Abstract
PURPOSE
We hypothesized that lymphoid-selective host conditioning and subsequent adoptive transfer of sirolimus-resistant allogeneic T cells (T-Rapa), when combined with high-dose sirolimus drug therapy in vivo, would safely achieve anti-tumor effects while avoiding GVHD.
EXPERIMENTAL DESIGN
Patients (n=10) with metastatic renal cell carcinoma (RCC) were accrued because this disease is relatively refractory to high-dose conditioning yet may respond to high-dose sirolimus. A 21-day outpatient regimen of weekly pentostatin (P; 4 mg/m2/dose) combined with daily, dose-adjusted cyclophosphamide (C; ≤ 200 mg/day) was designed to deplete and suppress host T cells. After PC conditioning, patients received matched sibling, T cell-replete peripheral blood stem cell allografts and high-dose sirolimus (serum trough target, 20–30 ng/ml). To augment graft-versus-tumor (GVT) effects, multiple T-Rapa donor lymphocyte infusions (DLI) were administered (days 0, 14, and 45 post-transplant) and sirolimus was discontinued early (day 60 post-transplant).
RESULTS
PC conditioning depleted host T cells without neutropenia or infection and facilitated donor engraftment (10/10 cases). High-dose sirolimus therapy inhibited multiple T-Rapa DLI, as evidenced by stable mixed donor/host chimerism. No anti-tumor responses were detected by RECIST criteria and no significant classical acute GVHD was observed.
CONCLUSIONS
Immune-selective PC conditioning represents a new approach to safely achieve alloengraftment without neutropenia. However, allogeneic T cells generated ex vivo in sirolimus are not resistant to the tolerance-inducing effects of in vivo sirolimus drug therapy, thereby cautioning against use of this intervention in patients with refractory cancer.
INTRODUCTION
Allogeneic hematopoietic cell transplantation (HCT) is limited by conditioning toxicity, graft rejection, graft-versus-host disease (GVHD), and insufficient graft-versus-tumor (GVT) effects. Reduced-intensity conditioning decreases toxicity but promotes mixed chimerism(1) and graft rejection or tumor progression(2). Intensified post-HCT immune suppression or graft T cell depletion reduces GVHD but can decrease GVT effects(3); furthermore, donor lymphocyte infusion (DLI) using unmanipulated T cells can mediate GVT effects but also mediate GVHD(4). To address these limitations, we conducted a pilot clinical trial of immune-selective conditioning, in vivo sirolimus GVHD prophylaxis, and multiple infusions of DLI products manufactured ex vivo in sirolimus.
Conditioning varies from myeloablative to reduced-intensity to non-myeloablative(5). However, an ultra-low intensity platform that avoids any neutropenia has not been fully explored. Stem cell engraftment may not be fully reliant on conditioning-induced “marrow space”(6); we thus reasoned that non-neutropenic conditioning would permit stem cell engraftment if immunologic rejection was prevented. Conditioning also reduces tumor burden, but this rationale is weakened in chemotherapy refractory settings. Finally, because conditioning reduces graft rejection, it should be directed towards host T cells that primarily mediate rejection(7). An immune-selective regimen that avoided neutropenia would yield direct safety advantages and also reduce conditioning-related induction of GVHD(8).
We used pentostatin plus daily cyclophosphamide (Cy) conditioning that was personalized based on efficacy (absolute lymphocyte count [ALC] reduction) and safety (absolute neutrophil count [ANC] preservation). Pentostatin was used as transplant conditioning with neutropenia-inducing doses of total body irradiation(9, 10) or busulfan(11). Pentostatin plus bolus-dose Cy (600 mg/m2) caused neutropenia(12); as such, we used low-dose Cy (200 mg/day) and allowed Cy reductions depending upon achievement of ALC reduction targets. In a murine model, pentostatin plus daily Cy (PC) depleted and suppressed T cells and prevented marrow allograft rejection more effectively than fludarabine plus Cy(13). PC therapy also prevented murine sensitization to a foreign immunotoxin(14); in the clinic, PC therapy modulated immunity without neutropenia and facilitated immunotoxin therapy of mesothelioma(15).
We used rapamycin-resistant T cells (T-Rapa) for DLI therapy. Unmanipulated DLI mediate GVHD and have limited efficacy for treating malignancy(16) or promoting engraftment(17). Co-stimulated DLI products have previously been evaluated(18); recently, we evaluated DLI comprised of T-Rapa cells(19). Murine CD4+ T-Rapa cells were apoptosis-resistant, prevented rejection, and were effective against GVHD(20–22). In the previous trial, one T-Rapa infusion was associated with: conversion of mixed chimerism towards full donor elements; a low rate of acute GVHD; and GVT effects against lymphoid malignancy. In the current trial, we used T cell-replete allografts augmented with T-Rapa DLI at days 0, 14, and 45 post-HCT.
GVHD prophylaxis typically consists of a calcineurin inhibitor plus a second agent(23). Previously, we used cyclosporine plus short-course, standard-dose sirolimus through d 14 post-HCT. Sirolimus inhibits mTOR and thereby has an anti-tumor mechanism, including mediation anti-lymphoma effects post-HCT(24). Because the degree of mTOR inhibition correlates with sirolimus concentration(25), higher dosing may optimize anti-tumor effects. Sirolimus has substantial toxicity after intensive conditioning(26) or with calcineurin inhibitors(27). However, Campath plus high-dose sirolimus (target, 30 ng/ml) after non-myeloablative conditioning was safe and effective for GVHD prevention(28). We thus reasoned that high-dose, single-agent sirolimus would be safe after immune selective PC conditioning and represent adequate GVHD prophylaxis after T cell-replete transplant and multiple T-Rapa DLI.
We evaluated this therapy in refractory metastatic renal cell carcinoma (RCC), thereby providing a rationale for lymphocyte-specific conditioning intended for rejection abrogation rather than tumor reduction. Metastatic RCC is susceptible to an allogeneic GVT effect that is generally associated with GVHD, as described by the National Heart Lung and Blood Institute(29) and a summation report from 21 European countries(30). However, GVT effects were not observed in a separate study(31). Thus, more robust methods of harnessing GVT effects and modulating GVHD are required in RCC patients. Finally, metastatic RCC can respond to temsirolimus(32), thus suggesting that high-dose sirolimus might yield an anti-tumor benefit.
