Abstract
Cancer screening and surveillance programmes and the use of sophisticated imaging tools such as positron emission tomography-computed tomography (PET-CT) have increased the detection of impalpable lesions requiring imaging guidance for excision. A new technique involves intra-lesional insertion of a low-activity iodine-125 (125I) seed and detection of the radioactive signal in theatre using a hand-held gamma probe to guide surgery. Whilst several studies describe using this method to guide the removal of impalpable breast lesions, only a handful of publications report its use to guide excision of lesions outside the breast. We describe a case in which radio-guided occult lesion localisation using an iodine 125 seed was used to guide excision of an impalpable posterior chest wall metastasis detected on PET-CT.
Keywords: Radioactive seed localisation, radio-guided surgery, iodine-125, iodine seed localisation
Introduction
Methods to guide excision of impalpable lesions include hook-wire insertion (HWL), intra-operative ultrasound (IOUS) and radio-guided occult lesion localisation (ROLL) using the injection of 99mTc-labelled colloidal human serum albumin.1 A new technique, ROLL using 125I Seeds (ROLLIS) offers many advantages2 as illustrated in this report. Written permission was obtained from the patient to use their information for this publication.
Case Report
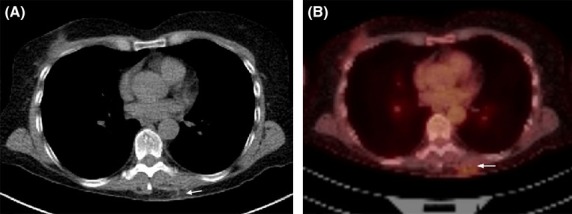
A surveillance F-18 fludeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) scan in a 59-year-old female with a history of metastatic melanoma showed intense uptake within a 3 × 4 mm subcutaneous nodule on the left posterior chest wall (Fig.1A and B). A previous history of excision of metastatic deposits elsewhere was noted. Clinical exam was normal. Ultrasound (US) showed an oval-shaped well defined hypoechoic vascular mass (Fig.2).
Figure 1.
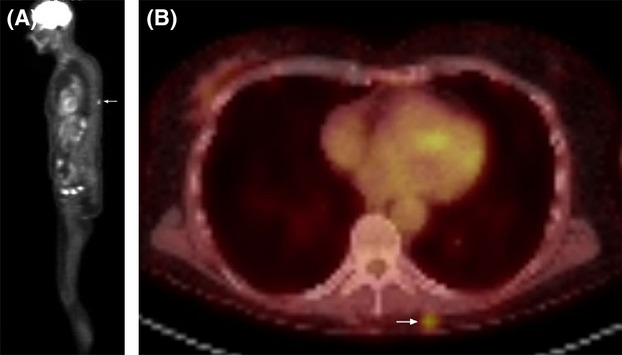
(A) and (B) Whole-body F-18 fludeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) scan shows focus of intense uptake in the left posterior chest wall (arrow).
Figure 2.
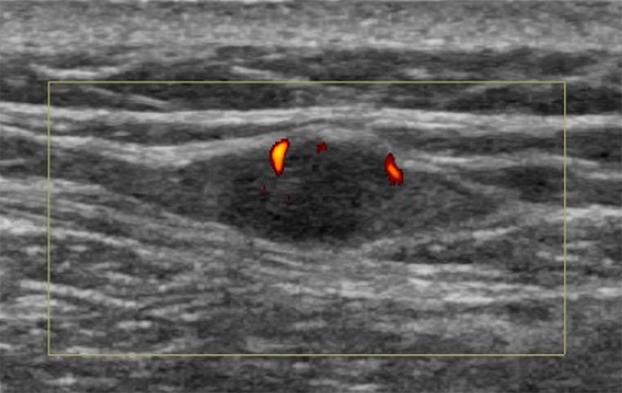
Ultrasound scan of the chest wall shows the hypoechoic lesion with vascularity.
On the morning of surgery an 125I seed (∼2 MBq) was inserted using US (Fig.3A, B and C). In theatre, the surgeon used a hand-held gamma probe, set to detect the energy from the 27 keV photon emitted by the 125I seed to locate and remove the lesion. Successful removal of seed and lesion was confirmed by absent radioactive counts in the wound, high counts within the specimen and visualisation of the lesion and seed on X-ray (Fig.4A). Following tissue fixation, a further grid specimen radiograph (Fig.4B) demonstrated lesion and seed co-ordinates for the pathologist. Histopathology showed a 6 mm melanoma deposit with negative tumour margins. A follow-up F-18 FDG PET/CT scan showed only faint uptake in the surgical bed consistent with post-operative change (Fig.5A and B).
