Abstract
Context
Patients and families commonly experience spiritual stress during an intensive care unit (ICU) admission. While a majority of patients report that they want spiritual support, little is known about how these issues are addressed by hospital chaplains.
Objectives
To describe the prevalence, timing, and nature of hospital chaplain encounters in ICUs.
Methods
This was a retrospective cross-sectional study of adult ICUs at an academic medical center. Measures included: days from ICU admission to initial chaplain visit, days from chaplain visit to ICU death or discharge, hospital and ICU length of stay, severity of illness at ICU admission and chaplain visit, and chart documentation of chaplain communication with the ICU team.
Results
Of a total of 4169 ICU admissions over six months, 248 (5.9%) patients were seen by chaplains. Of the 246 patients who died in an ICU, 197 (80%) were seen by a chaplain. There was a median of two days from ICU admission to chaplain encounter and a median of one day from chaplain encounter to ICU discharge or death. Chaplains communicated with nurses after 141 encounters (56.9%), but with physicians after only 14 encounters (5.6%); there was no documented communication in 55 encounters (22%).
Conclusion
In the ICUs at this tertiary medical center, chaplain visits are uncommon and generally occur just before death among ICU patients. Communication between chaplains and physicians is rare. Chaplaincy service is primarily reserved for dying patients and their family members rather than providing proactive spiritual support. These observations highlight the need to better understand challenges and barriers to optimal chaplain involvement in ICU patient care.
Keywords: intensive care, critical care, chaplain, spiritual care, death, religion
Introduction
Admission to the Intensive Care Unit (ICU) is a stressful and vulnerable experience for both patients and families, often eliciting spiritual questions and concerns (1). One in five deaths in the United States will occur in the ICU or shortly after discharge from the ICU, and most of these deaths will occur from withdrawing life support or incurable illnesses (2). During this time, patients and families look not only to medical interventions for healing, but many also desire emotional and spiritual healing (3).
A majority of Americans consider religion important in daily life (4). A study in cancer outpatients showed that patients with positive religious coping tend to have higher rates of ICU death, more aggressive care at the end of life, less hospice use, and greater health care costs at the end of life, signifying that religion and spirituality may be important in end-of-life decision making (5, 6). Also, when spiritual needs are not met by the heath care team, patients tend to rate care more poorly (7, 8). In contrast, when spiritual needs are met by the health care team, patients have less aggressive care, more hospice use, lower rates of ICU death, and lower health care costs at the end of life (9, 10). There also have been possible correlations specifically between chaplain visits and hospice use (11). Addressing spiritual issues of patients is now required by National Palliative Care guidelines as well the Joint Commission (12, 13). In addition, a task force of experts in Critical Care Medicine, in a consensus statement on clinical practices, expressed the importance of addressing spiritual needs of patients and families in the ICU (14). However, few patient care teams explicitly address the spiritual needs of patients and families (4, 15).
Physicians typically feel unprepared to elicit patients’ spiritual beliefs, to include religion and spirituality in decision making, or to address the spiritual needs of patients and families (16, 17). Hospital chaplains are considered the spiritual professionals in the inpatient setting. While the literature regarding chaplain involvement in the hospital setting is growing, in Australia and New Zealand, chaplains have been shown to be important in various clinical contexts including pain control, bioethics, and treatment decisions (18–20). Studies in discharged general medical inpatients have found that patients would welcome chaplain visits, but these visits tend to be infrequent (21). However, there is still limited research in understanding the role of chaplains specifically in the ICU—a potentially important opportunity to help address patients’ and families’ spiritual crises.
To begin to identify targets for improving spiritual care for patients and families in the ICU, we performed a six-month retrospective study in a single large academic medical center. Our primary aim in this study was to describe the patient population in the ICUs at Duke University Hospital who receive chaplain visitation, as well as the timing and content of these visits in relationship to ICU admission and discharge or death. Our secondary aim was to understand the referral and communication patterns between hospital chaplains and the primary ICU team. Based on our clinical experience, we hypothesized that chaplain visits in the ICU are primarily reserved for the families of actively dying patients and that communication between hospital chaplains and ICU physicians is limited. Our overarching goal is to understand how spiritual care is currently being provided, and to identify ways to improve spiritual care for patients and families in the ICU.