MATERIALS AND METHODS
Clinical Trial Design and Implementation
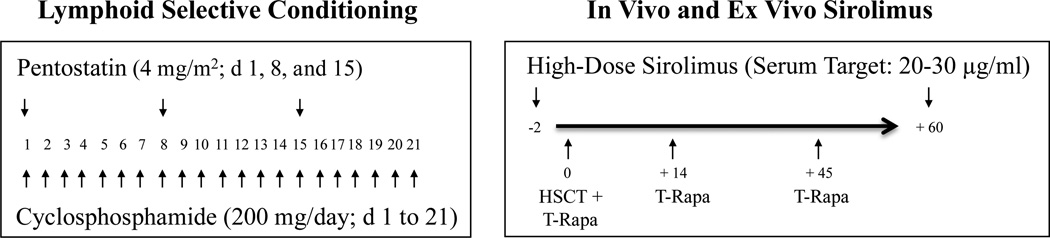
The trial (schema, Figure 1; ClinicalTrials.gov, NCT00923845) was approved by the National Cancer Institute (NCI) institutional review board and implemented according to an Investigational New Drug Application accepted by the Food and Drug Administration. On-study dates ranged from June 2008 to June 2010. Subjects were enrolled based on age (18–75 years), presence of metastatic renal cell carcinoma (any histology; active CNS disease excluded), availability of an eligible 6/6 HLA-matched sibling donor, history of nephrectomy, ≥ one prior systemic therapy, life expectancy ≥3 months, Karnofsky score ≥80, and adequate organ function. Patients received a 21-day course of pentostatin [Nipent®, Hospira; intravenous infusion on days 1, 8, and 15; 4 mg/m2/dose, adjusted for renal insufficiency] and oral Cy (200 mg flat dose/day). The protocol stated goal of PC therapy was to reduce the ALC (< 200 cells/µl) while preserving the ANC (> 1000 cells/µl). Cy was reduced or held if ALC reduction goals were met. Specifically, Cy was reduced to 100 mg per day if ALC values on days 8, 11, 15, or 18 were 251–499, 201–399, 151–299, or 101–199, respectively; Cy was held if ALC values on days 8, 11, 15, or 18 were ≤ 250, ≤ 200, ≤ 150, ≤ 100, respectively. Cy was also to be reduced for ANC values < 1000; however, this never occurred. After PC conditioning (“day -2”), patients started sirolimus (16 mg loading dose; then, 4 mg/day), with further dosing adjusted to achieve 20–30 ng/ml trough levels through day 60 post-HCT. On day 0, patients received a mobilized, T-cell replete allograft (>3 × 106 CD34+/kg) and the first infusion of T-Rapa cells (2.5 × 107 cells/kg), which were generated by a 12-day or 6-day culture, as previously described(19, 33); further T-Rapa cells (2.5 × 107 cells/kg) were administered at days 14 and 45 post-HCT.
Figure 1.
Clinical trial of ex vivo and in vivo sirolimus after immune selective PC conditioning. Prior to allogeneic hematopoietic cell transplantation, patients received a 21-day course of Pentostatin (4 mg/m2 given on days 1, 8, and 15) combined with Cyclophosphamide (200 mg/day, days 1 to 21; dose-adjusted for efficacy [reduction in ALC] and toxicity [reduction in ANC]). After PC conditioning, patients were started on high-dose sirolimus (serum trough levels of 20–30 µg/ml through day 60 post-transplant). The T cell-replete allograft was augmented with an infusion of ex vivo manufactured donor rapamycin-resistant T cells (T-Rapa), which were also administered at days 14 and 45 post-transplant.
The primary study objective was to determine whether this transplant approach could safely achieve clinical regression of metastatic RCC (goal of ruling out a 20% overall PR/CR rate in favor of a 40% PR/CR rate); using a Simon two-stage design, the occurrence of ≥3 responses in the first 12 evaluable patients would be required to proceed to the second stage of study design. Organ toxicity was evaluated by NCI Common Toxicity Criteria (version 2.0). GVHD was evaluated using acute(34) and chronic grading(35); acute GVHD onset within the first 100 days post-HCT was considered classical acute(34) whereas onset after day 100 was considered late acute(35). Disease responses were evaluated by computed tomographic measurements and according to the Response Evaluation Criteria in Solid Tumors (RECIST) Committee criteria. Alloengraftment was monitored using variable N-terminal repeat PCR assays on total PBMC, enriched T cells (CD3-selected), or enriched myeloid cells (CD15-selected).
Immune Monitoring
Plasma IL-7 and IL-15 levels were measured by bioplex assay (EMD Millipore; Billerica, MA). Cytokine assays were performed on cryopreserved peripheral blood samples taken pre- and post-conditioning and at various points post-HCT. As described(19), cells were thawed and stimulated with anti-CD3/28 beads and resultant supernatants were tested for cytokine content by multi-plex assay (EMD Millipore); flow cytometry for transcription factor and differentiation marker expression was also performed as previously described. The statistical significance of the absolute difference or the relative difference from the baseline (or earlier) values was determined using a Wilcoxon signed rank test. Whether the absolute difference or relative difference was selected for evaluation depended on which one was less dependent on the baseline values. All p-values are reported without formal adjustment for multiple comparisons. In view of the number of tests performed, only p-values <0.01 would be interpretable as being associated with significant differences, while p-values between 0.01 and 0.05 would suggest strong trends.
RESULTS
PATIENT CHARACTERISTICS
Table I describes characteristics of the ten enrolled patients (six male and four female; median age, 55 years [range, 40 to 69]). Histology was exclusively or primarily clear cell (7/10 cases); two patients had collecting duct carcinoma and one patient had papillary carcinoma with a clear cell component. Median number of prior therapies was 3.5 (range, 3 to 5); all patients had nephrectomy of the primary tumor. Median number of metastatic sites was 3.5 (range, 3 to 9).
Table I.
Patient Characteristics
| UPN | Age/Sex | Tumor Type |
Prior Therapy |
Metastatic Sites |
||
|---|---|---|---|---|---|---|
| # | Types | # | Organs | |||
| 01 | 63/M | Clear Cell | 3 | IFN-α, Sunitinib, Temsirolimus | 3 | Lung, Lymph Nodes, Brain |
| 02 | 69/F | Clear Cell (+ glandular) | 3 | Sorafenib, Sunitinib, Ixabepilone | 3 | Lung, Lymph Nodes, Bone |
| 03 | 54/F | Clear Cell (+ sarcomatoid) | 4 | Sunitinib, Temsirolimus, Ixabepilone, XRT | 3 | Lung, Renal, Soft Tissue |
| 04 | 63/M | Clear Cell | 4 | Avastin + Erlotinib + Imatinib, Sunitinib, Everolimus, IL-2 | 9 | Pleura, Lung, Bone, Lymph Nodes, Renal, Heart, Mesentery, Pancreas, Adrenal |
| 05 | 65/F | Clear Cell (+ papillary) | 5 | Carboplatin [C] + Taxol [T], CT + Avastin, Temsirolimu, Sorafenib, Ixabepilone | 3 | Lung, Lymph Nodes, Renal |
| 06 | 55/M | Collecting Duct | 3 | Sunitinib, XRT Everolimus | 3 | Lung, Mediastinum, Retroperitoneum |
| 07 | 50/F | Clear Cell | 3 | Ixabepilone, XRT, Sunitinib | 6 | Lung, Lymph Nodes, Brain, Bone, Skin, Thyroid |
| 08 | 55/M | Papillary (+ clear cell) | 4 | Radio-frequency ablation, Sunitinib, XRT, Everolimus | 4 | Lung, Lymph Nodes, Bone, Soft Tissue |
| 09 | 40/M | Collecting Duct | 4 | Cisplatin + Gemcitabine, CT, Sorafenib + Erlotinib, XRT | 5 | Bone, Lung, Liver, Lymph Nodes, Chest Wall |
| 10 | 52/M | Clear Cell | 3 | Sorafenib, Temsirolimus, XRT | 4 | Lung, Lymph Nodes, Bone, Liver |
Abbreviations: UPN, unique patient number; XRT, local radiation therapy; #, indicates either number of prior therapies or number of metastatic sites.
