Abstract
Background
Identifying and engaging excessive alcohol users in primary care may be an effective way to improve patient health outcomes, reduce alcohol-related acute care events, and lower costs. Little is known about what structures of primary care team communication are associated with alcohol-related patient outcomes.
Methods
Using a sociometric survey of primary care clinic communication, this study evaluated the relation between team communication networks and alcohol-related utilization of care and costs. Between May 2013 and December 2013, a total of 155 healthcare employees at 6 primary care clinics participated in a survey on team communication. Three-level hierarchical modeling evaluated the link between connectedness within the care team and the number of alcohol-related emergency department visits, hospital days, and associated medical care costs in the past 12 months for each team’s primary care patient panel.
Results
Teams (n=31) whose RNs displayed more strong (at least daily) face-to-face ties and strong (at least daily) electronic communication ties had 10% fewer alcohol-related hospital days (RR=0.90; 95% CI: 0.84, 0.97). Furthermore, in an average team size of 19, each additional team member with strong interaction ties across the whole team was associated with $1030 (95% CI: −$1819, −$241) lower alcohol-related patient health care costs per 1000 team patients in the past 12 months. Conversely, teams whose primary care practitioner had more strong face-to-face communication ties and more weak (weekly or several times a week) electronic communication ties had 12% more alcohol-related hospital days (RR=1.12; 95: CI: 1.03, 1.23) and $1428 (95% CI: $378, $2478) higher alcohol-related healthcare costs per 1000 patients in the past 12 months. The analyses controlled for patient age, gender, insurance, and co-morbidity diagnoses.
Conclusions
Excessive alcohol-using patients may fair better if cared for by teams whose face-to-face and electronic communication networks include more team members and whose communication to the PCP has been streamlined to fewer team members.
Keywords: alcohol, primary care, team, social network, communication
INTRODUCTION
Providing high quality care for excessive alcohol users, including heavy and binge drinkers, is a major challenge for health care professionals in primary care. Heavy alcohol consumption is defined as consuming more than 7 drinks per week for women or 14 drinks per week for men (CDC, 2014); binge drinking corresponds to 5 or more drinks for men or 4 or more drinks for women on a single occasion (NIAAA, 2004). Approximately 24% of men and 15% of women engage in excessive alcohol consumption (CDC, 2012). In 2006, there were more than 1.2 million emergency room visits and 2.7 million physician office visits due to excessive drinking (The Lewin Group, 2013). Alcohol-medication interactions are responsible for one quarter of all US emergency room visits. Roughly 16% to 26% of hospitalized inpatients report excessive alcohol use (Saitz et al., 2006, Roche et al., 2006). Excessive alcohol drinkers have higher rates of hospital readmissions (Walley et al., 2012) and experience lower levels of screening, preventive, and comorbidity care in comparison to patients without alcohol misuse (Beck et al., 2013, Mitchell et al., 2009). Excessive alcohol consumption is associated with $25 billion in healthcare costs annually (Bouchery et al., 2011). Given the tremendous disease burden and the prevalence rates of excessive alcohol use, from the societal perspective it is essential that health care practitioners provide high quality care in order to reduce potentially avoidable utilization and costs for excessive alcohol drinkers (Rehm, 2011, Mertens et al., 2003).
Identifying and engaging excessive alcohol users in primary care may be an effective way to reduce rates of excessive alcohol use and to alleviate alcohol-related co-morbidity and mortality in primary care patients (Fleming and Manwell, 1999, Zgierska A, 2009, Fleming et al., 2002, Kraemer, 2007). A number of meta-analyses have shown that alcohol services delivered in primary care settings can reduce alcohol use and associated harm, mortality, and medical costs for excessive alcohol drinkers (Solberg et al., 2008, Kaner et al., 2009, Bray et al., 2011, Jonas et al., 2012).
Current efforts to improve quality of alcohol-related care for excessive alcohol drinkers in primary care call for teams of clinicians and staff who perform interdependent tasks to deliver alcohol-related care for patients (Sullivan et al., 2011, Israel et al., 1996, Cruvinel et al., 2013, Aspy et al., 2008, Reiff-Hekking et al., 2005). Notably, in 2011, a joint Office of National Drug Control Policy, Substance Abuse and Mental Health Services Administration, and Health Resources and Services Administration meeting asked for more investment in team training for the primary care workforce to properly integrate alcohol services delivery in primary care (Dilonardo, 2011). Little is known, however, about the attributes of team care that are associated with better alcohol services delivery (Chambers et al., 2012). Team communication networks may be fundamental to the team’s capacity to deliver high quality alcohol-related care and to lower utilization and costs. Team communication networks could influence alcohol-related patient health outcomes through better team coordination (i.e., management of interdependent but distinct activities involved in care provision) resulting in shared vision and innovation (Stevenson et al., 2001, Campbell et al., 2001, Hess et al., 2010). Furthermore, team communication networks may foster the development of trust among team members performing distinct roles (Baker et al., 2006) as well as promote energy and emotional engagement which are essential for coordination (Quinn, 2005) and for patient outcomes.
Based on literature, the electronic health record (EHR) has low rates of documented alcohol services (McGlynn et al., 2003, Kim et al., 2013, Willenbring, 2013, Hingson et al., 2012). While alcohol services may go underreported in the EHR (Kim et al., 2013), better functioning teams may still be aware of patients’ alcohol use and take it under consideration in treating co-morbid medical conditions, which will result in fewer acute care visits. Therefore, we examine alcohol-related emergency department (ED) visits and hospital days as our measure of alcohol-related quality of care. While this is not an all-encompassing measure of alcohol-related quality of care, it allows us to quantify alcohol-related patient outcomes related to quality of care. Unfortunately, no reliable and valid measures of alcohol-related quality of care in primary care practices are readily available in the literature.
Without understanding what team communication structures contribute to alcohol-related utilization of care and medical costs, it will be difficult to meet the health needs for this patient population. With this in mind, this study addresses the following research question:
Research Question
What primary care team communication networks are associated with alcohol-related utilization of care and medical costs for primary care patients?
MATERIALS AND METHODS
Study Procedure
The study data come from a selected sample of 6 primary care clinics covering a wide range of the patient population across southern Wisconsin. A total of 8 primary care clinics were invited and 6 clinics agreed to participate. Study sites were chosen based on consultation with leadership from the health care system. Sites invited were non-residency-based primary care clinics that were not currently involved in other research or quality improvement initiatives. Reasons for refusal included recent staff turnover and lack of time. The 6 participating clinics are urban (2), suburban (3), and rural (1). The clinics have from 3 to 11 primary care practitioners (PCPs), with average active patient panel sizes (at least 2 visits in the past 3 years) ranging from 987 to 1548 patients per PCP. On average, roughly 65 percent of the clinic population has health insurance through a commercial health plan. Medicare coverage varies by clinic, from 6 to 19 percent, and 5 to 6 percent of the population is covered by Medicaid. The Institutional Review Board of the University of Wisconsin approved the study.
The first author initially introduced the study procedures and provided study consent forms at an all-staff clinic meeting in participating clinics. All physicians (MD/DO), physician assistants (PA), nurse practitioners (NP), registered nurses (RN), medical assistants (MA), licensed practical nurses (LPN), laboratory technicians, radiology technicians, clinic managers, medical receptionists, and other patient care staff were then invited to schedule the 30-minute face-to-face structured survey interview. Eligibility criteria included 18 years of age or older, ability to read and understand English, and employment at the study site in a patient care or patient interaction capacity. Subjects received $10 for completing the study survey and were entered into a lottery drawing for $100. In addition, the research team donated $200 to a local outreach effort of the clinic’s choice to participating clinics with 90% participation. Over 97% (155 of 160 invited) of eligible subjects took part in the study.
