Abstract
Cancer is projected to become a leading cause of morbidity and mortality in low-income and middle-income countries in the future. However, cancer incidence in South Africa is largely under-reported because of a lack of nationwide cancer surveillance networks. We describe present cancer surveillance activities in South Africa, and use the International Agency for Research on Cancer framework to propose the development of four population-based cancer registries in South Africa. These registries will represent the ethnic and geographical diversity of the country. We also provide an update on a cancer surveillance pilot programme in the Ekurhuleni Metropolitan District, and the successes and challenges in the implementation of the IARC framework in a local context. We examine the development of a comprehensive cancer surveillance system in a middle-income country, which might serve to assist other countries in establishing population-based cancer registries in a resource-constrained environment.
Introduction
Non-communicable diseases (NCDs) are the leading cause of deaths worldwide, with 80% of NCD-related deaths occurring in low-income and middle-income countries (LMICs).1 Among NCDs prioritised for action at the UN General Assembly on NCDs in 2011 were cardiovascular disease, diabetes, chronic respiratory disease, and cancer.1 Cancer is projected to become a leading cause of morbidity and mortality in developing countries in the near future,2 with an increase from 6·1 million new cases in 2012 to 9·9 million new cases in 2030.3
Cancer is under-reported in South Africa because of the lack of a comprehensive cancer surveillance system. The implementation of population-based registration in South Africa is in its infancy, which presents an ideal opportunity to review the challenges and outcomes of the process thus far.
South Africa is a medium-sized country, divided into nine provinces, with a population of just over 54 million people.4 The country’s complex political history has shaped health-care service provision and the present disease burden,5,6 with health-care services available from both public and private facilities. Although most South Africans (83%) use public health-care services, private health care accounts for 43% of total South African health expenditure.7
As with other LMICs, South Africa has a shortage of qualified health-care professionals. In 2011, roughly 162 630 health-care professionals were registered with the Health Professions Council of South Africa,8 excluding nurses, pharmacists, and pharmacy assistants. For comparative reasons, South Africa and Chile are considered peer countries since both are middle-income countries with dual health-care systems (public and private), high private health-care expenditure, a primary health-care driven public health system, and both recognise the need for health-care reform.9 Despite similarities, South Africa has 5·4 doctors per 10 000 population, whereas Chile has 15·7 doctors per 10 000 population.8 In 2011, the number of South African medical specialists per 10 000 population was 1·96 (with substantial variation per province), compared with 4·65 per 10 000 in Chile. In South Africa, 57% of health-care specialists are estimated to engage in private practice, which serves only 17% of the population.7,10 Thus, the already disadvantaged 83% of the population who rely solely on public health care have access to disproportionately fewer health-care services. Oncology healthcare workers registered with the Health Professions Council of South Africa in 2014, distributed in both the public and private health-care system, are listed in the table. Although the table shows a combined listing, many oncology personnel practise only in the private health-care system.
Table.
Cancer-related specialists registered with the Health Professions Council of South Africa, 2014
| Number | Per 10 000 population | |
|---|---|---|
| Medical oncologists | 33 | 0·006 |
| Paediatric medical oncologists | 20 | 0·01 |
| Radiation oncologists | 201 | 0·04 |
| Pathologists (anatomical) | 258 | 0·05 |
Ratios calculated using statistics from the South Africa mid-year population estimates for 2014; paediatric population includes all children aged 0–14 years.4 Information courtesy of the Health Professions Council of South Africa.
Currently, South Africa is experiencing a health shift with an increasing burden of NCDs in addition to already existing health-care issues.11 Since 1990, South Africa has seen an increase in both morbidity and mortality as a result of the increasing burden of HIV and AIDS, other communicable diseases, NCDs, and trauma, which disproportionately affect lower socioeconomic groups.5–7 Cancer is no exception, with 112 921 new cases of cancer predicted to be diagnosed in South Africa in 2030 compared with just 77 440 in 2012.3
In view of the expected cancer burden growth in the future, a national cancer surveillance system is needed to track incidence trends, plan for screening and diagnostic services, direct health-care system resources, and assess cancer prevention activities. We discuss the history and current status of present surveillance systems in South Africa, and present a rationale for developing a new system for routine cancer surveillance by using the International Agency for Research on Cancer (IARC) framework for implementation of four population-based cancer registries.12 Furthermore, the needs for implementation and sustainability of this new system will be examined.
