Abstract
Sexual and reproductive health is important quality of life outcomes, which can have a major impact on patient satisfaction. Spinal pathology arising from trauma, deformity, and degenerative disease processes may be detrimental to sexual and reproductive function. Furthermore, spine surgery may impact sexual and reproductive function due to post-surgical mechanical, neurologic, and psychological factors. The aim of this paper is to provide a concise evidence-based review on the impact that spine surgery and pathology can have on sexual and reproductive function. A review of published literature regarding sexual and reproductive function in spinal injury and spinal surgery patients was performed. We have found that sexual and reproductive dysfunction can occur due to numerous etiological factors associated with spinal pathology. Numerous treatment options are available for those patients, depending on the degree of dysfunction. Spine surgeons and non-operative healthcare providers should be aware of the issues surrounding sexual and reproductive function as related to spine pathology and spine surgery. It is important for spine surgeons to educate their patients on the operative risks that spine surgery encompasses with regard to sexual dysfunction, although current data examining these topics largely consists of level IV data.
Key words: Spine surgery, spine trauma, sexual function, sexual health, spinal cord injury
Introduction
Sexual and reproductive function are important factors contributing to quality of life in many patients.1 Spine pathology can have negative impacts on sexual and reproductive function.2,3 The effects of spinal cord injury, which has a prevalence of 906 per million in the United States, are particularly profound.4 In a study examining spinal cord injury (SCI) subjects with a median of 2 years post-injury, the authors found that higher levels of sexual djustment, measured using the Sexual Interest and Satisfaction Scale (SIS), were positively correlated with higher quality of life (QL) scores using a visual analogue scale (VAS) (r=0.52, P<0.001).5 Kreuter et al. also reported a positive correlation between sexual adjustment (SAS scale) and quality of life using VAS (r=0.39, P<0.01).6 In a survey of 681 SCI men and women, 13% of quadriplegics ranked sexual function as the highest priority to improve quality of life, with 26.7% of paraplegics ranking it the highest.1
There are many methods of assessing outcomes after injury, including the: ASIA Impairment Scale (AIS),7 the International Standards to document remaining Autonomic Function after Spinal Cord Injury (ISAFSCI),8 the Lumbar Stiffness Disability Index (LSDI),9 the Oswestry Disability Index (ODI).10 While some of these tools specifically address sexual function, others address more general global functioning with additional assessment of sexual function. The purpose of this review is to provide a concise, evidence-based review examining the impact that spine trauma and spine surgery can have on sexual and reproductive function, and to review the available diagnostic and treatment modalities, which exist.
Anatomy: science of erection and ejaculation
The penis is comprised of erectile and nonerectile tissue. The internal pudendal artery supplies erectile tissue, comprised of the corpus spongiosum and two corpora cavernosa. Dilation of arterioles supplying the erectile tissue causes blood to flow into the expanding empty spaces, expanding and constricting draining veins against the surrounding tunica albuginea.11 Innervation consists of parasympathetic, sympathetic, and somatic fibers from the sacral segments S2-S4 nerve roots. The pelvic nerves provide autonomic function where as the pudendal nerves are responsible for somatic function. The hypogastric nerves also provide innervation and originate in the thoracic-lumbar (TL) segments T11-L2.2 Ejaculation occurs in two phases: emission and expulsion. Emission (introduction of spermatozoa to the posterior urethra) is controlled by sympathetic and parasympathetic innervation from the pelvic plexus. The expulsion phase consists of rhythmic contraction of the bulbospongiosus and ischiocavernosus muscles along with relaxation of the external urethral sphincter, which are all somatically innervated by the pudendal nerve. The internal urethral sphincter is responsible for preventing retrograde ejaculation and has sympathetic and parasympathetic innervation. The exact triggering of expulsion is not entirely known, but is viewed as likely being a spinal reflex.12
Effects of spinal trauma on sexual and reproductive function
Spinal cord, cauda equina, and sacral root injury
Predicting and understanding sexual and reproductive function following SCI requires a sound understanding of spine trauma pathoanatomy. The neurological level of injury (NLI) is defined as the most caudal segment of the spinal cord with intact sensory and anti-gravity motor function on right and left sides of the body. Sensation and motor function rostral to that level must be intact. Sacral sparing refers to preservation of sensory and/or motor function at the S4-S5 sacral segments and is used to refer to an incomplete spinal cord injury; complete spinal cord injuries do not exhibit sacral sparing. A complete injury to the cauda equina is a lower motor neuron injury which may result in flaccid paralysis of the lower limb muscles, an areflexic bowel and bladder, and the bulbocavernosus reflex may be lost.7
Severity of injury: American Spinal Injury Association classification
The ASIA Impairment Scale (AIS) is used to describe the completeness or severity of SCI (Table 1).7 Kim et al. found no significant difference in AIS scores between those reporting sexual dysfunction and those reporting no difficulties with sexual dysfunction. Although the American Spinal Injury Association (ASIA) impairment scale helps to classify the extent of neurological injury, it does not provide any information regarding sexual function.13
Table 1.
