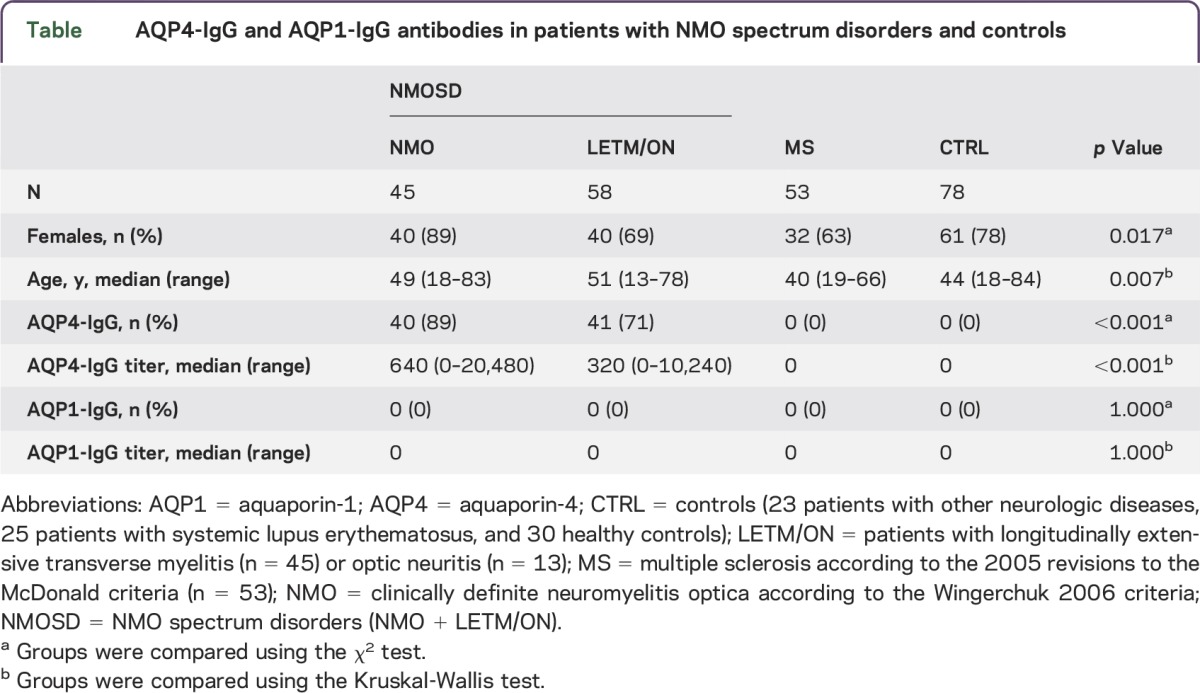
Although more than 70% of all patients with neuromyelitis optica (NMO) are seropositive for aquaporin-4 (AQP4) antibodies, a substantial proportion of patients fulfilling the clinical criteria for NMO or limited forms of the disease (NMO spectrum disorders [NMOSD]) are negative for these antibodies.1 This raises the possibility of other autoantibodies in these patients. One putative target, the ubiquitously expressed water channel aquaporin-1 (AQP1), which is partially lost or internalized in certain NMO lesions,2 was described in a subset of patients with NMOSD.3–5 However, AQP1 antibodies were also found in patients with multiple sclerosis (MS), thus raising concerns about the specificity of these findings. Therefore, we developed a recombinant live cell immunofluorescence assay (CBA) for AQP1 antibodies based on our AQP4 antibody assay.6 We analyzed 176 serum samples from Austrian patients with NMOSD (n = 67), Austrian patients with MS (n = 31), and controls (n = 78) for the presence of IgG AQP1 antibodies and AQP4 antibodies. Furthermore, both assays were validated in a blinded cohort of 58 patients with NMOSD (n = 36) or MS (n = 22) from Lyon (France) and Oxford (United Kingdom). Clinical and demographic data of patients and controls are shown in the table.
Table.
AQP4-IgG and AQP1-IgG antibodies in patients with NMO spectrum disorders and controls
Methods.
