Abstract
A 55-year-old woman was admitted for orthotopic heart transplantation. Her medical history was notable for multiple cardiovascular problems, including ischemic cardiomyopathy that necessitated circulatory support with a left ventricular assist device. Five weeks after undergoing orthotopic heart transplantation, she developed Aspergillus calidoustus mediastinitis, for which she underwent a prolonged course of antifungal treatment that comprised (in sequence) posaconazole for 11 days, voriconazole for 10 days, and amphotericin B for 42 days. During this period, she also underwent repeated mediastinal drainage and sternal débridement, followed by sternal wiring and coverage with bilateral pectoralis advancement flaps. Four months postoperatively, she was discharged from the hospital with a successfully controlled infection and a healed sternum. To our knowledge, only 3 previous cases of Aspergillus mediastinitis after orthotopic heart transplantation have been reported in the literature, none of which was Aspergillus calidoustus.
Keywords: Amphotericin B/therapeutic use; antifungal agents; aspergillosis/therapy; Aspergillus calidoustus; heart transplantation, orthotopic; mediastinitis, postoperative; surgical wound infection/complications
Postoperative Aspergillus mediastinitis is extremely rare in cardiac surgery patients. To the best of our knowledge, only 11 such cases have been reported.1,2 The U.S. Centers for Disease Control and Prevention defines Aspergillus mediastinitis as the presence of a positive culture result from a mediastinal sample, plus one of the following: 1) fever higher than 38 °C, or 2) chest pain or sternal instability with purulent effusion in the mediastinum or positive culture results from surgically obtained samples or blood.1 Of all cardiothoracic procedures, orthotopic heart transplantation (OHT) is associated with the highest risk of mediastinitis (including bacterial and fungal), with infection rates of 2.5% to 6%.3 A review of the literature reveals only 3 cases in which Aspergillus mediastinitis occurred after OHT; all 3 cases involved A. fumigatus. We describe what we believe to be the first case of Aspergillus calidoustus mediastinitis after OHT.
Case Report
A 55-year-old woman was admitted for OHT. Her medical history was notable for ischemic cardiomyopathy, as well as for hypertension, dyslipidemia, coronary artery disease, myocardial infarction, ventricular tachycardia, paroxysmal atrial fibrillation, and chronic kidney disease. Her surgical history included implantation of a left ventricular assist device (LVAD), resection of a left ventricular aneurysm, and implantation of a biventricular defibrillator. She had no history of infectious sequelae with her LVAD. During the OHT procedure, the patient was coagulopathic and needed several units of different blood products. Her chest was temporarily closed at the end of the operation and was permanently closed 3 days later.
Postoperatively, she had prolonged respiratory and renal failure that necessitated ventilator support, hemodialysis, and inotropic and vasopressor support. Despite the new heart, she also needed further circulatory support, including an intra-aortic balloon pump. Two weeks postoperatively, she underwent a tracheostomy. Five weeks postoperatively, she developed fever with an elevated white blood cell count. Physical examination revealed tenderness, erythema, and sternal wound drainage. A computed tomographic scan revealed a mediastinal fluid collection and thereby confirmed the diagnosis. Surgical drainage of the fluid and aggressive débridement of the infected sternum were performed. During débridement, we locally irrigated the infected tissue with a solution (ca. 2 L) containing amphotericin, bacitracin, and vancomycin; this we did repeatedly. Specimens sent for microbiologic and histopathologic examination revealed A. calidoustus, acutely inflamed granulation tissue (Fig. 1), and numerous fungal hyphae with acute angle branching (Fig. 2). We initiated a prolonged course of antifungal treatment that comprised (in sequence) posaconazole for 11 days, voriconazole for 10 days, and amphotericin B for 42 days. During this period, the patient underwent repeated surgical procedures for sternal wound débridement and the placement of vancomycin antibiotic beads. To form the beads on nylon suture (during the 2nd and 3rd débridements), we mixed polymethyl methacrylate cement with 2 g of vancomycin, 2.4 g of tobramycin, and 200 mg of amphotericin B, to form beads 1 cm in diameter. During the patient's 2nd débridement, a portion of her retained LVAD outflow graft was identified in the field of infection and subsequently removed. When the patient developed A. calidoustus, the regimen and dose of immunosuppression was changed to liposomal Amphotericin B. Mycophenolate mofetil (MMF) was withheld for most of the course of infection; tacrolimus was initially withheld, then slowly restarted, after débridement and closure of the wound, to a low dose (target levels lower than the normal 8–10 μg/L)—and steroids were reduced to 5 mg/d until the wound was closed.