The American Spinal Injury Association Impairment Scale.
| Grade | Description |
|---|---|
| A | Complete. No sensory or motor function is preserved in the sacral segments S4-S5. |
| B | Sensory incomplete. Sensory but not motor function is preserved below the neurological level and includes the sacral segments S4-S5, AND no motor function is preserved more than three levels below the motor level on either side of the body. |
| C | Motor incomplete. Motor function is preserved below the neurological level,* and more than half of key muscle functions below the single neurological level of injury have a muscle grade less than 3 (Grades 0-2). |
| D | Motor incomplete. Motor function is preserved below the neurological level,* and at least half (half or more) of key muscle functions below the NLI have a muscle grade >3. |
| E | Normal. If sensation and motor function as tested with the ISNCSCI are graded as normal in all segments, and the patient had prior deficits, then the AIS grade is E. Someone without a SCI does not receive an AIS grade. |
* For an individual to receive a grade of C or D, i.e. motor incomplete status, they must have either (1) voluntary anal sphincter contraction or (2) sacral sensory sparing (at S4/5 or DAP) with sparing of motor function more than three levels below the motor level for that side of the body. The Standards at this time allows even non-key muscle function more than 3 levels below the motor level to be used in determining motor incomplete status (AIS B versus C).
Severity of injury: International Standards to document remaining Autonomic Function after Spinal Cord Injury
The ASIA and the International Spinal Cord Society (ISCoS) have developed an assessment to document the autonomic functioning in an individual after spinal cord injury called the International Standards to document remaining Autonomic Function after Spinal Cord Injury (ISAFSCI).8 The assessment form includes scoring on sexual function (Figure 1).
Figure 1.
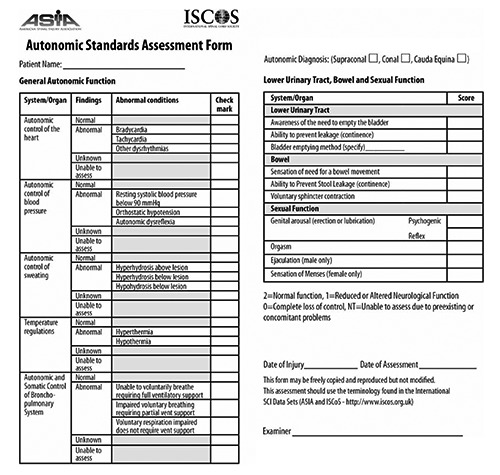
International Standards to document remaining Autonomic Function after Spinal Cord Injury assessment.
Erection
Erectile function depends on the level of injury in SCI men. Both sacral segments and thoracic-lumbar segments modulate erectile function. In a study of 71 SCI men,2 100% of the men retained reflexogenic erections when the complete lesion was above the sacral segments. Subjects with injury to the conus medularis and cauda equina were able to generate erections using psychogenic and reflexogenic stimuli in 90% and 80% of cases, respectively. The production of reflexogenic erections in this group is likely due to the fact that lesions to the conus medularis or cauda equina are often partial in nature. A limitation of this study was the definition of erection as an increase in penile circumference of at least 3 mm with no definition of rigidity necessary for penetrative intercourse.2 Lesions below T11 generally only allow filling of the corpora cavernosa via reflexogenic erections, while lesions above T11 will allow filling of both the corpora cavernosa and the corpus spongiosum.14
Ejaculation
In the study by Courtois et al., men with lumbosacral spinal cord injuries sparing the upper lumbar and thoracic segments were able to maintain ejaculation; however, this was generally immediately after tumescence.2
Sexual function: data on outcomes and satisfaction
Numerous investigations have examined sexual satisfaction after SCI. Kreuter et al. showed that 61% of SCI patients were satisfied with their sex life, compared to 86% of the controls (without SCI) expressing satisfaction (P<0.001).6 Additionally, there may not be an association between sexual satisfaction and decubitus ulcers (P=0.073).15 A retrospective study showed a correlation between younger age at injury and more satisfaction with sexual life after injury in SCI men and women (P<0.001).5 Kreuter et al. demonstrated the importance of psychological factors in sexual adjustment after spinal cord injury. They found that partner satisfaction with sex and satisfaction with the patient’s sexual adequacy, both as perceived by the patient were strongly correlated with sexual adjustment after SCI (r=0.86 and 0.89 respectively, P<0.001).6