Methods
Design
We performed a cross-sectional, retrospective chart review over a six-month period, coinciding with the implementation of a new electronic health record (EHR) system. We identified the study population using queries of the EHR. First, we identified all adult patients aged 18 years and older who were admitted to one of five adult ICUs at Duke University Hospital between June 24, 2013 and December 24, 2013. These ICUs included the Medical Intensive Care Unit (MICU), Cardiac Care Unit (CCU), Neuro Intensive Care Unit (NICU), Cardiothoracic Intensive Care Unit (CTICU), and Surgical Intensive Care Unit (SICU). The final study population was then captured by identifying all patients with at least one encounter note signed by a chaplain, chaplain resident, or chaplain intern during the ICU admission that immediately preceded hospital discharge or death. At Duke University Hospital, there are four chaplain residents who train for one year, staffing the five adult ICUs during the day, while chaplain interns and residents take call overnight. Any member of the ICU team may request a chaplain visit, or chaplains may self-initiate visits. While a question regarding spiritual needs is part of the initial nursing admission assessment, there are no other clear systematic triggers or protocols for chaplain visits during an ICU stay. Among non-ICU patients, the only clear trigger for a chaplain visit is when a code blue for cardiorespiratory arrest is called. All chaplains at Duke University Hospital are trained in electronic documentation of all patient encounters, including when patients or families are unavailable at the time of visitation. The subject of documentation includes ministry interventions performed, from whom the consult was received, and with whom the patient encounter was discussed.
Study Measures
We recorded age, gender, race, religion, and ICU location of all patients from EHR queries. Similarly, primary ICU admission diagnosis, ICU length of stay (LOS), ventilator days (if applicable), and hospital LOS were collected by review of the medical record. Severity of illness was calculated both at the time of index ICU admission as well as the time of first chaplain visit using the SOFA (sequential organ failure assessment) score. The SOFA score takes into account PaO2/FiO2, mean arterial pressure/vasopressor use, Glasgow Coma Scale (GCS), bilirubin, platelets, and creatinine/urine output to create a composite score of organ dysfunction, with one study showing an initial/highest SOFA of greater than 11 predicting up to 80% mortality (22). For missing values, normal values were substituted. Bilirubin and GCS were most frequently missing, in which case SOFA may be underestimated. Circumstance of death (cardiac arrest with active attempt at resuscitation or withdrawal of life support) or discharge disposition was recorded. The date of the first chaplain note was recorded, and from this we determined the number of days from ICU admission to the first chaplain note as well as days from the first chaplain note to death or discharge. From the chaplain note, we obtained data regarding who requested the chaplain visit as well as with whom the chaplains discussed the patient encounter. Additionally, in order to compare experiences in different ICUs, we obtained characteristics of each study ICU, including total number of admissions, total number of ventilated patients, and total ICU mortality.
This study was conducted in accordance with the amended Declaration of Helsinki. The Duke Institutional Review Board (Pro00050710) approved all study procedures. Written informed consent was waived for this chart review.
Statistical Analyses
We present categorical data using percentages and continuous data as means (standard deviation) or medians (interquartile ranges [IQR]). We used Chi-square tests to evaluate differences in key clinical variables between patients who died and did not die (Table 1), as well as differences across ICUs (Table 2).
Table 1.
Demographics of Patients with Documented Chaplain Care, Stratified by ICU Mortality
| Characteristic | Patients n=248 | Patients Who Died n=197 (79) | Patients Who Did Not Die, n=51 (21) |
|---|---|---|---|
| Age, yrs, mean (SD), P=0.7 | 60.6 (16.7) | 60.4 (16.4) | 61.2 (18.1) |
|
| |||
| Female, n (%), P=0.12 | 112 (45) | 84 (43) | 27 (53) |
|
| |||
| Race, n (%) P=0.8 | |||
| White | 160 (65) | 126 (64) | 34 (67) |
| African American | 70 (28) | 56 (28) | 14 (27) |
| Asian | 3 (1) | 2 (1) | 1 (2) |
| Other | 15 (6) | 13 (7) | 2 (4) |
|
| |||
| Religion, n (%), P=0.34 | |||
| Protestant | 169 (68) | 135 (69) | 34 (69) |
| Baptist | 65 (26) | 53 (27) | 12 (24) |
| Catholic | 16 (6) | 10 (5) | 6 (12) |
| Hindu | 3 (1) | 2 (1) | 1 (2) |
| Jewish | 2 (1) | 1 (1) | 1 (2) |
| Other | 58 (23) | 49 (25) | 9 (18) |
Table 2.