Present cancer surveillance systems in South Africa
Cancer surveillance data for South Africa are provided by three cancer registries: the South African National Cancer Registry (NCR), the Eastern Cape Province Cancer Registry, and the South African Paediatric Tumour Registry.
The South African NCR
The present NCR was established in 1986 as a national, pathology-based cancer registry at the South African Institute for Medical Research (now the National Health Laboratory Service) as a collaborative venture with the Cancer Association of South Africa and the National Department of Health. The NCR is the only source of national cancer statistics and incidence data in South Africa, collecting data and analysing cancer cases diagnosed in pathology laboratories (both public and private) nationwide and reporting annual cancer incidence stratified by sex, age, and ethnic groups. The NCR’s methods follow the recommendations of IARC and have been described previously.13 The NCR has an archive of more than 1·2 million cancer records in its database and adds about 55 000 new records per year.
Despite its early success, the challenges the South African NCR has encountered might provide valuable lessons for other LMICs that may also wish to establish cancer surveillance programmes. The position of Director of the NCR was vacant from 2002 to 2009 because of funding constraints to recruit an appropriate candidate. Appropriate leadership is essential to ensure the strategic direction of the cancer registry, promote research activities, and encourage international collaborations and confidence in the registry. From 2005 to 2010, some private laboratories did not submit data as a result of concerns regarding the reporting of confidential patient data to an organisation without the necessary legislative mandate. However, these data accounted for a very small proportion of reported cases.13 During the past decade, the HIV and tuberculosis epidemics in South Africa have resulted in a re-direction of resources away from NCDs, which restricted operations that could be carried out by the NCR. As a result, the NCR continued to collect most pathology reports through low-cost passive surveillance activities. Due to this restriction on services, the NCR was unable to capture, code, and analyse data efficiently, resulting in a 10 year backlog of incidence reports.
Improvements, including the repositioning of cancer surveillance as a national health priority, stable NCR leadership (with an executive director and deputy director appointed during 2009–10), and extended collaborations and partnerships, have enabled the NCR to substantially reduce the backlog. Funding has been secured to recruit new staff, including six additional coders, a biostatistician, and an information technology (IT) developer (on a contract basis to interface NCR IT systems with its partners). With the additional staff, the backlog is expected to be within internationally accepted lag times for cancer registration by 2015–16. Internal quality control mechanisms have been implemented and the registry has increased its research output through collaborations with the IARC and the Centers for Disease Control and Prevention (CDC) in the USA. Through mentoring and technical support from the CDC’s Division of Cancer Prevention and Control, the NCR has been able to refine its research focus, mine the available data, and plan additional reports for publication.
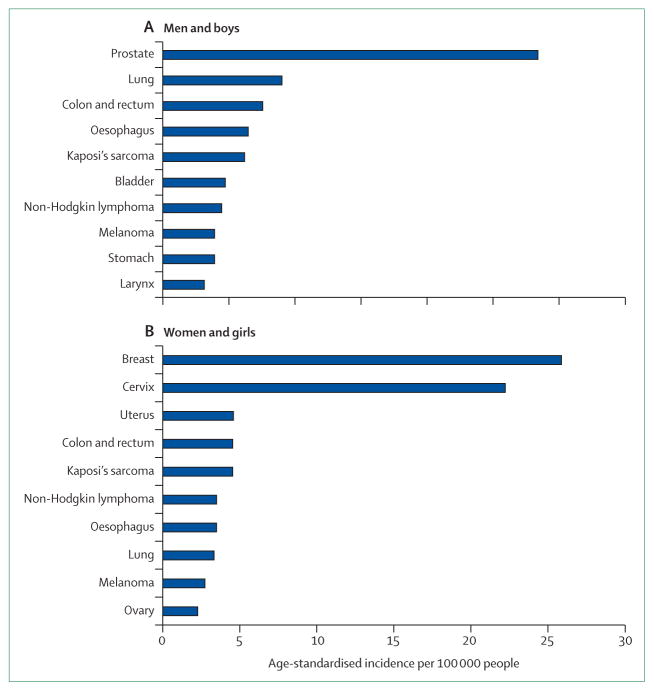
In 2008, 55 286 new cases of cancer were reported to the NCR (52% of these cases were in women and girls).14 Overall, the lifetime risk for cancer is one in eight for men and one in nine for women in South Africa. Age-standardised incidences for the top ten cancers in men and women for 2008 are shown in the figure, excluding basal and squamous cell carcinomas of the skin and cancers with an unknown primary site. The top five primary cancer sites for women and girls were breast, cervical, uterine, colon and rectum, and Kaposi’s sarcoma, whereas the top five primary cancer sites for men were prostate, lung, colon and rectum, oesophagus, and Kaposi’s sarcoma. Although variation was seen across subpopulations, the most noteworthy finding was the high incidence of cervical cancer in black women and girls and the high incidence of Kaposi’s sarcoma (linked to HIV infection) in both black men and boys, and black women and girls. Kaposi’s sarcoma was the second most common cancer in black men and boys and third most common cancers in black women and girls.14 However, there are limitations to this pathology-based data as the number of clinically diagnosed cases may have been underestimated, and pathology-based data was not linked to mortality data.
