Abstract
May-Thurner syndrome (MTS) is an anatomically variable condition resulting in compression of the left common iliac vein between the right common iliac artery and the underlying spine with subsequent development of a left deep vein thrombosis (DVT). Although this syndrome is rare, its true prevalence is likely underestimated. Mainly, clinical symptoms and signs include, but are not limited to, pain, swelling, venous stasis ulcers, skin pigmentation changes and post-thrombotic syndrome. Correct treatment is not well established and is based on clinical presentation. Staged thrombolysis with/without prophylactic retrievable inferior vena cava filter placement followed by angioplasty/stenting of the left iliac vein appears to be the best option in MTS patients with extensive DVT. The aim of this review is to present in a simple and didactic form all variable clinical presentations of MTS and to outline possible management within the current guidelines.
Keywords: May-Thurner Syndrome, DVT, endovascular treatment, thrombectomy, medical education
I. INTRODUCTION
May-Thurner Syndrome (MTS), otherwise known as iliac vein compression syndrome [1], is an anatomically variable condition of the left common iliac vein (LCIV) with outflow obstruction caused by the right common iliac artery compression against the lower lumbar vertebrae (Fig. 1). Right-sided MTS cases are definitively more rare but have also been reported [2,3] in the literature. The majority of patients with right-sided MTS are male which may be due to the shape of the male pelvis. Although numerous articles have described the left-sided and female predominance of MTS, no correlation has been found between right-sided MTS and male gender. Some Authors postulate that the conical shape of the male pelvis may predispose the right iliac vein to compression by the iliac artery. However Virchow was the first who described this condition in 1851 and noted that deep vein thrombosis (DVT) was five times more likely to occur in the left lower limb [4]. In 1906 Mcmurrich proposed a congenital aetiology for LCVI obstruction [5] while Ehrich and Krumbhaar postulated, instead, a degenerative change of a venous valve at or near the origin of the LCIV [6]. Compression of the left iliac vein with detailed anatomic description was later described by May and Thurner in 1958 [7]. Cockett and Thomas also reported this condition in 1965, illustrating the relation between iliac vein compression and post-thrombotic syndrome and for this reason it is also known as “Cockett syndrome” [1]. Compression of the left common iliac vein by the right common iliac artery is a frequent anatomic variant observed in 22–32% of cadavers [8]. Most MTS patients throughout the course of their lives have no symptoms and therefore no treatment is required. Some Authors have proposed using the term “May-Thurner anatomy” in patients without hemodynamic significance and reserve the term “May-Thurner syndrome” for cases with compromised venous flow [9].
Fig. 1:
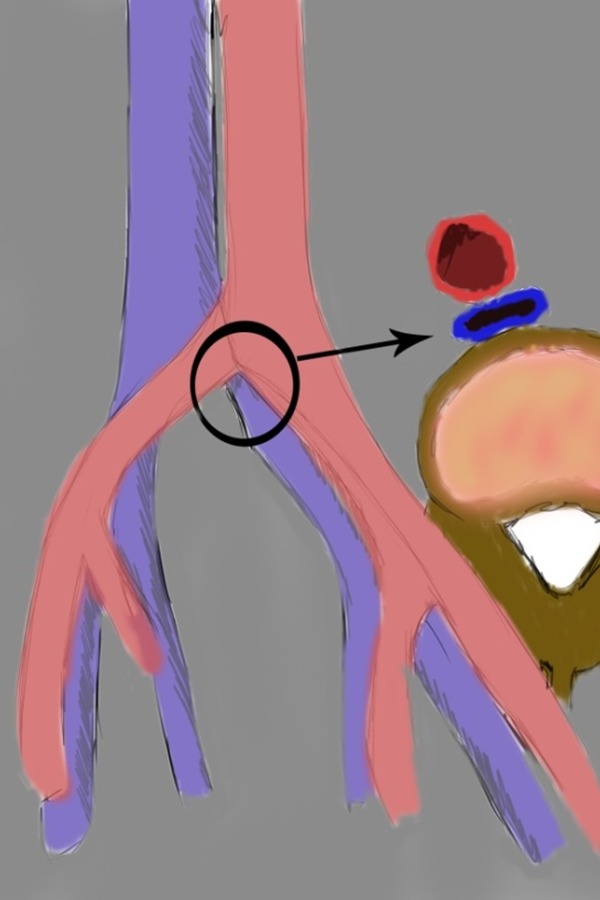
drawing showing left common iliac vein compression by right common iliac artery (morphologic type I).