Analysis of AQP1 antibodies and AQP4 antibodies was performed using a live CBA described previously.6 Briefly, HEK293A cells were transiently transfected using the pcDNA6.2C-EmGFP-GW/TOPO plasmid (Invitrogen, Carlsbad, CA), expressing AQP4 (isoform M23) or AQP1 (isoform 1) fused C-terminally to emerald green fluorescence protein. Transfected cells were blocked with goat IgG in phosphate-buffered saline (PBS)/10% fetal calf serum (FCS) (Sigma-Aldrich, St. Louis, MO) followed by serum diluted 1:20 and 1:40 in PBS/FCS for 1 hour at 4°C. Serum preabsorption with liver powder was not performed because a previous report indicated loss of AQP1 antibodies after pretreatment.3 Bound antibodies were detected using Cy3Tm-conjugated goat anti-human IgG antibody (Jackson ImmunoResearch Laboratories, West Grove, PA) for 30 minutes at room temperature. Bound antibodies were determined using a fluorescence microscope (Leica DMI 4000B). All samples were evaluated by 2 independent, clinically blinded investigators who agreed on all samples.
Standard protocol approvals, registrations, and patient consents.
The present study was approved by the ethical committee of Medical University of Innsbruck (#AM3041a), the Oxfordshire Research Ethics Committee (#10/H0606/56), and the French data protection authority.
Results.
Expression of AQP1 was verified by staining with a commercial AQP1-specific antibody recognizing full-length AQP1. However, the antibody only recognized the target after fixation of AQP1-transfected HEK293A cells with paraformaldehyde (figure e-1A at Neurology.org/nn). In order to prove surface expression and correct topology of AQP1, a myc-tag was inserted at position T120 (extracellular loop C) by site-directed mutagenesis. Staining with an anti-myc-tag monoclonal antibody clearly showed the surface expression of AQP1 in live HEK293A cells (figure e-1B).
As seen in the table, AQP4 antibodies were detected in 81 of 103 (79%) patients with NMOSD in the combined cohorts. AQP4 antibodies were absent in 53 patients with MS and 78 controls; therefore, the specificity of the AQP4 antibody assay was 100%. In contrast, AQP1 antibodies were absent in all 234 samples from patients with NMOSD and MS and controls. Although the AQP4 antibody CBA showed high sensitivity and specificity, a comparable AQP1 antibody CBA did not detect any antibodies in 234 serum samples (figure e-1C).
Discussion.
This finding is in contrast to previous studies by 2 groups reporting the presence of AQP1 antibodies in 17%–74% of patients with NMOSD,3–5 but also in controls. In our opinion, these differences could be explained by methodologic differences between the studies (using radioimmunoprecipitation, ELISA with peptides, or fixed CBAs might have exposed intracellular epitopes, whereas our assay only detects antibodies to extracellular epitopes). Methodologic differences have proven to be a constant problem in this field for decades. For example, there is now clear evidence that antibodies to the myelin oligodendrocyte glycoprotein are specific for a subset of demyelinating diseases only if appropriate CBAs are used (these antibodies are detected at similar frequencies in patients and controls using ELISA).1 Similarly, although numerous studies confirm the importance of AQP4 antibodies as diagnostic biomarkers for NMOSD, the seropositivity rates are influenced by the assays used, and some methods, such as ELISA or immunoblotting, also detect these antibodies in controls.1 A possible limitation of our AQP1 assay is the use of HEK293A cells, because astrocytic AQP1 might be expressed in a complex against which the immune system could react.
However, the absence of AQP1 antibodies in NMOSD and controls fits very well with AQP1's role in hematology. AQP1, also known as channel-forming integral protein, is well-known in transfusion medicine because it contains the Colton blood group antigen expressed on erythrocytes. Anti-Colton antibodies are very rare and lead to significant delayed or acute transfusion reactions or hemolytic disease,7 a clinical phenotype absent in NMOSD. To conclude, our study failed to confirm the presence of AQP1 antibodies in NMOSD.
Supplementary Material
Acknowledgments
Acknowledgment: The authors are grateful to the Austrian NMO study group for contributing to this work.
Footnotes
Supplemental data at Neurology.org/nn
Author contributions: K.S., P.W., and M.R. conceived and designed the experiments. K.S., H.H., and M.R. performed the experiments. K.S., P.W., T.B. and M.R. analyzed the data. P.W., F.A.-D., M.I.L., J.P., S.V., R.M., and M.R. contributed reagents/materials/analysis. K.S., P.W., and M.R. wrote the manuscript.
Study funding: This study was funded by the Eugene Devic European Network (EDEN) project (ERA–Net ERARE 2: http://www.erare.eu/financed–projects/eden; Austrian Science Fund FWF project I916). P.W., M.I.L., and J.P. are funded by the NHS National Specialised Services for Neuromyelitis optica and the NIHR Oxford Biomedical Research Centre.
