Abstract
Professions grapple with defining advanced practice and the characteristics of advanced practitioners. In nursing and allied health, advanced practice has been defined as ‘a state of professional maturity in which the individual demonstrates a level of integrated knowledge, skill and competence that challenges the accepted boundaries of practice and pioneers new developments in health care’. Evolution of advanced practice in Australia has been slower than in the United Kingdom, mainly due to differences in demography, the health system and industrial relations. This article describes a conceptual model of advanced practitioner characteristics in the medical radiation professions, taking into account experiences in other countries and professions. Using the CanMEDS framework, the model includes foundation characteristics of communication, collaboration and professionalism, which are fundamental to advanced clinical practice. Gateway characteristics are: clinical expertise, with high level competency in a particular area of clinical practice; scholarship and teaching, including a masters qualification and knowledge dissemination through educating others; and evidence-based practice, with judgements made on the basis of research findings, including research by the advanced practitioner. The pinnacle of advanced practice is clinical leadership, where the practitioner has a central role in the health care team, with the capacity to influence decision making and advocate for others, including patients. The proposed conceptual model is robust yet adaptable in defining generic characteristics of advanced practitioners, no matter their clinical specialty. The advanced practice roles that evolve to meet future health service demand must focus on the needs of patients, local populations and communities.
Keywords: Advanced practice, conceptual model, diagnostic, radiography, radiation therapy
Introduction
The challenge of defining ‘advanced practice’ and differentiating between standard and advanced clinical practice is not new. Over the past two decades the medical radiation professions in Australia have grappled with this challenge, with several reports produced.1–3 Recent evidence suggests that the concept of advanced practice and related concepts have also confounded those in other disciplines, such as nursing.4,5 For example, Stasa et al.5 concluded that confusion could be reduced by minimising the use of terms such as ‘expanded’ and ‘extended’ practice, opting instead for a clear definition of ‘advanced practice’. They suggested that advanced practice nursing refers to ‘a level of nursing practice that uses extended and expanded skills’. In other words, extended and expanded practice are what advanced practitioners do, rather than being separate, though related concepts.
Much of the impetus for developing advanced practice roles in Australia has come from recognition of the need for additional clinical skills, beyond those of the standard, accredited and registered practitioner, and the blurring of traditional role boundaries in the face of technological advances.2 Meanwhile, changes have taken place in the United Kingdom (UK) over recent decades, with advanced and consultant practitioners now being legitimised occupational roles for diagnostic radiographers and radiation therapists.6,7 Those roles are recognised and valued in the health care system by government authorities, as well as by the professions.8 However, in spite of efforts made by the profession in Australia, it can be argued that little progress has been made in establishing a universal, sustainable and nationally transferable model of advanced practice in the Australian medical radiation workforce. In 2014, progress was made by introducing ‘advanced practice’ accreditation in the Australian Institute of Radiography (AIR), but there remains a disconnect between that achievement and the larger scale cultural change necessary to establish a widely recognised and clearly defined role for advanced practitioners in Australia.
Advanced practice has developed more rapidly in the UK compared with Australia because of several key differences. Although others have suggested a wide range of factors,9 the principal reasons are:
Demographic differences, with Australia having a higher ratio of radiologists and oncologists to population compared with the UK.10,11 In the UK, the shortage of specialist medical workforce has been a major driver of change, together with health care reform policy changes in the late 1990s and early 2000s aimed at creating a more equitable and patient-focused health care system.12
In Australia, there is much greater privatisation of health care, which has the influence of restricting the transferability of roles and delegation of tasks across professional boundaries between the medical and non-medical members of the medical radiation team. To date there are no accepted practice models in either the private or public sectors that permit radiologists to delegate tasks to radiographers, such as plain radiographic image reporting.9 However, private practice need not be an impermeable barrier to radiographer role development, with the radiologist assistant role in the United States having developed in a privatised health care system.13
The UK Society and College of Radiographers has a significant industrial relations role (http://www.sor.org/about-us/who-we-are), which enables them to negotiate with employers and to set practice standards, policies and conditions of employment. In Australia there is a separation between professional and industrial responsibilities, with the latter resting with the trade unions in the public health care system and, in the private system, dependent on negotiated enterprise bargaining agreements.