Figure 3.
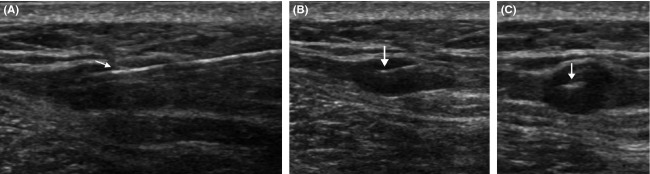
Ultrasound guided seed insertion (A) Long-axis view showing seed deployment needle (arrow) within a hypoechoic posterior chest wall mass corresponding to the lesion seen on the PET-CT study. (B) Long-axis and (C) short-axis views of the lesion taken immediately after seed deployment. The seed is seen as a linear echogenic structure (arrow).
Figure 4.
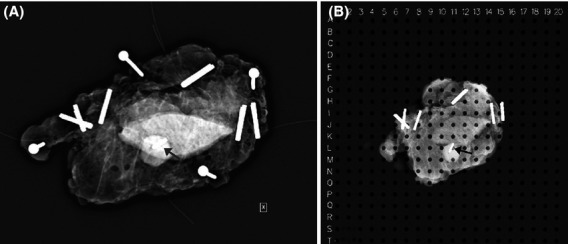
(A) Intra-operative specimen radiograph confirms excision of lesion with seed in situ (arrow). (B) X-ray of specimen in a grid following tissue fixation in formalin shows the co-ordinates for the lesion and 125I Seed (arrow).
Figure 5.
Post-operative (A) CT and (B) F-18 fludeoxyglucose positron emission tomography/computed tomography (FDG PET/CT) images taken at the same slice position. The previous focus of intense tracer uptake is no longer seen. There is minimal uptake in the surgical bed consistent with post-operative change (arrow).
Discussion
In parallel with the increasing detection of impalpable breast lesions with screening mammography, the development and increasing use of sophisticated imaging techniques (such as F-18 FDG PET/CT) has led to earlier detection of small lesions in other parts of the body, some of which require pre-operative image-guided localisation for excision. Various methods of doing this have been described, including the use of HWL of pulmonary nodules, musculoskeletal, retroperitoneal and liver lesions3–6 and ROLL to mark recurrent renal cell carcinoma, papillary carcinoma of the thyroid, retroperitoneal sarcoma, lesions of the popliteal fossa and recurrent thigh rhabdomyosarcoma.7
In general, HWL is the most commonly used technique but has been associated with complications including movement of the wire after insertion and wire transection during surgery.8 Because the wire extends outside the skin, the localisation procedure must be performed on the day of surgery. This makes the surgical and radiology lists interdependent with delays or cancellations in either department inevitably reducing efficient use of resources. For lesions in difficult locations (such as in our patient) the presence of a hook-wire may also be physically awkward and uncomfortable.
Intra-operative ultrasound is being increasingly used by surgeons to guide lesion removal. The great advantages are that this eliminates the need for a separate pre-operative localisation procedure, does not expose the patient or staff to ionising radiation and gives real-time three-dimensional feedback during surgery. However, to use IOUS the lesion must be sonographically visible and US equipment and a suitably trained surgeon available.
Radio-guided techniques such as ROLL have been effectively used for breast and non-breast lesions.7,9 As with the use of hook-wires, however, the insertion procedure must be performed within 24 h of surgery due to the short half-life of 99mTc (6 h). The inherently non-radio-opaque nature of 99mTc labelled colloids also means that confirming accuracy of placement of the injection is difficult unless a contrast agent or marker clip is also used.10
125I seeds are radiopaque 4.5 × 0.8 mm titanium cylinders containing approximately 2 MBq of iodine-125 adsorbed onto a silver wire. Because they are solid and radiopaque, accuracy of placement can easily be confirmed using US, X-ray or CT. Experience with ROLLIS to localise impalpable breast lesions has shown that 125I seeds rarely migrate.11 The seed acts as a point source of radio-activity, giving precise real-time feedback as to the location of the lesion in three dimensions.12 All of this helps to make surgery easier.