II. METHODOLOGY
Clinical Manifestations
MTS usually presents in the second or third decade of life and is more common in women. The majority of these patients are asymptomatic. Once symptoms develop, patients can present during the acute or chronic MTS phase. Patients with acute manifestations most frequently (18–49% of cases) present with unilateral left lower LCIV thrombosis, swelling and pain [10]. Prolonged immobilization, dehydration, multiple pregnancies, the postpartum period, contraceptive therapy, surgical intervention for gynaecologic [11] and abdominal pathologic conditions [12] or febrile illness, including pneumonia and pleurisy [13,14,15], have been described as the main risk factors.
Acute MTS can be life-threatening if there is a spontaneous retroperitoneal hematoma associated with iliac vein rupture [16,17] or an associated pulmonary embolism (PE). However, it should be pointed out that these patients rarely present with PE probably because ilio-caval compression may offer protection by trapping large emboli [18]. Chronic MTS is the result of long-term venous hypertension and is characterized by chronic venous insufficiency (CVI), varicose veins, lower-extremity skin pigmentation changes (lipodermatosclerosis), chronic leg pain, recurrent skin ulcers [14], phlegmasia cerulea dolens [19], or recurrent superficial venous thrombophlebitis. Other MTS presentations include cryptogenic stroke in patients with a patent foramen ovale [20,21], pelvic congestion syndrome [22], or priapism [23].
Diagnostic techniques
Clinical information alone (history and physical examination) is insufficient for the diagnosis of MTS. A thrombophilia workup should always be performed to identify the risk factors for DVT, specifically in younger patients, and objective diagnostic testing is essential.
Non-invasive imaging modalities useful in the evaluation of MTS include color Doppler ultrasound, Computed Tomography (CT), Magnetic Resonance Imaging (MRI) and Intravascular Ultrasound (IVUS), while a useful invasive diagnostic test is contrast venography.
Color Doppler Ultrasound
The potential pitfalls of each of these diagnostic modalities must be recognized to avoid false interpretation. Over the years, because of its wide availability, portability and cost-effectiveness, ultrasound has been routinely used in the first-line evaluation of MTS patients, as it allows for a correct evaluation of the status of the deep veins of the extremity involved.
However the accuracy of ultrasonography in patients with MTS is not very convincing because of its lower sensitivity above the inguinal plane [24,19].
When visualization of the common iliac vein is possible, MTS may be diagnosed with trans-abdominal color Doppler ultrasound [25], but the overall sensitivity of US in visualization of the external iliac vein and common iliac vein is reportedly 79% and 47%, respectively [26]. If MTS is suspected in patients following ultrasound, cross-sectional imaging should be used to visualize the pelvic region.
In 2007 Labropoulos et al. [27] determined the following ultrasound criteria to detect a clinically substantial vein obstruction:
Color flow demonstrates mosaic flow, indicating post-stenotic turbulence due to proximal venous stenosis;
Pulse Doppler discloses absence of flow at the area of stenosis;
Continuous flow (absence of phasic blood blow);
Abnormal Valsalva response with continuous flow during Valsalva maneuver;
A peak vein velocity ratio of >2.5 across the stenosis.
Computed Tomography and Magnetic Resonance Imaging
CT and MRI, as compared with ultrasonography, yield markedly higher accuracy values.
There is no consensus about specific radiological signs however the most useful findings are:
Compression of the left common iliac vein by the right common iliac artery
Tortuous venous collaterals crossing the pelvis to drain into the contralateral veins
Thrombus formation.
Both CT and MRI have high sensitivity and specificity in the identification of DVT [28,29,30] of the venous compression and pelvic venous collaterals.
CT, particularly with a standardized protocol, is useful for a fast, comprehensive evaluation of the vascular system. [14]. Jeon et al. in 2010 investigated the potential role of CT venography by analyzing the morphologic features in predicting endovascular technical difficulties (fibrotic stenosis increase stent insertion) and long-term stent patency [31]. Three morphologic types of MTS have been individuated, each representing different stages of the obstruction: focal extrinsic compression, diffuse atrophy and cordlike obliteration, (Fig. 1,2,3).
Fig. 2:

drawing showing diffuse atrophy of left common iliac vein in May-Thurner Syndrome (morphologic type II).
Fig. 3:

drawing showing cordlike obliteration of left common iliac vein in May-Thurner Syndrome (morphologic type III)
The MRI, instead, permits accurate estimation of venous compression, length of obstruction and collateral vein network (Fig. 4a,b).