IMMUNE SELECTIVE PENTOSTATIN PLUS CYCLOPHOSPHAMIDE REGIMEN
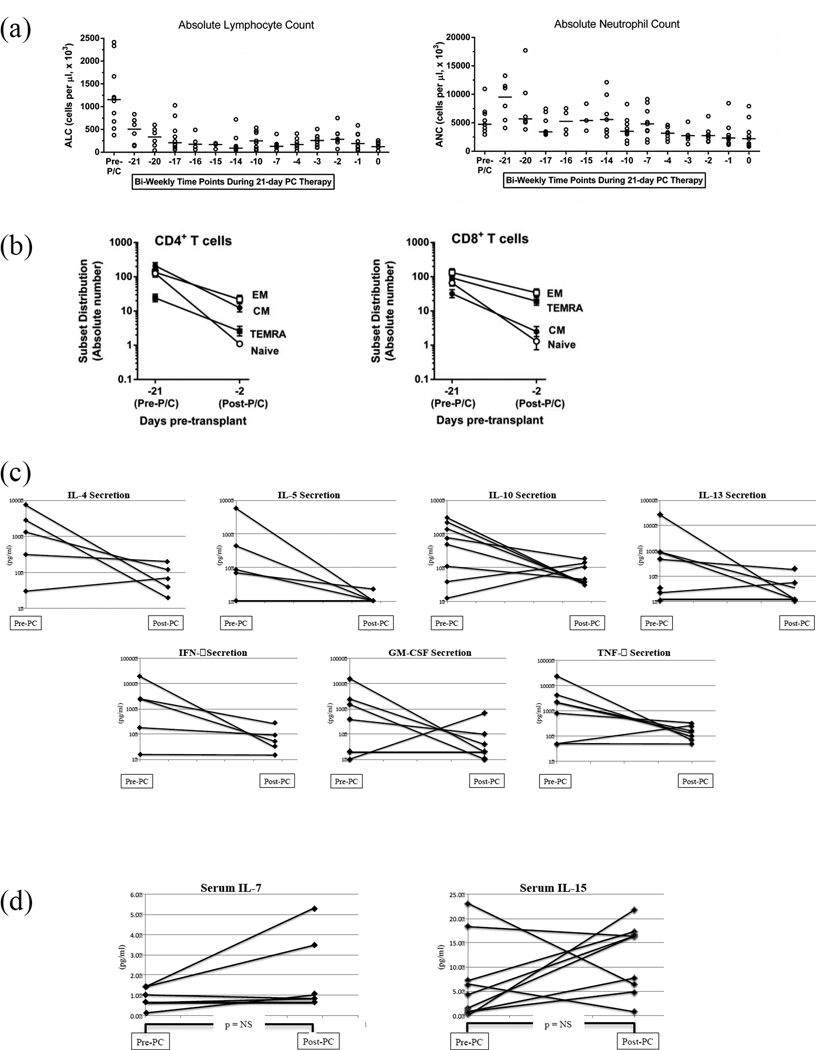
The 21-day PC regimen was safely administered in 10/10 cases: there were no infections and no grade 2 or greater toxicities attributable to the chemotherapy. Each patient received the planned three doses of pentostatin. Only two patients received the planned 200 mg/day dose of Cy for the entire 21-day interval (total Cy, 4200 mg); the range of total Cy dosing was 1400 to 4200 mg (median, 1900). Relative to pre-conditioning, PC therapy reduced the median ALC (all values, cells/µl) from 1156 (range, 375 to 2415) to 160 (range, 40 to 400); the majority of ALC reduction was achieved in the first week (Fig. 2a, left panel). The PC regimen did not reduce the ANC (no single value < 1000 cells/µl; Fig. 2a, right panel) and did not reduce red cells or platelets (not shown; no transfusions required). CD4+ T cells were markedly depleted, with reduction in median CD4 from 503 (range, 124 to 1497) to 23 (range, 54 to 107); CD8+ T cells were reduced from a median of 239 (range, 56 to 770) to 45 (range, 12 to 131). Absolute numbers of naïve, central memory, and effector memory subsets for CD4+ and CD8+ T cells were all significantly reduced after PC therapy (Fig. 2b). B cells were essentially eliminated [median CD19 cells reduced from 56 (range, 20 to 176) to 1 (range, 0 to 7)]. NK cells were relatively resistant [median NK cell reduction from 151 (range, 60 to 269) to 64 (22 to 485)].
Figure 2.
The PC regimen depletes and suppresses host lymphocytes. (a) Absolute lymphocyte count (ALC; left panel) and absolute neutrophil count (ANC; right panel) are shown for each patient before start of the pentostatin plus cyclophosphamide (PC) regimen, and then at six time points performed on a bi-weekly basis over the 21-day treatment interval. The crossbar at each measurement indicates the median value. (b) The absolute number of CD4+ T cell subsets (left panel) and CD8+ T cell subsets (right panel) was determined before and after the 21-day PC regimen (subsets including naïve, central memory [EM], effector memory [EM], and T effector memory expressing CD45RA [TEMRA]; values shown are mean values ± SEM). (c) T cells collected before and after administration of the PC regimen were co-stimulated for 24 hours; the resultant supernatant was tested for cytokine content (results expressed as pg/ml per 1 × 106 cells/ml per 24 hours). (d) Plasma was collected before the PC regimen (day -21) and after the PC regimen (day -3) and tested for IL-7 and IL-15 content by Luminex assay (results in pg/ml).
In murine models, the PC regimen was immune suppressive, as defined by reduced cytokine secretion in residual, post-therapy T cells(13). Pre-PC T cells responded to co-stimulation with secretion of IFN-γ, TNF-α, GM-CSF, IL-4, IL-5, IL-10, and IL-13, often at levels greater than 100 pg/ml (n=17 measurements were above this value; Fig. 2c); in each of these cases (17/17), post-PC T cells had a reduction in the cytokine measurement. In clinical trials using Flu/Cy conditioning, the T cell homeostatic cytokines IL-7 and IL-15 increased to median values (at the time of transplant) of 37 and 57 pg/ml, respectively(36, 37). In contrast, using PC conditioning, there was no statistically significant increase in IL-7 and IL-15 levels (Figure 2d).