Data Sources
Team Member Survey
Study participants completed a 30-minute face-to-face structured survey, which asked about the subject’s communication with team members. Communication network questions were generated and pilot tested by the research team. See Appendix for network questions and formatting.
To minimize response bias and enhance data validity across study participants, the study team assured participants of the confidentiality of their responses, asked questions in a face-to-face interview format, and standardized interviewer training.
Active Primary Care Patient Panels of Primary Care Team
An EHR search linked primary care teams with active patient panels seen by the team. To ensure continuity of care, the active primary care team patient panel sample consisted of patients who had at least one visit with the lead clinician in the past 12 months, and at least 2 visits in the past 36 months. Patients with visits to multiple primary care clinicians were assigned to the clinician whom they saw most frequently, or, in the case of a tie, to the clinician seen at the most recent visit.
Primary Care Team Measures
Team Membership
Team communication networks are defined as the patterns of communication that exist among members of a primary care team. To determine membership in a care team, clinic staff were asked to consider a team definition and indicate on a full clinic staff roster who was on their care team. The care team was defined as ‘the smallest unit of individuals within the clinic that care for a specific patient panel.’ For the analysis, care team membership included a lead primary care practitioner (PCP), either a physician, nurse practitioner, or physician assistant, and all clinic employees who indicated on the survey that they belonged to that lead PCP’s care team. Finally, any individual whom the PCP named as a care team member was also included in the care team.
Clinic staff members could be included on multiple care teams based on responses to the team membership query. As an example, RNs could indicate that they belonged to the care teams of multiple PCPs. In this case, care team memberships would overlap as each RN would be considered a member of each PCP-led team.
Team Communication Network
Using the clinic staff roster as an aid for memory recall, all clinic staff members identified with whom and how frequently they interacted both face-to-face and by electronic means about patient care with other staff members in the clinic in the past 6 months (see Appendix). A connection between two team members was coded as a strong tie if the frequency of communication was reported as ‘once each day’ or ‘a few times each day’. A connection between team members was coded as a weak tie if the frequency of communication was reported as ‘once per week’ or ‘a few times per week’.
The communication network variable in-degree classified the face-to-face and EHR connections between team members. In-degree is a count of the communication ties directed to an individual from the rest of the team (Borgatti and Halgin, 2011). In-degree measures the connectedness of the individual to his/her team as a collective perspective of the team as a whole as opposed to a single person’s perception.
Team Member Individual and Demographic Characteristics
Team members self-reported gender, job title, percentage of full-time employment, and years working at the clinic.
Team Patient Outcome Measures
Alcohol-Related Health Care Utilization Measures
Frequency of alcohol-related ED visits and hospital visit days were extracted from an enterprise EHR database (Epic Systems Corporation) for teams’ active patient panels as utilization counts over the past 12 months. EHR records were searched for ED or hospital visits that included an alcohol-related ICD-9 code (2910 2911 2912 2913 2914 2915 2918 29181 29182 29189 2919 30300 30301 30302 30303 30390 30391 30392 30393 30500 30501 30502 30503 76071 9800 3575 4255 53530 53531 5710 5711 5712 5713), as defined by the Agency for Healthcare Research and Quality’s Clinical Classification Software alcohol diagnoses category (CCS category 660) (Quality, 2006–2009).
Alcohol-Related Medical Costs
Medical costs in the past 12 months were calculated by applying average medical costs in Wisconsin derived from published reports to health care utilization counts (Beckers Hospital Review, 2010, Agency for Healthcare Research and Quality, 2006, Weinick et al., 2009). Costs are considered from a societal single payer perspective (Adam et al., 2003). An average 2013 cost of $664 per ED visit and $1,628 per hospital day was applied to each recorded visit. Costs reflect average Medicare reimbursement rates for emergency and hospital care and do not assess patient costs. Charge data billed to the patients were not available for study ED and hospital visits.
Patient-Level Control Variables
To account for differences in patient panel characteristics and for factors that may be independently associated with health care utilization and cost, the analysis adjusted for a multitude of individual patient-level control variables. Patient-level variables drawn from the EHR included patient age, gender, race/ethnicity, insurance type, and available EHR diagnoses of chronic conditions referenced in the Centers for Medicare and Medicaid Services Chronic Condition Warehouse (CMS) (e.g., acute myocardial infarction, asthma, atrial fibrillation, cancer, chronic kidney disease, chronic obstructive pulmonary disease, depression, hyperlipidemia, hypertension, ischemic heart disease, osteoarthritis, osteoporosis, rheumatoid arthritis) and in the Charlson Comorbidity Index (Charlson et al., 1987) (e.g., cerebrovascular disease, congestive heart failure, dementia, peptic ulcer disease). The Charlson Comorbidity Index (CCI) was also included to adjust for potential confounding by multiple simultaneous chronic conditions (Charlson et al., 1987).
Statistical Analysis
Social Network Analysis
The analysis created a four-cell communication matrix for each team member by cross-tabulating face-to-face communication ties (strong/weak) with EHR communication ties (strong/weak) to every other team member. First, we calculated the number of an individual’s in-degree connections that were present in each quadrant of the communication matrix (strong/strong, strong/weak, weak/strong, weak/weak) out of the total possible connections. Next, we summed the individual tie strength tallies across all members of the care team. Finally, we computed average tie strength totals for specific job titles (i.e., PCP, RN, LPN/MA, laboratory/radiology technician, and medical receptionist) within each team. For the statistical models, the numbers of ties in each tie strength category (e.g., strong face-to-face and strong EHR) were standardized so that a one unit increase in the predictor variable was equivalent to one team member making an additional connection of that tie strength to every other member of the care team.
Hierarchical Linear Modeling
Multivariate analyses used 3-level (clinic/care team/patient) generalized linear mixed models (GLMMs) to test the association between team-level tie strength and patient-level alcohol-related ED visits, hospital days, and associated medical costs. The 3-level GLMMs fit ED and hospital count data with a Poisson regression model (GLMM model with a log link). The Poisson distribution is a heavy tailed, positively skewed distribution. Medical costs were fit with a normal link function.
Hierarchical data analysis accounted for clustering of patients by primary care team and primary care teams by clinic (Dickinson and Basu, 2005). By incorporating a nested structure (clinic/team/patient) into the 3-level model, the analysis controlled for both patient-level and clinic-level effects. A random intercept term in the model captured clinic-level fixed effects.
First, GLMMs #1–24 independently tested the number of strong/strong, strong/weak, weak/strong, and weak/weak face-to-face and electronic communication ties as predictors of alcohol-related utilization and cost. Separate models were developed for the team as a whole and for the team’s PCP, RNs, LPNs/MAs, laboratory/radiology technicians, and medical receptionists, while adjusting for patient-level covariates (age, gender, race/ethnicity, insurance, chronic medical conditions and Charlson Comorbidity Index) and clinic-level fixed effects.
Second, stepwise multivariate GLMM models #25–28 evaluated the independent main effects of simultaneously entered communication network measures while controlling for patient-level covariates (age, gender, race/ethnicity, insurance, chronic medical conditions and Charlson Comorbidity Index) and clinic-level fixed effects.
Finally, we conducted a series of sensitivity analyses to test whether our GLMM models had fully controlled for patient characteristics and whether additional team attributes could confound the relationship between team social network structures and patient outcomes. Sensitivity models added last recorded alcohol use, tobacco use, team size, the percent of part-time team members, the average number of years team members worked at the clinic, and the ratio of RNs to other staff members in the team as potential confounders.