Fig. 4a:

MRI of 18 year-old women showing compression and thrombotic occlusion of the left iliac vein
Fig. 4b:

Subtracted maximum intensity projection coronal post contrast MRI showing dilated left pelvic collaterals.
The recent blood pool contrast agent “gadofosveset trisodium” has increased imaging resolution, sensitivity, specificity and accuracy versus the non-enhanced MR angiography and has not been shown to cause nephrogenic systemic fibrosis [32,33].
Intravascular Ultrasound
Intravascular US (IVUS) has been used successfully to demonstrate iliac vein compression. It allows assessment of the intimal changes, mural abnormalities (spurs), intraluminal webs and channels in the vessel wall and can help in treatment by guiding stent placement and sizing. [34,35,36]
Venography
The gold standard diagnostic test is contrast venography, but it is invasive, expensive, and the contrast can cause allergic reactions or post-injection DVT. Venography with the use of trans-venous pressure measurements is considered the modality of choice for diagnosing MTS. Simultaneous pressure measurements in both external iliac veins should be obtained. Normally the pressure is 5 to 6 mm Hg at rest while during exercise it measures 7 mm Hg. To diagnose a significant stenosis, the resting pressure gradient between the 2 iliac veins should be greater than 2 mm Hg at rest and greater than 3 mm Hg during exercise. Other authors measured the pressure in the lower inferior vena cava above the site of obstruction and performed pullback pressure studies and found these methods more valid than the above measurements [37].
Advantages and disadvantages of US, CT, MRI, IVUS and contrast-enhanced venography are summarized in Tables 1.
Table I:
Techniques for the diagnosis of May-Thurner syndrome
| Advantages | Disadvantages | |
|---|---|---|
| ULTRASOUND | Highly sensitive and specific for proximal lower extremity DVT Least expensive imaging method Non-invasive, portable, can be done at patient’s bedside Non-ionizing radiation hazards, hence ideal for young women |
Low sensitivity above the inguinal plane [25] Iliac vein thrombosis may be technically challenging to depict [25] Iliac vein compressibility may not be possible to assess [25] Operator dependent Pain, bandages, or casts may limit or prevent examination |
| CT | Non operator dependent High sensitivity and specificity MDCT allows multiplanar reconstruction of images with exquisite details More readily available and approachable compared to MRI Less expensive compared to MRI |
Radiation exposure Large volume of contrast agent required to achieve opacification of veins Contrast agent toxicity Limited resolution in the pelvic region due to bony artifacts |
| MRI ANGIOGRAPHY | Non operator dependent Better contrast resolution Non-ionizing radiation hazards, hence ideal for young women Direct multiplanar imaging Better safety profile of gadolinium-based contrast agents Useful in assessing the haemodynamic significance of venous compression as it has the ability to demonstrate retrograde flow [25,38,39] |
Contraindicated for patients with pacemakers and other metallic implants Not readily available High cost Metallic implant in the pelvis can create imaging artifacts |
| IVUS | Most sensitive and dynamic test to determine the degree of stenosis and to calibrate vessel before stent deployment During endovascular treatments facilitates accurate placement of a wire across the stenosis [40] |
Invasive Does not yield extra-vascular information |
| CATHETER VENOGRAPHY | Allows the assessment of haemodynamic Significance Allows treatment in the same setting Pressure gradients could be measured across the compression [41] |
Invasive Expansive Can cause allergic reactions or post-injection DVT Does not yield extra-vascular information |
Treatment
Treatment dependents on the presence of DVT [40]:
in the absence of DVT, conservative treatment is preferred;
in the presence of DVT, the standard therapy is anticoagulation with compression bandages.
Management strategies for the treatment of MTS are summarized in Table 2.
Table II:
Flow-chart of May-Thurner syndrome management

|
Pharmacological Treatment
Historically, the treatment for MTS patients has been anticoagulation therapy. Although anticoagulation prevents clot propagation, the existing clot and the underlying mechanical compression persist. Consequently, anticoagulation alone and thrombectomy with prospective anticoagulation yielded a recurrent thrombosis in up to 73% of patients with a venous spur [41,22 ].
Surgical Management
Surgical management can be offered with different surgical treatment methods. (Fig. 5).
Fig. 5:

drawing showing Palma operation with autologous saphenous vein graft
Today, MTS patients rarely undergo surgery management because endovascular techniques have been shown to have fewer operative risks [43,44]. For this reason, to date, the only indication for open surgery is failure of endovascular therapy.