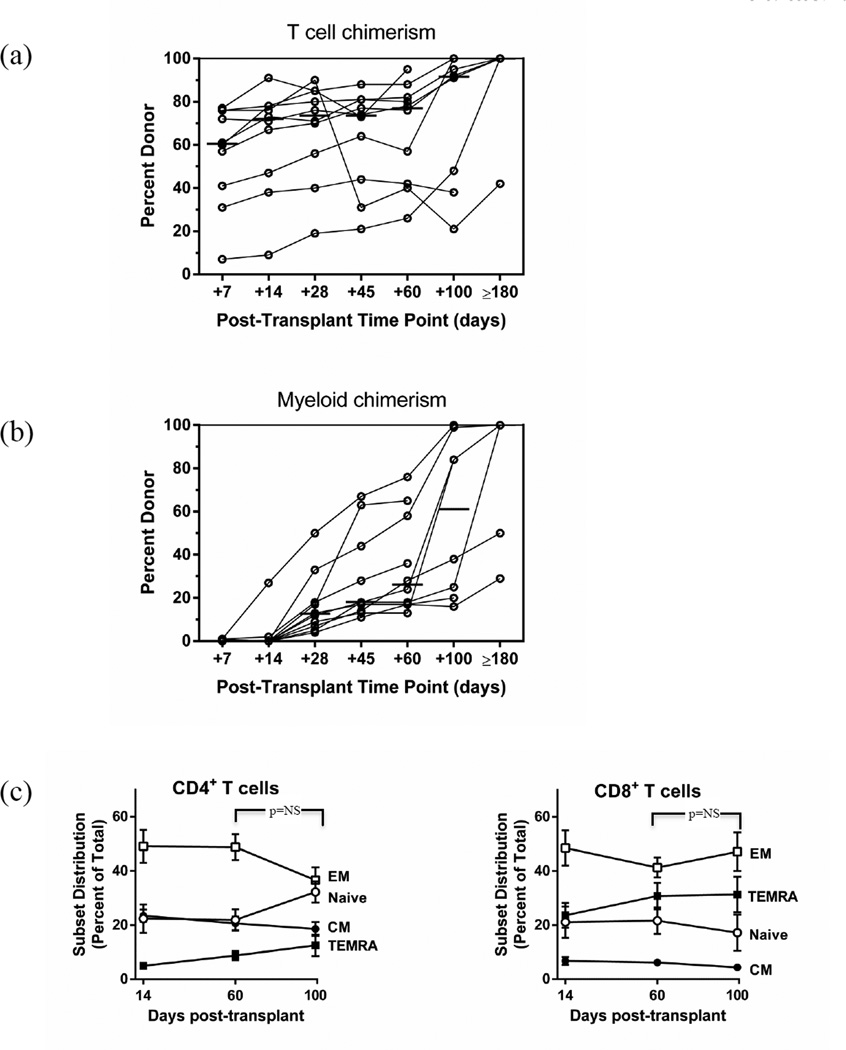
STABLE MIXED CHIMERISM IN SPITE OF MULTIPLE T-RAPA CELL DLI
Median percent donor T cell chimerism at days 7, 14, 28, 45, and 60 post-HCT were 61 (range, 7 to 77), 72 (range, 9 to 91), 74 (range, 21 to 88), and 77 (range, 26 to 95), respectively (Fig. 3a). Transplantation of T cell replete allografts plus the first infusion of T-Rapa cells thus yielded immediate donor T cell engraftment; however, chimerism values remained relatively constant during sirolimus therapy in spite of multiple T-Rapa DLI. After discontinuation of sirolimus at day 60 post-HCT, donor T cell chimerism increased to a median value of 92% (range, 21 to 100). The PC regimen yielded limited donor myeloid engraftment (Fig. 3b): median donor myeloid chimerism at days 7 and 14 post-HCT were each 0% (ranges: 0 to 1; 0 to 27). Median percent donor myeloid chimerism increased modestly during sirolimus therapy, with values at days 28, 45, and 60 post-HCT of 13 (range, 4 to 50), 18 (range, 11 to 67), and 26 (range, 13 to 76). After discontinuation of sirolimus at day 60 post-HCT, donor myeloid chimerism increased to a median of 61% (range, 16 to 100). The two patients with the lowest T cell chimerism through day 100 post-HCT also had the lowest myeloid cell chimerism; both of these patients received each of the planned T-Rapa DLI plus additional unmanipulated DLI.
Figure 3.
Establishment and maintenance of split, mixed chimerism. Percent donor chimerism was determined for each patient by VNTR assay at the indicated time points for purified T cells (a) and for purified myeloid cells (b). (c) The percentage of CD4+ T cell subsets (left panel) and CD8+ T cell subsets (right panel) was determined by flow cytometry at the indicated post-transplant time points (subsets including naïve, central memory [EM], effector memory [EM], and T effector memory expressing CD45RA [TEMRA]).
In experimental models, rapamycin therapy increased CD8+ T cell memory responses(38). Given these data, we measured naïve, central memory, and effector memory CD4+ and CD8+ T cell subsets during and after sirolimus therapy: these subsets did not differ substantially when comparing the day 14, day 60, and day 100 post-HCT time points (Fig. 3c).
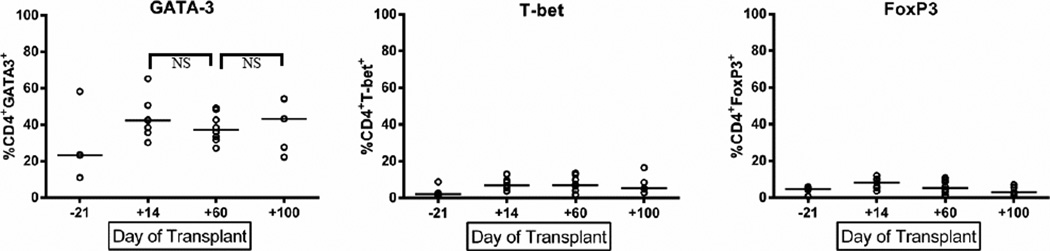
T CELL PHENOTYPE POST-HCT
Previously, T-Rapa DLI increased Th1- and Th2-type responses by transcription factor analysis and cytokine secretion assays(19). Similar to this initial trial, we found a preponderance of GATA-3+CD4+ T cells relative to T-bet+CD4+ T cells at day 14 post-HCT (Th2-type > Th1-type); however, these values did not increase with additional T-Rapa DLI and did not increase after sirolimus discontinuation (Fig. 4). In experimental models, rapamycin prevention of acute GVHD increased regulatory T cells(39); in our trial, FoxP3+CD4+ T cells did not increase during sirolimus therapy (Fig. 4, right panel). Upon ex vivo co-stimulation, post-HCT T cells secreted both Th1 (IFN-γ, TNF-α, GM-CSF) and Th2 (IL-4, IL-5, IL-10, IL-13) cytokines, with the magnitude of cytokine secretion being similar at days 14, 60, and 100 post-HCT (not shown).
Figure 4.
Determination of post-transplant T cell phenotype. CD4+ T cells were evaluated by intra-cellular flow cytometry for expression of transcription factors for Th2, Th1, or regulatory T cell subsets (GATA-3, left panel; T-bet, middle panel; FoxP3, right panel). Time points evaluated were before initiation of the PC regimen (day -21) and at the indicated post-transplant times.
