Abstract
Objective
We examined the social and economic factors associated with nursing home (NH) admission in older women, overall and post-stroke.
Methods
The Women’s Health Initiative (WHI) included women aged 50–79 years at enrollment (1993–1998). In the WHI Extension Study (2005–2010), participants annually reported any NH admission in the preceding year. Separate multivariate logistic regression models analyzed social and economic factors associated with long-term NH admission, defined as an admission on two or more questionnaires, overall and post-stroke.
Results
Of 103,237 participants, 8,904 (8.6%) reported NH admission (2005–2010); 534 of 2,225 (24.0%) women with incident stroke reported post-stroke NH admission. Decreased likelihoods of NH admission overall were demonstrated for Asian, Black and Hispanic women (versus whites, aORs=0.35–0.44, p<.001) and women with higher income (aOR= 0.75, 95%CI=0.63–0.90); while increased likelihoods of NH admission overall were seen for women with lower social support (aOR=1.34, 95%CI=1.16–1.54) and with incident stroke (aOR=2.59, 95%CI=2.15–3.12). Increased odds of NH admission after stroke were demonstrated for women with moderate disability after stroke (aOR=2.76, 95%CI=1.73–4.42). Further adjustment for stroke severity eliminated the association found for race/ethnicity, income and social support.
Conclusion
The level of care needed after a disabling stroke may overwhelm social and economic structures in place that might otherwise enable avoidance of nursing home admission. We need to identify ways to provide care consistent with patients’ preferences, even after a disabling stroke.
Keywords: disability, institutionalization, race, ethnicity, social support, long-term care
INTRODUCTION
Stroke is a known risk factor for nursing home (NH) admission (1,2). After stroke, the abrupt onset of disabilities in activities of daily living (particularly bathing and toileting) often leads to NH placement, as patients and families are no longer able to meet care needs at home or in independent living settings. Post-stroke, women are more likely to have functional disability than men (3,4), have more NH admissions for stroke disabilities than men (5), and are less likely than men to be discharged home (6–10). The loss of independence that accompanies stroke may cause significant distress to patients faced with adjusting to a new set of disabilities in a NH while being isolated from their family and friends.
In non-stroke populations, socioeconomic resources and availability of social support may reduce older adults’ odds of NH admission. Being married, living with children or others and owning a house have been associated with a 10–50% decreased likelihood of NH admission among older adults in general populations, not selected specifically for stroke (11). Race/ethnicity has also been reported as a factor associated with NH admission. White race was associated with increased likelihood of NH admission in a recent Health and Retirement Study (12), a systematic review (13) and a meta-analysis (2), although a recent study reported increasing NH admissions among non-white elders (14).
In studies of stroke populations, data on race, ethnicity, income and social support factors relative to post-stroke NH admission are limited. Having more social networks was associated with decreased odds of institutionalization post-stroke in a small (n=62) subsample from the EPESE study (15). Living alone was associated with increased odds of NH admission after stroke in the Northern Manhattan Stroke Study (16). To our knowledge, no studies have compared factors such as race, ethnicity, income and educational attainment, and social support resources that are structural (e.g. living arrangement, marital status) and functional (e.g. availability of someone to provide help or emotional support) associated with NH admission between non-stroke and stroke samples.
Although many patients and families may prefer to avoid NH placement, post-stroke care for disabilities may overwhelm families’ best intentions, causing guilt, frustration and even depression during the critical transition period when patients are admitted to NHs. It is unclear whether socioeconomic factors and social support resources that reduce the likelihood of NH admission among older adults are also protective in the setting of an incident stroke, particularly among older women. A greater understanding of factors that are associated with NH admission among women after stroke may guide future interventions to maximize independence and quality of life.
The Women’s Health Initiative (WHI) provides a unique opportunity to examine factors associated with NH admission in older women, and to study the role of stroke and stroke severity. This multi-center longitudinal prospective study collected NH admission data on a large number of racially, ethnically and geographically diverse older women, a significant number of whom suffered incident strokes.
Analytical Framework
Factors previously associated with NH admission are shown in Figure 1 and are organized within the Behavioral Model for Vulnerable Populations (12,13,17–19). This model conceptualizes healthcare utilization of vulnerable populations as affected by three types of factors: predisposing factors for healthcare utilization, enabling factors that allow individuals to use and choose healthcare, and need factors that drive healthcare utilization. For this analysis, we identified predisposing factors for NH admission (age, race/ethnicity, functional dependence, obesity, and comorbidities), enabling factors that may help an individual avoid NH admission by providing alternatives such as home care or community-based care (socioeconomic factors and social support resources) and need factors that result in a need for NH care (in particular, stroke and stroke-related factors). We were especially interested in determining whether the enabling factors were associated with decreased NH admission after stroke, after adjusting for stroke severity. We hypothesized that enabling socioeconomic and social support resource factors would be associated with decreased NH admission in older women and would remain protective after stroke in older women.
Figure 1.