The analyses used Ucinet 6 for constructing networks and obtaining SNA measurements, and used HLM 7.0 for constructing GLMM models.
RESULTS
This study included 31 primary care teams operating at 6 primary care clinics. A total of 160 health professionals were invited to participate and 155 (97%) completed the study survey (Table 1). Participating staff included 27 primary care practitioners (20 MD/DO, 7 NP/PA), 30 RNs, 30 MAs or LPNs, 38 medical receptionists, 24 laboratory or radiology technicians, and 6 clinic managers.
Table 1.
Study Sample
| Primary Care Team Members (N=155 from 6 primary care clinics, 97% response rate) | |
|---|---|
| Team Member Characteristics | N (%) |
| Female | 147 (94.8) |
| Job Position in Clinic | |
| Physician (MD/DO) | 20 (12.9) |
| NP/PA | 7 (4.5) |
| Clinic Manager | 6 (3.9) |
| RN | 30 (19.4) |
| LPN/MA | 30 (19.4) |
| Lab/Radiology Tech | 24 (15.4) |
| Medical Receptionist | 38 (24.5) |
| Years at Clinic | |
| 1 year or less | 30 (19.4) |
| >1 to 3 years | 43 (27.7) |
| >3 to 6 years | 29 (18.7) |
| >6 to 10 years | 16 (10.3) |
| >10 years | 37 (23.9) |
| % Full Time Employment | |
| 50% or less | 23 (14.8) |
| >50% to 75% | 28 (18.1) |
| >75% | 104 (67.1) |
| Team Size | Mean (sd) |
| Number of Primary Care Team Members | 18.7 (4.9) |
| Range | 12–28 |
| Team Patient Panels (N=18,402 patients in 6 primary care clinics) | |
| Patient Characteristics | Mean (sd) |
| Age | 45.7 (1.9) |
| Female (%) | 60.6 (0.4) |
| Race/Ethnicity (%) | |
| Non-Hispanic White | 87.4 (1.2) |
| Black | 2.4 (0.5) |
| White Hispanic | 3.1 (0.7) |
| Asian | 1.1 (0.2) |
| Insurance (%) | |
| Commercial | 71.2 (1.6) |
| Medicare | 16.4 (1.7) |
| Medicaid | 6.3 (0.6) |
| Uninsured | 6.0 (0.3) |
| Chronic Conditions (%) | |
| Acute Myocardial Infarction | 3.0 (0.7) |
| Asthma | 11.6 (0.9) |
| Atrial Fibrillation | 6.9 (0.7) |
| Cancer | 4.4 (0.5) |
| Cerebrovascular Disease | 4.1 (0.5) |
| Chronic Kidney Disease | 8.1 (1.0) |
| Chronic Obstructive Pulmonary Disease | 3.4 (0.3) |
| Congestive Heart Failure | 2.1 (0.3) |
| Dementia | 1.6 (0.2) |
| Depression | 25.7 (1.3) |
| Diabetes | 10.3 (1.0) |
| Hyperlipidemia | 31.6 (3.0) |
| Hypertension | 31.5 (2.7) |
| Ischemic Heart Disease | 4.1 (0.6) |
| Osteoarthritis | 9.6 (1.5) |
| Osteoporosis | 3.9 (0.5) |
| Peptic Ulcer | 0.9 (0.1) |
| Rheumatoid arthritis | 1.7 (0.2) |
| Charlson Co-Morbidity Index, mean | 0.8 (0.4) |
| Alcohol-Related Health Care Use, Past 12 Months | Mean (sd) |
| Emergency dept. visits (per 1000 patients in team panel) | 1.7 (0.5) |
| Hospital days (per 1000 patients in team panel) | 16.1 (3.8) |
| Medical costs (US$ per 1000 patients in team panel) | $27,292 ($6,366) |
| Team Patient Panel Size | Mean (sd) |
| Patient Panel Size per Primary Care Team | 613.4 (364.9) |
| Range | 54–1268 |
MD=Medical Doctor; DO=Doctor of Osteopathy; NP=Nurse Practitioner; PA=Physician Assistant; RN=Registered Nurse; LPN=Licensed Practical Nurse; MA=Medical Assistant
Participants were 95% female, which is in line with U.S. Census Bureau data indicating that 91% of all nurses, nurse practitioners, and licensed practice nurses, and 97% of all medical receptionists, are female (National Center for Health Workforce Analysis (U.S.), 2013). One fifth of study participants had worked at their practice for 1 year or less and just under a third worked part-time, defined as 75% time or less.
Care teams ranged in size from 12 to 28 individuals, with an average team size of 19 team members (Table 1). PCPs led a single care team; other team members (RNs, LPNs/MAs, etc.) could belong to multiple care teams as self-reported on the team membership question. On average, clinic members other than the PCP belonged to 4 primary care teams.
Patient panels were 61% female, predominantly non-Hispanic white (87%), and most had private insurance (71%). Chronic diseases were common, with 26% of patients diagnosed with diabetes and 31% with hypertension. On average there were 1.7 alcohol-related ED visits and 16.1 alcohol-related hospital days per 1,000 patients in the team patient panel in the past 12 months. Alcohol-related health care costs in the past 12 months averaged US$27,000 per 1,000 team panel patients.
As seen in Table 2, within their primary care teams, PCPs received more strong EHR communication ties (6.7, sd 3.4) than face-to-face ties (5.6, sd 2.1). The data indicate that, on average approximately 7 team members communicated face-to-face with the PCP daily or multiple times per day, and 6 team members communicated electronically with the PCP daily or multiple times per day. RNs received the most communication ties both face-to-face (8.8, sd 2.6) and electronically (6.7, sd 1.6). On average, the team’s RNs received daily or more frequent face-to-face communication about patient care from 9 other team members and daily or more frequent electronic communication about patient care from 7 other team members. Laboratory and radiology technicians had the fewest number of daily communication connections, both face-to-face and electronically.
Table 2.
Strong and Weak Connections in Team Communication Networks (n=31 care teams)
| Face-to-Face Communication, In-Degreea ties | EHR Communication, In-Degreea ties | ||||
|---|---|---|---|---|---|
| N | Strong Tiesb | Weak Tiesc | Strong Tiesb | Weak Tiesc | |
| PCP | 27 | 5.6 (2.1) | 4.6 (2.2) | 6.7 (3.4) | 4.3 (2.4) |
| RN | 30 | 8.8 (2.6) | 4.7 (2.5) | 6.7 (1.6) | 3.8 (1.8) |
| LPN/MA | 29 | 8.6 (2.3) | 4.4 (2.0) | 6.4 (2.0) | 3.5 (1.6) |
| Lab/Radiology Tech | 23 | 5.0 (2.1) | 5.3 (2.6) | 1.9 (1.3) | 2.4 (2.1) |
| Medical Receptionist | 38 | 7.4 (2.3) | 4.9 (2.5) | 4.6 (1.7) | 2.9 (1.8) |
In-Degree denotes count of communication connections or ties directed toward the individual from other team members
Strong ties denote team member communication connections occurring “a few times each day” or “once each day”.
Weak ties denote team member communication connections occurring “a few times a week” or “once per week”.