CLINICAL OUTCOME
Clinical results are summarized in Table II. No partial or complete clinical responses were observed by RECIST criteria in the first 10 evaluable patients; because the primary objective was not achieved, further accrual to the protocol was stopped at this point.
Table II.
Transplantation Outcome
| Summary of DLI Therapy |
GVHD |
Tumor Staging |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Acute |
||||||||||||
| UPN | # DLI |
Specifics | s | g | l | Gr | Late Acute |
Chronic | day +28 |
day +60 |
day +100 |
Overall Outcome |
| 01 | 3 | T-Rapa Series | 0 | 0 | 0 | 0 | G | N.E. | SD | SD | PD | Death (d 131) RCC |
| 02 | 4 | T-Rapa Series + Standard DLI (1) | 1 | 0 | 0 | I | None | V-V | SD | SD | PD | Death (d 740) RCC |
| 03 | 3 | T-Rapa Series | 0 | 0 | 0 | 0 | N.E. | N.E. | SD | PD | PD | Death (d 134) RCC |
| 04 | 7 | T-Rapa Series + Standard DLI (4) | 0 | 0 | 0 | 0 | S, G, L | None | SD | SD | PD | Death (d 303) Infection, GVHD, RCC |
| 05 | 5 | T-Rapa Series + Standard DLI (2) | 0 | 0 | 0 | 0 | N.E. | N.E. | SD | SD | PD | Death (d 127) RCC |
| 06 | 4 | T-Rapa Series + Standard DLI (1) | 0 | 0 | 0 | 0 | S | None | SD | SD | SD | Alive (d +1591) |
| 07 | 2 | T-Rapa #1, #2 | 0 | 0 | 0 | 0 | S | N.E. | SD | PD | PD | Death (d 165) RCC |
| 08 | 5 | T-Rapa Series + Standard DLI (2) | 0 | 0 | 0 | 0 | None | None | SD | SD | PD | Death (d 300) RCC |
| 09 | 4 | T-Rapa Series + Standard DLI (1) | 0 | 0 | 0 | 0 | N.E. | N.E. | SD | PD | PD | Death (d 143) RCC |
| 10 | 1 | T-Rapa #1 | 2 | 0 | 0 | I | N.E. | N.E. | SD | PD | NA | Death (d 78) RCC |
Abbreviations: T-Rapa Series, indicates patient received T-Rapa cells at day 0 of transplant and at days 14 and 45 post-transplant; Standard DLI, indicates donor lymphocyte infusion consisting of unmanipulated donor T cells; N.E., not evaluable; N.A., not applicable; S, G, L indicates skin, gut, or liver acute GVHD; V-V, indicates vulvar vaginal chronic GVHD; SD, indicates stable disease; PD, indicates progressive disease; RCC, indicates disease active at time of death (SD or PD).
Patients UPN07 and UPN10 did not receive all T-Rapa infusions due to poor performance status.
Eight of 10 patients received each of the three, planned T-Rapa DLI; one patient each received either one or two doses of T-Rapa cells because of poor performance status or inability to tolerate sirolimus. Six of 10 patients received additional, unmanipulated DLI to treat progressive disease (median day of unmanipulated DLI therapy was day 87 post-HCT [range, 76–607 days]). In terms of adverse events through day 100 post-HCT: there was no engraftment syndrome or other serious adverse events attributable to T-Rapa cell therapy. High-dose sirolimus was generally well tolerated; one patient needed to discontinue planned sirolimus therapy (due to exacerbation of renal insufficiency related to hypercalcemia). One patient required red cell transfusion during sirolimus therapy; transplant associated micro-angiopathy did not occur. Four patients required topical cortico-steroid therapy for sirolimus-related oral ulcers (grade 2 toxicity); there were no other GI toxicities. Two patients each had catheter-related thrombosis or catheter-related line infection. One patient each had bacteremia attributable to an intestinal metastasis, bacterial pneumonia, or viral infection (BK cystitis).
Classical acute GVHD of grade II or higher did not occur. Four of six patients developed late acute GVHD (at days 115, 124, 163, and 284 post-HCT); two cases involved skin only and two involved the gut. One of four evaluable patients developed chronic GVHD, which was limited to vulvo-vaginal involvement. By day 60 post-HCT, in spite of high-dose sirolimus therapy, four of 10 patients had progressive disease by RECIST criteria; five additional patients developed progressive disease by day 100 post-transplant. One patient continues to have stable disease more than four years post-transplant (collecting duct carcinoma). Each of the nine protocol deaths was primarily attributable to progressive RCC; one case was additionally attributable to late acute gut GVHD and CMV enteritis that occurred after multiple unmanipulated DLI.
DISCUSSION
Pentostatin plus low-dose, dose-adjusted Cy yielded sufficient host T cell depletion and suppression to permit prompt donor T cell engraftment. The PC regimen preserved the host myeloid compartment, as evidenced by absence of neutropenia and extremely low initial levels of donor myeloid cell engraftment. Single-agent, high-dose sirolimus was sufficient for acute GVHD prophylaxis in spite of T cell-replete transplantation and multiple T-Rapa DLI. High-dose sirolimus yielded stable mixed T cell chimerism and a stable post-transplant T cell cytokine phenotype. However, high-dose sirolimus did not control tumor progression. In sum, these results have identified a novel platform for establishing stable mixed chimerism, yet on the other hand caution against use of high-dose sirolimus in conjunction with allogeneic T cell therapy.
The PC regimen is an immune-selective method of non-myeloablative transplantation that resides at the far range of this discipline (towards non-myelosuppressive transplantation). The PC regimen was immune depleting and immune suppressive, as residual host T cells were not capable of high-level cytokine secretion. This result mirrors our findings in a murine model of graft rejection(13), where pentostatin was more immune suppressive than fludarabine; it is thus possible that the clinical trial results described here may be relatively unique to pentostatin (that is, not necessarily inter-changeable with other purine analogues). The PC regimen differentially depleted immune subsets, with CD4+ T cells and B cells more sensitive than CD8+ T cells; the majority of lymphocytes remaining after PC therapy were NK cells. Also, the naïve T cell subset, which in murine models mediate increased alloreactivity(40), was nearly eliminated. Finally, in contrast to previous immune-ablative regimens(36, 37) and other non-myeloablative conditioning(41), PC therapy did not significantly increase IL-7 or IL-15 levels. Given that some studies have associated IL-7 and IL-15 levels with acute GVHD risk(36, 42), this characteristic may have contributed to the nominal GVHD and stable mixed T cell chimerism.
The mixed chimerism was split in terms of T cell versus myeloid populations. The paucity of donor myeloid engraftment early post-HCT likely represents the lowest values reported to date and demonstrates the relative lack of myeloid toxicity from the PC regimen. Nonetheless, stem cell engraftment was secured, as each patient had a gradual increase in donor myeloid components; this apparent competitive advantage of donor stem cells was likely generated through a GVH reaction that was largely sub-clinical. Although this pattern of alloengraftment was not conducive to refractory cancer therapy, split mixed chimerism favoring donor T cell elements may be favorable for therapy of T cell-based immune deficiencies.