125I has a physical half-life of 60.14 days, which means the seed can be inserted several days (and in the case of patients undergoing neoadjuvant chemotherapy many months)13 before surgery. This has been shown to improve the utilisation of radiology resources,14 theatre lists,15 and patient convenience.16 The radiation exposure to patient, family and staff from the use of 125I seeds is minimal17 however the seed is a regulated sealed source of radioactivity, therefore its whereabouts must always be tracked. To minimise the risk of seed loss, good multidisciplinary communication and a seed handling protocol are essential.
Whilst there are meta-analyses evaluating the use of 125I seeds to localise breast lesions,2,18 there are only a few reports describing the use of this technique outside the breast. Fleming et al.19 used ROLLIS to localise a cluster of in-transit melanoma nodules in the lower leg of a 73-year-old man and Grotz et al.20 used it in eight patients; two with in-transit melanoma metastases. Straver et al.21 used seeds to mark malignant axillary nodes prior to neoadjuvant chemotherapy, and Jackson et al.22 to localise a PET-positive node in a patient with an unknown primary. The use of 125I seeds to guide excision of pulmonary nodules has also been trialled.23
In conclusion, this case report provides another example of the successful use of ROLLIS as a relatively simple and accurate method to guide the excision of an impalpable lesion, other than in the management of breast cancer.
Acknowledgments
Dr Taylor is currently supported by a Sylvia and Harold Rowell Clinician Research Fellowship from the Medical Research Foundation of Royal Perth Hospital. We thank Ms Barbara Taylor for assistance with manuscript preparation. The use 125I seeds for lesion localisation in Australia currently requires TGA approval via the Special Access Scheme or within the confines of an Ethics Committee approved clinical trial.
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Dua SM, Gray RJ, Keshtgar M. Strategies for localisation of impalpable breast lesions. Breast. 2011;20:246–53. doi: 10.1016/j.breast.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 2.Ahmed M, Douek M. Radioactive seed localisation (RSL) in the treatment of non-palpable breast cancers: systematic review and meta-analysis. Breast. 2013;22:383–8. doi: 10.1016/j.breast.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 3.Morrison WB, Sanders TG, Parsons TW, Penrod BJ. Preoperative CT-guided hookwire needle localization of musculoskeletal lesions. Am J Roentgenol. 2001;176:1531–3. doi: 10.2214/ajr.176.6.1761531. [DOI] [PubMed] [Google Scholar]
- 4.Kagalwala DZ, Shankar S, Zota V, Sandor A, Litwin DE. Preoperative computed tomography-guided hookwire needle localization of a peritoneal multilocular inclusion cyst. J Comput Assist Tomogr. 2005;29:602–3. doi: 10.1097/01.rct.0000174377.56134.8b. [DOI] [PubMed] [Google Scholar]
- 5.Sato M, Watanabe Y, Tokui K, et al. Laparoscopic hepatic surgery guided by hookwire localization. Surg Endosc. 2000;14 doi: 10.1007/s004649901206. 296. [DOI] [PubMed] [Google Scholar]
- 6.Mullan BF, Stanford W, Barnhart W, Galvin JR. Lung Nodules: improved Wire for CT-guided Localization 1. Radiology. 1999;211:561–5. doi: 10.1148/radiology.211.2.r99ma35561. [DOI] [PubMed] [Google Scholar]
- 7.Bitencourt AGV, Lima ENP, Pinto PNV, Martins EBL, Chojniak R. New applications of radioguided surgery in oncology. Clinics. 2009;64:397–402. doi: 10.1590/S1807-59322009000500005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bronstein AD, Kilcoyne RF, Moe RE. Complications of needle localization of foreign bodies and nonpalpable breast lesions. Arch Surg. 1988;123:775–9. doi: 10.1001/archsurg.1988.01400300121022. [DOI] [PubMed] [Google Scholar]
- 9.Sajid MS, Parampalli U, Haider Z, Bonomi R. Comparison of radioguided occult lesion localization (ROLL) and wire localization for non-palpable breast cancers: a meta-analysis. J Surg Oncol. 2012;105:852–8. doi: 10.1002/jso.23016. [DOI] [PubMed] [Google Scholar]
- 10.Landman J, Taylor D, McCarthy M, Troedson R. 2012. Is 99mTc MAA a suitable radiopharmaceutical for radioguided localisation of impalpable breast prior to surgical excision? Australian and New Zealand Society of Nuclear Medicine 42nd Annual Scientific Meeting, Melbourne.