Overall ICU Admission and Mortality Dataa
| MICU | CCU | NICU | CTICU | SICU | TOTAL | |
|---|---|---|---|---|---|---|
| Admission, Total (n) | 693 | 1060 | 668 | 1166 | 582 | 4169 |
| Mechanical ventilation provided, n (%) | 302 (44) | 170 (16) | 215 (32) | 815 (70) | 276 (47) | 1778 (43) P<0.0001 |
| Patients seen by a chaplain, total n (% of all ICU admissions) | 91 (13) | 59 (6) | 42 (6) | 23 (2) | 33 (6) | 248 (6) P<0.0001 |
| Mechanically ventilated patients seen by a chaplain, n (%) | 68 (23) | 34 (20) | 30 (14) | 22 (3) | 25 (9) | 179 (10) P<0.0001 |
| ICU deaths, total n (%) | 108 (16) | 53 (5) | 29 (4) | 26 (2) | 30 (5) | 246 (6) P<0.0001 |
| ICU deaths among those seen by a chaplain, n (%) | 82 (76) | 40 (75) | 25 (86) | 23 (88) | 27 (90) | 197 (80) P=0.24 |
MICU, Medical Intensive Care Unit; CCU, Cardiac Care Unit; NICU, Neuro Intensive Care Unit; CTICU, Cardiothoracic Intensive Care Unit; SICU, Surgical Intensive Care Unit.
Separated by ICU and patients who were seen by chaplains during 6 study months between June 24–December 24, 2013.
Results
Patient Demographics
Among a total of 4169 admissions to adult ICUs over six months, 248 patients (5.9%) had documented chaplaincy care during their index ICU stay. Most patients receiving visits were white (64%), male (55%), and Protestant Christian (64%).
Chaplain visits were most frequently requested for patients in the MICU (13% of total MICU admissions), and they were least frequently requested for patients in the CTICU (2% of total CTICU admission) (Tables 1 and 2).
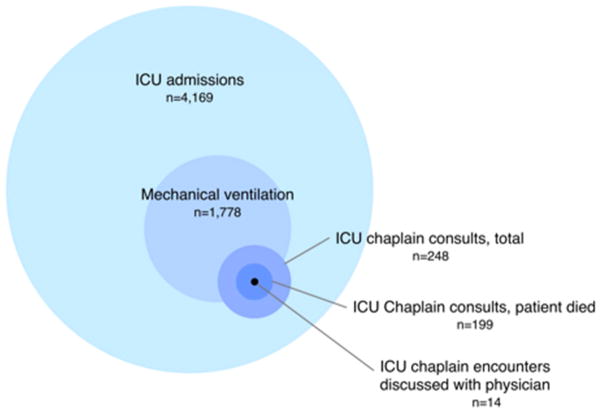
Of 246 patients who died in the ICU, 199 (81%) received chaplain visits (Table 2, Fig. 1). The most common diagnoses for all patients with documented chaplain care were solid tumors (14%), cardiac arrest (13%), septic shock (12%), cerebral vascular accident/intracerebral hemorrhage (CVA/ICH) (8%), cardiogenic shock (8%), and acute lung injury/acute respiratory distress syndrome (ALI/ARDS) (7%). Median hospital LOS was six days (IQR 2–15), median ICU LOS was four days (IQR 2–9.25), and median ventilator days was four days (IQR 1–9). Median SOFA score at ICU admission was 7.5 (IQR 4–11), while the median SOFA score at the time of first chaplain note was 9 (IQR 4–12). Among patients who died, 179 (73%) died from withdrawal of life support and/or under “comfort care,” and 18 (7%) died because of cardiorespiratory arrest with active attempts at resuscitation (Table 3).