Several factors likely contributed to the low rate and severity of acute GVHD. First, the PC regimen did not increase GVHD-provoking T cell homeostatic cytokines. Second, the lymphocyte specificity of the PC regimen may have constrained host inflammation, which is known to potentiate GVHD(8). Third, mixed chimerism itself limits clinical acute GVHD(43). Experimental GVHD is restricted by host T cells(44) and promoted by donor antigen-presenting-cells(45); because the PC regimen preserved some component of host T cells and severely limited donor myeloid engraftment, the pattern of split mixed chimerism generated may have been particularly protective against GVHD. Fourth, the T-Rapa DLI product expresses a balanced pattern of Th1- and Th2-type cytokines and previously yielded a low rate of acute GVHD(19). Finally, high-dose sirolimus can protect against acute GVHD(28). In experimental models, rapamycin anti-GVHD effects occurred by Th1 cytokine inhibition(46) and regulatory T cell promotion(39); because we found low-levels of T-bet+ and FoxP3+ CD4+ T cells post-HCT, inhibition of Th1 cells may have been largely operational in this trial. Given these collective results, similar to our findings in an experimental model(47), we conclude that ex vivo manufactured T-Rapa cells are not resistant to in vivo rapamycin therapy.
Several factors likely contributed to the lack of GVT effects. First, responses against RCC after allogeneic HCT preferentially occur in patients with less than three metastatic sites(48); our study was comprised of heavily pre-treated patients (median, 3.5 prior regimens) with extensive metastatic burden (median, 3.5 sites). Second, our hypothesis that high-dose sirolimus would limit tumor progression was not confirmed, as nine of 10 patients had progressive disease during or shortly after sirolimus therapy. Third, high-dose sirolimus was counter-productive due to promotion of stable mixed chimerism [which was seen in a previous study of high-dose sirolimus(28)] and due to inhibition of Th1-type cells [which are necessary for murine GVT effects against RCC cells(49)]. Fourth, the low donor myeloid engraftment after PC conditioning was likely counter-productive, as donor APC contribute to GVT effects in experimental models(50). Finally, previous clinical trials have indicated that GVT effects against RCC are associated with clinical GVHD(29, 30).
The overall transplant approach we evaluated was not suitable for therapy of refractory cancer, but may be advantageous for therapy of non-malignant disease. These results provide a cautionary note in terms of combining adoptive T cell therapy with high-dose sirolimus therapy, which did not prevent tumor progression and limited post-transplant T cell effects. Our future investigations will continue to incorporate ultra-low intensity conditioning such as the PC regimen as a safe platform for evaluation of novel T cell therapy products. However, such platforms will incorporate calcineurin inhibitors as GVHD prophylaxis to avoid the in vivo tolerizing effects of sirolimus therapy.
TRANSLATIONAL RELEVANCE.
Graft rejection, graft-versus-host disease (GVHD), and insufficient graft-versus-tumor (GVT) effects each limit the therapeutic application of allogeneic hematopoietic cell transplantation (HCT), particularly for solid tumors such as metastatic renal cell carcinoma. This trial used three interventions to address these limitations: (1) lymphocyte selective host conditioning using pentostatin plus dose-adjusted cyclophosphamide (PC regimen); (2) high-dose sirolimus therapy; and (3) augmentation of T cell replete allogeneic HSCT with additional donor lymphocyte infusions (DLI) consisting of CD4+ T cells manufactured ex vivo in sirolimus (T-Rapa cells). The PC regimen represents a new approach to prevent graft rejection, as it selectively modulated host T cells without neutropenia or infection and safely permitted alloengraftment. High-dose sirolimus effectively prevented GVHD but also inhibited multiple T-Rapa DLI, thereby off-setting any potential beneficial direct anti-tumor effect of sirolimus. These results caution against use of high-dose sirolimus during allogeneic T cell therapy in patients with refractory cancer.
ACKNOWLEDGEMENTS
Special recognition goes to Vicki Fellowes for her efforts in T-Rapa cell manufacturing; Daniele Avila, Amanda Urban, Jennifer Mann, and Tiffani Taylor of the NCI-ETIB for their excellence and dedication in the care of protocol patients; Rashmika Patel of the NCI-CCR for her protocol support efforts; the NIH Clinical Center and Department of Nursing; and to the Medical Oncology Fellows at the NCI.
Grant Support: This work was supported by the Center for Cancer Research, NCI.
Footnotes
Conflict of Interest Statement: No author has any conflict of interest.
REFERENCES
- 1.Baron F, Baker JE, Storb R, Gooley TA, Sandmaier BM, Maris MB, et al. Kinetics of engraftment in patients with hematologic malignancies given allogeneic hematopoietic cell transplantation after nonmyeloablative conditioning. Blood. 2004;104:2254–2262. doi: 10.1182/blood-2004-04-1506. [DOI] [PubMed] [Google Scholar]
- 2.Kahl C, Storer BE, Sandmaier BM, Mielcarek M, Maris MB, Blume KG, et al. Relapse risk in patients with malignant diseases given allogeneic hematopoietic cell transplantation after nonmyeloablative conditioning. Blood. 2007;110:2744–2748. doi: 10.1182/blood-2007-03-078592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pavletic SZ, Kumar S, Mohty M, de Lima M, Foran JM, Pasquini M, et al. NCI First International Workshop on the Biology, Prevention, and Treatment of Relapse after Allogeneic Hematopoietic Stem Cell Transplantation: report from the Committee on the Epidemiology and Natural History of Relapse following Allogeneic Cell Transplantation. Biol Blood Marrow Transplant. 2010;16:871–890. doi: 10.1016/j.bbmt.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frey NV, Porter DL. Graft-versus-host disease after donor leukocyte infusions: presentation and management. Best Pract Res Clin Haematol. 2008;21:205–222. doi: 10.1016/j.beha.2008.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gill S, Porter DL. Reduced-intensity hematopoietic stem cell transplants for malignancies: harnessing the graft-versus-tumor effect. Annu Rev Med. 2013;64:101–117. doi: 10.1146/annurev-med-121411-103452. [DOI] [PubMed] [Google Scholar]