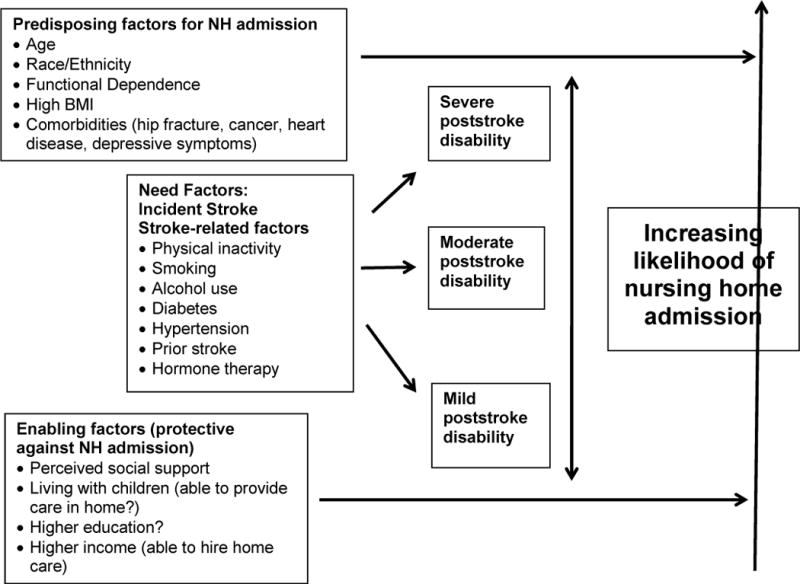
Conceptual framework of factors enabling reduced nursing home admission, with and without incident stroke, based on previous literature and behavioral model for vulnerable populations.
DESIGN AND METHODS
The WHI study began in 1993 as a national, longitudinal study to examine cardiovascular, cancer and other disease outcomes in post-menopausal women. Previous papers have described the study design, population and methods (20–23). The study consisted of several randomized clinical trials (CT), including the Hormone Therapy (HT) Trials, the Dietary Modification Trial and the Calcium and Vitamin D Trial, and the Observational Study (OS). A total of 161,808 postmenopausal women participants aged 50–79 years enrolled in the WHI study at 40 clinical centers from 1993 through 1998. The WHI study continued follow-up of participants who consented with the WHI 2005–2010 and 2010–2015 Extension Studies.
Study Sample
Figure 2 displays the participants in our study. Our eligible sample included 103,237 CT + OS WHI participants who consented to continued follow-up in the WHI 2005–2010 Extension Study, after excluding former participants of the HT trials (n=10,323), due to the increased risk of stroke found among women assigned to active treatment (24), and 1,847 women who were missing data on NH admission. The final regression model analytic sample included 83,657 women after excluding 19,580 women who were missing data on covariates. A sub-group consisted of 2,225 women within the primary eligible cohort who experienced an incident stroke during CT + OS trial or Extension; the final regression model analytic sample was 1,489 women after excluding 736 women missing data on covariates.
Figure 2.
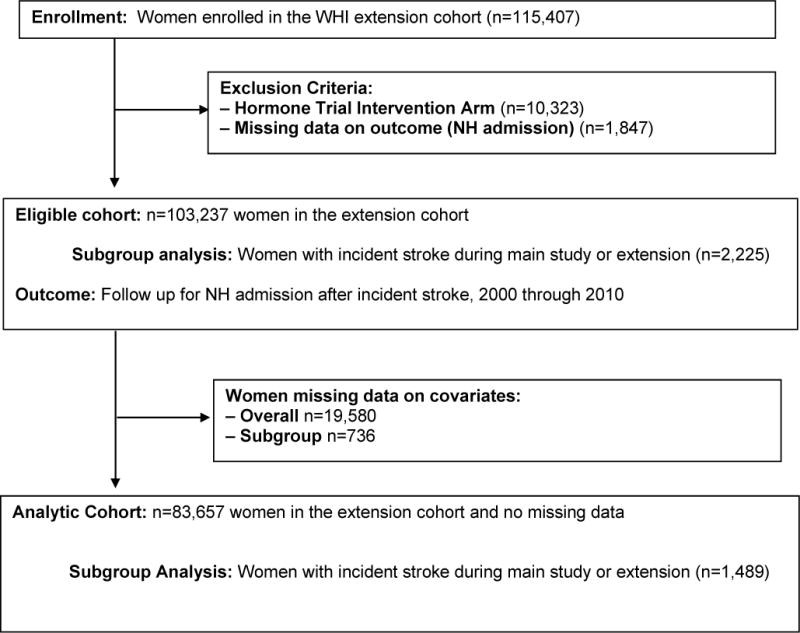
Flow of participants through study and analytic cohort.
Definitions of Variables
Occurrence of NH admission and date of admission were collected by self-report from annual questionnaires administered through the 2005–2010 Extension Study. Women were censored at death, end of study period, or after they last provided follow-up information on NH admission. For the purposes of analyses, NH admission was defined as NH admission reported on two or more annual questionnaires (“In the past year, have you stayed in a nursing home?”), approximating a long-term care NH stay.