Figure.
Age-standardised incidences (per 100 000) of the top ten cancers by sex from the pathology-based National Cancer Registry, South Africa, 2008
Eastern Cape Province Cancer Registry
In 1981, the Medical Research Council of South Africa established a small population-based cancer registry in the former Transkei region of the Eastern Cape Province.15 The Programme on Mycotoxin and Experimental Carcinogenesis has since become known as the Eastern Cape Province Cancer Registry. The registry was initially developed to investigate oesophageal cancer incidence, but has expanded to include all diagnosed cancers.16 Just over 1 million people in eight magisterial districts are covered by the registry,17 which includes 15 hospitals and one public health-care laboratory.16 The Eastern Cape Province Cancer Registry is not networked to the NCR, and does not report to it at present.
The registry reported 2808 malignancies from 2003 to 2007, with 60·3% of these cancers diagnosed in women and girls. About 68% of cases were histologically or cytologically confirmed, highlighting the high availability of pathology services in South Africa. However, 54% of these cases were recorded in hospitals outside the catchment area, suggesting poor availability of cancer diagnostic and management services in the largely rural area of the Eastern Cape, as well as highlighting the high mobility of its population.17
The most common cancers in this region were oesophageal, prostate, and lung cancers in men and oesophageal, cervical, and breast cancers in women. This region of South Africa has some of the highest oesophageal cancer incidence rates in the world, and accounts for the difference between the Eastern Cape Province Cancer Registry top cancer rankings and the NCR data.17,18
Limitations of this registry include a high proportion of the black population living a non-urbanised lifestyle. This might explain the differences in patterns of cancer reported for the national population, as other populations and socioeconomic groups are under-represented in the Eastern Cape sample. The structure of the catchment population is characteristic of a migrant community, with an excess of older women and children, and a shortage of working age adults, particularly men.16 Most migrant workers are thought to seek health care in their province of work rather than their rural home province, resulting in a shortfall in the number of cancers reported, especially for men, in the Eastern Cape Registry.16 Additionally, HIV prevalence among South African women is highest nationally in the economically active age group of 30–34 years.19 In view of the deficit of working age adults in the catchment population of this registry, the pattern of HIV-related cancers might not be a true representation of South Africa as a whole. Finally, the scarcity of screening and diagnostic health-care services in this area suggests that there is an under-diagnosis of cancers in general. Nevertheless, this registry provides a unique and valuable insight on cancer epidemiology in a difficult-to-reach population. The quality of these data has been validated through its inclusion in the 2013 IARC publication.20
South African Paediatric Tumour Registry
The South African Paediatric Tumour Registry was initiated in 1987 to collect and classify malignancies in individuals younger than 15 years. Since other registries reported adult and childhood cancers together, specific nuances in the epidemiology of childhood cancers might have been missed; therefore, there was a need for a childhood-specific cancer registry. The registry acts as a central repository for paediatric oncology units across the country, including oncologists and other interested parties in private practice. The South African Paediatric Tumour Registry has previously been hosted at various paediatric oncology units in the country and, at the time of writing, is currently at Stellenbosch University in the Western Cape Province of South Africa. It is staffed by four part-time employees and is fully funded by private donors.21 An informal arrangement exists between the South African Paediatric Tumour Registry and the NCR whereby cases not reported to the NCR are provided by the South African Paediatric Tumour Registry for individuals younger than 15 years.