Proposing a model of advanced practice in the nursing and the allied health professions, McGee and Castledine14 put forward the following definition: ‘a state of professional maturity in which the individual demonstrates a level of integrated knowledge, skill and competence that challenges the accepted boundaries of practice and pioneers new developments in health care’.14 They described a concentric model, with the role of providing direct care to individuals or groups as the central element, which they claim to be an essential criterion for all advanced practice. The next concentric layer is professional maturity, which includes the elements of mastery of clinical practice and interpersonal skills, the latter being characterised by an inherent focus on the needs of patients. The next layer is challenging professional boundaries. They claim, as have others,15–17 that the hierarchical model of health care where decision making is vested in an all-knowing medical practitioner is becoming increasingly less feasible. Technological change together with an ageing patient population with complex co-morbidities means that collaborative, interprofessional practice, where decision-making and responsibility are shared between highly knowledgeable and skilled team members is a much more viable practice model.18 The outer layer of the model is pioneering innovations, with key aspects being leadership and ethical, evidence-based decision making, supported by scholarly activity, critical reflection and research.
This sort of modelling is useful in helping professions, individual advanced practitioner aspirants, health care administrators and others outside the professions understand the generic qualities of advanced practitioners and to appreciate the full potential of their roles. From this perspective, this article aims to outline a conceptual model for advanced practitioner characteristics, as opposed to advanced practice per se, in the Australian medical radiation professions, taking into account the experiences in other countries and other professions, as well as many years of consultation with various stakeholders in Australia and overseas.
Characteristics of Advanced Practitioners
Figure1 is a diagram of a conceptual model developed by the Advanced Practitioners Advisory Panel (APAP) of the AIR. While informed by a variety of sources, it has strong foundations in the CanMEDS framework developed by the Societal Needs Working Group of the Royal College of Physicians and Surgeons of Canada.19 CanMEDS is a competency-based framework originally created to inform the educational curricula for specialist medical practitioners but it has been adapted to other health professions20,21 and to interprofessional education and practice.22 Table 1 lists some suggestions as to the competencies expected of advanced practitioners against each of the characteristics shown in Figure1 and gives examples of the types of evidence and evaluation criteria that might support elevation to advanced practitioner status for a diagnostic radiographer, sonographer or radiation therapist.
Figure 1.
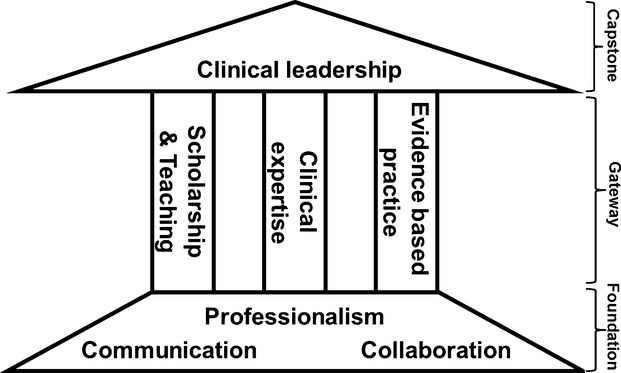
A conceptual model of advanced practice relevant to the medical radiation professions.
Table 1.