Disclosure: K. Schanda reports no disclosures. P. Waters received speaker honoraria from Biogen Idec Japan and Euroimmun AG, is a review editor for Frontiers in Molecular Innate Immunity, and holds a patent for and receives royalties from assays for the detection of antibodies to lgi1, Caspr2, Tag-1, and GABAAR. H. Holzer and F. Aboulenein-Djamshidian report no disclosures. M.I. Leite received travel grants and/or speaker honoraria from Biogen Idec and Novartis, is supported by NHS National Specialised Commissioning Group for Neuromyelitis Optica and NIHR Oxford Biomedical Research Centre, and is on the editorial board for Neuromuscular Disorders. J. Palace is on the scientific advisory boards for Merck Serono, Bayer Schering, Biogen Idec, Teva, Novartis, Sanofi-Aventis, and Alexion; received travel funding and/or speaker honoraria from Merck Serono, Novartis, Biogen Idec, Bayer Schering, and Medimmune; has consulted for Ono Pharmaceuticals, Chugai, CI Consulting, Biogen Idec, GlaxoSmithKline, and Alexion; is on the speakers' bureau for Teva and CMSC; received research support from Bayer Schering, Merck Serono, Novartis, Teva, Department of Health Risk Sharing Scheme, Department of Health, MS Society, Guthy Jackson Foundation, and ISIS Innovation Limited, a wholly owned subsidiary of the University of Oxford; and has filed a patent application to protect for the use of metabolomics as a method to diagnose and stage disease in multiple sclerosis. S. Vukusic is on the scientific advisory board for Biogen Idec, Genzyme, Merck Serono, Novartis Pharma, Sanofi-Aventis, and Teva; received travel funding and/or speaker honoraria from Biogen Idec, Genzyme, Merck Serono, Novartis, Sanofi, and Teva; has consulted for Merck Serono, Sanofi-Aventis, Teva, Biogen Idec, Genzyme, and Novartis; and received research support from Bayer Schering, Biogen Idec, Genzyme, Merck Serono, Novartis, Sanofi-Aventis, and Teva. R. Marignier served on the scientific advisory board for Medimmune. T. Berger reports no disclosures. M. Reindl is an academic editor for PLoS ONE; is on the editorial board for Current Medicinal Chemistry and Autoimmune Diseases; received research support from Eugene Devic European Network and Austrian Science Fund FWF; and The University Hospital and Medical University of Innsbruck (Austria, Markus Reindl) receive payments for antibody assays (NMDAR, AQP4, and other autoantibodies) and for AQP4 antibody validation experiments organized by Euroimmun. Go to Neurology.org/nn for full disclosure forms. The Article Processing Charge was paid by the Austrian Science Funds (project I916, Erare EDEN).
References
- 1.Berger T, Reindl M. Antibody biomarkers in CNS demyelinating diseases—a long and winding road. Eur J Neurol 2015;22:1162–1168. [DOI] [PubMed] [Google Scholar]
- 2.Misu T, Hoftberger R, Fujihara K, et al. Presence of six different lesion types suggests diverse mechanisms of tissue injury in neuromyelitis optica. Acta Neuropathol 2013;125:815–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tzartos JS, Stergiou C, Kilidireas K, Zisimopoulou P, Thomaidis T, Tzartos SJ. Anti-aquaporin-1 autoantibodies in patients with neuromyelitis optica spectrum disorders. PLoS One 2013;8:e74773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Long Y, Zheng Y, Shan F, et al. Development of a cell-based assay for the detection of anti-aquaporin 1 antibodies in neuromyelitis optica spectrum disorders. J Neuroimmunol 2014;273:103–110. [DOI] [PubMed] [Google Scholar]
- 5.Tüzün E, Tzartos J, Ekizoğlu E, et al. Aquaporin-1 antibody in neuromyelitis optical patients. Eur Neurol 2014;72:271–272. [DOI] [PubMed] [Google Scholar]
- 6.Mader S, Lutterotti A, Di Pauli F, et al. Patterns of antibody binding to aquaporin-4 isoforms in neuromyelitis optica. PLoS One 2010;5:e10455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halverson GR, Peyrard T. A review of the Colton blood group system. Immunohematology 2010;26:22–26. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