Fig. 1.
Graphical depiction comparing ICU chaplain consults to total ICU admissions. Chaplain consults represent a small proportion of total ICU admissions, with most of these consults occurring in patients who were mechanically ventilated and died in the ICU. Communication between chaplain and physician occurs infrequently.
Table 3.
Hospital Characteristics and Outcomes of Patients Seen by Chaplainsa
| Characteristic | |
|---|---|
| Diagnosis | |
| Solid Tumor | 35 (14) |
| Cardiac Arrest | 31 (13) |
| Septic Shock | 29 (12) |
| CVA/ICH | 20 (8) |
| Cardiogenic Shock | 19 (8) |
| ALI/ARDS | 17 (7) |
| Other | 151 (61) |
|
| |
| Hospital length of stay | 6 (2,15) |
|
| |
| ICU length of stay | 4 (2,9.25) |
|
| |
| Mechanical ventilation | 179 (72) |
|
| |
| Ventilator Days, total | 4.0 (1,9) |
|
| |
| SOFA at ICU admission | 7.5 (4,11) |
|
| |
| SOFA at time of first chaplain note | 9 (4,12) |
|
| |
| Discharge Disposition | |
| Death (total) | 197 (79) |
| Death (withdrawal/comfort) | 179 (72) |
| Death (code) | 18 (7) |
| Home | 30 (12) |
| Long-Term Acute Care | 9 (4) |
| Hospice | 8 (3) |
| Transfer to another hospital | 3 (1) |
| Nursing Home | 1 (0.4) |
ALI = acute lung injury; ARDS = acute respiratory distress syndrome; CVA = cerebral vascular accident; ICH = intracerebral hemorrhage; SOFA = sequential organ failure assessment.
Shown as number (percent) or median (interquartile range).
Other Clinically Relevant Outcomes of Patients Seen by Chaplains
The median time from ICU admission to first chaplain note was two days (IQR 1–5), while there was only a median of one day (IQR 0–4) from the first chaplain encounter to the time of ICU death or discharge. Chaplain visits were most frequently requested by families (19%), chaplains initiated (17%), or nurses (15%). Fewer chaplain visits (4%) were requested by physicians. Following an encounter with a patient or family, chaplains most frequently discussed the encounter with nurses (57%). Chaplains documented speaking with the physician after only 6% of these encounters. There was no documentation of communication with a health care provider after 22% of encounters (Table 4).
Table 4.
Other Clinically Relevant Outcomes of Patients Seen by Chaplains, n=248a
| Characteristic | |
|---|---|
| Days from ICU admit to 1st chaplain note | 2 (1,5) |
|
| |
| Days from 1st chaplain note to ICU death or discharge | 1 (0,4) |
|
| |
| Consults Requested by: | |
| Family | 46 (19) |
| Chaplain Initiated | 43 (17) |
| Nurse | 38 (15) |
| Interdisciplinary Team | 29 (12) |
| Patient | 13 (5) |
| Physician | 10 (4) |
| Code Blue | 10 (4) |
| No Documentation | 37 (15) |
| Other | 22 (9) |
|
| |
| Encounter discussed with: | |
| Nurse | 141 (57) |
| Interdisciplinary Team | 20 (8) |
| Physician | 14 (6) |
| No Documentation | 55 (22) |
| Other | 18 (7) |
Shown as number (percent) or median (interquartile range)
Of 248 patients seen by chaplains, 115 (46%) had no follow-up visit. Eighty-one (32%) had just one follow-up visit, and of these patients with only one follow-up, 56 (69%) occurred at the time of death.
Discussion
This retrospective cross-sectional study at a tertiary academic medical center demonstrates the generally narrow scope within the institution of hospital chaplains’ involvement in the care of patients in the ICUs. We found that most patients seen by a chaplain in the ICU were intubated and died soon thereafter. Most of the chaplain encounters occurred in the last day or two of life, signifying that chaplain visits are generally being requested for patients who are actively dying rather than for the purpose of proactive spiritual support for families and patients. Involvement of chaplains in the ICU was generally infrequent, but it appears to become more frequent in patients who are more critically ill, and it becomes the norm for patients who are dying.