Annually, 500–700 cases are reported to the South African Paediatric Tumour Registry. Between 2003 and 2007, the registry reported yearly incidence figures between 33·4 and 47·2 cases per million, with leukaemia being the most common cancer in children aged 0–14 years.21 However, the number of childhood cancers might be lower than expected because of an under-reporting of cancer diagnosis for this patient population.21 This under-reporting might be the result of children dying before they seek health care, a failure to refer children to oncology centres at the appropriate time, and a failure to include cancers in the differential diagnosis. Low reporting figures could also be a result of childhood cancer cases being treated by adult oncologists in under-served areas, inadequate reporting from other paediatric subspecialists, and incomplete reporting from private paediatric oncologists.21 Although data from the South African Paediatric Tumour Registry are regularly presented at national and international meetings, formal reporting on a routine basis would help clarify the epidemiology of childhood cancers across the country. However, the South African Paediatric Tumour Registry remains an important source of data for researchers in the paediatric oncology field since it records clinical cases treated by paediatric oncologists.
Rationale for the South African cancer surveillance programme
Present cancer surveillance systems in South Africa are restricted to pathology-based national surveillance programmes and smaller, independent clinical-based registries that do not formally report to the NCR. These registries do not have the resources to collect robust cancer incidence data, which can be used to estimate national cancer incidence. As a result, policy makers and researchers are committed to implementing a network of population-based cancer registries representative of the ethnic and geographical diversity of the South African population, and provide a reliable indication of cancer incidence for the entire country.
The following sections outline the environmental changes that provided the platform for the development and implementation of population-based cancer registries, the practical challenges faced, and the lessons learned.
Population-based cancer registries in South Africa: an update
Policy, systems, and environmental changes
In 2011, the South African Department of Health created Regulation No 380 of the National Health Act (Act 61 of 2003),22 which formally established the NCR as its delegated agency for the collection of cancer surveillance information. Importantly, the regulation made cancer a reportable disease with every health-care worker obligated to report confirmed cancers to the NCR. The regulation raised the profile of cancer surveillance and the NCR in South Africa, and provided legislative protection for reporting sources. To ensure that South African cancer surveillance activities were in line with the rest of the world, the regulation mandated the NCR to establish population-based cancer registries for the country. Together with the regulation, a data collection form was published necessitating the provision of patient demographic, clinical, and risk factor information, including HIV status, and a detailed description of tumour pathology.
In 2012, the appointment of the National Advisory Committee on the Prevention and Control of Cancer affirmed the commitment of the Ministry of Health to cancer health-care reforms. Representation from the NCR presented the opportunity for policy makers to share solutions to cancer surveillance issues. Since then, the NCR has become a permanent agenda item at the committee’s meetings.
Imminent reforms in health-care financing in South Africa, in the form of the National Health Insurance,23 aim to improve access to health care for all South Africans. This reform has the potential to improve cancer screening and diagnosis, resulting in more complete cancer surveillance estimates from the NCR.
Public–private partnerships were crucial in the formation of population-based cancer registries in the resource-restricted public health-care sector in South Africa. The NCR developed a 10 year business plan for a phased-in approach towards four fully operational population-based cancer registries. This business plan was proposed to the pharmaceutical, medical insurance, and private laboratory industries in South Africa to raise funds. Many private partners recognised the value of population-based cancer surveillance data for the South African public and private health-care systems and committed support to this initiative with no expectation other than the production of reliable cancer surveillance data in South Africa. However, the sustainability of the cancer surveillance programme is reliant on a long-term funding commitment from both South Africa’s National Department of Health and private partnerships.
Appropriate and effective leadership is essential for the success of national cancer surveillance. After 7 years without a director, the NCR appointed an executive director in 2009, ensuring a new strategic direction for the organisation, improving work processes and raising staff morale. Manual, labour-intensive tasks were replaced by electronic methods, and relationships with private sector laboratories were renewed. Additionally, the NCR established relationships with international organisations such as IARC, the African Cancer Registry Network, which serves as IARC’s regional Hub for Cancer Registration in Africa, and the CDC in the USA, which has provided research support and mentoring to NCR researchers. Support from these organisations has been crucial in the planning of cancer surveillance activities and research agenda by the NCR.
Finally, the Ministry of Health has committed to establishing South Africa’s first National Public Health Institute, incorporating surveillance on communicable diseases and NCDs, and injury prevention.24 The institute will be modelled on the CDC in the USA. The NCR will be a core element of this new institute, benefiting from and contributing to the skills available in other surveillance divisions.
Legislative and system changes have provided a supportive environment for the establishment of population-based cancer registries in South Africa and the revitalisation of the pathology-based cancer surveillance system.
Implementation
We expect that the implementation of population-based cancer registries will provide the best resource for national incidence estimates in South Africa, and will mitigate the limitation of present pathology-based surveillance systems caused by the under-reporting of cancers that have not been biopsied.
