Abstract
Percutaneous coronary intervention and coronary artery bypass grafting may be performed before orthotopic liver transplantation (OLT) to try to improve the condition of patients who have severe ischemic heart disease. However, data supporting improved outcomes are lacking.
We reviewed the medical records of 2,010 patients who underwent OLT at our hospital from 2000 through 2010. The 51 patients who underwent coronary artery angiography within 6 months of transplantation were included in this study: 28 had mild coronary artery disease, 10 had moderate disease, and 13 had severe disease. We compared all-cause and cardiac-cause mortality rates.
We found a significant difference in cardiac deaths between the groups (P <0.001), but none in all-cause death (P=0.624). Of the 10 patients who had moderate coronary artery disease, one underwent pre-transplant coronary artery bypass grafting. Of 13 patients with severe disease, 3 underwent percutaneous coronary intervention, and 6 underwent coronary artery bypass grafting. Overall, 50% of patients who underwent either intervention died of cardiac-related causes, whereas no patient died of a cardiac-related cause after undergoing neither intervention (P <0.0001).
We conclude that, despite coronary intervention, mortality rates remain high in OLT patients who have severe coronary artery disease.
Keywords: Coronary artery disease/complications/physiopathology, decision support techniques, liver transplantation, patient selection, predictive value of tests, retrospective studies, risk factors, treatment outcome
Patients scheduled for orthotopic liver transplantation (OLT) typically undergo an extensive preoperative cardiac evaluation.1–5 In cirrhotic patients, higher cardiac outputs with reduced ventricular responses to stress and concomitant systemic vasodilation make the initial evaluation challenging.3,5,6 Variations in the accuracy of this evaluation have been noted, despite guidelines from the American College of Cardiology (ACC)2 and the American Association for the Study of Liver Disease (AASLD).1
Patients with end-stage liver disease are at greater risk than the general population for coronary artery disease (CAD), and up to 25% of these patients might have subclinical CAD.3,4 Investigators have questioned whether current practices are effective in diagnosing underlying CAD in OLT patients.7–13 The cardiac-cause mortality rate in patients with liver disease and CAD exceeds 40%.5,14 Therefore, it is important to understand appropriate preoperative evaluation and treatment of these patients.
Existing guidelines help in preoperative evaluation of patients scheduled for OLT, but no study results guide practice in the presence of diagnosed CAD. We studied whether coronary interventions before OLT might yield a survival benefit after OLT.
Patients and Methods
We reviewed the electronic medical records of 2,010 patients who underwent OLT at our hospital from 2000 through 2010. The 51 patients who had undergone invasive coronary angiography were selected for the study and were classified to have mild CAD (<50% stenosis of a major coronary artery), moderate CAD (50%–70% stenosis), or severe CAD (>70% stenosis).7–13
We collected the patients' demographic, clinical, and echocardiographic data, and determined whether coronary artery bypass grafting (CABG) or percutaneous coronary intervention (PCI) with stent placement had been performed within 6 months before OLT. All preoperative data had been obtained within 30 days of the diagnostic coronary angiography. All the patients had undergone dobutamine stress echocardiography (DSE) before OLT.1,2 Patients had a positive tobacco history if there was documentation of prior use. Patients had renal dysfunction if their glomerular filtration rate was <60 mL/min/1.73 m2. Our institutional review board approved the study.
Statistical Analysis
Comparisons were made on the basis of CAD significance, and between patients who underwent PCI or CABG and those who did not. Survival and death data were collected from the medical records and Social Security Death Index. Cardiac death was defined as a primary acute coronary syndrome as the cause of death. Data were analyzed by means of analysis of variance, the χ2 test, and the Student t test. A P value <0.05 was considered statistically significant. Statistical analyses were performed with use of JMP® 11 software (SAS Institute Inc.; Cary, NC).
Results
Table I shows the 51 patients' baseline characteristics. Twenty-eight patients had mild CAD, 10 had moderate CAD, and 13 had severe CAD. Among all the demographic, laboratory, and echocardiographic values, the only significant difference between the groups was the presence of diabetes mellitus (P=0.004).
TABLE I.