Predisposing factors increasing NH admission risk because of increased caregiving needs included age, race/ethnicity, functional dependence, obesity, and comorbidities including prior hip fracture, cardiovascular disease, cancer and depressive symptoms. The self-report form used six mutually exclusive categories for race/ethnicity: American Indian or Alaskan Native, Asian or Pacific Islander, Black or African-American, Hispanic/Latino (regardless of race), White (not of Hispanic origin), and other. Functional dependence was based on the lowest quartile of the SF-36 physical function scale. Body mass index measurements was categorized as underweight (<18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2) and obese (30 or more kg/m2) (25). Comorbidities included prior adjudicated hip fracture, adjudicated cardiovascular disease, adjudicated cancer and baseline depressive symptoms based on Burnam’s modification to the Center for Epidemiologic Studies Depression Scale (26).
Enabling factors included educational attainment, income, and structural and functional social support resources, captured by living arrangement, marital status, and the perceived availability of social support. Education was categorized as high school or less, some college and college degree or more. Income was categorized on the data collection form as <$35,000/year, $35,000 to $50,000/year, $50,000 to $75,000/year, and $75,000 or more per year. Functional social support was assessed by two variables, marital status and living arrangements. Marital status was dichotomized as divorced, widowed, never married vs. married or marriage-like relationship. Living arrangement was categorized as living with children, living with others, living with partner/spouse, or living alone. Perceived availability of functional social support was computed from the Medical Outcomes Study questions, (9 components: presence of someone who listens, gives good advice, takes to the doctor, shares a good time, helps understand a problem, helps with daily chores if sick, shares private worries/fears, does something fun with, loves her/makes her feel wanted; 1=none of the time to 5=all of the time; sum score range 9–45; higher score indicates more perceived social support).
Need factors in the conceptual model included incident stroke, age at stroke, stroke severity, stroke timing, stroke type and cardiovascular risk factors. Incident stroke events were adjudicated using standardized criteria by study physicians who reviewed hospital records. Events not requiring hospitalization and transient ischemic events were not included as strokes. As part of the adjudication process, study physicians reviewed brain imaging reports and determined stroke type (hemorrhagic vs. ischemic) (27,28). We included any stroke during the CT + OS trial or 2005–2010 extension that occurred before or in the same year as NH admission. NH admissions reported in the same year as a stroke event were assumed to be post-stroke after we performed sensitivity analyses where we treated half of such events as pre-stroke admission and half as post-stroke admission.
Stroke severity was determined from the Glasgow Outcomes Scale scores at stroke hospitalization discharge (good recovery, moderate disability and severe disability) (29). Stroke timing was defined as before vs. after the Extension Study.
Physical activity was defined as minutes per week of moderate to vigorous exercise (0 to less than 75 minutes/week, 75 to less than 150 minutes/week, and 150 minutes or more/week). Smoking was defined as current (high pack years (≥20), low pack years (<20)), past high pack years, past low pack years and never). Alcohol use was defined as heavy (7 or more drinks/week), moderate (<7 drinks/week), past drinker, and nondrinker. Diabetes was based on self-report of physician-diagnosed diabetes mellitus treated with insulin or medication, hypertension was based on self-report of physician-diagnosed hypertension treated with medication. Use of menopausal hormone therapy (current, past, never) was also included as a covariate, given the relationship between hormone therapy and incident stroke (24). Type of WHI participation was categorized as Observational Study or Clinical Trial participation.
Statistical methods
The primary endpoint was long-stay NH admission, defined as reported NH admissions on two or more questionnaires during the 2005–2010 Extension Study period. Factors associated with NH admission were assessed with multivariable logistic regression models, separately among all women in the 2005–2010 Extension Study cohort and then among women who were diagnosed with incident stroke during the CT+OS (1993–2005) phase or 2005–2010 Extension Study. Women who were missing data on any covariates were excluded from the statistical analyses. All reported p-values are two-sided and are not corrected for multiple comparisons. Analyses used SAS (version 9.3, SAS Institute Inc., Cary, NC) and Stata (version 11, Stata Corp) software.
RESULTS
Table 1 displays participant characteristics stratified by incident stroke during the CT+OS phase or Extension Study. Women with incident stroke were older and higher percentages had high school or less education, lower income, were not married, lived alone and reported lower social support. Of the eligible WHI Extension Study participant group without stroke, 8,370 (8.3%) reported NH admissions in two or more years between 2005 and 2010. Of the women with incident stroke during the CT+OS phase or Extension Study, 534 (24.0%) reported NH admissions in two or more years after the stroke.
Table 1.