One study looking at satisfaction of families of patients who died in the ICU has shown that families are more satisfied with their overall care when spiritual support is provided within the last 24 hours of the patients’ life (15). There was also a strong correlation between satisfaction with spiritual care and overall satisfaction with the care that they received in the ICU. A study from the same group recently showed that specific activities of spiritual care providers, including discussion of end-of-life wishes and preparation for family meetings, were associated with greater levels of family satisfaction (23). Our study shows that this support of families within the last 24 hours of a patient’s life is most commonly the way that hospital chaplains are being incorporated into patient care in the ICU. While providing support for families is important, many of the patients who do not die (and, therefore, are unlikely to be seen by chaplains) will be severely debilitated following ICU discharge and may ultimately have spiritual needs that remain unmet. Just as ICU admissions may be a source of trauma for patients (24), spiritual crises also may be precipitated by ICU admission (1). In these cases, provision of spiritual support from a hospital chaplain may be useful in bringing about spiritual health in addition to physical and emotional health.
Our study also highlights a potentially troubling communication deficit between chaplains and physicians. Not only were chaplain visits rarely requested by physicians, but chaplains rarely communicated with physicians about their interactions with patients and families. An Australian study looking at chaplains and their interactions with physicians showed that 90% of chaplains believed it was an important part of their role to discuss cases with physicians (25). If medical teams aim to deliver multidisciplinary, holistic care that addresses the physical, emotional, and spiritual needs of patients, improving this communication between chaplains and physicians seems necessary (26). Additionally, it is possible that clinicians may be unaware of chaplains or unfamiliar with their clinical impact, may fail to value their clinical impact highly, or may intimidate them.
Our study has several limitations. First, it was a retrospective chart review from a single tertiary medical center, and as such, the findings may not reflect the experiences of patients in other hospitals. In addition, this study was performed in a more religious, predominantly Christian Protestant area of the country, so findings may not be generalizable to centers in less religious areas, with varying religious backgrounds (27). Moreover, while there are important observations that have come from this study, no clear causal relationships can be made based on this methodology. It is possible that chaplain visits were not requested when a patient’s own community religious leaders were involved—and we were not able to assess how often that was the case. The chaplain department in our institution relies heavily on interns and residents involved with clinical pastoral education (CPE) training. While it is unclear whether ICU clinicians understand the various roles of training within chaplaincy, there may be a possibility that ICU clinicians are more reluctant to request chaplain visits from less experienced chaplains. Centers with more full-time, board-certified chaplains may have differing practice patterns. In her book, Paging God, Wendy Cadge describes several different models for chaplain care in hospitals. Duke University Hospital’s chaplain department most resembles what she describes as a Transitional department, in which there is a mix of board-certified chaplains with chaplains in training. This model may differ from the Professional departments and Traditional departments that she describes (28). Finally, given the nature of chaplaincy care, and the relatively novel nature of chaplain documentation, there is some question as to whether all chaplain encounters were captured by this chart review. However, our senior chaplains have corroborated that all chaplains have been trained in chaplain documentation, even when patients and families are unavailable, so it is unlikely that there are patients who were seen by a chaplain with no documentation.
Despite these limitations, there are reasons to believe that our findings may be applicable to other centers. According to the Association of Professional Chaplains, there are only about 4000 registered chaplains throughout the country who are members of their organization (29). There are several other smaller chaplain organizations in the country, but total membership combined still does not exceed around 10,000 members (28). While this does not take into account all CPE students and volunteer chaplains, it does highlight the relative scarcity of chaplains throughout the country. In addition, Duke University Hospital has close connections with Duke Divinity School as a source of CPE students. Many academic medical centers may not have as robust a program if there is no local theological training institution.