Examples of key competencies and evaluation criteria for advanced practitioners
| Characteristics | Competencies | Evaluation and evidence |
|---|---|---|
| Foundation | ||
| Communication | • Establishes supportive relationships with patients and carers | • Peer review and performance appraisal |
| • Elicits and uses relevant information | • Patient testimonials | |
| • Empathises with patients, regardless of their background | • Professional portfolio | |
| • Discusses and provides appropriate information with/to patients, carers and other health care providers | ||
| Collaboration | • Shares knowledge and information with other members of the health care team | • Peer review and performance appraisal |
| • Participates in interprofessional activities and contributes to the overall effectiveness of the team | • Professional portfolio | |
| Professionalism | • Delivers optimum quality care | • Peer review and performance appraisal |
| • Displays integrity, honesty and compassion | • Professional portfolio | |
| • Acts according to social, legal and ethical codes of conduct | • Professional memberships and affiliations | |
| • Engages in professional activities and behaviours | ||
| Gateway | ||
| Clinical expertise | • High level clinical skills to effectively and ethically manage the care of patients within relevant scope of practice | • Position description |
| • Gathers, synthesises and applies relevant clinical data and information | • Peer review and performance appraisal | |
| • Effectively manages complexity | • Professional portfolio | |
| • Recognises boundaries and limitations | ||
| • Effective clinical consultation skills | ||
| Scholarship and teaching | • High level academic knowledge and skills | • Academic award(s) |
| • Participates and records continuing professional development (CPD) | • CPD record | |
| • Facilitates learning of patients, students, colleagues and other health professionals | • Teaching portfolio | |
| • Participant evaluation of teaching | ||
| Evidence based practice | • Understands and can articulate research design and methodology | • Research track record |
| • Applies the principles of critical appraisal of research literature | • Conference presentations | |
| • Translates new knowledge into practice | • Peer-reviewed publications | |
| Capstone | ||
| Clinical leadership | • Accepts responsibility for personal and team performance | • Peer review and performance appraisal |
| • Advocates for the health and wellbeing of patients and the community | • Community service portfolio | |
| • Mentors and advocates for colleagues | • Board/committee representation | |
| • Participates in and influences strategic planning and development | ||
Foundation characteristics
An accredited and registered practitioner who aspires to become an advanced practitioner is required to demonstrate foundation characteristics at a higher level of performance than standard accredited practitioners. They would be expected to be performing at the pinnacle of accredited practitioner status to be considered for promotion to advanced practitioner status. These foundation characteristics form the base of the model in Figure1 and are described below.
Communication
Communication skills are essential for all radiographers, radiation therapists and sonographers in order to provide humane, high-quality patient care and to work effectively with other members of the health care team. However, advanced practitioners need high-level written and verbal communication skills, taking a lead role in obtaining information from, and conveying information to colleagues, patients and their carers. In doing so, they need to respond appropriately to patients' beliefs, concerns and expectations and reliably assess factors impacting on patients' health and well-being, conveying this to other members of the team, as necessary. An advanced practitioner fosters patient compliance and gains their confidence, resulting in high levels of satisfaction with care. Their patient care would typically portray understanding, trust, respect, empathy and confidentiality, no matter the age, gender, ethnicity or cultural and socioeconomic background of the patient. They would model this behaviour to others.
A key requirement is the ability to give instructions and communicate complex concepts, such as diagnostic information or treatment side effects, whether to patients with limited understanding or to medical specialists. Advanced practitioners would be expected to use appropriate terminology and communication strategies accordingly. In dealing with other members of the health care team they would communicate effectively, demonstrate respect and take responsibility for outcomes, even in stressful situations. They would also be capable if called upon to address the general public or the media.
Collaboration
High level collaborative skills, beyond those expected of most practitioners, are essential for advanced practitioners in order to work in partnership and to guide other members of the team. This may be in the context of providing appropriate care to individual patients, providing education to groups of patients or the general community, or when providing information and gaining consent for research. They will understand the limitations of their own role and recognise and value the expertise of other members of the multidisciplinary team, delegating tasks as necessary. In addition, they will be able to communicate knowledgeably and honestly, with firm intent, while being respectful of the rights and opinions of others. They would reflect on and reliably assess situations, giving and receiving feedback on the performance and, where necessary, providing support and conflict resolution within the team. While their focus would be team oriented in the clinical context, they would possess an awareness of local, state or national governance and organisational responsibilities and thus be capable of liaising with stakeholders within those realms.
Professionalism
Professionalism does not automatically come with the award of a testamur from a university or with a professional registration certificate; it is developed over time and to varying degrees by individuals who might claim the title of ‘a professional’. It is a complex and highly valued quality. Professions have been described as occupations that possess a distinct body of knowledge, skills and attitudes that they apply in altruistic service of the paramount problems of human existence – disease, injustice, sin and death.23 The definition of ‘a profession’ has broadened over time to include more occupations, including allied health professions,24 and even in medicine there has been a renewed interest in defining and promoting the concept of professionalism.25
All professionals should be committed to the highest achievable standards of clinical practice and ethical conduct, as well as to the continual pursuit of excellence in their discipline. The advanced practitioner will have demonstrably high standards of integrity, honesty and compassion, unbiased by racial, cultural, religious or societal differences. Importantly, they will be responsible and accountable for their own personal and professional behaviour; however they will also assume responsibility for the behaviour of others. This requires awareness, knowledge of content and observance of legal and ethical codes of practice and, consequently, avoidance of unprofessional behaviour. While this is the case for all practitioners, because the advanced practitioner performs higher level clinical duties and tasks they naturally carry greater professional responsibility.