Eligible cohort characteristics by incident stroke status during main study or extension.
| Participant characteristics | No stroke during main study or extension N=101,012 (97.8%) |
Stroke during main study or extension N=2,225 (2.2%) |
p-value |
|---|---|---|---|
| Admitted to nursing home during extension | 8370 (8.3) | 534 (24.0) | <.001* |
| Mean age at extension enrollment (± SD)1 | 70.85 (± 6.83) | 75.06 (± 6.38) | <.001* |
| Race/Ethnicity2 | 0.002* | ||
| American Indian or Alaskan Native | 338 (0.3) | 3 (0.1) | |
| Asian or Pacific Islander | 2127 (2.1) | 32 (1.4) | |
| Black or African-American | 7054 (7.0) | 187 (8.4) | |
| Hispanic/Latino (regardless of race) | 2786 (2.8) | 43 (1.9) | |
| White (not of Hispanic origin) | 87469 (86.8) | 1930 (86.9) | |
| Other | 1018 (1.0) | 25 (1.1) | |
| Marriage/marriage-like relationship at baseline | 66453 (66.1) | 1310 (59.2) | <.001* |
| Social support constructc | 0.001* | ||
| Quartile 1 (0 – 32) | 25346 (25.6) | 629 (29.0) | |
| Quartile 2 (33 – 37) | 23318 (23.6) | 492 (22.7) | |
| Quartile 3 (38 – 42) | 24027 (24.3) | 532 (24.5) | |
| Quartile 4 (43+) | 26196 (26.5) | 516 (23.8) | |
| Living with at baseline | <.001* | ||
| Live with kids | 11775 (11.8) | 231 (10.6) | |
| Live with others | 8785 (8.8) | 208 (9.5) | |
| Live with partner | 56136 (56.2) | 1135 (51.8) | |
| Live alone | 23116 (23.2) | 616 (28.1) | |
| Education at baseline | <.001* | ||
| High school or less | 19250 (19.2) | 501 (22.7) | |
| Some college | 36836 (36.7) | 880 (39.9) | |
| College degree | 44238 (44.1) | 825 (37.4) | |
| Income at baseline | <.001* | ||
| <35k | 33344 (35.0) | 983 (47.1) | |
| 35–50k | 20035 (21.0) | 460 (22.1) | |
| 50–75k | 20850 (21.9) | 369 (17.7) | |
| 75k+ | 20983 (22.0) | 274 (13.1) |
Significant at p< .05.
N (%) for categorical variables; mean (±SD=Standard deviation) for continuous variables.
Numbers may not add to total N due to missing data.
Social Support variable based on Rand 36 (higher score = higher social support)
Table 2 displays the final adjusted multivariable logistic regression model for the outcome of long-term NH admission for the Extension Study cohort, excluding women with any covariates missing. Non-white women, particularly Asian, Black and Hispanic women, had a 56–65% decreased odds of NH admission compared to White women. Higher income was associated with up to 25% decreased odds of NH admission. Having a college degree (vs. high school education) was associated with a 26% increased odds of NH admission. Lower perceived social support was associated with a 34% increased odds of NH admission and living with one’s children was associated with at 25% decreased odds of NH admission.
Table 2.
Adjusted multivariate logistic regression models of factors associated with long-term NH admission for 1) Full extension study cohort and 2) among women who had an incident stroke.
| Overall Cohort (n=83,657) |
Stroke Only Cohort (n=1,489) |
|||
|---|---|---|---|---|
| Characteristic1 | aOR (95% CI) | p-value | aOR (95% CI) | p-value |
| Factors enabling NH avoidance | ||||
| Ethnicity | <.0001* | 0.1142 | ||
| American Indian vs. White | 0.78 (0.32, 1.91) | – | ||
| Asian vs. White | 0.35 (0.19, 0.64) | – | ||
| Black vs. White | 0.44 (0.34, 0.57) | 0.35 (0.13, 0.94) | ||
| Hispanic vs. White | 0.42 (0.25, 0.69) | 0.36 (0.04, 3.09) | ||
| Other vs. White | 0.70 (0.41, 1.20) | 0.45 (0.1, 2.02)2 | ||
| Not married vs. married | 0.94 (0.75, 1.16) | 0.5517 | 0.43 (0.17, 1.05) | 0.0647 |
| Social support Quartiles | <.0001* | 0.6560 | ||
| Q1 vs. Q4 (lowest vs. highest) | 1.34 (1.16, 1.54) | 0.8 (0.45, 1.4) | ||
| Q2 vs. Q4 | 1.05 (0.90, 1.22) | 1.06 (0.62, 1.82) | ||
| Q3 vs. Q4 | 1.08 (0.93, 1.25) | 1.1 (0.65, 1.86) | ||
| Living with | 0.0154* | 0.2561 | ||
| Kids vs. None | 0.75 (0.60, 0.93) | 0.36 (0.13, 1) | ||
| Others vs. None | 0.80 (0.66, 0.97) | 0.72 (0.33, 1.6) | ||
| Partner vs. None | 0.72 (0.57, 0.91) | 0.49 (0.18, 1.31) | ||
| Education | 0.0004* | 0.6542 | ||
| Some college vs. high school | 1.04 (0.91, 1.18) | 1.2 (0.72, 2) | ||
| College vs. high school | 1.26 (1.10, 1.45) | 1.3 (0.74, 2.28) | ||
| Income | 0.0147* | 0.1553 | ||
| 35–50k vs. <35k | 0.95 (0.84, 1.08) | 0.67 (0.4, 1.13) | ||
| 50–75k vs. <35k | 0.87 (0.75, 1.01) | 1.08 (0.63, 1.88) | ||
| 75k+ vs. <35k | 0.75 (0.63, 0.90) | 0.57 (0.27, 1.17) | ||
| Predisposing Factors for NH admission | ||||
| Age at extension enrollment | 1.09 (1.08, 1.10) | <.0001* | 1.03 (0.96, 1.11) | 0.3496 |
| Physical functioning Quartiles | <.0001* | 0.1838 | ||
| Q1 vs. Q4 (lowest vs. highest) | 2.77 (2.38, 3.23) | 1.58 (0.92, 2.7) | ||