The establishment of population-based cancer registries in South Africa was based on the framework provided by IARC.12,25 In principle, the framework suggests that population-based cancer registries should be established within a clearly defined district with a distinct catchment area and known population size.25 Ideally, the district should include the referral hospital or hospitals. The catchment population should be representative of the geographical and ethnic diversity of the country.
The population of South Africa is large and ethnically diverse. Overall, 80% of the South African population is black African, 8·8% mixed race (ancestral components including Khoisan, African, European, and Asian),26 8·4% white, and 2·5% Asian or Indian. The distribution of population groups, disease burdens, mortality, and life expectancy vary by province.4 The South African population-based cancer registry programme was able to meet some, but not all, of the IARC criteria in the local context.
In view of the size of the South African population, an estimated minimum of four population-based cancer registries will be needed to confidently extrapolate national cancer incidence. Each registry will have a catchment population of between 1·5 and 3 million inhabitants, and, together, will represent fully the ethnic and geographical diversity of the South African population. These regional registries will report annually to the NCR. Districts in the Western Cape province (largely white and mixed-race communities), and the Eastern Cape province (rural communities), a National Health Insurance Pilot Site23 (a resource-poor setting), and the Ekurhuleni Metropolitan District (ethnically and socioeconomically diverse communities) were selected as the sites for the four population-based cancer registries. Plans for the Eastern Cape province consist of increasing capacity of the present Eastern Cape Province cancer registry.
Challenges and opportunities
The first population-based cancer registry in the Ekurhuleni district was established in 2012, and revealed many of the challenges and successes of attempting to implement the IARC framework for population-based cancer registries in South Africa.
Ekurhuleni Metropolitan Municipality in the Gauteng Province is home to 3·1 million inhabitants.2 Of the total population, 79·0% are black African, 15·9% are white, 2·7% mixed race, and 2·2% Indian. Women and girls represent 49·3% of the population.27 The district has six government hospitals and eight private health-care facilities. Patients using public health-care facilities are diagnosed in the district but referred outside of the district for investigation and treatment to three tertiary or quaternary academic hospitals in Gauteng. Thus, case ascertainment for this population-based cancer registry will need data collection outside the municipality at the three large referral hospitals (between 800 and 3200 beds per hospital). This will probably be the case for many of the population-based cancer registries in South Africa because of the arrangement of the South African health system.
Access to private hospitals and oncology practices has proved a challenge for the NCR in Ekurhuleni. Although large hospital groups have been receptive to the idea of data provision, independent practitioners have been less enthusiastic to provide data. Issues of patient consent, confidentiality, and time needed to accommodate data collection have been raised with the NCR. Considerable relationship building and education is needed between the NCR and individual private practitioners to allow NCR staff access to the practices.
Active surveillance will be used in the Ekurhuleni population-based cancer registry, with field workers visiting private and public hospitals to extract relevant information about confirmed cases of cancer from patient records. Despite the legislation being in place, and as the NCR has experienced, passive surveillance that relies on health-care workers to notify patients with cancer has been unsuccessful. In the future, the support of local health-care departments will be invaluable in facilitating robust reporting.
The absence of central electronic information systems in public health-care sector creates a challenge to case ascertainment. Two options are available: to access files in the central medical records department of each hospital or to collect discharge files from each ward before they are stored in central medical records. The second option, although more labour intensive (requiring field workers to visit each ward), is preferred for completeness of registration, since locating hard copy medical files in the records department of larger hospitals can often be challenging.
Data capturing will ideally be accomplished using the IARC free software, CanReg. However, this software will need substantial modification of the data input section to accommodate the reporting form legislated for South Africa.
An NCR champion has proved to be very useful in the development of population-based cancer registries. In the development of a population-based cancer registry in the Ekurhuleni Metropolitan Municipality, this has been a senior oncologist with a special interest in cancer registration who has a good network of colleagues in the district. The individual is responsible for encouraging colleagues to report cancer cases, raising awareness of cancer registration, and answering queries about registry entries. In the future, a regional expert committee will be convened to help access data sources, encourage reporting, and provide scientific advice to a district’s population-based cancer registry.
Search strategy and selection criteria.