PCP=Primary Care Practitioner (MD, DO, NP, or PA); RN=Registered Nurse; LPN=Licensed Practical Nurse; MA=Medical Assistant
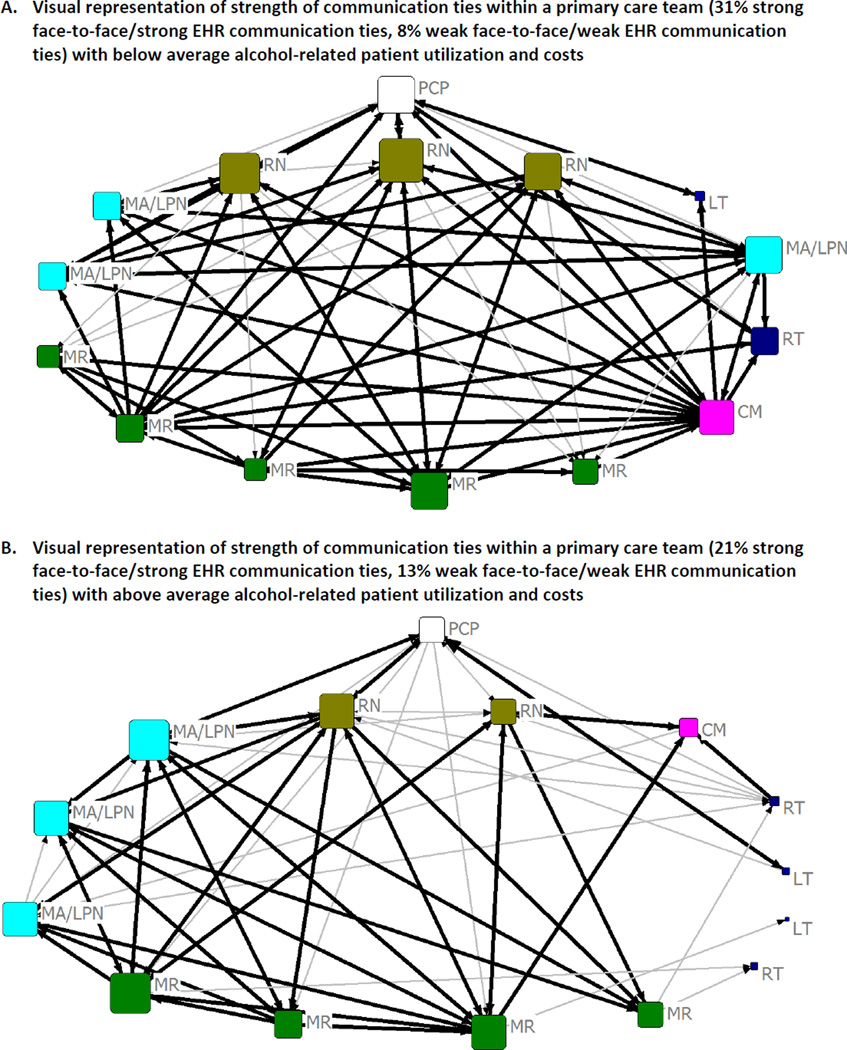
Figure 1 visually represents the communication networks in two study teams. Team A, which was in the lowest quartile of alcohol-related health care utilization and costs, had significantly more strong communication connections among the team members than weak ties both face-to-face and through the EHR. Team B, which was in the highest quartile of alcohol-related health care utilization and costs, had fewer strong communication ties and more weak communication connections. Notably, in Team B the laboratory and radiology technicians had very few strong communication ties. One technician had a single weak (weekly or several times a week) connection within the patient care team.
Figure 1. Primary Care Team Communication Networks about Patient Care.
Bold line=strong connection; Pale line=weak connection; Symbol size proportional to in-degree (strong+weak); PCP=Primary Care Practitioner, RN=Registered Nurse, CM=Clinic Manager, MA/LPN=Medical Assistant, MR=Medical Receptionist, LT=Laboratory Technician, RT=Radiology Technician
Table 3 presents results from GLMM models #1–24. The first and second panels of Table 3 model frequency of alcohol-related ED visits and hospital days while adjusting for patient-level control variables and clinic-level effects. As seen in the first panel of Table 3, teams whose LPNs and MAs had more weak face-to-face ties and weak EHR communication ties had higher rates of alcohol-related ED visits (RR=1.23; 95% CI: 1.07, 1.42). Teams whose RNs or laboratory technicians had more weak face-to-face interaction paired with strong EHR communication had patients with 17% fewer alcohol-related ED visits (RR=0.83; 95% CI: 0.69, 0.99) and 20% fewer alcohol-related ED visits (RR=0.80; 95% CI: 0.65, 0.99), respectively. There was also a significant association between strong face-to-face and EHR communication ties to the team’s medical receptionists and fewer alcohol-related ED visits (RR=0.90; 95% CI: 0.82, 0.98).
Table 3.
Generalized Linear Mixed Models #1–24 of Communication Patterns by Job Position and Alcohol-Related Patient Outcomes, Adjusted for Patient Characteristics (N=31 teams, n=18,402 patients)
| Alcohol-Related Emergency Department Visits | ||||||
|---|---|---|---|---|---|---|
| In-Degree Ties | PCP | RN | Job Position LPN/MA |
Lab/Radiology | Medical Reception | Care Team |
| RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Strong F2F/Strong EHR | 1.01 (0.95, 1.08) | 0.97 (0.93, 1.02) | 1.03 (0.91, 1.15) | 0.99 (0.89, 1.09) | 0.90* (0.82, 0.98) | 0.93 (0.82, 1.06) |
| Strong F2F/Weak EHR | 1.10 (0.99, 1.22) | 1.10 (0.99, 1.22) | 0.94 (0.81, 1.10) | 0.96 (0.89, 1.03) | 1.11 (0.93, 1.34) | 1.21 (0.97, 1.52) |
| Weak F2F/Strong EHR | 0.94 (0.85, 1.04) | 0.83* (0.69, 0.99) | 0.94 (0.78, 1.14) | 0.80* (0.65, 0.99) | 1.00 (0.88, 1.15) | 0.81 (0.59, 1.13) |
| Weak F2F/Weak EHR | 0.98 (0.90, 1.06) | 1.11 (0.97, 1.27) | 1.23** (1.07, 1.42) | 0.98 (0.86, 1.11) | 1.06 (0.93, 1.22) | 1.24 (0.94, 1.65) |
| Alcohol-Related Hospitalizations | ||||||
| In-Degree Ties | PCP | RN | LPN/MA |
Job Position Lab/Radiology |
Medical Reception | Care Team |
| RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Strong F2F/Strong EHR | 1.04 (0.97, 1.11) | 0.95* (0.89, 1.00) | 1.02 (0.91, 1.15) | 1.02 (0.93, 1.12) | 0.95 (0.87, 1.05) | 1.00 (0.88, 1.14) |
| Strong F2F/Weak EHR | 1.10* (1.01, 1.21) | 1.09 (0.95, 1.21) | 1.05 (0.92, 1.210 | 1.00 (0.87, 1.15) | 1.17 (0.97, 1.41) | 1.17 (0.92, 1.49) |
| Weak F2F/Strong EHR | 1.00 (0.92, 1.09) | 0.91 (0.75, 1.10) | 0.95 (0.78, 1.17) | 1.22 (0.98, 1.51) | 1.14 (0.97, 1.35) | 1.33 (0.88, 2.01) |
| Weak F2F/Weak EHR | 1.00 (0.91, 1.09) | 1.12 (0.99, 1.26) | 1.25** (1.10, 1.41) | 0.93 (0.77, 1.13) | 1.03 (0.90, 1.19) | 1.27 (0.98, 1.66) |
| Alcohol-Related Health Costs | ||||||
| In-Degree Ties | PCP | RN | LPN/MA |
Job Position Lab/Radiology |
Medical Reception | Care Team |
| β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | β (95% CI) | |
| Str F2F/Str EHR | $33 (−$461, $527) | −$549*** (−$870, −$228) | −$39 (−$1058, $980) | $129 (−$717, $975) | −$339 (−$1023, $345) | $1030* (−$1819, −$241) |
| Str F2F/Wk EHR | $1455** ($485, $2425) | $825 (−$175, $1824) | −$297 (−$1502, $909) | $832** (−$1400, −$263) | $888 (−791, $2566) | $1274 (−$941, $3490) |
| Wk F2F/Str HER | −$128 (−$809, $552) | −$299 (−$1785, $1188) | −$412 (−$2352, $1528) | $435 (−$1319, $2188) | $15 (−$1182, $1213) | −$824 (−$4018, $2371) |
| Wk F2F/Wk EHR | $325 (−$438, $1088) | $1484** ($428, $2540) | $1909*** ($1074, $2743) | −$312 (−$1605, $980) | $550 (−$589, $1689) | $2922** ($734, $5109) |
p<.05,
p<.01,
p<.001
Patient-level covariates entered in the model: gender, age, age squared, race/ethnicity, insurance, acute myocardial infarction, asthma, atrial fibrillation, cancer, cerebrovascular disease, chronic kidney disease stage, chronic obstructive pulmonary disease severity, congestive heart failure, dementia, depression, diabetes, hyperlipidemia, hypertension, ischemic heart disease, osteoarthritis, osteoporosis, peptic ulcer disease, rheumatoid arthritis, and Charlson Comorbidity Index
F2F=Face-to-Face; EHR=Electronic Health Record; Strong tie=Communication daily or multiple times per day; Weak tie=Communication weekly or several times per week
RR=Rate Ratio; PCP=Primary Care Practitioner (MD, DO, NP, or PA); RN=Registered Nurse; LPN=Licensed Practical Nurse; MA=Medical Assistant
Panel 2 of Table 3 shows that teams whose PCP had more strong face-to-face communication ties combined with weak EHR communication had higher rates of alcohol-related hospitalization (RR=1.10; 95% CI: 1.01, 1.21). Teams whose LPNs/MAs had more weak face-to-face ties and weak EHR communication ties also had higher rates of alcohol-related hospitalization (RR=1.25; 95% CI 1.10, 1.41). In contrast, teams whose RNs had more strong face-to-face communication ties and strong electronic communication ties had significantly fewer alcohol-related hospital days (RR=0.95; 95% CI: 0.89, 1.00) in the past 12 months.