| Q2 vs. Q4 | 1.85 (1.59, 2.15) | 1.14 (0.67, 1.95) | ||
| Q3 vs. Q4 | 1.49 (1.25, 1.79) | 0.83 (0.41, 1.69) | ||
| Baseline BMI | <.0001* | 0.2471 | ||
| Obese vs. Normal | 1.71 (1.49, 1.95) | 1.4 (0.83, 2.36) | ||
| Overweight vs. Normal | 1.13 (1.00, 1.29) | 0.96 (0.59, 1.53) | ||
| Underweight vs. Normal | 1.18 (0.68, 2.05) | −3 | ||
| Cardiovascular disease at baseline | 1.34 (1.20, 1.49) | <.0001* | 1.15 (0.76, 1.72) | 0.5121 |
| Cancer at baseline | 1.00 (0.86, 1.17) | 0.9771 | 0.66 (0.34, 1.29) | 0.2247 |
| Hip fracture ever | 4.40 (3.77, 5.14) | <.0001* | 2.39 (1.32, 4.35) | 0.0043* |
| Depressive symptoms | 1.21 (1.04, 1.41) | 0.0119* | 1.05 (0.53, 2.11) | 0.8852 |
| Stroke-related variables | ||||
| Stroke in main trial/extension | 2.59 (2.15, 3.12) | <.0001* | – | |
| Age at stroke | – | 1.02 (0.96, 1.09) | 0.4806 | |
| Hemorrhagic vs. Ischemic Stroke | – | 1.57 (0.92, 2.68) | 0.0988 | |
| Glasgow Score at Hospital Discharge | – | 0.0001* | ||
| Moderately disabled vs. Good recovery | – | 2.76 (1.73, 4.42) | ||
| Severely disabled vs. Good recovery | – | 1.61 (1.02, 2.53) |
Significant at p< .05.
Separate multivariable linear regression models for overall cohort and stroke only cohort. Fully adjusted models shown also adjusted for factors related to risk of stroke, including physical activity, smoking, alcohol use, diabetes, hypertension, stroke prior to baseline of the WHI study, hormone therapy and participation in WHI observational vs. clinical trial.
Other ethnicities include Asian American and Native American because of very small numbers within these groups.
Normal BMI includes underweight because of very small numbers of subjects in that category.
Table 2 also displays the final adjusted multivariable logistic regression model for the outcome of post-stroke long-term NH admission for the Extension Study cohort women with incident stroke during the follow up period (n=1,489 women with complete data for all included variables). Race/ethnicity, income and social support resources were not significantly associated with odds of NH admission in this model after adjusting for stroke severity. Moderate disability, indicated by Glasgow Score at the time of discharge from the stroke hospitalization, was associated with a 2.76-fold increased odds of post-stroke long-term NH admission compared to good recovery.
DISCUSSION
In this large cohort of postmenopausal American women, incident stroke was associated with a 2.59-fold increased odds of long-term NH admission, and moderate disability after stroke was associated with a 2.76-fold increased odds of post-stroke long-term NH admission. Race/ethnicity, income, and social support resources were associated with decreased likelihood of long-term NH admission overall, but were not significantly associated with post-stroke long-term NH admission after adjusting for stroke severity.
Among our overall cohort, Asian, Black and Hispanic women had a 56–65% decreased odds of NH admission compared to white women. Previous studies have reported mixed findings on the relationship between race/ethnicity and NH admission. A recent Health and Retirement study, a systematic review and a meta-analysis reported increased likelihood of NH admission for white race (2,12,30,31). A recent national U.S. study reported increasing numbers of non-white elders admitted to NHs and suggested that prior disparities in access to NH care for non-white elders may be changing, with more white elders seeking alternatives to NH care while more non-white elders may be reliant on NH care due to changing family dynamics (14). It is unclear in our study whether fewer non-white women reported NH admissions because of preference to avoid NH admissions or due to lack of access to NH care.
We also found perceived social support and living with others were independently associated with long-term NH admission. Low perceived social support was associated with a 34% increased odds of NH admission and living with children or a partner was associated with a 25–28% decreased odds of NH admission in the overall sample. Marital status was not associated with odds of NH admission. Living with others and higher social support were associated with 17–65% decreased likelihood of NH admission in previous studies (2,13,30,32). This finding highlights the distinction between structural (such as marital status or living with others) vs. functional/perceived support, as these may represent different entities, so adjusting for only structural support, such as living alone, may not adequately capture the social support environment.