Endovascular Management
Endovascular management should be the first-line treatment for MTS as demonstrated by retrospective and prospective studies [34,45,46,15,47]. Endovascular management typically begins with venography to confirm MTS and demonstrate the degree of LCIV stenosis followed by a percutaneous transluminal angioplasty (PTA) to expand the intraluminal space and finally the implantation of a self-expanding stent (Fig. 6).
Fig. 6:

drawing showing endovascular treatment with self-expanding stent placement in left common iliac vein
Some topics remain highly controversial:
The use of IVC filters.
If DVT is present, some practitioners suggest that a IVC filter should be placed [48,49].
However, recent Society for Vascular Survey (SVS) 2012 guidelines [50] do not recommend the placement of an IVC filter given the known long-term complications associated with IVC filters and the low risk for PE events of MTS.
Pharmacomechanical thrombolysis versus full anticoagulation alone.
SVS guidelines suggest the benefit of early intervention with percutaneous thrombolysis [50] while the American College of Chest Physicians guidelines suggest, instead, full anticoagulation alone over regional, systemic, or mechanical thrombolysis [51].
Some respected authorities today include staged thrombolysis in the treatment of MTS, especially in the presence of extensive iliofemoral DVT [52–56]
The superiority of a particular endovascular combination in long-term primary patency
Today it is well established that stent placement has higher patency rates than angioplasty [42] and that stainless steel stents are to be preferred to high radial force stents [57]. Brazeau et al. [58] examined various treatments but no specific treatment has yet demonstrated better outcomes.
Type of stent
As above-mentioned, iliofemoral venous stenting is now the primary treatment option for occlusions of the venous outflow tract. Today stenting has definitively replaced the open procedures that were utilized in the past and is often performed after pharmacological or mechanical thrombus removal. The first results of ilio-femoral venous stenting were reported during the early 1990s [59]. Since then technology in stent design has much improved. Zilver vena (Cook Medical, Bloomington, IN, USA) is one of the most recent stents on the market designed specifically for this purpose. It is a self-expandable nitinol stent that provides flexibility, consistent radial force and continuous stent to vein wall apposition from end to end. Zilver vena is currently available in 14 and 16 mm diameters and 60,100 and 140 mm lengths. Most often, this type of stent is delivered from the IVC to approximately the level of the lesser trochanter. Post-dilatation is usually performed up to the nominal diameter of the stent [60].
III. CONCLUSION
May-Thurner syndrome is a relatively rare entity and therefore knowledge of this syndrome associated with deep veins is essential. The aim of this study is to present, in a very didactic form, current management of this disorder, including diagnostic and interventional strategies. Endovascular techniques have evolved and now play a significant role in the treatment of May-Thurner syndrome. In the majority of individuals with May-Thurner syndrome it is believed that direct compression of the left iliac vein between the right iliac artery and fifth lumbar vertebrae predisposes to the formation of deep vein thrombi. The syndrome is thought to progress through 3 stages: (1) asymptomatic compression of the vein, (2) the development of intraluminal spurs (fibrous bands) at the site of compression and (3) development of deep vein thrombi. Spontaneous rupture of the LCIV is a rare occurrence.
IV. AKNOWLEDGMENT
The authors would like to thank Mrs. Juliet Ippolito for reviewing the English text of this paper.