Panel 3 in Table 3 shows model results associating team network ties with health care costs. As seen in Panel 3, in an average size team of 19, for every additional team member with interactions across the whole team (strong face-to-face and strong EHR ties), there was a corresponding $1030 (95% CI: −$1819, −$241) reduction in alcohol-related patient health care costs per 1000 team patients in the past 12 months. In contrast, each additional team member with weak face-to-face and weak EHR communication connections was correlated with $2922 (95% CI: $734, $5109) higher alcohol-related patient health costs per 1000 team patients in the past 12 months. Examining connections within specific job titles, teams with PCPs who had more strong face-to-face and weak EHR communication ties had $1455 (95% CI: $485, $2425) higher alcohol-related patient costs per 1000 team patients in the past 12 months. Teams with RNs who had more strong/strong ties within the team had $549 (95% CI: −$870, −$228) lower alcohol-related healthcare costs per 1000 patients, and teams with LPNs/MAs who had more weak/weak communication ties had $1909 (95% CI: $1074, $2743) higher alcohol-related health costs per 1000 team patients in the past 12 months. There were no statistically significant associations between medical receptionist ties and alcohol-related patient costs.
Finally, Table 4 presents the multivariate GLMM model #25–28 results. Panel 1 of Table 4 shows that for each additional team member with strong ties (face-to-face and EHR) to the team’s RNs, there was an independent main effect of 10% fewer alcohol-related hospital days (RR=0.90; 95% CI: 0.84, 0.97) and $722 (95% CI: −$1261, −$183) lower alcohol-related health costs per 1000 team patients in the past 12 months. Panel 2 of Table 4 demonstrates that teams whose PCPs had more strong face-to-face ties and more weak EHR ties were linked to 12% (RR=1.12; 95% CI: 1.03, 1.23) more alcohol-related hospital days and $1428 (95% CI: $378, $2478) higher alcohol-related health costs per 1000 team patients in the past 12 months. Finally, Panel 4 of Table 4 indicates that teams whose LPNs/MAs had more weak face-to-face and weak EHR communication ties had 20% (RR=1.20; 95% CI: 1.03, 1.39) higher rates of ER visits, 24% (RR=1.24; 95% CI: 1.12, 1.37) more hospital days, and $1600 (95% CI: $592, $2608) greater alcohol-related healthcare costs per 1000 team patients in the past 12 months.
Table 4.
Multivariate Generalized Linear Mixed Models #25–28 of Team Communication Networks and Alcohol-Related Patient Outcomes, Adjusted for Patient Characteristics (N=31 teams, n=18,402 patients)
| In-Degree Ties | Job Position | ER Visits | Hospital Days | Medical Cost |
|---|---|---|---|---|
| Strong F2F/Strong EHR | PCP | 0.96 (0.87, 1.05) | 0.99 (0.91, 1.08) | −$49 (−$591, $493) |
| Strong F2F/Strong EHR | RN | 1.00 (0.94, 1.07) | 0.90** (0.84, 0.97) | −$722** (−$1261, −$183) |
| Strong F2F/Strong EHR | LPN/MA | 1.08 (0.94, 1.25) | 1.05 (0.93, 1.19) | $203 (−$749, $1155) |
| Strong F2F/Strong EHR | Lab/Radiology Tech | 1.01 (0.90, 1.14) | 1.08 (0.97, 1.21) | $486 (−$419, $1391) |
| Strong F2F/Strong EHR | Medical Receptionist | 0.86* (0.76, 0.98) | 0.99 (0.89, 1.10) | $92 (−$659, $843) |
| In-Degree Ties | Job Position | ER Visits | Hospital Days | Medical Cost |
| Strong F2F/Weak EHR | PCP | 1.08 (0.98, 1.19) | 1.12* (1.03, 1.23) | $1428** ($378, $2478) |
| Strong F2F/Weak EHR | RN | 1.12 (0.98, 1.28) | 1.07 (0.94, 1.21) | $880 (−$207, $1968) |
| Strong F2F/Weak EHR | LPN/MA | 0.90 (0.81, 1.01) | 0.97 (0.88, 1.07) | −$364 (−$1402, $675) |
| Strong F2F/Weak EHR | Lab/Radiology Tech | 0.94 (0.83, 1.06) | 0.91 (0.83, 1.00) | −$429 (−$1198, $340) |
| Strong F2F/Weak EHR | Medical Receptionist | 1.20 (0.92, 1.57) | 1.15 (0.93, 1.42) | −$334 (−$2132, $1463) |
| In-Degree Ties | Job Position | ER Visits | Hospital Days | Medical Cost |
| Weak F2F/Strong EHR | PCP | 0.92 (0.82, 1.03) | 0.98 (0.90, 1.06) | −$276 (−$1150, $597) |
| Weak F2F/Strong EHR | RN | 0.87 (0.74, 1.02) | 0.89 (0.74, 1.07) | −$626 (−$2257, $1004) |
| Weak F2F/Strong EHR | LPN/MA | 1.05 (0.89, 1.25) | 1.11 (0.91, 1.34) | $259 (−$1947, $2466) |
| Weak F2F/Strong EHR | Lab/Radiology Tech | 0.76* (0.59, 0.98) | 1.33* (1.06, 1.68) | $1062 (−$1054, $3179) |
| Weak F2F/Strong EHR | Medical Receptionist | 0.97 (0.88, 1.08) | 1.16 (0.99, 1.35) | −$58 (−$1434, $1319) |
| In-Degree Ties | Job Position | ER Visits | Hospital Days | Medical Cost |
| Weak F2F/Weak EHR | PCP | 0.95 (0.86, 1.04) | 0.99 (0.93, 1.06) | $298 (−$385, $981) |
| Weak F2F/Weak EHR | RN | 1.13 (0.94, 1.36) | 1.14** (1.04, 1.26) | $991 (−$101, $2082) |
| Weak F2F/Weak EHR | LPN/MA | 1.20* (1.03, 1.39) | 1.24*** (1.12, 1.37) | $1600** ($592, $2608) |
| Weak F2F/Weak EHR | Lab/Radiology Tech | 0.96 (0.86, 1.07) | 0.91* (0.84, 0.99) | −$798 (−$1619, $23) |
| Weak F2F/Weak EHR | Medical Receptionist | 1.04 (0.91, 1.19) | 0.90 (0.81, 1.00) | −$640 (−$1683, $404) |
p<.05,
p<.01,
p<.001
Patient-level covariates entered in the model: gender, age, age squared, race/ethnicity, insurance, acute myocardial infarction, asthma, atrial fibrillation, cancer, cerebrovascular disease, chronic kidney disease stage, chronic obstructive pulmonary disease severity, congestive heart failure, dementia, depression, diabetes, hyperlipidemia, hypertension, ischemic heart disease, osteoarthritis, osteoporosis, peptic ulcer disease, rheumatoid arthritis, and Charlson Comorbidity Index
PCP=Primary Care Practitioner (MD, DO, NP, or PA); RN=Registered Nurse; LPN=Licensed Practical Nurse; MA=Medical Assistant
Sensitivity analyses showed similar results after adjusting for last recorded alcohol use, tobacco use, team size, percent of part-time team members, average number of years that team members worked at the clinic, and ratio of RNs to other staff members in the team (full results available upon request). In addition, one PCP had been in the study clinic for only 6 months, which resulted in a low number of patients (n=54) seen twice in the past 3 years by this PCP. Sensitivity analyses that excluded this PCP from the analysis sample found consistent or nearly identical results (available upon request).