Gateway characteristics
To make the transition from a registered practitioner to an advanced practitioner, the individual is expected to acquire and be able to demonstrate specific knowledge, skills and abilities that take them above and beyond the foundation level. These gateway characteristics form the central part of the model in Figure1.
Clinical expertise
The provision of direct clinical care to patients is an essential part of advanced practice, as in McGee and Castledine's model.14 Therefore, possession of expert clinical knowledge and skills in an area of practice traditionally performed by another health profession is shown in Figure1 as the central pillar of the model. It is not the purpose of this article to identify specific areas of clinical expertise, as these may vary depending on local need, but to describe this characteristic generically. Thus, while the specific, clinically relevant knowledge, skills and abilities depend on the particular role of the advanced practitioner, the generic competencies include:
the ability to elicit a relevant, concise and accurate clinical and social history from patients;
knowledge and skills to search for and critically appraise evidence to optimise patient outcomes;
possession of highly developed technical, practical and procedural clinical skills;
capacity to manage complex clinical issues and situations; and
insight into their own ability through self-evaluation and reflection.
Again, because of their higher level duties, advanced practitioners would be expected to demonstrate these competencies at a commensurately higher level. Within the scope of their specific field of clinical practice they make appropriate clinical decisions and provide services accurately, ethically and cost-effectively. In fact, the characteristic of clinical expert naturally intersects with all of the other characteristics in the model, as the advanced practitioner takes into account the needs of patients and works collaboratively with other health professionals.
Scholarship and teaching
Advanced practitioners would be expected to hold a higher qualification than required for entry into the profession. The Interprofessional Advisory Team (IPAT) report recommended that they would have to attain a masters degree ‘incorporating coursework in core competencies in advanced practice, a research thesis of no less than 25,000 words and supervised and examined advanced clinical work, facilitated by the practitioner's workplace and oversighted by a supervisor’.3 According to the Australian Qualifications Framework (AQF) (http://www.aqf.edu.au), masters degree (AQF Level 9) graduates ‘will apply knowledge and skills to demonstrate autonomy, expert judgement, adaptability and responsibility’, which seems appropriate to advanced practitioners. In addition, the advanced practitioner would need to engage in lifelong learning, evidenced through a program of continuing professional development (CPD). They would be expected to gain more CPD points within a triennium than other practitioners (APWG 2009), with this learning focused particularly on their field of expert practice.
Dissemination of knowledge through education would also be a core role of advanced practitioners. This would involve facilitating the learning of others, including patients, students, colleagues and junior practitioners, as well as members of neighbouring health professions. They would help others define their learning needs and provide critical, scholarly feedback and advice, with knowledge of adult learning principles.
Evidence-based practice
Evidence-based practice (EBP) is about ‘the conscientious, explicit and judicious use of current best evidence’ in clinical decision making, integrated with the clinical expertise of the practitioner and the patient's preferences and choices.26 Contrary to common beliefs, EBP is not practiced only by academics ‘from ivory towers and arm chairs’.26 It is intended to be a ground-up paradigm; a particular way of thinking and practicing in which up-to-date knowledge of valid and reliable research is fundamental in making informed judgements about patients’ care.
Because their role is primarily clinically oriented, an advanced practitioner might not necessarily be directly involved research themselves. They would, however, be expected to have a sound understanding of research principles and be capable of interpreting and applying research findings. In that context, they would understand how to write a research question and hypothesis, as well as design a study to answer that question. Most important in accordance with the evidence-based practise paradigm,27 would be the ability to critically appraise research and use valid and reliable results to inform their clinical practice and that of others. Advanced practitioners would promote a research culture within the clinical environment in which they work and encourage other practitioners to engage in EBP and research training.
It would also be an expectation that advanced practitioners would regularly author or co-author journal articles and conference papers, as a means of disseminating best practice in their field. They may also be on the editorial board or peer-review panel of professional or scientific journals and on conference organising committees.
Capstone characteristic
An accredited and registered practitioner who demonstrates high-level foundation characteristics and has, through both clinical experience and sustained academic effort, acquired gateway characteristics in a particular field of medical radiation practice, may be considered to have attained the status of an advanced practitioner. As a consequence, it would be expected that they would possess the characteristics that would make them a leader in the clinical field in which they work.