Baseline Patient Characteristics before Liver Transplantation
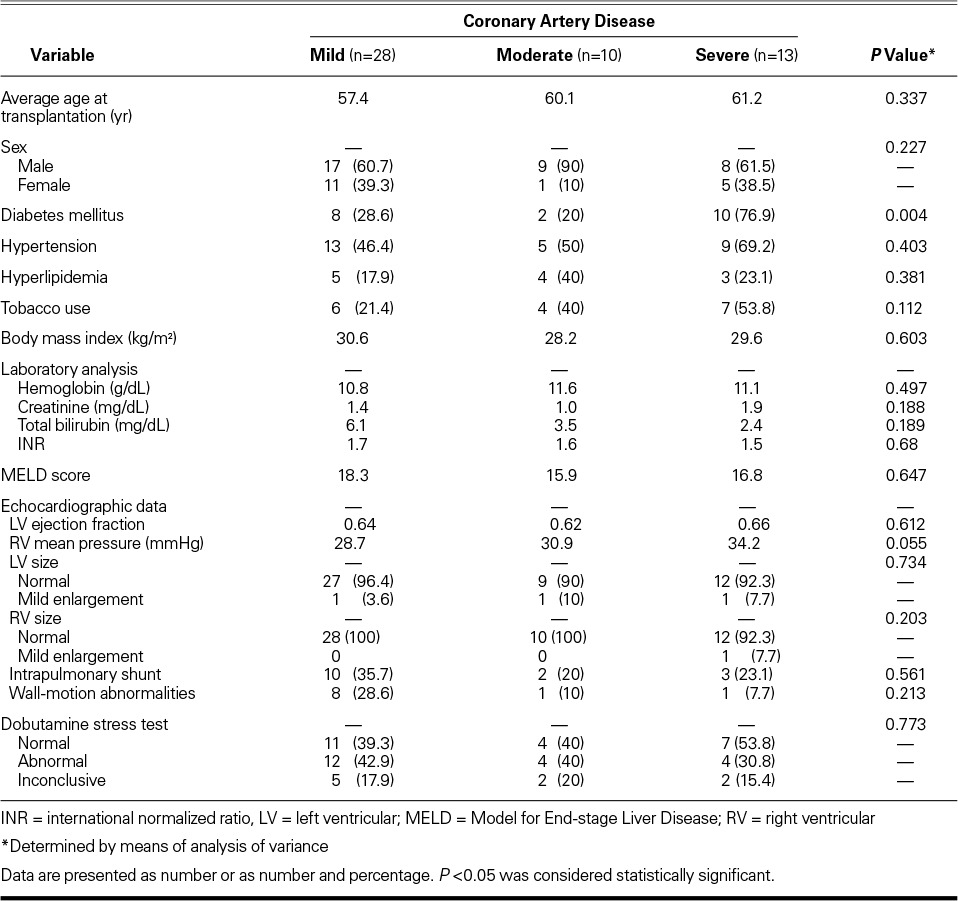
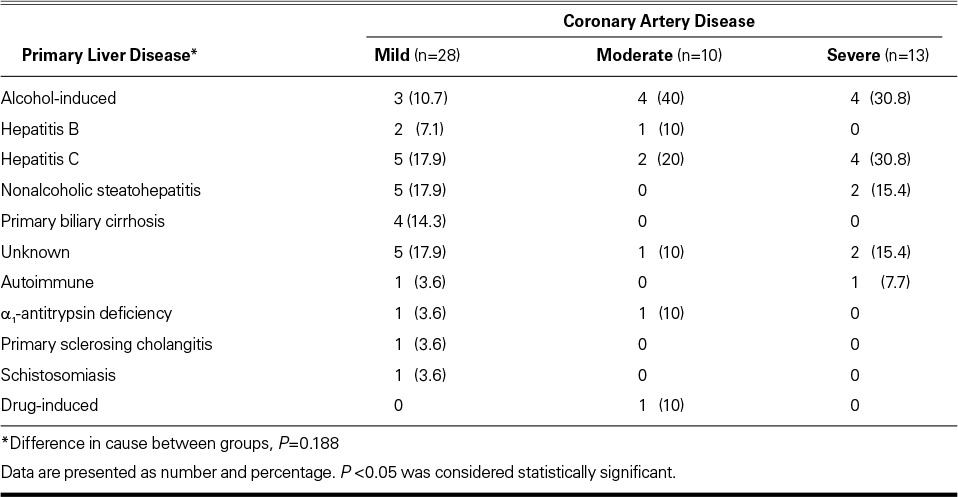
The patients with mild CAD had a somewhat higher overall Model for End-stage Liver Disease score than did the patients with moderate or severe CAD (Table I). The most prevalent causes of end-stage liver disease in the cohort were hepatitis C and nonalcoholic steatohepatitis (Table II). The differences in disease cause were not statistically significant (P=0.188).