In our study, higher income was associated with up to a 25% decreased odds of NH admission, while income was not significantly associated with NH admission in prior general population studies (2,13). However, higher income might enable women to hire private home care services rather than going to a NH.
Among women with incident stroke, race/ethnicity, income and social support resources were not associated with NH admission after adjusting for stroke severity. Severity of disability from stroke may have overwhelmed the protection afforded by these variables among the women in this cohort. Among 87 post-stroke patients in the EPESE study in New Haven Connecticut, larger social network was associated with decreased risk of institutionalization after stroke, but the analyses did not adjust for severity of stroke (15). Living alone was associated with an 80% increased odds of NH admission in the Northern Manhattan Stroke Study, but this was overshadowed by the finding that a severely disabling stroke was associated with a 27-fold increased odds of NH admission (16). In previous U.S. studies of stroke patients, perceived social support was often not included as a covariate (33), and was inconsistently associated with post-acute discharge destination in a systematic review of six stroke articles with 46 to 524 hospitalized patients in each study (34). The National Stroke Project study did not examine other social factors, and race/ethnicity was not selected for the final models due to lack of significant associations (35). It is important to examine factors associated with NH admission after stroke, especially among diverse populations such as the WHI, because non-white residents have been reported to have higher prevalence of stroke at the time of NH admission (36). Newly admitted non-white NH residents were also shown to have higher ADL disability than white residents, suggesting that these non-white residents had been able to better delay NH placement until the ADL disability became overwhelming (36).
Limitations and Strengths
This study had several limitations. Social factors, such as marital status, which could change over time, were not analyzed as time-dependent covariates. Although structural and functional components of social support were assessed in these analyses, we did not assess the size of the support network, which might be important if larger social support networks allow for pooling of resources which may mitigate NH admission. These may be of interest for a future study. The smaller sample size of the stroke subgroup may limit our detection of significant findings in this subgroup. The data on nursing home admission was collected annually, and dates of admission and length of stay were not available. The nature of the strongly interval-censored data required the use of logistic regression, rather than a method that is sensitive to varying lengths of post-stroke follow-up.
We examined the outcome of long-term NH admission, defined as a report of NH admission on two or more annual questionnaires. Interestingly, the findings did not significantly change in sensitivity analyses examining one versus more than one reports of NH admission on the annual questionnaires (only one NH admission might indicate a short-term rehabilitation stay, rather than a long-term NH stay).
Strengths of our study include the large sample size and the racial, ethnic and geographic diversity of older women in the study population, allowing us to carefully examine the effects of race/ethnicity, income and social factors, fully adjusting for stroke and other important disease and function-related factors associated with NH admission. These characteristics were prospectively obtained prior to the incident stroke event. Stroke outcomes were classified and prospectively collected using standardized criteria.
Implications
Our findings suggest that while race, ethnicity, income and social support resources may be associated with lower odds of NH admissions, these factors are less influential in the setting of an incident stroke with subsequent moderate to severe disability. This may be due to the overwhelming burden on the social support network that was providing assistance to the woman at home prior to the stroke. Further research is needed to examine the women with severe functional impairment post-stroke who did not report long-term NH admission. It is not clear from our data whether women did not report NH admissions because they were able to receive care at home or elsewhere, or if they lacked access to NH care. A better understanding of patterns in receipt of care and recovery after stroke may help us to identify disparities in care and identify ways to provide care consistent with patients’ preferences.
Conclusion
We examined long-term NH admission among postmenopausal American women in the WHI 2005–2010 Extension Study (n=103,237), and among a subgroup of these women with incident stroke (n=2,225). Non-white race/ethnicity, higher income and higher social support were associated with reduced likelihood of NH admission in the overall cohort, but were not associated with subsequent NH admission among women with incident stroke after adjusting for stroke severity. Our results imply that the level of care needed after a disabling stroke may overwhelm social and economic structures in place that might otherwise enable avoidance of nursing home admission. Further research is needed to better understand how to augment caregiving for patients to minimize or ease the transition to NH admission, particularly after an acute stroke.
Acknowledgments
The WHI is funded by the National Heart, Lung, and Blood Institute, NIH, U.S. Department of Health and Human Services (HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C). This research was supported by WHl Extension 2010–2015 Westem Regional Subcontract through Stanford University from the National Heart, Lung and Blood Institute, National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Christina L. Bell, Email: bellcl@hawaii.edu.
Andrea Z. LaCroix, Email: alacroix@whi.org.
Manisha Desai, Email: manishad@stanford.edu.
Haley Hedlin, Email: hedlin@stanford.edu.
Stephen R. Rapp, Email: srapp@wakehealth.edu.
Crystal Cene, Email: crystal_cene@med.unc.edu.