Clinical leadership
This characteristic should be considered the pinnacle of achievement in advanced practice. The advanced practitioner would have the ability to influence and manage change and would provide a sense of stability and certainty within a team, providing expert guidance and advice and engaging in knowledge translation.4 The clinical leader advocates for their colleagues, as well as for consumers at the level of individual patients, the relevant practice population and the broader community.28 They would, in the context of their higher level clinical duties and responsibilities, have an awareness of the determinants of health and disease. As is appropriate for health professionals generally, they would incorporate this knowledge into their clinical practice by promoting healthy behaviour, understanding patients' needs and encouraging patient participation in clinical decision-making.
Health professional leaders have the capacity to influence the environment in which health care is delivered, as well as how it is delivered. From this perspective, although not managers in an administrative sense, they need to have an important role in influencing policy debate and management decisions.28 This may take place through attending meetings with health administrators or participating in discussions about allocation of health care resources. Thus, awareness would be necessary of external influences on health services and the importance of patient-focussed, cost-effective, safe and high-quality health care. It would be expected that they would promote and actively participate in quality improvement processes and strategic planning and would also monitor and reflect on their own clinical performance and that of their clinical team.
Discussion
Others have also attempted to define the key concepts of advanced practice in radiography,29,30 as well as in nursing.31,32 For the most part, there is agreement with the concepts included in the model described in this article. In reflecting on the need for an international perspective on advanced radiographic practice, Hardy et al.30 concluded that certain commonalities exist, such as the central role of education and mentorship, and the need for processes that required critical thinking, research and evaluation of performance.
In another article, Snaith and Hardy29 listed eight elements of advanced practice in addressing the question of how to become an advanced practitioner, many of which overlap with those in this article. They included, for example, ‘expert practice’, ‘education and training’, ‘research’ and ‘leadership’ but did not include some of the characteristics derived from the CanMEDS framework, such as ‘communication’, ‘collaboration’ and ‘professionalism’. It could perhaps be argued that these foundation characteristics, as described in this article, should be inherent in all accredited and registered practitioners and thus have no place in the advanced practice model. However, the counter-argument is that they are so essential to the higher level role, duties and responsibilities of the advanced practitioner that they cannot be assumed and must be included in any conceptual model of advanced practice. In other advanced practice models, such as that of McGee and Castledine,14 such foundation characteristics are embedded; however, there is value in making them explicit and, thus, demonstrable and assessable by means such as those suggested in Table 1.
Similar debate may be had about the inclusion of the concept of EBP in the gateway characteristics. Even new graduates are expected to have knowledge of EBP; however, it requires a degree of professional maturity to implement EBP and to create a research-oriented practice culture within the clinical environment. At times this necessitates challenging the status quo and traditional practices that may be lacking in valid evidence. Consequently, it would be expected that advanced practitioners would be clinical leaders in this, as in other regards by incorporating research into their own practice and role modelling it to others. As explained previously, this does not necessarily require advanced practitioners to become full-time researchers, although some may collaborate to implement research projects to investigate particular clinical questions that arise. It does, however, require that they possess research skills that can be applied as necessary, particularly in interpreting research literature and determining if that research uses valid methodologies and whether it is reliable enough to be generalisable to the context of local clinical practice. It may be, for example, that the advanced practitioner meets the expectations in this characteristic by taking a lead role in a weekly journal club that examines clinically relevant recently published articles.
Conceptual modelling is a useful way to define professional practice. The CanMEDS model on which much of the work described in this paper was based is broadly accepted and robust, having survived several iterations. A series III CanMEDS 2015 physician competency framework is available.33 While the essential elements are the same, it uses simpler, more direct language, minimises overlap between role descriptions and places greater emphasis on demonstrable capabilities, as opposed to more abstract aspects of roles. Simple editing is all that is required to make it relevant to diagnostic imaging and radiation therapy practice, even at new graduate, entry level into the profession.
The lesson that can be learned from this is that such conceptual models can be and should be flexible and adaptable over time, as well as across professions. They should not be rigidly confined by the uniqueness of temporal, geographical or occupational boundaries. Indeed, the advanced practice model described in this paper is intended to address generic characteristics, without being prescriptive or specific to particular roles that might be performed by advanced practitioners. The advantage is that the same characteristics apply no matter whether the specific advanced practice role is emergency department image interpretation and reporting, or clinical specialisation in breast radiation therapy. To some extent this may also be viewed as a limitation, in that it still requires clinical sites to develop advanced practitioner position descriptions that fill the gaps in local service availability and needs.