TABLE II.
Comparison of Types of Liver Disease
Five patients (38.5%) who had severe CAD died of all causes. This compared with the all-cause deaths of 2 who had moderate CAD (20%) and 10 (35.7%) who had mild CAD (P=0.624) (Table III). Four of those 5 in the severe-CAD group died of a cardiac cause, in comparison with no cardiac deaths in either of the other groups (P=0.001). Of those 4 cardiac deaths, 2 were of non-ST-segment-elevation myocardial infarctions with refractory cardiogenic shock, and 1 of new-onset decompensated heart failure. Another patient died during the same hospitalization as the transplantation. The 5th death in the severe-CAD group was attributed to septic shock. The average time from OLT to cardiac death was 1.25 years. On average, the patients who died of noncardiac causes lived less than one year after OLT.
TABLE III.
Patient Outcomes Based on Severity of Coronary Artery Disease
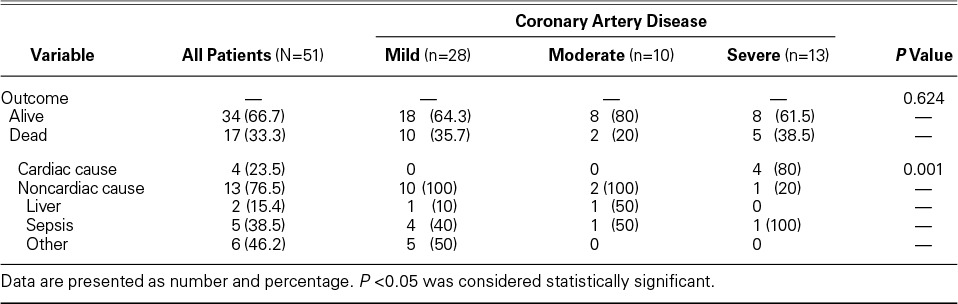
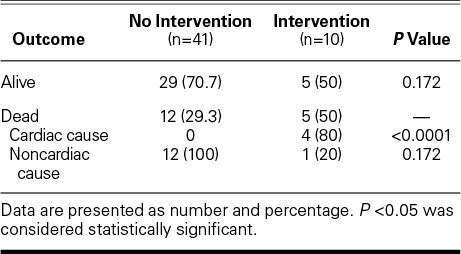
No difference in cardiac mortality rates was observed between PCI and CABG patients (P=0.312) (Fig. 1). Of the 10 patients who underwent either intervention, 5 (50%) died of any cause, in comparison with 12 of 41 patients (29.3%) who died after no cardiac intervention (P=0.172) (Table IV). Four of the 5 deaths were of cardiac cause in the intervention group, versus no cardiac deaths in the no-intervention group (P <0.0001).
Fig. 1.
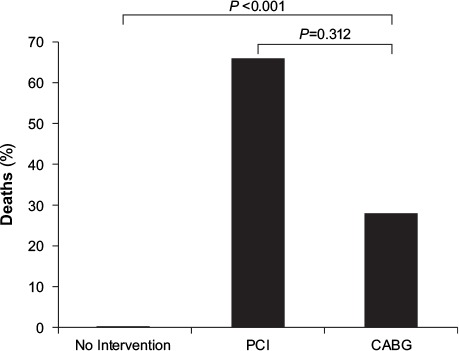
Graph compares mortality rate on the basis of coronary intervention. P <0.05 was considered statistically significant.
CABG = coronary artery bypass grafting; PCI = percutaneous coronary intervention
TABLE IV.