- 11.Alderliesten T, Loo CE, Pengel KE, Rutgers EJ, Gilhuijs KG, Vrancken Peeters MJ. Radioactive seed localization of breast lesions: an adequate localization method without seed migration. Breast J. 2011;17:594–601. doi: 10.1111/j.1524-4741.2011.01155.x. [DOI] [PubMed] [Google Scholar]
- 12.Jakub JW, Gray RJ, Degnim AC, Boughey JC, Gardner M, Cox CE. Current status of radioactive seed for localization of non palpable breast lesions. Am J Surg. 2010;199:522–8. doi: 10.1016/j.amjsurg.2009.05.019. [DOI] [PubMed] [Google Scholar]
- 13.van Riet YE, Maaskant AJ, Creemers GJ, et al. Identification of residual breast tumour localization after neo-adjuvant chemotherapy using a radioactive 125 Iodine seed. Eur J Surg Oncol. 2010;36:164–9. doi: 10.1016/j.ejso.2009.10.009. [DOI] [PubMed] [Google Scholar]
- 14.Sharek D, Zuley ML, Zhang JY, Soran A, Ahrendt GM, Ganott MA. Radioactive seed localization versus wire localization for lumpectomies: a comparison of outcomes. Am J Roentgenol. 2015;204:872–7. doi: 10.2214/AJR.14.12743. [DOI] [PubMed] [Google Scholar]
- 15.Dauer LT, Thornton C, Miodownik D, et al. Radioactive seed localization with 125I for nonpalpable lesions prior to breast lumpectomy and/or excisional biopsy: methodology, safety, and experience of initial year. Health Phys. 2013;105:356–65. doi: 10.1097/HP.0b013e31829c03e1. [DOI] [PubMed] [Google Scholar]
- 16.Gray RJ, Pockaj BA, Karstaedt PJ, Roarke MC. Radioactive seed localization of nonpalpable breast lesions is better than wire localization. Am J Surg. 2004;188:377–80. doi: 10.1016/j.amjsurg.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 17.Pavlicek W, Walton HA, Karstaedt PJ, Gray RJ. Radiation safety with use of I-125 seeds for localization of nonpalpable breast lesions. Acad Radiol. 2006;13:909–15. doi: 10.1016/j.acra.2006.03.017. [DOI] [PubMed] [Google Scholar]
- 18.Pouw B, de Wit-van der Veen L, Stokkel MP, Loo CE, Vrancken Peeters MJ, Valdés Olmos RA. Heading toward radioactive seed localization in non-palpable breast cancer surgery? A meta-analysis. J Surg Oncol. 2015;111:185–91. doi: 10.1002/jso.23785. [DOI] [PubMed] [Google Scholar]
- 19.Fleming MD, Pockaj BA, Hansen AJ, Gray RJ, Patel MD. Radioactive seed localization for excision of non-palpable in-transit metastatic melanoma. Radiol Case Rep. 2006;1:54–7. doi: 10.2484/rcr.v1i2.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grotz TE, Tortorelli CL, Degnim AC, Boughey JC, Whaley DH, Jakub JW. The use of radioactive seed localization for non-palpable non-breast lesions. J Surg Rad. 2010;1:90–5. [Google Scholar]
- 21.Straver ME, Loo CE, Alderliesten T, Rutgers EJ, Vrancken Peeters MT. Marking the axilla with radioactive iodine seeds (MARI procedure) may reduce the need for axillary dissection after neoadjuvant chemotherapy for breast cancer. Br J Surg. 2009;97:1226–31. doi: 10.1002/bjs.7073. [DOI] [PubMed] [Google Scholar]
- 22.Jackson L, Bourke AG, Abdul Aziz F, Taylor D. Radioactive seed localisation to guide removal of impalpable lymph nodes (Radioguided Occult Lesion Localisation using Iodine-125 seeds, “ROLLIS”) BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2013-203267. doi: 10.1136/bcr-2013-203267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gobardhan P, Djamin R, Romme P, et al. The use of iodine seed (I-125) as a marker for the localisation of lung nodules in minimal invasive pulmonary surgery. Eur J Surg Oncol. 2013;39:945–50. doi: 10.1016/j.ejso.2013.06.020. [DOI] [PubMed] [Google Scholar]