Jyoti Savla, Email: marcias@stanford.edu.
Tetyana Shippee, Email: tshippee@umn.edu.
Sylvia Wassertheil-Smoller, Email: Sylvia.Smoller@einstein.yu.edu.
Kamal Masaki, Email: km1@hawaii.rr.com.
References
- 1.Gill TM, Allore HG, Holford TR, et al. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292:2115–2124. doi: 10.1001/jama.292.17.2115. [DOI] [PubMed] [Google Scholar]
- 2.Gaugler JE, Duval S, Anderson KA, et al. Predicting nursing home admission in the U.S: a meta-analysis. BMC Geriatr. 2007;7:13. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reeves MJ, Bushnell CD, Howard G, et al. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008;7:915–926. doi: 10.1016/S1474-4422(08)70193-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petrea RE, Beiser AS, Seshadri S, et al. Gender differences in stroke incidence and poststroke disability in the Framingham heart study. Stroke. 2009;40:1032–1037. doi: 10.1161/STROKEAHA.108.542894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leibson CL, Ransom JE, Brown RD, et al. Stroke-attributable nursing home use: a population-based study. Neurology. 1998;51:163–168. doi: 10.1212/wnl.51.1.163. [DOI] [PubMed] [Google Scholar]
- 6.Reeves MJ, Fonarow GC, Zhao X, et al. Quality of care in women with ischemic stroke in the GWTG program. Stroke. 2009;40:1127–1133. doi: 10.1161/STROKEAHA.108.543157. [DOI] [PubMed] [Google Scholar]
- 7.Persky RW, Turtzo LC, McCullough LD. Stroke in women: disparities and outcomes. Curr Cardiol Rep. 2010;12:6–13. doi: 10.1007/s11886-009-0080-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Turtzo LC, McCullough LD. Sex differences in stroke. Cerebrovasc Dis. 2008;26:462–474. doi: 10.1159/000155983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holroyd-Leduc JM, Kapral MK, Austin PC, et al. Sex differences and similarities in the management and outcome of stroke patients. Stroke. 2000;31:1833–1837. doi: 10.1161/01.str.31.8.1833. [DOI] [PubMed] [Google Scholar]
- 10.Kapral MK, Fang J, Hill MD, et al. Sex differences in stroke care and outcomes: results from the Registry of the Canadian Stroke Network. Stroke. 2005;36:809–814. doi: 10.1161/01.STR.0000157662.09551.e5. [DOI] [PubMed] [Google Scholar]
- 11.Luppa M, Luck T, Weyerer S, et al. Gender differences in predictors of nursing home placement in the elderly: a systematic review. Int Psychogeriatr. 2009;21:1015–1025. doi: 10.1017/S1041610209990238. [DOI] [PubMed] [Google Scholar]
- 12.Thomeer MB, Mudrazija S, Angel JL. How Do Race and Hispanic Ethnicity Affect Nursing Home Admission? Evidence From the Health and Retirement Study. J Gerontol B Psychol Sci Soc Sci. 2014 doi: 10.1093/geronb/gbu114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luppa M, Luck T, Weyerer S, et al. Prediction of institutionalization in the elderly. A systematic review. Age Ageing. 2010;39:31–38. doi: 10.1093/ageing/afp202. [DOI] [PubMed] [Google Scholar]
- 14.Feng Z, Fennell ML, Tyler DA, et al. The Care Span: Growth of racial and ethnic minorities in US nursing homes driven by demographics and possible disparities in options. Health Aff (Millwood) 2011;30:1358–1365. doi: 10.1377/hlthaff.2011.0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Colantonio A, Kasl SV, Ostfeld AM, et al. Psychosocial predictors of stroke outcomes in an elderly population. J Gerontol. 1993;48:S261–268. doi: 10.1093/geronj/48.5.s261. [DOI] [PubMed] [Google Scholar]
- 16.Rundek T, Mast H, Hartmann A, et al. Predictors of resource use after acute hospitalization: the Northern Manhattan Stroke Study. Neurology. 2000;55:1180–1187. doi: 10.1212/wnl.55.8.1180. [DOI] [PubMed] [Google Scholar]
- 17.Gelberg L, Andersen RM, Leake BD. The Behavioral Model for Vulnerable Populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34:1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 18.Borrayo EA, Salmon JR, Polivka L, et al. Utilization across the continuum of long-term care services. Gerontologist. 2002;42:603–612. doi: 10.1093/geront/42.5.603. [DOI] [PubMed] [Google Scholar]
- 19.Keysor JJ, Desai T, Mutran EJ. Elders’ preferences for care setting in short- and long-term disability scenarios. Gerontologist. 1999;39:334–344. doi: 10.1093/geront/39.3.334. [DOI] [PubMed] [Google Scholar]