We used Pubmed and Google Scholar to search for abstracts, articles, policy documents, and reports describing present and previous cancer surveillance activities in South Africa and related health-care legislation between 1994 and 2014. Only articles published in English were included. We searched for the following keywords: “cancer registration”, “cancer registry”, “cancer policy”, “cancer surveillance”, “population-based cancer registration”, “non-communicable diseases”, “NCD’s”, “Eastern Cape Province Cancer Registry”, “South African Paediatric Tumour Registry”, “childhood cancer”, and “South Africa”. We identified peer-reviewed published work with possible descriptions of cancer surveillance or registration systems and results for South Africa. Additionally, we identified policy and legislative documents directly or indirectly affecting cancer surveillance and cancer registration in South Africa. We manually searched for cancer policy or legislation in South Africa, which we cross-referenced for identified articles. We included studies relevant to the scope of the Series paper and the local context.
Outcomes
The model we have produced of four independent but linked population-based cancer registries reporting to the NCR will hopefully result in the production of nationally representative cancer incidence estimates for the country. The cancer burden will be described according to specific cancer type, geographical location, ethnic origin, age, and sex. Additionally, depending on the availability of the information in the medical records, risk factor information such as HIV status, occupation, alcohol, and smoking history will be available. However, the usefulness of these risk factors will need to be tested in the Ekurhuleni population-based cancer registry. To be useful for cancer risk analysis, variables will need to be available for 80–90% of patients.12 We expect HIV status to be the most widely available risk factor in medical records, with other risk factors having poorer availability. Furthermore, simple treatment information is requested in the notification form with a tick box for different treatment modalities.
The data provided by the population-based surveillance system could allow for policy development and appropriate planning and placement of cancer diagnostic and management facilities. In South Africa, the use of data to assess primary prevention programmes such as the implementation of the human papillomavirus (HPV) vaccination, which was rolled out in South Africa for the first time in March, 2014, is particularly important.28 Population-based cancer registry data might provide an understanding of the long-term effect of HPV vaccination through comparison of baseline and post-vaccination cervical cancer incidences. Additionally, population-based cancer registries could provide the first population-level data to track cancer treatment, which will assist in the development of standardised treatment regimens for various cancers.
Monitoring and evaluation
The population-based cancer registries will strive to meet IARC quality standards. Monitoring and assessment will include the generally accepted variables of completeness, comparability, validity, and timeliness.29 Semiquantitative methods, such as the mortality–incidence ratio and the proportion of cases that have been morphologically verified, will be used to measure completeness of cancer registration in each population-based cancer registry.29,30 Additionally, data consistency will be assessed in-house through the comparison of annual incidence to long-term trends to detect unusual increases or decreases. Comparison with the pathology-based registry to identify data gaps will be essential. Regular reports of estimated national cancer incidence will be produced by the NCR using data from individual population-based cancer registries. These will be disseminated to individual population-based cancer registries, the Department of Health, other partners, and stakeholders, and will also be available online for public access.
The completeness of South Africa’s national death registration system has been rated as satisfactory with limitations noted in certification and coding of causes of death.31 Access to identifiable death notification data is crucial for the population-based cancer registries to compare data with the registry cancer reports. However, legislation pertaining to the confidentiality of death certificates has presented challenges in accessing this information. The NCR is in negotiations with the relevant authorities to help facilitate this process. Important aspects of this negotiation will be the Regulations Relating to Cancer Registration,22 which gives the NCR permission to collect all information about cancer in the country, and the security and confidentiality measures in place to safeguard data. Once the population-based cancer registry programme is granted access to this mortality data, the death certificate method of calculating completeness will be applied.29
Validity and comparability of data will be assessed using methods described in previously published work.30 The registry will aim to publish cancer incidence data for the country within a worldwide accepted lag period of 3–5 years.25 Additionally, guidance on the monitoring and assessment of registry activities will be sought from the African Cancer Registry Network and its partner registries.
Lessons learned
The prioritisation of cancer, public–private partnerships, and effective leadership has been essential to the revival of the pathology-based registry and the implementation of population-based cancer registries in South Africa. The introduction of legislation, the establishment of the National Advisory Committee on Cancer Prevention and Control, and support from the National Department of Health has been invaluable in ensuring the evolution of these processes. Although drafting legislation for cancer surveillance programmes is a local matter, international expertise in the design of the data collection form would have been constructive. In addition, piloting the design of the collection form before formal declaration of the legislation would have been beneficial to help with implementation of data collection.
The NCR has learned that although the support of cancer surveillance legislation is essential for establishing the registry, it is insufficient on its own to guarantee stakeholder engagement. Considerable relationship-building, networking, and stakeholder consultation with health-care professionals has been necessary. In this regard, support from the oncology community has been very important in creating and maintaining these partnerships.