Outcome Based on Preoperative Intervention versus No Intervention
Of the 13 patients who had severe CAD, the 4 who underwent no intervention were alive upon post-OLT follow-up evaluation. In contrast, 5 (55.5%) of the 9 patients who underwent an intervention died (Fig. 2).
Fig. 2.
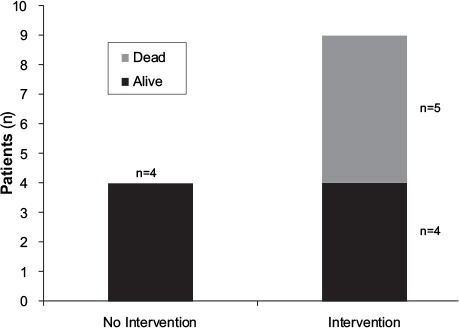
Graph compares the outcome of patients with severe coronary artery disease based on coronary intervention.
Discussion
Our findings suggest that PCI or CABG before OLT does not necessarily impart a cardiovascular survival benefit. We found that the patients who underwent intervention before OLT were at high risk for cardiac-cause death. All the patients who died of a cardiac cause had undergone PCI or CABG before OLT.
As expected, the patients with severe CAD had a higher cardiac-related mortality rate than did the patients with mild or moderate CAD. Of note, 4 patients in the severe-CAD group who underwent intervention died of a cardiac cause, whereas all who did not undergo intervention survived. Although interventions help with cardiac perfusion and in avoiding myocardial ischemia, other adverse effects of CAD might not improve after intervention.
We noted no differences in pre-OLT resting and stress echocardiographic results in the 3 CAD groups. The AASLD recommends that DSE be performed in patients who will undergo OLT, and the ACC recommends against invasive testing; however, investigators in several cohort studies have noted that the sensitivity and specificity of DSE can be influenced by the hyperdynamic and vasodilatory states in such patients.1,2 In cirrhotic patients, DSE has poor sensitivity and specificity.12,15 Additional studies will be crucial in determining the value and methodology of preoperative stress testing in this patient population.
The overall survival rate in our study cohort of 66.7% is lower than our institution's 3-year survival rate of 87.5% and the national average of 81.5%.16 Our cohort probably had more severe comorbid conditions and more complications of the liver disease, so we conducted rigorous pre-OLT testing. Our institution does not mandate routine cardiac catheterization in all patients who undergo OLT; for consistency, we studied only the patients who had undergone this procedure, and we found that more than half had mild CAD. In addition, most had normal preoperative echocardiographic findings.
Multiple study limitations were present. Relatively few of our institution's patients routinely underwent pre-OLT coronary angiography, which limited the study's population size and introduced possible selection bias. This cohort was probably more ill than is typical. The study was retrospective, and a randomized controlled trial was not feasible. Patients with severe CAD might not have routinely undergone formal evaluation before OLT. In addition, patients undergoing revascularization might not all undergo OLT, further limiting the population size.
We conclude that, despite coronary interventions, mortality rates remain high in patients who have severe CAD before OLT. Multicenter studies are warranted to confirm our findings, and additional data comparing the extent of CAD and outcomes in this population would be relevant.