This study highlights several areas of improvement for spiritual care of patients and families in the ICU. First, given the general infrequency of chaplain visitation in the ICU, particularly for patients who survive critical illness, it seems crucial to develop clinical triggers that may prompt a chaplain visit request by either a nurse or physician that would be in line with best practices for chaplain care (30). While the volume of patients and the relatively small number of chaplains may preclude all patients from being seen, having clinical triggers such as prolonged mechanical ventilation that might suggest high likelihood of spiritual or existential crisis, would be a way of ensuring that greater levels of spiritual support are provided in the ICU. In addition, further work needs to be done regarding communication patterns between physicians and chaplains. It is unclear whether physicians truly understand the important care that chaplains provide in the ICU. Beginning with education regarding not only the importance of the provision of spiritual care, but also the specific role of hospital chaplaincy may be an important area of intervention for ICU clinicians. Also, working with the chaplaincy department and the various ICUs to create a more integrated, interdisciplinary approach, would improve communication patterns between chaplains and physicians, thereby more closely adhering to chaplain best practices.
In summary, this study is one of the first to describe the process of hospital chaplain visitation in ICUs. We found that hospital chaplains are uncommonly consulted in ICUs, and when they are consulted, it is generally to see patients who are actively dying. Chaplains appear to rarely communicate with physicians about their interactions with patients and families. Future study is needed to understand how best to meet ICU patients’ and families’ spiritual needs and to engage chaplains in multidisciplinary ICU care proactively—as well as how chaplains impact satisfaction and spiritual distress.
Acknowledgments
Funding for this study was provided by 5T32HL007538-30.
The authors thank Jim Rawlings, Director of Pastoral Services, and Annette Olsen, Senior Chaplain, for their input at various stages of this project.
Footnotes
Disclosures
The authors declare no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gaeta S, Price KJ. End-of-life issues in critically ill cancer patients. Crit Care Clin. 2010;26:219–227. doi: 10.1016/j.ccc.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Angus DC, Barnato AE, Linde-Zwirble WT, et al. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004;32:638–643. doi: 10.1097/01.ccm.0000114816.62331.08. [DOI] [PubMed] [Google Scholar]
- 3.Steinhauser KE, Christakis NA, Clipp EC, et al. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284:2476–2582. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]
- 4.Balboni TA, Vanderwerker LC, Block SD, et al. Religiousness and spiritual support among advanced cancer patients and associations with end-of-life treatment preferences and quality of life. J Clin Oncol. 2007;25:555–560. doi: 10.1200/JCO.2006.07.9046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maciejewski PK, Phelps AC, Kacel EL, et al. Religious coping and behavioral disengagement: opposing influences on advance care planning and receipt of intensive care near death. Psychooncology. 2012;21:714–723. doi: 10.1002/pon.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Phelps AC, Maciejewski PK, Nilsson M, et al. Religious coping and use of intensive life-prolonging care near death in patients with advanced cancer. JAMA. 2009;301:1140–1147. doi: 10.1001/jama.2009.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Astrow AB, Wexler A, Texeira K, et al. Is failure to meet spiritual needs associated with cancer patients’ perceptions of quality of care and their satisfaction with care? J Clin Oncol. 2007;25:5753–5757. doi: 10.1200/JCO.2007.12.4362. [DOI] [PubMed] [Google Scholar]