A common understanding among stakeholders (including politicians, Department of Health officials, cancer surveillance staff, and academics) of the definition of population-based registration, the scope of the registration area (national vs regional), the climate and environment within which the registry is operating (eg, cooperation from health-care workers), and the resources needed to establish the population-based cancer registry programme is essential. Many delays can be avoided if there is a mutual understanding among all partners and stakeholders at the beginning of the process, which will in turn lend itself to the development of a shared vision that is supported and accepted by all included.
Conclusion
As the future of cancer surveillance in South Africa lies in the establishment of a network of nationally representative, population-based cancer registries, the National Department of Health and the South African NCR are working to establish population-based cancer surveillance in four regions of the country, strategically chosen to replicate the diversity of the national population. The population-based registries will run in parallel with the established pathology-based cancer surveillance system, which has produced national cancer incidence data for the past 28 years. We expect that these simultaneous efforts will provide a robust and efficient cancer surveillance system in South Africa.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Contributors
ES conceptualised the paper, contributed to the literature review, and wrote the manuscript. JMU, CB, PK, and MS contributed to the writing, content, and review of the manuscript. MS, MB, and LK performed the literature review and wrote the search strategy. All authors approved the final version of the manuscript.
Declaration of interests
We declare no competing interests.
References
- 1.Alleyne G, Binagwaho A, Haines A, et al. and the Lancet NCD Action Group. Embedding non-communicable diseases in the post-2015 development agenda. Lancet. 2013;381:566–74. doi: 10.1016/S0140-6736(12)61806-6. [DOI] [PubMed] [Google Scholar]
- 2.Bray F, Jemal A, Grey N, Ferlay J, Forman D. Global cancer transitions according to the Human Development Index (2008–2030): a population-based study. Lancet Oncol. 2012;13:790–801. doi: 10.1016/S1470-2045(12)70211-5. [DOI] [PubMed] [Google Scholar]
- 3.International Agency for Research on Cancer. GLOBOCAN 2012. [accessed Dec 19, 2014];Cancer incidence, mortality and prevalence worldwide. 2014 http://globocan.iarc.fr/pages/burden_sel.aspx.
- 4.Statistics South Africa. Statistical release P0302 mid year population estimates. Pretoria: Statistics South Africa; 2014. [Google Scholar]
- 5.Petrie D, Tang KK. Relative health performance in BRICS over the past 20 years: the winners and losers. Bull World Health Organ. 2014;92:396–404. doi: 10.2471/BLT.13.132480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coovadia H, Jewkes R, Barron P, Sanders D, McIntyre D. The health and health system of South Africa: historical roots of current public health challenges. Lancet. 2009;374:817–34. doi: 10.1016/S0140-6736(09)60951-X. [DOI] [PubMed] [Google Scholar]
- 7.Rao KD, Petrosyan V, Araujo EC, McIntyre D. Progress towards universal health coverage in BRICS: translating economic growth into better health. Bull World Health Organ. 2014;92:429–35. doi: 10.2471/BLT.13.127951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Department of Health, Republic of South Africa. HRH Strategy for the health sector: 2012/13–2016/17. Pretoria: Department of Health, Republic of South Africa; 2011. Human resources for health: South Africa. [Google Scholar]
- 9.Coustasse A, Hilsenrath P, Rojas P. The case of South African and Chilean health systems: comparison of financial, economic and health indicators. Internet J World Health Soc Polit. 2004:2. [Google Scholar]
- 10.Strachan B, Zabow T, van der Spuy Z. More doctors and dentists are needed in South Africa. S Afr Med J. 2011;101:523–28. [PubMed] [Google Scholar]
- 11.Mayosi BM, Flisher AJ, Lalloo UG, Sitas F, Tollman SM, Bradshaw D. The burden of non-communicable diseases in South Africa. Lancet. 2009;374:934–47. doi: 10.1016/S0140-6736(09)61087-4. [DOI] [PubMed] [Google Scholar]
- 12.Bray F, Znaor A, Cueva P, et al. Planning and developing population-based cancer registration in low- and middle-income settings. Lyon, France: International Agency for Research on Cancer; 2014. [PubMed] [Google Scholar]
- 13.Singh E, Underwood MJ, Nattey C, Babb C, Sengayi M, Kellett P. South African National Cancer Registry: effect of withheld data from private health systems on cancer incidence estimates. S Afr Med J. 2015;105:107–09. doi: 10.7196/SAMJ.8858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.South African National Cancer Registry. National Cancer Registry: Cancer in South Africa 2008. Johannesburg: 2014. [accessed Dec 15, 2014]. http://www.ncr.ac.za. [Google Scholar]
- 15.African Cancer Registry Network. [accessed Aug 4, 2014];Eastern Cape Province Registry. http://afcrn.org/membership/members/84-promec.