Conclusions
Whether the medical radiation professions as whole were to adopt this or another model of advanced practice, the real challenge is to modernise the way that medical radiation services are provided in future. The current practice models used for the delivery of medical radiation services in the health care system are not sustainable in the face of projected increasing demand and a per capita reduction in the size of health care workforce.
However, advanced practice is not just about what the profession wants but about what the patient population needs. Therefore, it is essential that there is a clear focus on need in relation to the development of advanced practice roles and that the scope of practice of those who achieve advanced practice status in the future is oriented towards meeting the needs of the patients and the community they serve. Consequently, there is still a lot of work to do in identifying the needs of specific patient populations, negotiating role boundaries with neighbouring occupations (principally radiologists and oncologists) and defining the educational needs of those within the medical radiation professions who wish to pursue an advanced practice, clinically oriented career path. As observed elsewhere,2 however, it should not be assumed that ‘one size fits all’ and that practice models developed overseas will necessarily be suitable to Australia with vastly different population size and distribution, as well as health care and tertiary education systems.
Acknowledgments
The authors acknowledge the past and present members of the APAP of the AIR who have contributed to the development of the model described in this paper. Without listing each of them, the advice and feedback received from AIR working parties, groups and panels, as well as other professional bodies and external organisations, is also acknowledged.
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Australian Institute of Radiography (AIR) Professional Advancement Working Party Report, April 2006 [cited 26 Nov 2014]. Available from: http://www.air.asn.au/cms_files/09_AdvancedPractice/1201_PAWP_Report_Final_April06.pdf.
- 2.Australian Institute of Radiography (AIR) Discussion paper: A model of advanced practice in diagnostic radiography and radiation therapy in Australia. Report of the Advanced Practice Working Group (APWG), May 2009 [Cited 26 Nov 2014]. Available from: http://www.air.asn.au/cms_files/09_AdvancedPractice/APWG_Final_Report_260609.pdf.
- 3.Freckelton I. Advanced practice in radiography and radiation therapy: Report from the Interprofessional Advisory Team, April 2012 [Cited 26 Nov 2014]. Available from: http://www.air.asn.au//cms_files/09_AdvancedPractice/ipat_final_report21april2012.pdf.
- 4.Hutchinson M, East L, Stasa H, Jackson D. Deriving consensus on the characteristics of advanced practice nursing. Nurs Res. 2014;62:116–28. doi: 10.1097/NNR.0000000000000021. [DOI] [PubMed] [Google Scholar]
- 5.Stasa H, Cashin A, Buckley T, Donoghue J. Advancing advanced practice. Nurs Edu Today. 2014;34:356–61. doi: 10.1016/j.nedt.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 6.Department of Health (UK) Radiography Skills Mix: A Report on the Four-Tier Service Delivery Model. London: Department of Health; 2003. [Google Scholar]
- 7.Society and College of Radiographers. Scope of Radiographic Practice Survey 2012. London: Society and College of Radiographers; 2012. [Google Scholar]
- 8.Royal College of Radiologists and Society and College of Radiographers. London: Royal College of Radiologists; 2012. Team Working in Clinical Imaging. [Google Scholar]
- 9.Page B, Bernoth M, Davidson R. Factors influencing the development and implementation of advanced radiographer practice in Australia: A qualitative study using an interpretation phenomenological approach. J Med Radiat Sci. 2014;61:142–50. doi: 10.1002/jmrs.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Munro PL, Bradshaw N, Stephenson N. 2012 RANZCR Radiology Workforce Census Report: Australia. Sydney: Royal Australian and New Zealand College of Radiologists; 2013. [Google Scholar]
- 11.Royal College of Radiologists. Clinical Radiology UK Workforce Report 2011. London: Royal College of Radiologists; 2012. [Google Scholar]
- 12.Hewison A. UK health policy and health service reform. In: McGee P, editor. Advanced Practice in Nursing and the Allied Health Professionals. 3rd edn. Oxford: Wiley-Blackwell; 2009. pp. 15–28. [Google Scholar]
- 13.American Registry of Radiologic Technologists. Radiologist Assistant Role Delineation, January 2005 [cited 28 Nov 2014]. Available from: http://www.acr.org/∼/media/ACR/Documents/PDF/QualitySafety/Resources/Radiologist%20Assistant/RoleDelineation.