DISCUSSION
This study evaluates the primary care team interactions about patient care that are associated with better alcohol-related patient outcomes and lower costs. Overall, our results show that teams’ variations in communication patterns are associated with statistically significant differences in alcohol-related patient utilization and medical costs in their patient panels.
Our findings demonstrate that teams with RNs who have more strong face-to-face and strong EHR ties (multiple times per day) have patients with significantly fewer alcohol-related acute care visits and lower costs. In an average size team of 19, for each additional team member interacting with the RN (daily face-to-face and EHR connection), the team’s patients experienced 10% fewer alcohol-related hospital days and $722 less in alcohol-related medical costs per 1000 team patients in the past 12 months.
In contrast, teams with PCPs who interact with more team members daily face-to-face and who have more infrequent (weekly) EHR communications with other team members have more alcohol-related care and costs. For every additional team member in the PCP’s strong face-to-face connection network (frequent daily ties, or in-degree), the team’s patients experienced 12% more alcohol-related hospital days and spend $1428 more in alcohol-related medical costs per 1000 team patients in the past 12 months. This suggests that teams whose daily face-to-face communication to the PCP has been streamlined to a smaller number of team members (i.e., fewer strong face-to-face ties to PCP) could have better alcohol-related outcomes.
Interestingly, the less integrated the LPNs/MAs are into the team care, as evidenced by weak connections (weekly face-to-face and EHR in-degree), the more alcohol-related patient visits and higher costs. If each LPN/MA converted one weak connection to a strong connection, there could be 24% fewer hospital days and $1600 lower costs per 1000 team patients in the past 12 months.
Our findings suggest that increasing (even by 1 connection) frequent daily face-to-face and EHR interactions between RNs and all team members, including LPNs/MAs, and streamlining PCP communication with fewer team members, could be a cost-effective way to provide better alcohol-related patient outcomes and lower medical costs. Future interventions are needed to explore this further.
Notably, our findings may underestimate the full impact of teams’ communication patterns on alcohol-related patient outcomes and costs due to the well-established underreporting of alcohol-related diagnoses in EHRs. While primary care clinicians and staff may identify 52% of cases of excessive alcohol use, they would make a correct notation of it in the EHR in only 37% of cases (Mitchell et al., 2012). Since our alcohol-related health utilization data are drawn from EHRs, it is possible that our study observed only a third of alcohol-related ER visits and hospital stays due to underreporting of alcohol-related ICD9 codes. As such, this analysis may have observed just a tip of the iceberg in health care utilization by excessive alcohol drinking patients (United States. Substance Abuse and Mental Health Services Administration., 2012).
Our results come to full light if they are considered in view of the Affordable Care Act. When fully implemented, the Patient Protection and Affordable Care Act (ACA) of 2010 will provide unprecedented access to an estimated 27 million uninsured individuals and will reach in total 62.5 million Americans (Beronio et al., 2013, 2010). New ACA enrollees are at higher risk for alcohol-related health issues (Somers et al., 2014). New ways are needed to improve alcohol-related care and lower costs for the greater number of excessive alcohol-using patients expected in primary care. A centerpiece of this effort is patient-centered primary care redesign. Our study contributes to this initiative by demonstrating which communication networks are associated with better outcomes and lower costs.
Finally, it is important to emphasize that this study cannot argue for a causal mechanism between team communication networks and alcohol-related patient outcomes due to the cross-sectional nature of the study. Longitudinal and experimental studies are called for to explore the causal pathways between team communication variables and alcohol-related patient care.
Strengths and Limitations
Strengths of the undertaking lie in the very high response rates and virtually complete communication networks data for all the primary care teams, the team level quality of care patient outcomes derived from EHRs, numerous medical chronic condition data to adjust for patient-level confounding and sophisticated statistical methods.
Our findings should be viewed in light of the limitations. First, our study is based on data from only 6 practices in the same geographical location, so the results may not be generalizable to a broad national level context. Second, our study looked only at frequency of communication and did not attempt to measure communication content. Prior research suggests that high quality care for excessive alcohol-using patients, comprised of identifying and engaging excessive alcohol users in the primary care setting, addressing how excessive alcohol use confounds preventive and chronic disease care, and providing brief intervention or referral to treatment for excessive alcohol-using patients, reduces primary-care sensitive hospital and ED visits. We do not have precise information on the frequency and quality of alcohol services delivered to excessive alcohol-using patients in the study clinics. Future research is needed to directly address the link between team communication structures and quality of alcohol services delivered for excessive alcohol drinkers. Third, our study did not explore why different team members choose a particular mode of communication (i.e., face-to-face vs EHR) to discuss patient care. Fourth, we do not limit our alcohol-related ED and hospital stay diagnoses to the primary visit diagnosis. Therefore, we cannot rule out the possibility that the alcohol-related ED and hospital visits identified in our EHR search are utilization by patients with alcohol-related diagnoses as opposed to alcohol-related events. It is possible that our EHR search identifies health utilization outcomes for risky alcohol drinkers as well as for alcohol-dependent drinkers. It is essential to target both groups of alcohol misusing patients in primary care. The US Preventive Services Task Force recommends that clinicians screen adults aged 18 years or older for alcohol misuse and provide persons engaged in risky or hazardous drinking with brief behavioral counseling interventions to reduce alcohol misuse (Moyer and USPSTF, 2013). Our study findings contribute to this urgent need. Finally, due to the large number of statistical tests reported, there is an increased chance of Type I error (i.e., detecting an effect that is not present) in our findings. As the number of comparisons increases, the likelihood of comparison groups to differ in at least one attribute increases. In light of this analytical consideration, the study results should be viewed as exploratory and should be confirmed by future research. The outcome patterns seen in our data are not necessarily consistent across all study outcomes, suggesting that the frequency or mode of team communication may vary in its significance based on the severity and complexity of the alcohol using patient’s medical, psychological and social condition. For example, the excessive alcohol user who uses the emergency department (e.g., following a motor vehicle crash) may be fundamentally different than the excessive alcohol user who has a hospital stay (e.g., as a result of liver cirrhosis) and may be affected differently by primary care team communication. In light of the major changes happening in U.S. primary care under the Affordable Care Act of 2010 (Beronio et al., 2013), and the enormous societal burden associated with excessive alcohol use, future research is needed to evaluate further how different patterns of team communication relate to individualized patient-centered care delivery to manage alcohol misuse, a complex multifaceted health condition.