- 20.Anderson GL, Manson J, Wallace R, et al. Implementation of the Women’s Health Initiative study design. Ann Epidemiol. 2003;13:S5–17. doi: 10.1016/s1047-2797(03)00043-7. [DOI] [PubMed] [Google Scholar]
- 21.Langer RD, White E, Lewis CE, et al. The Women’s Health Initiative Observational Study: baseline characteristics of participants and reliability of baseline measures. Ann Epidemiol. 2003;13:S107–121. doi: 10.1016/s1047-2797(03)00047-4. [DOI] [PubMed] [Google Scholar]
- 22.Ritenbaugh C, Patterson RE, Chlebowski RT, et al. The Women’s Health Initiative Dietary Modification trial: overview and baseline characteristics of participants. Ann Epidemiol. 2003;13:S87–97. doi: 10.1016/s1047-2797(03)00044-9. [DOI] [PubMed] [Google Scholar]
- 23.Stefanick ML, Cochrane BB, Hsia J, et al. The Women’s Health Initiative postmenopausal hormone trials: overview and baseline characteristics of participants. Ann Epidemiol. 2003;13:S78–86. doi: 10.1016/s1047-2797(03)00045-0. [DOI] [PubMed] [Google Scholar]
- 24.Wassertheil-Smoller S, Hendrix SL, Limacher M, et al. Effect of estrogen plus progestin on stroke in postmenopausal women: the Women’s Health Initiative: a randomized trial. JAMA. 2003;289:2673–2684. doi: 10.1001/jama.289.20.2673. [DOI] [PubMed] [Google Scholar]
- 25.LaCroix AZ, Gray SL, Aragaki A, et al. Statin use and incident frailty in women aged 65 years or older: prospective findings from the Women’s Health Initiative Observational Study. J Gerontol A Biol Sci Med Sci. 2008;63:369–375. doi: 10.1093/gerona/63.4.369. [DOI] [PubMed] [Google Scholar]
- 26.Burnam MA, Wells KB, Leake B, et al. Development of a brief screening instrument for detecting depressive disorders. Med Care. 1988;26:775–789. doi: 10.1097/00005650-198808000-00004. [DOI] [PubMed] [Google Scholar]
- 27.McGinn AP, Kaplan RC, Verghese J, et al. Walking speed and risk of incident ischemic stroke among postmenopausal women. Stroke. 2008;39:1233–1239. doi: 10.1161/STROKEAHA.107.500850. [DOI] [PubMed] [Google Scholar]
- 28.Curb JD, McTiernan A, Heckbert SR, et al. Outcomes ascertainment and adjudication methods in the Women’s Health Initiative. Ann Epidemiol. 2003;13:S122–128. doi: 10.1016/s1047-2797(03)00048-6. [DOI] [PubMed] [Google Scholar]
- 29.Albanese MA, Clarke WR, Adams HP, Jr, et al. Ensuring reliability of outcome measures in multicenter clinical trials of treatments for acute ischemic stroke. The program developed for the Trial of Org 10172 in Acute Stroke Treatment (TOAST) Stroke. 1994;25:1746–1751. doi: 10.1161/01.str.25.9.1746. [DOI] [PubMed] [Google Scholar]
- 30.Zweig SC, Popejoy LL, Parker-Oliver D, et al. The physician’s role in patients’ nursing home care: “She’s a very courageous and lovely woman. I enjoy caring for her”. JAMA. 2011;306:1468–1478. doi: 10.1001/jama.2011.1420. [DOI] [PubMed] [Google Scholar]
- 31.Harris Y, Cooper JK. Depressive symptoms in older people predict nursing home admission. Journal of the American Geriatrics Society. 2006;54:593–597. doi: 10.1111/j.1532-5415.2006.00687.x. [DOI] [PubMed] [Google Scholar]
- 32.Noel-Miller C. Spousal loss, children, and the risk of nursing home admission. J Gerontol B Psychol Sci Soc Sci. 2010;65B:370–380. doi: 10.1093/geronb/gbq020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Colantonio A, Kasl SV, Ostfeld AM, et al. Prestroke physical function predicts stroke outcomes in the elderly. Arch Phys Med Rehabil. 1996;77:562–566. doi: 10.1016/s0003-9993(96)90295-6. [DOI] [PubMed] [Google Scholar]
- 34.Meijer R, van Limbeek J, Kriek B, et al. Prognostic social factors in the subacute phase after a stroke for the discharge destination from the hospital stroke-unit. A systematic review of the literature. Disability & Rehabilitation. 2004;26:191–197. doi: 10.1080/09638280310001636437. [DOI] [PubMed] [Google Scholar]
- 35.Dallas MI, Rone-Adams S, Echternach JL, et al. Dependence in prestroke mobility predicts adverse outcomes among patients with acute ischemic stroke. Stroke. 2008;39:2298–2303. doi: 10.1161/STROKEAHA.107.506329. [DOI] [PubMed] [Google Scholar]
- 36.Buchanan RJ, Rosenthal M, Graber DR, et al. Racial and ethnic comparisons of nursing home residents at admission. J Am Med Dir Assoc. 2008;9:568–579. doi: 10.1016/j.jamda.2008.04.012. [DOI] [PubMed] [Google Scholar]