- 6.Fujisaki J, Wu J, Carlson AL, Silberstein L, Putheti P, Larocca R, et al. In vivo imaging of Treg cells providing immune privilege to the haematopoietic stem-cell niche. Nature. 2011;474:216–219. doi: 10.1038/nature10160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schwartz E, Lapidot T, Gozes D, Singer TS, Reisner Y. Abrogation of bone marrow allograft resistance in mice by increased total body irradiation correlates with eradication of host clonable T cells and alloreactive cytotoxic precursors. J Immunol. 1987;138:460–465. [PubMed] [Google Scholar]
- 8.Jankovic D, Ganesan J, Bscheider M, Stickel N, Weber FC, Guarda G, et al. The Nlrp3 inflammasome regulates acute graft-versus-host disease. J Exp Med. 2013;210:1899–1910. doi: 10.1084/jem.20130084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pavletic SZ, Bociek RG, Foran JM, Rubocki RJ, Kuszynski CA, Wisecarver JL, et al. Lymphodepleting effects and safety of pentostatin for nonmyeloablative allogeneic stem-cell transplantation. Transplantation. 2003;76:877–881. doi: 10.1097/01.TP.0000084869.08639.A0. [DOI] [PubMed] [Google Scholar]
- 10.Miller KB, Roberts TF, Chan G, Schenkein DP, Lawrence D, Sprague K, et al. A novel reduced intensity regimen for allogeneic hematopoietic stem cell transplantation associated with a reduced incidence of graft-versus-host disease. Bone Marrow Transplant. 2004;33:881–889. doi: 10.1038/sj.bmt.1704454. [DOI] [PubMed] [Google Scholar]
- 11.Kharfan-Dabaja MA, Anasetti C, Fernandez HF, Perkins J, Ochoa-Bayona JL, Pidala J, et al. Phase II study of CD4+-guided pentostatin lymphodepletion and pharmacokinetically targeted busulfan as conditioning for hematopoietic cell allografting. Biol Blood Marrow Transplant. 2013;19:1087–1093. doi: 10.1016/j.bbmt.2013.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kay NE, Geyer SM, Call TG, Shanafelt TD, Zent CS, Jelinek DF, et al. Combination chemoimmunotherapy with pentostatin, cyclophosphamide, and rituximab shows significant clinical activity with low accompanying toxicity in previously untreated B chronic lymphocytic leukemia. Blood. 2007;109:405–411. doi: 10.1182/blood-2006-07-033274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mariotti J, Taylor J, Massey PR, Ryan K, Foley J, Buxhoeveden N, et al. The pentostatin plus cyclophosphamide nonmyeloablative regimen induces durable host T cell functional deficits and prevents murine marrow allograft rejection. Biol Blood Marrow Transplant. 2011;17:620–631. doi: 10.1016/j.bbmt.2010.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mossoba ME, Onda M, Taylor J, Massey PR, Treadwell S, Sharon E, et al. Pentostatin plus cyclophosphamide safely and effectively prevents immunotoxin immunogenicity in murine hosts. Clin Cancer Res. 2011;17:3697–3705. doi: 10.1158/1078-0432.CCR-11-0493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hassan R, Miller AC, Sharon E, Thomas A, Reynolds JC, Ling A, et al. Major cancer regressions in mesothelioma after treatment with an anti-mesothelin immunotoxin and immune suppression. Sci Transl Med. 2013;5:208ra147. doi: 10.1126/scitranslmed.3006941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van den Brink MR, Porter DL, Giralt S, Lu SX, Jenq RR, Hanash A, et al. Relapse after allogeneic hematopoietic cell therapy. Biol Blood Marrow Transplant. 2010;16:S138–S145. doi: 10.1016/j.bbmt.2009.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bethge WA, Hegenbart U, Stuart MJ, Storer BE, Maris MB, Flowers ME, et al. Adoptive immunotherapy with donor lymphocyte infusions after allogeneic hematopoietic cell transplantation following nonmyeloablative conditioning. Blood. 2004;103:790–795. doi: 10.1182/blood-2003-07-2344. [DOI] [PubMed] [Google Scholar]
- 18.Kumar AJ, Hexner EO, Frey NV, Luger SM, Loren AW, Reshef R, et al. Pilot study of prophylactic ex vivo costimulated donor leukocyte infusion after reduced-intensity conditioned allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2013;19:1094–1101. doi: 10.1016/j.bbmt.2013.04.021. [DOI] [PubMed] [Google Scholar]
- 19.Fowler DH, Mossoba ME, Steinberg SM, Halverson DC, Stroncek D, Khuu HM, et al. Phase 2 clinical trial of rapamycin-resistant donor CD4+ Th2/Th1 (T-Rapa) cells after low-intensity allogeneic hematopoietic cell transplantation. Blood. 2013;121:2864–2874. doi: 10.1182/blood-2012-08-446872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Foley JE, Mariotti J, Ryan K, Eckhaus M, Fowler DH. Th2 cell therapy of established acute graft-versus-host disease requires IL-4 and IL-10 and is abrogated by IL-2 or host-type antigen-presenting cells. Biol Blood Marrow Transplant. 2008;14:959–972. doi: 10.1016/j.bbmt.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mariotti J, Foley J, Jung U, Borenstein T, Kantardzic N, Han S, et al. Ex vivo rapamycin generates apoptosis-resistant donor Th2 cells that persist in vivo and prevent hemopoietic stem cell graft rejection. J Immunol. 2008;180:89–105. doi: 10.4049/jimmunol.180.1.89. [DOI] [PubMed] [Google Scholar]
- 22.Mariotti J, Foley J, Ryan K, Buxhoeveden N, Kapoor V, Amarnath S, et al. Graft rejection as a Th1-type process amenable to regulation by donor Th2-type cells through an interleukin-4/STAT6 pathway. Blood. 2008;112:4765–4775. doi: 10.1182/blood-2008-05-154278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ram R, Storb R. Pharmacologic prophylaxis regimens for acute graft-versus-host disease: past, present and future. Leuk Lymphoma. 2013;54:1591–1601. doi: 10.3109/10428194.2012.762978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Armand P, Gannamaneni S, Kim HT, Cutler CS, Ho VT, Koreth J, et al. Improved survival in lymphoma patients receiving sirolimus for graft-versus-host disease prophylaxis after allogeneic hematopoietic stem-cell transplantation with reduced-intensity conditioning. J Clin Oncol. 2008;26:5767–5774. doi: 10.1200/JCO.2008.17.7279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hartmann B, Schmid G, Graeb C, Bruns CJ, Fischereder M, Jauch KW, et al. Biochemical monitoring of mTOR inhibitor-based immunosuppression following kidney transplantation: a novel approach for tailored immunosuppressive therapy. Kidney Int. 2005;68:2593–2598. doi: 10.1111/j.1523-1755.2005.00731.x. [DOI] [PubMed] [Google Scholar]