- 8.Williams JA, Meltzer D, Arora V, et al. Attention to inpatients’ religious and spiritual concerns: predictors and association with patient satisfaction. J Gen Intern Med. 2011;26:1265–1271. doi: 10.1007/s11606-011-1781-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balboni TA, Paulk ME, Balboni MJ, et al. Provision of spiritual care to patients with advanced cancer: associations with medical care and quality of life near death. J Clin Oncol. 2010;28:445–452. doi: 10.1200/JCO.2009.24.8005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Balboni T, Balboni M, Paulk ME, et al. Support of cancer patients’ spiritual needs and associations with medical care costs at the end of life. Cancer. 2011;117:5383–5391. doi: 10.1002/cncr.26221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flannelly KJ, Emanuel LL, Handzo GF, et al. A national study of chaplaincy services and end-of-life outcomes. BMC Palliat Care. 2012;11:10. doi: 10.1186/1472-684X-11-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Angus DC. Charting (and publishing) the boundaries of critical illness. Am J Respir Crit Care Med. 2005;171:938–939. doi: 10.1164/rccm.2502002. [DOI] [PubMed] [Google Scholar]
- 13.Sulmasy DP. Spirituality, religion, and clinical care. Chest. 2009;135:1634–1642. doi: 10.1378/chest.08-2241. [DOI] [PubMed] [Google Scholar]
- 14.Davidson JE, Powers K, Hedayat KM, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004–2005. Crit Care Med. 2007;35:605–622. doi: 10.1097/01.CCM.0000254067.14607.EB. [DOI] [PubMed] [Google Scholar]
- 15.Wall RJ, Engelberg RA, Gries CJ, et al. Spiritual care of families in the intensive care unit. Crit Care Med. 2007;35:1084–1090. doi: 10.1097/01.CCM.0000259382.36414.06. [DOI] [PubMed] [Google Scholar]
- 16.Sloan RP, Bagiella E, Powell T. Religion, spirituality, and medicine. Lancet. 1999;353:664–667. doi: 10.1016/s0140-6736(98)07376-0. [DOI] [PubMed] [Google Scholar]
- 17.Ford DW, Downey L, Engelberg R, et al. Discussing religion and spirituality is an advanced communication skill: an exploratory structural equation model of physician trainee self-ratings. J Palliat Med. 2012;15:63–70. doi: 10.1089/jpm.2011.0168. [DOI] [PubMed] [Google Scholar]
- 18.Carey LB, Cohen, Jeffrey Religion, spirituality and health care treatment decision: the role of chaplains in the Australian clinical context. J Health Care Chaplain. 2009;15:25–39. doi: 10.1080/08854720802698491. [DOI] [PubMed] [Google Scholar]
- 19.Carey LB. Bioethical issues and health care chaplaincy in Aotearoa, New Zealand. J Relig Health. 2012;51:323–335. doi: 10.1007/s10943-010-9368-1. [DOI] [PubMed] [Google Scholar]
- 20.Carey LB, Newell CJ, Rumbold B. Pain control and chaplaincy in Australia. J Pain Symptom Manage. 2006;32:589–601. doi: 10.1016/j.jpainsymman.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 21.Piderman KM, Marek DV, Jenkins SM, et al. Predicting patients’ expectations of hospital chaplains: a multisite survey. Mayo Clin Proc. 2010;85:1002–1010. doi: 10.4065/mcp.2010.0168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferreira FL, Bota DP, Bross A, et al. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286:1754–1758. doi: 10.1001/jama.286.14.1754. [DOI] [PubMed] [Google Scholar]
- 23.Johnson JR, Engelberg RA, Nielsen EL, et al. The association of spiritual care providers’ activities with family members’ satisfaction with care after a death in the ICU. Crit Care Med. 2014;42:1991–2000. doi: 10.1097/CCM.0000000000000412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davydow DS, Gifford JM, Desai SV, et al. Posttraumatic stress disorder in general intensive care unit survivors: a systematic review. Gen Hosp Psychiatry. 2008;30:421–434. doi: 10.1016/j.genhosppsych.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carey LB, Cohen, Jeffrey Chaplain-physician consultancy: when chaplains and doctors meet in the clinical context. J Relig Health. 2009;48:353–367. doi: 10.1007/s10943-008-9206-x. [DOI] [PubMed] [Google Scholar]
- 26.Lo B, Ruston D, Kates LW, et al. Discussing religious and spiritual issues at the end of life: a practical guide for physicians. JAMA. 2002;287:749–754. doi: 10.1001/jama.287.6.749. [DOI] [PubMed] [Google Scholar]
- 27.Pew Research Religion and Public Life Project. [Accessed September 18, 2014]; Available at: www.pewforum.org.
- 28.Cadge W. Religion in the halls of medicine. Chicago: Unveristy of Chicago Press; 2012. Paging God. [Google Scholar]
- 29.Association of Professional Chaplains. [Accessed September 18, 2014];2012–2013 Annual Report. Available at: http://www.professionalchaplains.org/content.asp?pl=24&contentid=24.
- 30.Handzo GF. Best practices in professional pastoral care. South Med J. 2006;99:663–664. doi: 10.1097/01.smj.0000222481.70129.7d. [DOI] [PubMed] [Google Scholar]