which factors the most prominent are the results of prior taper attempts, the type of epilepsy the patient has, and the results of EEG. If the patient is discontinuing one of two agents or transitioning from one to another because of side effects, the split is even more stark: about a third of epileptologists restrict driving in these circumstances, another third do not, and the remaining third decide based on patient-specific factors. At least there is some fair agreement that in these latter two situations the driving restriction should be shorter in duration than for someone tapering off the only AED.
Particularly fascinating (to me, anyway) is the treatment of driving for patients with psychogenic non-epileptic seizures (PNESs). The respondent panel did not treat these patients much differently from patients with epilepsy on monotherapy; about half restricted driving (mostly for the same duration as for patients with epilepsy), and most of the rest decided based on patient-specific factors. About three-quarters of the former group indicated that they restrict driving for patients with PNESs because they experience loss of consciousness and should not be treated any differently from those with organic seizures, so at least they were consistent in their rationale. Those who do not restrict driving for patients with PNESs had a smattering of reasons for doing so.
All of this might be amusing if it were not, well, a little pathetic. I am the first to applaud those who think differently—after all, I'm one of the 5% who do not restrict driving in patients with PNESs—but I also cannot help feeling that for such a common issue, there ought to be a common approach. What we have, clearly, is anything but, and I suspect that these distinctions are not even between different lineages or schools of thought, because my own anecdotal experience suggests that the questions posed here are answered differently even by epileptologists at the same center. The stark reality is that the same patient, providing the same history, will be restricted or not restricted from driving depending upon whom they happen to see in the clinic. There is something unjust about this.
One can only speculate about the root cause of this lack of consensus, but perhaps one factor is that issue of seizures and driving puts physicians in the uncomfortable role of guarding public health at the expense of a patient's quality of life. Yes, driving with seizures is a risk to the patient himself, but this is something that can be weighed and discussed with the patient, especially in ambiguous situations, such as several of the situations posed to the panel. The real issue is the potential for harm to others. Physicians are responsible for acting in the interests of our patients' well-being; this is particularly so in a condition like epilepsy, which has ramifications that extend far beyond the acute medical condition. As I have written before (1), when those interests are in conflict with the interests of society in general, we are, in effect, being asked to contravene our primary professional and ethical obligation, which, aside from the most glaringly obvious and temporary circumstances (e.g., “You cannot leave until the Ebola is completely cleared”), we are ill-equipped to do. This is doubly true when the conflict of potential medicolegal implications is factored in, and it is becoming triply true with the burgeoning dependence of reimbursement on patient satisfaction (a topic which merits its own separate diatribe).
So we may discuss this, perhaps convene a consensus conference, maybe perform further studies into recurrence risks and accident risks in various clinical scenarios. But the best way to foster consistency and agreement on these issues would be the development of more detailed state laws to clarify physicians' responsibilities. At present there are no statutes covering AED taper in the majority of most states, and psychogenic seizures exist legally, just as they do medically, in a grey area.
For the time being, both patients and practitioners are left uncomfortably weighing risks. Perhaps we physicians can take some little solace in the results of this survey; since there is clearly no standard of care, it would be difficult to blame one of us for failing to meet it. In the meantime, while we all look to clinical researchers, academic laboratories, pharmaceutical companies, and medical device manufacturers for advances in the field, perhaps on this issue we should all look to Google: those self-driving cars can't come fast enough.
Footnotes
Editor's Note: Authors have a Conflict of Interest disclosure which is posted under the Supplemental Materials (149.9KB, pdf) link.
Reference
- 1.Mintzer S. License to ill: Playing the odds after withdrawing and restarting antiepileptic drugs. Epilepsy Curr. 2011;11:177–178. doi: 10.5698/1535-7511-11.6.177. [DOI] [PMC free article] [PubMed] [Google Scholar]