- 26.Cutler C, Stevenson K, Kim HT, Richardson P, Ho VT, Linden E, et al. Sirolimus is associated with veno-occlusive disease of the liver after myeloablative allogeneic stem cell transplantation. Blood. 2008;112:4425–4431. doi: 10.1182/blood-2008-07-169342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ho VT, Cutler C, Carter S, Martin P, Adams R, Horowitz M, et al. Blood and marrow transplant clinical trials network toxicity committee consensus summary: thrombotic microangiopathy after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2005;11:571–575. doi: 10.1016/j.bbmt.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 28.Hsieh MM, Kang EM, Fitzhugh CD, Link MB, Bolan CD, Kurlander R, et al. Allogeneic hematopoietic stem-cell transplantation for sickle cell disease. N Engl J Med. 2009;361:2309–2317. doi: 10.1056/NEJMoa0904971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Childs R, Chernoff A, Contentin N, Bahceci E, Schrump D, Leitman S, et al. Regression of metastatic renal-cell carcinoma after nonmyeloablative allogeneic peripheral-blood stem-cell transplantation. N Engl J Med. 2000;343:750–758. doi: 10.1056/NEJM200009143431101. [DOI] [PubMed] [Google Scholar]
- 30.Barkholt L, Bregni M, Remberger M, Blaise D, Peccatori J, Massenkeil G, et al. Allogeneic haematopoietic stem cell transplantation for metastatic renal carcinoma in Europe. Ann Oncol. 2006;17:1134–1140. doi: 10.1093/annonc/mdl086. [DOI] [PubMed] [Google Scholar]
- 31.Rini BI, Halabi S, Barrier R, Margolin KA, Avigan D, Logan T, et al. Adoptive immunotherapy by allogeneic stem cell transplantation for metastatic renal cell carcinoma: a CALGB intergroup phase II study. Biol Blood Marrow Transplant. 2006;12:778–785. doi: 10.1016/j.bbmt.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 32.Hudes G, Carducci M, Tomczak P, Dutcher J, Figlin R, Kapoor A, et al. Temsirolimus, interferon alfa, or both for advanced renal-cell carcinoma. N Engl J Med. 2007;356:2271–2281. doi: 10.1056/NEJMoa066838. [DOI] [PubMed] [Google Scholar]
- 33.Castiello L, Mossoba M, Viterbo A, Sabatino M, Fellowes V, Foley JE, et al. Differential gene expression profile of first-generation and second-generation rapamycin-resistant allogeneic T cells. Cytotherapy. 2013;15:598–609. doi: 10.1016/j.jcyt.2012.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant. 1995;15:825–828. [PubMed] [Google Scholar]
- 35.Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11:945–956. doi: 10.1016/j.bbmt.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 36.Dean RM, Fry T, Mackall C, Steinberg SM, Hakim F, Fowler D, et al. Association of serum interleukin-7 levels with the development of acute graft-versus-host disease. J Clin Oncol. 2008;26:5735–5741. doi: 10.1200/JCO.2008.17.1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boyiadzis M, Memon S, Carson J, Allen K, Szczepanski MJ, Vance BA, et al. Up-regulation of NK cell activating receptors following allogeneic hematopoietic stem cell transplantation under a lymphodepleting reduced intensity regimen is associated with elevated IL-15 levels. Biol Blood Marrow Transplant. 2008;14:290–300. doi: 10.1016/j.bbmt.2007.12.490. [DOI] [PubMed] [Google Scholar]
- 38.Araki K, Turner AP, Shaffer VO, Gangappa S, Keller SA, Bachmann MF, et al. mTOR regulates memory CD8 T-cell differentiation. Nature. 2009;460:108–112. doi: 10.1038/nature08155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zeiser R, Leveson-Gower DB, Zambricki EA, Kambham N, Beilhack A, Loh J, et al. Differential impact of mammalian target of rapamycin inhibition on CD4+CD25+Foxp3+ regulatory T cells compared with conventional CD4+ T cells. Blood. 2008;111:453–462. doi: 10.1182/blood-2007-06-094482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Anderson BE, McNiff J, Yan J, Doyle H, Mamula M, Shlomchik MJ, et al. Memory CD4+ T cells do not induce graft-versus-host disease. J Clin Invest. 2003;112:101–108. doi: 10.1172/JCI17601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.De Bock M, Fillet M, Hannon M, Seidel L, Merville MP, Gothot A, et al. Kinetics of IL-7 and IL-15 levels after allogeneic peripheral blood stem cell transplantation following nonmyeloablative conditioning. PLoS One. 2013;8:e55876. doi: 10.1371/journal.pone.0055876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thiant S, Yakoub-Agha I, Magro L, Trauet J, Coiteux V, Jouet JP, et al. Plasma levels of IL-7 and IL-15 in the first month after myeloablative BMT are predictive biomarkers of both acute GVHD and relapse. Bone Marrow Transplant. 2010;45:1546–1552. doi: 10.1038/bmt.2010.13. [DOI] [PubMed] [Google Scholar]
- 43.Nikolousis E, Robinson S, Nagra S, Brookes C, Kinsella F, Tauro S, et al. Post-transplant T cell chimerism predicts graft versus host disease but not disease relapse in patients undergoing an alemtuzumab based reduced intensity conditioned allogeneic transplant. Leuk Res. 2013;37:561–565. doi: 10.1016/j.leukres.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 44.Blazar BR, Lees CJ, Martin PJ, Noelle RJ, Kwon B, Murphy W, et al. Host T cells resist graft-versus-host disease mediated by donor leukocyte infusions. J Immunol. 2000;165:4901–4909. doi: 10.4049/jimmunol.165.9.4901. [DOI] [PubMed] [Google Scholar]
- 45.Anderson BE, McNiff JM, Jain D, Blazar BR, Shlomchik WD, Shlomchik MJ. Distinct roles for donor- and host-derived antigen-presenting cells and costimulatory molecules in murine chronic graft-versus-host disease: requirements depend on target organ. Blood. 2005;105:2227–2234. doi: 10.1182/blood-2004-08-3032. [DOI] [PubMed] [Google Scholar]
- 46.Blazar BR, Taylor PA, Panoskaltsis-Mortari A, Vallera DA. Rapamycin inhibits the generation of graft-versus-host disease- and graft-versus-leukemia-causing T cells by interfering with the production of Th1 or Th1 cytotoxic cytokines. J Immunol. 1998;160:5355–5365. [PubMed] [Google Scholar]
- 47.Jung U, Foley JE, Erdmann AA, Toda Y, Borenstein T, Mariotti J, et al. Ex vivo rapamycin generates Th1/Tc1 or Th2/Tc2 Effector T cells with enhanced in vivo function and differential sensitivity to post-transplant rapamycin therapy. Biol Blood Marrow Transplant. 2006;12:905–918. doi: 10.1016/j.bbmt.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 48.Nakayama K, Tannir NM, Liu P, Wathen JK, Cheng YC, Champlin RE, et al. Natural history of metastatic renal cell carcinoma in patients who underwent consultation for allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2007;13:975–985. doi: 10.1016/j.bbmt.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 49.Ramirez-Montagut T, Chow A, Kochman AA, Smith OM, Suh D, Sindhi H, et al. IFN-gamma and Fas ligand are required for graft-versus-tumor activity against renal cell carcinoma in the absence of lethal graft-versus-host disease. J Immunol. 2007;179:1669–1680. doi: 10.4049/jimmunol.179.3.1669. [DOI] [PubMed] [Google Scholar]
- 50.Reddy P, Maeda Y, Liu C, Krijanovski OI, Korngold R, Ferrara JL. A crucial role for antigen-presenting cells and alloantigen expression in graft-versus-leukemia responses. Nat Med. 2005;11:1244–1249. doi: 10.1038/nm1309. [DOI] [PubMed] [Google Scholar]