Fig. 1.
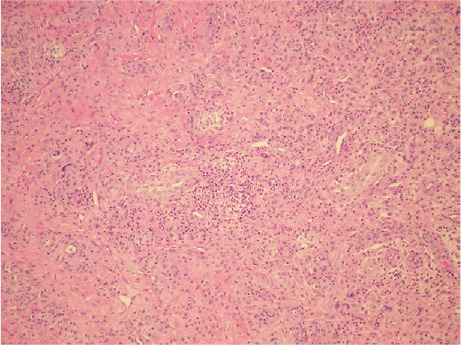
Photomicrograph of resected mediastinal tissue shows acutely inflamed granulation (H & E, orig. ×100).
Fig. 2.
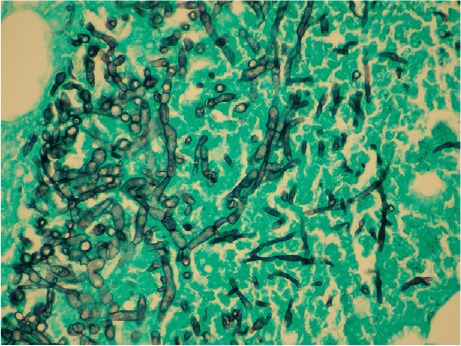
Photomicrograph of resected mediastinal tissue shows a mycelium of intercommunicating fungal hyphae, divided by septa, many of which show acute angle branching (Gomori methenamine silver, orig. ×400).
After aggressive surgical débridements (4 over 18 d), in the absence of gross infection and necrotic tissue and in the presence of newly developed pink granulation tissue, we wired the sternum and then covered it with bilateral pectoralis advancement flaps. Four months after OHT, the patient was weaned from the tracheostomy and discharged from the hospital on a regimen of hemodialysis therapy.
According to the revised (R) rejection criteria of the International Society for Heart and Lung Transplantation (ISHLT), our patient's last 3 cardiac biopsies revealed no cellular rejection (ISHLT grade, 0 R) and no complement split product C4d. Follow-up echocardiograms showed near-normal overall left ventricular systolic function, with a left ventricular ejection fraction of 0.50 to 0.55.
Discussion
Postsurgical mediastinitis is an infection involving the sternum, the subcutaneous tissues, and the structures between the sternum and the esophagus.3 Aspergillus fungal mediastinitis has been reported after open-heart procedures, such as coronary artery bypass operations, but it is extremely rare after heart transplantation.2,4 This could be because postsurgical mediastinitis usually occurs within 30 days,4–6 but the significant waning of cellular immunity that makes a patient increasingly vulnerable to fungal infection occurs more than 30 days postoperatively.7 Because the 2 events are not concordant, fungal mediastinitis is unlikely to occur.
To our knowledge, only 3 cases of Aspergillus mediastinitis after OHT, all involving A. fumigatus, have previously been reported. Byl and colleagues8 described the case of a 51-year-old man who underwent OHT and developed a sternal wound infection 24 days later. The wound was drained, and cultures showed A. fumigatus. On postoperative day 48, the patient died suddenly. Postmortem examination revealed mediastinitis and a ruptured pseudoaneurysm of the ascending aorta, with hyphae in the aortic wall. The authors reported that contamination of the surgical field and seeding during surgery were the most probable sources of infection. In addition, Levin and associates3 described the case of a 61-year-old man who was diagnosed with A. fumigatus mediastinitis about 2.5 months after OHT. The patient was treated with voriconazole and recovered fully. The 3rd case, reported by Forestier and co-authors,9 involved a 51-year-old woman who developed mediastinitis caused by A. fumigatus and Staphylococcus epidermidis about 12 weeks after OHT. She was successfully treated with amphotericin B in combination with caspofungin, voriconazole, antibiotics, and superficial wound drainage.
Varga and colleagues10 have described A. calidoustus as an emerging species. They concluded that all 27 A. calidoustus isolates were triazole resistant, with minimal inhibitory concentrations (MICs) of ≥8 μg/mL. In a study conducted by Baddley and colleagues,11 all A. calidoustus isolates had MICs of >4 μg/mL for the trizoles.
In our patient, A. calidoustus mediastinitis developed 5 weeks after OHT. For the antifungal treatment, posaconazole was started (on the day after the first débridement) when mold was first identified—in order to cover non-Aspergillus species empirically. Therapy was changed to voriconazole when the mold was identified as an Aspergillus species. However, therapy was changed to liposomal amphotericin B when the isolate was identified as A. calidoustus, because that species is resistant to voriconazole (MIC, 4 μg/mL), whereas the amphotericin MIC specifies only 1 μg/mL. Repeated cultures revealed that the infection was purely fungal, with no bacterial element. Aggressive antifungal medical therapy and surgical débridement, followed by sternal wiring and bilateral pectoralis advancement flap coverage, were efficacious in successfully managing this case.