Conclusions
This study demonstrates that team communication patterns may contribute to better alcohol-related patient care quality at a lower cost in primary care. Excessive alcohol-using patients may fair better if they are cared for by teams with RNs who interact with more team members including LPNs/MAs (face-to-face and by EHR multiple times per day), and by teams whose frequent daily face-to-face communication to the PCP has been streamlined to a smaller number of team members.
Supplementary Material
Acknowledgments
Funding/Support: Dr Mundt received support from NIAAA grant K01AA018410-04 for the design and conduct of the study. The project was partially supported by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
REFERENCES
- Adam T, Koopmanschap MA, Evans DB. Cost-effectiveness analysis: can we reduce variability in costing methods? Int J Technol Assess Health Care. 2003;19:407–420. doi: 10.1017/s0266462303000369. [DOI] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality. [Accessed May 6, 2014];Expenses for a Hospital Emergency Room Visit, 2003 [AHRQ Website] 2006 Available at: http://meps.ahrq.gov/mepsweb/data_files/publications/st111/stat111.pdf.
- Agency for Healthcare Research and Quality. HCUP Clinical Classifications Software (CCS) for ICD-9-CM [AHRQ Website] Rockville, MD: Healthcare Cost and Utilization Project (HCUP); 2009. [Accessed October 22, 2014]. Available at: www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp. [Google Scholar]
- Aspy CB, Mold JW, Thompson DM, Blondell RD, Landers PS, Reilly KE, Wright-Eakers L. Integrating screening and interventions for unhealthy behaviors into primary care practices. Am J Prev Med. 2008;35:S373–S380. doi: 10.1016/j.amepre.2008.08.015. [DOI] [PubMed] [Google Scholar]
- Baker DP, Day R, Salas E. Teamwork as an essential component of high-reliability organizations. Health Serv Res. 2006;41:1576–1598. doi: 10.1111/j.1475-6773.2006.00566.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck CA, Southern DA, Saitz R, Knudtson ML, Ghali WA. Alcohol and drug use disorders among patients with myocardial infarction: associations with disparities in care and mortality. PLoS One. 2013;8:e66551. doi: 10.1371/journal.pone.0066551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckers Hospital Review. [Accessed May 6, 2014];Average cost per inpatient day across 50 states in 2010 [Beckers Hospital Review Website] 2010 Available at: http://www.beckershospitalreview.com/lists/average-cost-per-inpatient-day-across-50-states-in-2010.html.
- Beronio K, Po R, Skopec L, Glied S. [Accessed October 22, 2014];ASPE Issue Brief, Affordable Care Act Will Expand Mental Health and Substance Use Disorder Benefits and Parity Protections for 62 Million Americans [ASPE Website] 2013 Available at: http://aspe.hhs.gov/health/reports/2013/mental/rb_mental.pdf.
- Borgatti SP, Halgin DS. On Network Theory. Organ Sci. 2011;22:1168–1181. [Google Scholar]
- Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD. Economic Costs of Excessive Alcohol Consumption in the US, 2006. Am J Prev Med. 2011;41:516–524. doi: 10.1016/j.amepre.2011.06.045. [DOI] [PubMed] [Google Scholar]
- Bray JW, Cowell AJ, Hinde JM. A systematic review and meta-analysis of health care utilization outcomes in alcohol screening and brief intervention trials. Med Care. 2011;49:287–294. doi: 10.1097/MLR.0b013e318203624f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell SM, Hann M, Hacker J, Burns C, Oliver D, Thapar A, Mead N, Safran DG, Roland MO. Identifying predictors of high quality care in English general practice: observational study. Brit Med J. 2001;323:784–787. doi: 10.1136/bmj.323.7316.784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. [Accessed October 22, 2014];Alcohol and Public Health [CDC Website] 2014 Available at: http://www.cdc.gov/alcohol/faqs.htm#heavyDrinking.
- CDC. [Accessed June 8, 2012];Alcohol Use [CDC Website] Centers for Disease Control and Prevention. 2012 2012 Available at: http://www.cdc.gov/Vitalsigns/BingeDrinking.
- Centers for Medicare and Medicaid Services (CMS) [Accessed October 22, 2014];Chronic Condition Data Warehouse [CMS Website] 2014 Available at: https://www.ccwdata.org/web/guest/condition-categories.
- Chambers D, Wilson P, Thompson C, Harden M. Social Network Analysis in Healthcare Settings: A Systematic Scoping Review. Plos One. 2012;7(8) doi: 10.1371/journal.pone.0041911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, Mackenzie CR. A New Method of Classifying Prognostic Co-Morbidity in Longitudinal-Studies - Development and Validation. J Chron Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Cruvinel E, Richter KP, Bastos RR, Ronzani TM. Screening and brief intervention for alcohol and other drug use in primary care: associations between organizational climate and practice. Addict Sci Clin Pract. 2013;8:4. doi: 10.1186/1940-0640-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickinson LM, Basu A. Multilevel modeling and practice-based research. Ann Fam Med. 2005;3:S52–S60. doi: 10.1370/afm.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dilonardo J. Workforce Issues Related to: Physical and Behavioral Healthcare Integration. Workforce Issues: Integrating Substance Use Services into Primary Care Conference-Joint ONDCP/SAMSHA/HRSA Meeting; Washington DC. 2011. [Accessed October 22, 2014]. Available at: http://www.integration.samhsa.gov/clinical-practice/ondcp_framework_paper.pdf. [Google Scholar]
- Fleming M, Manwell LB. Brief intervention in primary care settings. A primary treatment method for at-risk, problem, and dependent drinkers. Alcohol Res Health. 1999;23:128–137. [PMC free article] [PubMed] [Google Scholar]
- Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Brief physician advice for problem drinkers: long-term efficacy and benefit-cost analysis. Alcohol Clin Exp Res. 2002;26:36–43. [PubMed] [Google Scholar]
- Hess DR, Tokarczyk A, O'Malley M, Gavaghan S, Sullivan J, Schmidt U. The value of adding a verbal report to written handoffs on early readmission following prolonged respiratory failure. Chest. 2010;138:1475–1479. doi: 10.1378/chest.09-2140. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Edwards EM, Saitz R. Young Adults at Risk for Excess Alcohol Consumption Are Often Not Asked or Counseled About Drinking Alcohol. J Gen Intern Med. 2012;27:179–184. doi: 10.1007/s11606-011-1851-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel Y, Hollander O, Sanchez-Craig M, Booker S, Miller V, Gingrich R, Rankin JG. Screening for problem drinking and counseling by the primary care physician-nurse team. Alcohol Clin Exp Res. 1996;20:1443–1450. doi: 10.1111/j.1530-0277.1996.tb01147.x. [DOI] [PubMed] [Google Scholar]