Male-specific outcome data
A study examining outcomes at least 10 years post SCI-injury in 193 men found that 75% reported achieving an erection, with 39% of those reporting deliberate erections, 44% reported spontaneous erections, and 17% reported both. Of this study population, 65% reported the erection as hard/normal. Overall, 44% achieved ejaculation, 56% of those had used an ejaculatory aid. Those reporting ejaculation were significantly younger (mean 46 years versus 54 years) than those who reported inability to ejaculate (P<0.0001).16
Another investigation examining erection in SCI men found that the percent of men achieving erection varied with type of injury: complete upper motor neuron lesion, incomplete upper motor neuron, complete lower motor neuron, incomplete lower motor neuron lesions achieving 93%, 99%, 26%, 90% rates of erection respectively.14
Men are less satisfied with sex life than women following SCI.16 Sexual satisfaction has been shown to decrease with age in traumatic SCI men (P<0.001). Lower sexual satisfaction was found in men whom injury occurred at an older age (P=0.001).15 Cervical injury level was associated with higher levels of sexual satisfaction than lower injuries (P=0.030)15 and men with upper motor neuron injuries tend to have more frequent erections. Neuropathic pain and fecal incontinence led to sexual dissatisfaction in men (P=0.006, P=0.002, respectively).15
In another cross-sectional survey of 193 men with traumatic SCI, no statistically significant difference in sex life satisfaction between quadriplegic and paraplegic men was found (P=0.5). They also found that sex life satisfaction and age were not correlated, contrary to the study by Valtonen. They also reported a trend toward more sex life satisfaction if ejaculation was possible, although this relationship was not statistically significant (P=0.13). No statistically significant difference between satisfaction with sex life and problems with incontinence, pressure ulcers, spasticity, or pain were reported in this study (P=0.12).16
Females-specific outcome data
A cross-sectional survey of 472 women with SCI found that the percentage of women reporting sexual intercourse increased with years after injury. In total, 87% reported intercourse before injury, compared to 49% at 1-year post injury, 65% at 2 to 10 years post injury, and 76% at 11+ years post injury (P<0.001). Females with injury to the thoracic spinal cord reported a statistically significant decrease in sexual intercourse frequency after injury (P<0.05). Completeness of injury was not found to associate with frequency of sexual intercourse (P>0.05). Eleven point four percent of women reported autonomic dysreflexia associated with sex after injury. Cervical spine injury was most strongly associated with autonomic dysreflexia (P<0.01). Bladder incontinence was reported by 12% of the cervical spine injured patients, 21.9% of the thoracic spine injured patients, and 7.1% of the lumbar/sacral spine injured patients (P<0.05).17
In Jackson and Wadley’s study, only 37.3% of females reported they were able to achieve orgasm after injury compared to 79.1% before injury (P<0.0001). The study displayed that increasing number of years post injury, lower level of injury, and incomplete of injuries correlate with a greater chance to achieve an orgasm (P<0.0001, P<0.05, and P<0.05, respectively).17 Valtonen et al. found that urinary and fecal incontinence in addition to spasticity were the most common concerns of sexually active women following traumatic SCI.15 Valtonen et al.15 and Biering-Sørensen et al.16 found mixed results regarding level of injury and sexual satisfaction in women and mixed results regarding age at injury and sexual satisfaction.