Footnotes
From: Departments of Cardiovascular Surgery (Drs. Aftab, El-Sayed Ahmed, Frazier, Mallidi, and Singh) and Cardiology (Dr. Almanfi), Texas Heart Institute; and Division of Cardiothoracic Surgery (Drs. Aftab, Frazier, Mallidi, and Singh), Michael E. DeBakey Department of Surgery, Baylor College of Medicine; Houston, Texas 77030
Dr. El-Sayed Ahmed is now at Tampa General Hospital, Tampa, Florida, and is a member of the Department of Surgery, Zagazig University Faculty of Medicine, Zagazig, Egypt.
References
- 1.Dimopoulos G, Tsangaris I, Poulakou G, Panayiotides J, Tsaknis G, Orfanos S, Armaganides A. Post-operative Aspergillus mediastinitis in a man who was immunocompetent: a case report. J Med Case Rep. 2010;4:312. doi: 10.1186/1752-1947-4-312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pasqualotto AC, Denning DW. Post-operative aspergillosis. Clin Microbiol Infect. 2006;12(11):1060–76. doi: 10.1111/j.1469-0691.2006.01512.x. [DOI] [PubMed] [Google Scholar]
- 3.Levin T, Suh B, Beltramo D, Samuel R. Aspergillus mediastinitis following orthotopic heart transplantation: case report and review of the literature. Transpl Infect Dis. 2004;6(3):129–31. doi: 10.1111/j.1399-3062.2004.00064.x. [DOI] [PubMed] [Google Scholar]
- 4.Karwande SV, Renlund DG, Olsen SL, Gay WA, Jr, Richenbacher WE, Hawkins JA et al. Mediastinitis in heart transplantation. Ann Thorac Surg. 1992;54(6):1039–45. doi: 10.1016/0003-4975(92)90067-e. [DOI] [PubMed] [Google Scholar]
- 5.Baldwin RT, Radovancevic B, Sweeney MS, Duncan JM, Frazier OH. Bacterial mediastinitis after heart transplantation. J Heart Lung Transplant. 1992;11(3 Pt 1):545–9. [PubMed] [Google Scholar]
- 6.Samuel R, Axelrod P, John KS, Fekete T, Alexander S, McCarthy J et al. An outbreak of mediastinitis among heart transplant recipients apparently related to a change in the United Network for Organ Sharing guidelines. Infect Control Hosp Epidemiol. 2002;23(7):377–81. doi: 10.1086/502069. [DOI] [PubMed] [Google Scholar]
- 7.Fishman JA, Rubin RH. Infection in organ-transplant recipients. N Engl J Med. 1998;338(24):1741–51. doi: 10.1056/NEJM199806113382407. [DOI] [PubMed] [Google Scholar]
- 8.Byl B, Jacobs F, Antoine M, Depierreux M, Serruys E, Primo G, Thys JP. Mediastinitis caused by Aspergillus fumigatus with ruptured aortic pseudoaneurysm in a heart transplant recipient: case study. Heart Lung. 1993;22(2):145–7. [PubMed] [Google Scholar]
- 9.Forestier E, Remy V, Lesens O, Martinot M, Hansman Y, Eisenmann B, Christmann D. A case of Aspergillus mediastinitis after heart transplantation successfully treated with liposomal amphotericin B, caspofungin and voriconazole. Eur J Clin Microbiol Infect Dis. 2005;24(5):347–9. doi: 10.1007/s10096-005-1327-5. [DOI] [PubMed] [Google Scholar]
- 10.Varga J, Houbraken J, Van Der Lee HA, Verweij PE, Samson RA. Aspergillus calidoustus sp nov., causative agent of human infections previously assigned to Aspergillus ustus. Eukaryot Cell. 2008;7(4):630–8. doi: 10.1128/EC.00425-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baddley JW, Marr KA, Andes DR, Walsh TJ, Kauffman CA, Kontoyiannis DP et al. Patterns of susceptibility of Aspergillus isolates recovered from patients enrolled in the Transplant-Associated Infection Surveillance Network. J Clin Microbiol. 2009;47(10):3271–5. doi: 10.1128/JCM.00854-09. [DOI] [PMC free article] [PubMed] [Google Scholar]