Footnotes
From: Department of Medicine (Drs. McRee, Seeger, and Snipelisky) and Division of Cardiovascular Diseases (Drs. Levy and Shapiro), Mayo Clinic, Jacksonville, Florida 32224
References
- 1.Murray KF, Carithers RL, Jr, AASLD AASLD practice guidelines: evaluation of the patient for liver transplantation. Hepatology. 2005;41(6):1407–32. doi: 10.1002/hep.20704. [DOI] [PubMed] [Google Scholar]
- 2.Fleisher LA, Beckman JA, Brown KA, Calkins H, Chaikof EL, Fleischmann KE et al. 2009 ACCF/AHA focused update on perioperative beta blockade incorporated into the ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. Circulation. 2009;120(21):e169–276. doi: 10.1161/CIRCULATIONAHA.109.192690. [DOI] [PubMed] [Google Scholar]
- 3.Mandell MS, Lindenfield J, Tsou MY, Zimmerman M. Cardiac evaluation of liver transplant candidates. World J Gastroenterol. 2008;14(22):3445–51. doi: 10.3748/wjg.14.3445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raval Z, Harinstein ME, Skaro AI, Erdogan A, DeWolf AM, Shah SJ et al. Cardiovascular risk assessment of the liver transplant candidate. J Am Coll Cardiol. 2011;58(3):223–31. doi: 10.1016/j.jacc.2011.03.026. [DOI] [PubMed] [Google Scholar]
- 5.Snipelisky D, Donovan S, Levy M, Satyanarayana R, Shapiro B. Cardiac troponin elevation predicts mortality in patients undergoing orthotopic liver transplantation. J Transplant. 2013;2013:252838. doi: 10.1155/2013/252838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tiukinhoy-Laing S, Rossi JS, Bayram M, De Luca L, Gafoor S, Blei A et al. Cardiac hemodynamic and coronary angiographic characteristics of patients being evaluated for liver transplantation. Am J Cardiol. 2006;98(2):178–81. doi: 10.1016/j.amjcard.2006.01.089. [DOI] [PubMed] [Google Scholar]
- 7.Harinstein ME, Flaherty JD, Ansari AH, Robin J, Davidson CJ, Rossi JS et al. Predictive value of dobutamine stress echocardiography for coronary artery disease detection in liver transplant candidates. Am J Transplant. 2008;8(7):1523–8. doi: 10.1111/j.1600-6143.2008.02276.x. [DOI] [PubMed] [Google Scholar]
- 8.Williams K, Lewis JF, Davis G, Geiser EA. Dobutamine stress echocardiography in patients undergoing liver transplantation evaluation. Transplantation. 2000;69(11):2354–6. doi: 10.1097/00007890-200006150-00023. [DOI] [PubMed] [Google Scholar]
- 9.Keeffe BG, Valantine H, Keeffe EB. Detection and treatment of coronary artery disease in liver transplant candidates. Liver Transpl. 2001;7(9):755–61. doi: 10.1053/jlts.2001.26063. [DOI] [PubMed] [Google Scholar]
- 10.Sawada SG, Segar DS, Ryan T, Brown SE, Dohan AM, Williams R et al. Echocardiographic detection of coronary artery disease during dobutamine infusion. Circulation. 1991;83(5):1605–14. doi: 10.1161/01.cir.83.5.1605. [DOI] [PubMed] [Google Scholar]
- 11.Umphrey LG, Hurst RT, Eleid MF, Lee KS, Reuss CS, Hentz JG et al. Preoperative dobutamine stress echocardiographic findings and subsequent short-term adverse cardiac events after orthotopic liver transplantation. Liver Transpl. 2008;14(6):886–92. doi: 10.1002/lt.21495. [DOI] [PubMed] [Google Scholar]
- 12.Findlay JY, Keegan MT, Pellikka PP, Rosen CB, Plevak DJ. Preoperative dobutamine stress echocardiography, intraoperative events, and intraoperative myocardial injury in liver transplantation. Transplant Proc. 2005;37(5):2209–13. doi: 10.1016/j.transproceed.2005.03.023. [DOI] [PubMed] [Google Scholar]
- 13.Donovan CL, Marcovitz PA, Punch JD, Bach DS, Brown KA, Lucey MR, Armstrong WF. Two-dimensional and dobutamine stress echocardiography in the preoperative assessment of patients with end-stage liver disease prior to orthotopic liver transplantation. Transplantation. 1996;61(8):1180–8. doi: 10.1097/00007890-199604270-00011. [DOI] [PubMed] [Google Scholar]
- 14.Watt KD, Pedersen RA, Kremers WK, Heimbach JK, Charlton MR. Evolution of causes and risk factors for mortality post-liver transplant: results of the NIDDK long-term follow-up study. Am J Transplant. 2010;10(6):1420–7. doi: 10.1111/j.1600-6143.2010.03126.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Snipelisky D, Levy M, Shapiro B. Utility of dobutamine stress echocardiography as part of the pre-liver transplant evaluation: an evaluation of its efficacy. Clin Cardiol. 2014;37(8):468–72. doi: 10.1002/clc.22283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mayo Foundation for Medical Education and Research. Liver Transplant, 2012 [Internet]. Available from: http://www.mayoclinic.org/liver-transplant/liver-fl-survival-graph.html [revised 2015 Jun] [Google Scholar]