REFERENCES
- 1.Cockett FB, Thomas ML. The iliac compression syndrome. Br J Surg. 1965;52(10):816–21. doi: 10.1002/bjs.1800521028. [DOI] [PubMed] [Google Scholar]
- 2.Burke RM, Rayan SS, Kasirajan K, Chaikof EL, Milner R. Unusual case of right-sided May-Thurner syndrome and review of its management. Vascular. 2006;14(1):47–50. doi: 10.2310/6670.2006.00012. [DOI] [PubMed] [Google Scholar]
- 3.Abboud G, Midulla M, Lions C, El Ngheoui Z, Gengler L, Martinelli T, Beregi JP. “Right-sided” May-Thurner syndrome. Cardiovasc Intervent Radiol. 2010;33(5):1056–9. doi: 10.1007/s00270-009-9654-z. [DOI] [PubMed] [Google Scholar]
- 4.Virchow R. Uber die Erweiterung Kleiner Gefasse. Arch Path Anat. 1851;3:427. [Google Scholar]
- 5.McMurrich JP. The occurrence of congenital adhesions in the common iliac veins, and their relation to thrombosis of the femoral and iliac veins. Am J Med Sci. 1908;135:342–6. [Google Scholar]
- 6.Ehrich WE, Krumbhaar EB. A frequent obstructive anomaly of the mouth of the left common iliac vein. American Heart Journal. 1943;26:18–31. [Google Scholar]
- 7.May R, Thurner J. The cause of the predominantly sinistral occurrence of thrombosis of the pelvic veins. Angiology. 1957;8(5):419–27. doi: 10.1177/000331975700800505. [DOI] [PubMed] [Google Scholar]
- 8.Kibbe MR, Ujiki M, Goodwin AL, Eskandari M, Yao J, Matsumura J. Iliac vein compression in an asymptomatic patient population. J Vasc Surg. 2004;39(5):937–43. doi: 10.1016/j.jvs.2003.12.032. [DOI] [PubMed] [Google Scholar]
- 9.Oguzkurt L, Tercan F, Pourbagher MA, Kizilkilic O, Turkoz R, Boyvat F. Computed tomography findings in 10 cases of iliac vein compression (May-Thurner) syndrome. Eur J Radiol. 2005;55(3):421–5. doi: 10.1016/j.ejrad.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 10.Lee KH, Han H, Lee KJ, Yoon CS, Kim SH, Won JY, Lee do Y. Mechanical thrombectomy of acute iliofemoral deep vein thrombosis with use of an Arrow-Trerotola percutaneous thrombectomy device. J Vasc Interv Radiol. 2006;17(3):487–95. doi: 10.1097/01.RVI.0000202611.93784.76. [DOI] [PubMed] [Google Scholar]
- 11.Im S, Lim SH, Chun HJ, Ko YJ, Yang BW, Kim HW. Leg edema with deep venous thrombosis-like symptoms as an unusual complication of occult bladder distension and right May-Thurner syndrome in a stroke patient: a case report. Arch Phys Med Rehabil. 2009;90(5):886–90. doi: 10.1016/j.apmr.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 12.Campsen J, Bang TJ, Kam I, Gupta R. May-Thurner syndrome complicating left-sided renal transplant. Transplantation. 2010;89(7):904–6. doi: 10.1097/TP.0b013e3181cd87ce. [DOI] [PubMed] [Google Scholar]
- 13.O’Sullivan GJ. The role of interventional radiology in the management of deep venous thrombosis: advanced therapy. Cardiovasc Intervent Radiol. 2011;34(3):445–61. doi: 10.1007/s00270-010-9977-9. [DOI] [PubMed] [Google Scholar]
- 14.Baron HC, Shams J, Wayne M. Iliac vein compression syndrome: a new method of treatment. Am Surg. 2000;66(7):653–5. [PubMed] [Google Scholar]
- 15.Patel NH, Stookey KR, Ketcham DB, Cragg AH. Endovascular management of acute extensive iliofemoral deep venous thrombosis caused by May-Thurner syndrome. J Vasc Interv Radiol. 2000;11(10):1297–302. doi: 10.1016/s1051-0443(07)61304-9. [DOI] [PubMed] [Google Scholar]
- 16.Jiang J, Ding X, Zhang G, Su Q, Wang Z, Hu S. Spontaneous retroperitoneal hematoma associated with iliac vein rupture. J Vasc Surg. 2010;52(5):1278–82. doi: 10.1016/j.jvs.2010.06.102. [DOI] [PubMed] [Google Scholar]
- 17.Bracale G, Porcellini M, D’Armiento FP, Baldassarre M. Spontaneous rupture of the iliac vein. J Cardiovasc Surg. 1999;40(6):871–5. [PubMed] [Google Scholar]