- 14.McGee P, Castledine G. Advanced Practice. 2nd edn. Oxford: Blackwell Science; 2003. [Google Scholar]
- 15.McKinlay JB, Marceau LD. The end of the golden age of doctoring. J Health Serv. 2002;32:379–416. doi: 10.2190/JL1D-21BG-PK2N-J0KD. [DOI] [PubMed] [Google Scholar]
- 16.Nancarrow SA, Borthwick AM. Dynamic professional boundaries in the healthcare workforce. Soc Health Illness. 2005;27:897–919. doi: 10.1111/j.1467-9566.2005.00463.x. [DOI] [PubMed] [Google Scholar]
- 17.Allsop J. Medical dominance in a changing world: The UK case. Health Soc Rev. 2006;15:444–57. [Google Scholar]
- 18.Woznitza N, Piper K, Rowe S, West C. Optimizing patient care through team-working: As case study. Radiography. 2014;20:258–63. [Google Scholar]
- 19.Frank JR, Danoff D. The CanMEDS initiative: Implementing an outcomes-based framework for physician competencies. Med Teach. 2007;29:642–7. doi: 10.1080/01421590701746983. [DOI] [PubMed] [Google Scholar]
- 20.Verma S, Paterson M, Medves J. Core competencies for health care professionals: What medicine, nursing, occupational therapy and physiotherapy share. J Allied Health. 2006;35:109–15. [PubMed] [Google Scholar]
- 21.Verma S, Broers T, Paterson M, Schroder C, Medves J, Morrison C. Core competencies: The next generation: Comparison of a common framework for multiple professions. J Allied Health. 2009;38:47–53. [PubMed] [Google Scholar]
- 22.Canadian Interprofessional Health Collaborative (CIHC) A National Interprofessional Competency Framework. CIHC, Vancouver, February 2010 [cited 3 June 2012]. Available from: http://www.cihc.ca/files/CIHC_IPCompetencies_Feb1210.pdf.
- 23.Gieryn TF. Boundaries of science. In: Jasanoff S, Marble GE, Petersen JC, Pinch T, editors. Handbook of Science and Technology Studies. London: Sage; 1995. pp. 393–443. [Google Scholar]
- 24.Brown CA. The division of labour: Allied health professions. Int J Health Sci. 1973;3:435–44. doi: 10.2190/5U2G-3Q68-JKKC-VT13. [DOI] [PubMed] [Google Scholar]
- 25.Thistlethwaite J, Spencer J. Professionalism in Medicine. Oxford: Radcliffe Publishing; 2008. [Google Scholar]
- 26.Sackett D, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: What it is and what it isn't. BMJ. 1996;312:71. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Strauss SE, Sackett DL. Getting research findings into clinical practice: Using research in clinical practice. BMJ. 1998;317:339–42. doi: 10.1136/bmj.317.7154.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shaw S. Leadership in advanced practice: Challenging professional boundaries. In: McGee P, editor. Advanced Practice in Nursing and the Allied Health Professionals. 3rd edn. Oxford: Wiley-Blackwell; 2009. pp. 158–76. [Google Scholar]
- 29.Snaith B, Hardy M. How to achieve advanced practitioner status: A discussion paper. Radiography. 2007;13:142–6. [Google Scholar]
- 30.Hardy M, Legg J, Smith T, Ween B, Williams I, Motto J. The concept of advanced practice: An international perspective. Radiography. 2008;14(Suppl. 1):e15–19. [Google Scholar]
- 31.Mantzoukas S, Watkinson S. Review of advanced nursing practice: The international literature and developing generic features. J Clin Nur. 2006;16:28–37. doi: 10.1111/j.1365-2702.2006.01669.x. [DOI] [PubMed] [Google Scholar]
- 32.MacDonald JA, Herbert R, Thibeault C. Advanced practice nursing: Unification through a common identify. J Prof Nurs. 2006;22:172–9. doi: 10.1016/j.profnurs.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 33.Frank JR, Snell LS, Sherbino J, editors. Draft CanMEDS 2015 Physician Competency Framework – Series III. Ottawa: The Royal College of Physicians and Surgeons of Canada; 2014. [Google Scholar]