- 16.Somdyala NIM, Parkin DM, Sithole N, Bradshaw D. Trends in cancer incidence in rural Eastern Cape Province; South Africa, 1998–2012. Int J Cancer. 2015;136:E470–74. doi: 10.1002/ijc.29224. [DOI] [PubMed] [Google Scholar]
- 17.Somdyala N, Bradshaw D, Gelderblom W. Cancer incidence in selected municipalities of the Eastern Cape, 2003–2007. Cape Town: 2013. [Google Scholar]
- 18.Sewram V, Sitas F, O’Connell D, Myers J. Diet and esophageal cancer risk in the Eastern Cape Province of South Africa. Nutr Cancer. 2014;66:791–99. doi: 10.1080/01635581.2014.916321. [DOI] [PubMed] [Google Scholar]
- 19.National Department of Health. The 2012 National Antenatal Sentinel HIV and Herpes Simples Type-2 Prevalence Survey in South Africa. Pretoria: 2013. [accessed Oct 13, 2014]. http://www.hst.org.za/sites/default/files/ASHIVHerp_Report2014_22May2014.pdf. [Google Scholar]
- 20.Forman D, Bray F, Brewster DH, et al. Cancer incidence in five continents. X. Lyon, France: International Agency for Research on Cancer; 2013. [Google Scholar]
- 21.Stefan DC, Stones DK. The South African Paediatric Tumour Registry—25 years of activity. S Afr Med J. 2012;102:605–06. doi: 10.7196/samj.5719. [DOI] [PubMed] [Google Scholar]
- 22.Department of Health SA. Regulations Relating to Cancer Registration; Regulation No 380. Pretoria, South Africa: National Department of Health; Republic of South Africa; 2011. [Google Scholar]
- 23.National Department of Health. National Health Insurance in South Africa: Green Paper. Dep. Heal. Repub; South Africa: 2011. pp. 1–59. [Google Scholar]
- 24.Kahn T. Revamp for debt-ridden national health labs. [accessed Jan 12, 2015];Business Day Live. 2014 Sep 22; http://www.bdlive.co.za/national/health/2014/09/22/revamp-for-debt-ridden-national-health-labs.
- 25.Jensen O, Parkin DM, MacLennan R, Muir C, Skeet R. Cancer registration: principles and methods. Lyon, France: International Agency for Research on Cancer; 1991. [Google Scholar]
- 26.de Wit E, Delport W, Rugamika CE, et al. Genome-wide analysis of the structure of the South African Coloured Population in the Western Cape. Hum Genet. 2010;128:145–53. doi: 10.1007/s00439-010-0836-1. [DOI] [PubMed] [Google Scholar]
- 27.Statistics South Africa. Census 2011 municipal report Gauteng, report no 03-01-55. Pretoria: Statistics South Africa; 2011. [Google Scholar]
- 28.SouthAfrica.info. [accessed Oct 7, 2014];SA targets cervical cancer with HPV vaccine campaign. 2014 Mar 13; http://www.southafrica.info/services/health/hpv-vaccine-130314.htm#.VVYNyPm6e70.
- 29.Parkin DM, Bray F. Evaluation of data quality in the cancer registry: principles and methods Part II. Completeness. Eur J Cancer. 2009;45:756–64. doi: 10.1016/j.ejca.2008.11.033. [DOI] [PubMed] [Google Scholar]
- 30.Bray F, Parkin DM. Evaluation of data quality in the cancer registry: principles and methods. Part I: comparability, validity and timeliness. Eur J Cancer. 2009;45:747–55. doi: 10.1016/j.ejca.2008.11.032. [DOI] [PubMed] [Google Scholar]
- 31.Joubert J, Rao C, Bradshaw D, Vos T, Lopez AD. Evaluating the quality of national mortality statistics from civil registration in South Africa, 1997–2007. PLoS One. 2013;8:e64592. doi: 10.1371/journal.pone.0064592. [DOI] [PMC free article] [PubMed] [Google Scholar]