- 18.Chan KT, Popat RA, Sze DY, Kuo WT, Kothary N, Louie JD, Hovsepian DM, Hwang GL, Hofmann LV. Common iliac vein stenosis and risk of symptomatic pulmonary embolism: an inverse correlation. J Vasc Interv Radiol. 2011;22(2):133–41. doi: 10.1016/j.jvir.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 19.Suwanabol PA, Tefera G, Schwarze ML. Syndromes associated with the deep veins: phlegmasia cerulea dolens, May-Thurner syndrome, and nutcracker syndrome. Perspect Vasc Surg Endovasc Ther. 2010;22(4):223–30. doi: 10.1177/1531003511400426. [DOI] [PubMed] [Google Scholar]
- 20.Kiernan TJ, Yan BP, Cubeddu RJ, Rengifo-Moreno P, Gupta V, Inglessis I, Ning M, Demirjian ZN, Jaff MR, Buonanno FS, Schainfeld RM, Palacios IF. May-Thurner syndrome in patients with cryptogenic stroke and patent foramen ovale: an important clinical association. Stroke. 2009;40(4):1502–4. doi: 10.1161/STROKEAHA.108.527366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Greer DM, Buonanno FS. Cerebral infarction in conjunction with patent foramen ovale and May-Thurner syndrome. J Neuroimaging. 2001;11(4):432–4. doi: 10.1111/j.1552-6569.2001.tb00074.x. [DOI] [PubMed] [Google Scholar]
- 22.Rastogi N1, Kabutey NK, Kim D. Incapacitating pelvic congestion syndrome in a patient with a history of May-Thurner syndromeand left ovarian vein embolization. Ann Vasc Surg. 2012;26(5):732.e7–11. doi: 10.1016/j.avsg.2011.08.029. [DOI] [PubMed] [Google Scholar]
- 23.Alhalbouni S, Deem S, Abu-Halimah S, Sadek BT, Mousa A. Atypical presentation of priapism in a patient with acute iliocaval deep venous thrombosis secondary to May-Thurner syndrome. Vasc Endovascular Surg. 2013;47(6):488–92. doi: 10.1177/1538574413493680. [DOI] [PubMed] [Google Scholar]
- 24.Shebel ND, Whalen CC. Diagnosis and management of iliac vein compression syndrome. J Vasc Nurs. 2005;23:10–17. doi: 10.1016/j.jvn.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 25.Oğuzkurt L, Ozkan U, Tercan F, Koç Z. Ultrasonographic diagnosis of iliac vein compression (May-Thurner) syndrome. Diagn Interv Radiol. 2007;13(3):152–5. [PubMed] [Google Scholar]
- 26.Messina LM, Sarpa MS, Smith MA, Greenfield LJ. Clinical significance of routine imaging of iliac and calf veins by color flow duplex scanning in patients suspected of having acute lower extremity deep venous thrombosis. Surgery. 1993;114(5):921–7. [PubMed] [Google Scholar]
- 27.Labropoulos N, Borge M, Pierce K, Pappas PJ. Criteria for defining significant central vein stenosis with duplex ultrasound. J Vasc Surg. 2007;46(1):101–7. doi: 10.1016/j.jvs.2007.02.062. [DOI] [PubMed] [Google Scholar]
- 28.McDermott S, Oliveira G, Ergül E, Brazeau N, Wicky S, Oklu R. May-Thurner syndrome: can it be diagnosed by a single MR venography study? Diagn Interv Radiol. 2013;19(1):44–8. doi: 10.4261/1305-3825.DIR.5939-12.1. [DOI] [PubMed] [Google Scholar]
- 29.Molloy S, Jacob S, Buckenham T, Khaw KT, Taylor RS. Arterial compression of the right common iliac vein; an unusual anatomical variant. Cardiovasc Surg. 2002;10(3):291–2. doi: 10.1016/s0967-2109(01)00139-9. [DOI] [PubMed] [Google Scholar]
- 30.Morita S, Kimura T, Masukawa A, Saito N, Suzuki K, Mitsuhashi N. Flow direction of ascending lumbar veins on magnetic resonance angiography and venography: would “descending lumbar veins” be a more precise name physiologically? Abdom Imaging. 2007;32(6):749–53. doi: 10.1007/s00261-006-9166-0. [DOI] [PubMed] [Google Scholar]
- 31.Jeon UB, Chung JW, Jae HJ, Kim HC, Kim SJ, Ha J, Park JH. May-Thurner syndrome complicated by acute iliofemoral vein thrombosis: helical CT venography for evaluation of long-term stent patency and changes in the iliac vein. AJR Am J Roentgenol. 2010;195(3):751–7. doi: 10.2214/AJR.09.2793. [DOI] [PubMed] [Google Scholar]