- Jonas DE, Garbutt JC, Amick HR, Brown JM, Brownley KA, Council CL, Viera AJ, Wilkins TM, Schwartz CJ, Richmond EM, Yeatts J, Evans TS, Wood SD, Harris RP. Behavioral counseling after screening for alcohol misuse in primary care: a systematic review and meta-analysis for the U.S. Preventive Services Task Force. Ann Intern Med. 2012;157:645–654. doi: 10.7326/0003-4819-157-9-201211060-00544. [DOI] [PubMed] [Google Scholar]
- Kaner EF, Dickinson HO, Beyer F, Pienaar E, Schlesinger C, Campbell F, Saunders JB, Burnand B, Heather N. The effectiveness of brief alcohol interventions in primary care settings: a systematic review. Drug Alcohol Rev. 2009;28:301–323. doi: 10.1111/j.1465-3362.2009.00071.x. [DOI] [PubMed] [Google Scholar]
- Kim TW, Saitz R, Kretsch N, Cruz A, Winter MR, Shanahan CW, Alford DP. Screening for Unhealthy Alcohol and Other Drug Use by Health Educators: Do Primary Care Clinicians Document Screening Results? J Addict Med. 2013;7:204–209. doi: 10.1097/ADM.0b013e31828da017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer KL. The cost-effectiveness and cost-benefit of screening and brief intervention for unhealthy alcohol use in medical settings. Subst Abus. 2007;28:67–77. doi: 10.1300/J465v28n03_07. [DOI] [PubMed] [Google Scholar]
- McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, Kerr EA. The quality of health care delivered to adults in the United States. New Engl J Med. 2003;348:2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- Mertens JR, Lu YW, Parthasarathy S, Moore C, Weisner CM. Medical and psychiatric conditions of alcohol and drug treatment patients in an HMO: comparison with matched controls. Arch Intern Med. 2003;163:2511–2517. doi: 10.1001/archinte.163.20.2511. [DOI] [PubMed] [Google Scholar]
- Mitchell AJ, Malone D, Doebbeling CC. Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies. Br J Psychiatry. 2009;194:491–499. doi: 10.1192/bjp.bp.107.045732. [DOI] [PubMed] [Google Scholar]
- Mitchell AJ, Meader N, Bird V, Rizzo M. Clinical recognition and recording of alcohol disorders by clinicians in primary and secondary care: meta-analysis. Br J Psychiatry. 2012;201:93–100. doi: 10.1192/bjp.bp.110.091199. [DOI] [PubMed] [Google Scholar]
- Moyer VA US Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159:210–218. doi: 10.7326/0003-4819-159-3-201308060-00652. [DOI] [PubMed] [Google Scholar]
- National Institute of Alcohol Abuse and Alcoholism. [Accessed June 8, 2012];National Institute of Alcohol Abuse and Alcoholism Council approves definition of binge drinking [NIAAA Website] 2004 Available at: http://pubs.niaaa.nih.gov/publications/Newsletter/winter2004/Newsletter_Number3.pdf.
- Quinn RE, Dutton JE. Coordination as energy-in-conversation. Acad Manage Rev. 2005;30:36–57. [Google Scholar]
- Rehm J. The risks associated with alcohol use and alcoholism. Alcohol Res Health. 2011;34:135–143. [PMC free article] [PubMed] [Google Scholar]
- Reiff-Hekking S, Ockene JK, Hurley TG, Reed GW. Brief physician and nurse practitioner-delivered counseling for high-risk drinking - Results at 12-month follow-up. J Gen Intern Med. 2005;20:7–13. doi: 10.1111/j.1525-1497.2005.21240.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roche AM, Freeman T, Skinner N. From data to evidence, to action: findings from a systematic review of hospital screening studies for high risk alcohol consumption. Drug Alcohol Depend. 2006;83:1–14. doi: 10.1016/j.drugalcdep.2005.10.011. [DOI] [PubMed] [Google Scholar]
- Saitz R, Freedner N, Palfai TP, Horton NJ, Samet JH. The severity of unhealthy alcohol use in hospitalized medical patients. The spectrum is narrow. J Gen Intern Med. 2006;21:381–385. doi: 10.1111/j.1525-1497.2006.00405.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solberg LI, Maciosek MV, Edwards NM. Primary care intervention to reduce alcohol misuse ranking its health impact and cost effectiveness. Am J Prev Med. 2008;34:143–152. doi: 10.1016/j.amepre.2007.09.035. [DOI] [PubMed] [Google Scholar]
- Somers SA, Nicolella E, Hamblin A, Mcmahon SM, Heiss C, Brockmann BW. Medicaid expansion: Considerations for states regarding newly eligible jail-involved individuals. Health Aff. 2014;33:455–461. doi: 10.1377/hlthaff.2013.1132. [DOI] [PubMed] [Google Scholar]
- Stevenson K, Baker R, Farooqi A, Sorrie R, Khunti K. Features of primary health care teams associated with successful quality improvement of diabetes care: a qualitative study. Fam Pract. 2001;18:21–26. doi: 10.1093/fampra/18.1.21. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. National Survey on Drug Use and Health series H-44. Rockville, MD: U.S. Dept. of Health and Human Services Substance Abuse and Mental Health Services Administration Center for Behaviorial Health Statistics and Quality; 2012. Results from the 2011 National Survey on Drug Use and Health summary of national findings. [Google Scholar]
- Sullivan LE, Tetrault JM, Braithwaite RS, Turner BJ, Fiellin DA. A Meta-analysis of the Efficacy of Nonphysician Brief Interventions for Unhealthy Alcohol Use: Implications for the Patient-Centered Medical Home. Am J Addict. 2011;20:343–356. doi: 10.1111/j.1521-0391.2011.00143.x. [DOI] [PubMed] [Google Scholar]
- The Lewin Group. [Accessed October 22, 2014];Economic Costs of Excessive Alcohol Consumption in the United States [Lewin Group Website] 2013 Available at: http://www.lewin.com/~/media/Lewin/Site_Sections/Publications/CDC_Report_Rev.pdf.
- The Patient Protection and Affordability Act. Pub. L. No. 2010:111–148. [Google Scholar]
- U.S. National Center for Health Workforce Analysis. The U.S. Health Workforce Chartbook. Rockville, Md.: U.S. Dept. of Health and Human Services, Health Resources and Services Administration Bureau of Health Professions, National Center for Health Workforce Analysis; 2013. [Google Scholar]
- Walley AY, Paasche-Orlow M, Lee EC, Forsythe S, Chetty VK, Mitchell S, Jack BW. Acute care hospital utilization among medical inpatients discharged with a substance use disorder diagnosis. J Addict Med. 2012;6:50–56. doi: 10.1097/ADM.0b013e318231de51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinick RM, Bristol SJ, DesRoches CM. Urgent care centers in the US: Findings from a national survey. Bmc Health Serv Res. 2009:9. doi: 10.1186/1472-6963-9-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willenbring ML. Gaps in Clinical Prevention and Treatment for Alcohol Use Disorders Costs, Consequences, and Strategies. Alcohol Research-Current Reviews. 2013;35:238–243. doi: 10.35946/arcr.v35.2.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zgierska A, Fleming MF. Screening and brief interventions for alcohol and drug misuse and disorders. In: Ries RK, Fiellin DA, Miller SC, Saitz R, editors. Principles of Addiction Medicine. 4th ed. Chevy Chase, MD: Lippincott Williams & Wilkins; 2009. pp. 267–294. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.