- 32.McGregor R, Vymazal J, Martinez-Lopez M, Neuwirth J, Salgado P, Beregi JP, Peduto A, de la Pena-Almaguer E, Slater GJ, Shamsi K, Parsons EC., Jr A multi-center, comparative, phase 3 study to determine the efficacy of gadofosveset-enhanced magnetic resonance angiography for evaluation of renal artery disease. Eur J Radiol. 2008;65(2):316–25. doi: 10.1016/j.ejrad.2007.03.018. [DOI] [PubMed] [Google Scholar]
- 33.Nikolaou K, Kramer H, Grosse C, Clevert D, Dietrich O, Hartmann M, Chamberlin P, Assmann S, Reiser MF, Schoenberg SO. High-spatial-resolution multistation MR angiography with parallel imaging and blood pool contrast agent: initial experience. Radiology. 2006;241(3):861–72. doi: 10.1148/radiol.2413060053. [DOI] [PubMed] [Google Scholar]
- 34.Ahmed HK, Hagspiel KD. Intravascular ultrasonographic findings in May-Thurner syndrome (iliac vein compression syndrome) J Ultrasound Med. 2001;20(3):251–6. doi: 10.7863/jum.2001.20.3.251. [DOI] [PubMed] [Google Scholar]
- 35.J Forauer AR, Gemmete JJ, Dasika NL, Cho KJ, Williams DM. Intravascular ultrasound in the diagnosis and treatment of iliac vein compression (May-Thurner) syndrome. Vasc Interv Radiol. 2002;13(5):523–7. doi: 10.1016/s1051-0443(07)61535-8. [DOI] [PubMed] [Google Scholar]
- 36.Butros SR, Liu R, Oliveira GR, Ganguli S, Kalva S. Venous compression syndromes: clinical features, imaging findings and management. Br J Radiol. 2013;86(1030):20130284. doi: 10.1259/bjr.20130284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gurel K, Gurel S, Karavas E, Buharalıoglu Y, Daglar B. Direct contrast-enhanced MR venography in the diagnosis of May-Thurner syndrome. Eur J Radiol. 2011;80(2):533–6. doi: 10.1016/j.ejrad.2010.04.033. [DOI] [PubMed] [Google Scholar]
- 38.Wu WL, Tzeng WS, Wu RH, Tsai WL, Chen MC, Lin PC, et al. Comprehensive MDCT evaluation of patients with suspected May– Thurner syndrome. Am J Roentgenol. 2012;199:W638–45. doi: 10.2214/AJR.11.8040. [DOI] [PubMed] [Google Scholar]
- 39.Oguzkurt L, Ozkan U, Ulusan S, Koc Z, Tercan F. Compression of the left common iliac vein in asymptomatic subjects and patients with left iliofemoral deep vein thrombosis. J Vasc Interv Radiol. 2008;19:366–70. doi: 10.1016/j.jvir.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 40.Wolpert LM, Rahmani O, Stein B, Gallagher JJ, Drezner AD. Magnetic resonance venography in the diagnosis and management of May-Thurner syndrome. Vasc Endovascular Surg. 2002;36(1):51–7. doi: 10.1177/153857440203600109. [DOI] [PubMed] [Google Scholar]
- 41.Burroughs KE. New considerations in the diagnosis and therapy of deep vein thrombosis. South Med J. 1999;92(5):517–20. doi: 10.1097/00007611-199905000-00014. [DOI] [PubMed] [Google Scholar]
- 42.Kim JY, Choi D, Guk Ko Y, Park S, Jang Y, Lee do Y. Percutaneous treatment of deep vein thrombosis in May-Thurner syndrome. Cardiovasc Intervent Radiol. 2006;29(4):571–5. doi: 10.1007/s00270-004-0165-7. [DOI] [PubMed] [Google Scholar]
- 43.Lamont JP, Pearl GJ, Patetsios P, Warner MT, Gable DR, Garrett W, Grimsley B, Smith BL, Shutze WP. Prospective evaluation of endoluminal venous stents in the treatment of the May-Thurner syndrome. Ann Vasc Surg. 2002;16(1):61–4. doi: 10.1007/s10016-001-0143-3. [DOI] [PubMed] [Google Scholar]
- 44.Mussa FF, Peden EK, Zhou W, Lin PH, Lumsden AB, Bush RL. Iliac vein stenting for chronic venous insufficiency. Tex Heart Inst J. 2007;34(1):60–6. [PMC free article] [PubMed] [Google Scholar]
- 45.Hager ES, You T, Tahara R, Dillavou E, AlKhoury G, Marone L, Makaroun M, Chaer RA. Outcomes of endovascular intervention for May-Thurner syndrome. J Vasc Surg: Venous and Lym Dis. 2013;1:270–5. doi: 10.1016/j.jvsv.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 46.O’Sullivan GJ, Semba CP, Bittner CA, Kee ST, Razavi MK, Sze DY, Dake MD. Endovascular management of iliac vein compression syndrome. J Vasc Interv Radiol. 2000;11:823–836. doi: 10.1016/s1051-0443(07)61796-5. [DOI] [PubMed] [Google Scholar]
- 47.Cil BE, Akpinar E, Karcaaltincaba M, Akinci D. Case 76: May-Thurner syndrome. Radiology. 2004;233(2):361–5. doi: 10.1148/radiol.2332030152. [DOI] [PubMed] [Google Scholar]
- 48.Reekers JA. Re: Current practice of temporary vena cava filter insertion: a multicenter registry. J Vasc Interv Radiol. 2000;11:1363e4. [PubMed] [Google Scholar]
- 49.Lorch H, Welger D, Wagner V, et al. Current practice of temporary vena cava filter insertion: a multicenter registry. J Vasc Interv Radiol. 2000;11:83e8. doi: 10.1016/s1051-0443(07)61287-1. [DOI] [PubMed] [Google Scholar]
- 50.Meissner MH, Gloviczki P, Comerota AJ, Dalsing MC, Eklof BG, Gillespie DL, Lohr JM, McLafferty RB, Murad MH, Padberg F, Pappas P, Raffetto JD, Wakefield TW, Society for Vascular Surgery. American Venous Forum Early thrombus removal strategies for acute deep venous thrombosis: clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J Vasc Surg. 2012;55:1449e62. doi: 10.1016/j.jvs.2011.12.081. [DOI] [PubMed] [Google Scholar]
- 51.Metersky ML, Nathanson I. Introducing the future of ACCP Clinical Practice Guidelines. Chest. 2012;141:285e6. doi: 10.1378/chest.11-2906. [DOI] [PubMed] [Google Scholar]
- 52.Vedantham S, Vesely TM, Sicard GA, Brown D, Rubin B, Sanchez LA, Parti N, Picus D. Pharmacomechanical thrombolysis and early stent placement for iliofemoral deep vein thrombosis. J Vasc Interv Radiol. 2004;15:565e74. doi: 10.1097/01.rvi.0000127894.00553.02. [DOI] [PubMed] [Google Scholar]
- 53.Bush RL, Lin PH, Bates JT, Mureebe L, Zhou W, Lumsden AB. Pharmacomechanical thrombectomy for treatment of symptomatic lower extremity deep venous thrombosis: safety and feasibility study. J Vasc Surg. 2004;40:965e70. doi: 10.1016/j.jvs.2004.08.025. [DOI] [PubMed] [Google Scholar]
- 54.Lin PH, Zhou W, Dardik A, Mussa F, Kougias P, Hedayati N, Naoum JJ, El Sayed H, Peden EK, Huynh TT. Catheter-direct thrombolysis versus pharmacomechanical thrombectomy for treatment of symptomatic lower extremity deep venous thrombosis. Am J Surg. 2006;192:782e8. doi: 10.1016/j.amjsurg.2006.08.045. [DOI] [PubMed] [Google Scholar]
- 55.Neglen P, Darcey R, Olivier J, Raju S. Bilateral stenting at the iliocaval confluence. J Vasc Surg. 2010;51:1457e66. doi: 10.1016/j.jvs.2010.01.056. [DOI] [PubMed] [Google Scholar]
- 56.Hofmann LV, Kuo WT. Catheter-directed thrombolysis for acute DVT. Lancet. 2012;379:3e4. doi: 10.1016/S0140-6736(11)61875-8. [DOI] [PubMed] [Google Scholar]
- 57.Oguzkurt L, Tercan F, Ozkan U, Gulcan O. Iliac vein compression syndrome: outcome of endovascular treatment with long-term follow-up. Eur J Radiol. 2008;68(3):487–92. doi: 10.1016/j.ejrad.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 58.Brazeau NF, Harvey HB, Pinto EG, Deipolyi A, Hesketh RL, Oklu R. May-Thurner syndrome: diagnosis and management. Vasa. 2013;42(2):96–105. doi: 10.1024/0301-1526/a000252. [DOI] [PubMed] [Google Scholar]
- 59.Antonucci F, Salomonowitz E, Stuckmann G, Stiefel M, Largiadèr J, Zollikofer CL. Placement of venous stents: clinical experience with a self-expanding prosthesis. Radiology. 1992;183(2):493–7. doi: 10.1148/radiology.183.2.1561356. [DOI] [PubMed] [Google Scholar]
- 60.O’Sullivan GJ, Sheehan J, Lohan D, McCann-Brown JA. Iliofemoral venous stenting extending into the femoral region: initial clinical experience with the purpose-designed Zilver Vena stent. J Cardiovasc Surg. 2013;54(2):255–61. [PubMed] [Google Scholar]