Reproduction following spinal cord injury
Following SCI, some women are able to become pregnant and successfully bear children,17 although pregnancy in SCI women carries several risks. There was a statistically significant increase in diabetes and UTIs during pregnancy postinjury compared to preinjury (P<0.05). Pregnancy was also associated with higher rates of disability-related complications, including higher rates of autonomic dysreflexia, pressure ulcers, worsening spasticity, leakage around indwelling catheters, catheter expulsion due to spasm, and more frequent catheterization. Overall, 75% of SCI women who became pregnant complained of pregnancy complications compared to 49.8% of non-SCI pregnant women (P<0.05). Labor symptomatology can range from normal uterine contractions, pain, and rupture of membranes to pain above injury level, increased spasticity, autonomic dysreflexia, and bladder spasms. SCI women had lower rates of spontaneous vaginal delivery (48% vs 62%) and required more frequent use of C-sections (17.8% vs 8.3%) or forceps/vacuum extraction (13.9% vs 6.9%). Higher rates of labor and delivery complications were also noted, including: blood pressure instability (22.7% vs 5.3%, P<0.05) and prematurity (21.2% vs 12.6%, P=0.07). SCI women did however have higher rates of delivering without anesthesia (50% vs 23.9%, P<0.05). Among babies not born prematurely, those from SCI mothers were more likely to have low birth weight (less than 5 lbs 6 oz) (13.6% vs 4.5%, P<0.05). The babies were also less likely to be breastfed (11% vs 28%, P<0.05).17 In a survey of 188 SCI men, 81% had not made a woman pregnant after injury, with 34% of those saying the problem was due to the spinal cord injury and 22% responding with no answer. Of the men reporting pregnancy with a partner, 100% could achieve an erection and 89% ejaculation. Of the men reporting no pregnancy in a partner, 71% could achieve an erection and 34% ejaculation (P=0.0005 and P<0.0001 respectively).16
Spinal deformity and degenerative disease
Mechanical factors
Pathology of the spine other than SCI can also affect sexual and reproductive function. Berg et al. demonstrated a significant increase in sex life quality (P<0.001) after lumbar fusion surgery or total disc replacement. The improvement in sex life quality was most closely correlated with decreased back pain (r=0.71).10
Spinal stiffness: lumbar stiffness disability index
The Lumbar Stiffness Disability Index (LSDI) is a questionnaire designed to assess impairment in performing ADLs after spinal arthrodesis with scores on each of the 10 questions ranging from 0 (No effect at all) to 4 (Cannot do at all). The tenth question is Engage in sexual intercourse. Scores range from 0 to 40 with the final score being computed as (raw score)/40×100. Higher scores correspond with more impairment. Patients with fusion of five or more spinal levels had a significantly higher LSDI score than patients with one-level fusion (35.4 vs 24.2, P=0.05). The total LSDI scores did not vary significantly for thoracolumbar fusions versus upper thoracic (P=0.50).9 Hart et al. reported a significant decrease in disability associated with stiffness in patients receiving 1-level arthrodesis (P=0.012). Patients receiving 5 or more level arthrodesis reported an increase in disability associated with stiffness; however, not to a significant level (P=0.055).18
Physiological effects of spinal surgery
Anterior lumbar spine surgery: transperitoneal vs extraperitoneal approach
Retrograde ejaculation (RE) is associated with anterior lumbar spine surgery, and is a phenomenon caused by failure of the internal urethral sphincter to close. This failure causes ejaculate to enter the bladder potentially causing subfertility.19 In a multicenter, prospective 2-year study involving anterior lumbar discectomy and interbody fusion, retrograde ejaculation was noted in 1.7% of the group receiving the retroperitoneal approach and 13.3% of men receiving the transperitoneal approach with a statistically significant difference (P=0.017). The condition resolved by 12 months in one third of those affected, and there was no difference in recovery based on approach. The authors hypothesized that the difference in incidence of RE between the groups was due to surgical technique; the superior hypogastric plexus is protected by peritoneum during the retroperitoneal approach, whereas the plexus is dissected in the transperitoneal approach,20 however the patients were not randomized in this study.
Recombinant human bone morphogenetic protein 2 (rhBMP-2)
There has been debate as to whether the use of rhBMP-2 during anterior lumbar interbody fusion (ALIF) at the L4-L5 or L5-S1 level increases the risk of retrograde ejaculation (RE). An analysis of 5 prospective, randomized trials showed a higher incidence of RE with the use of rhBMP-2 (3.4% vs. 1.7%) but there was no statistical significance (P=0.242, Fisher exact test).21 A retrospective analysis of 69 ALIFs with rhBMP-2 versus 174 ALIFs without rhBMP-2 found higher rates of RE (7.2%) in the rhBMP-2 group versus 0.6% in the non-rhBMP-2 group (P=0.0025).22 Of note, half of those who developed RE recovered by one year. A retrospective chart review of 95 men with L5-S1 level surgery found no statistically significant difference in the rate of RE between those surgeries using ALIF and rhBMP-2 and ADR (artificial disc replacement). Both types of surgery were done using an anterior, retroperitoneal approach. RE rates were 7.4% in the ALIF with rhBMP-2 group and 9.8% in the ADR group (P=0.7226), with recovery of function in only one quarter of patients. This study did not compare patients using ALIF without rhBMP-2, but the authors argue that the ADR group was a suitable replacement because the anterior midline surgical exposure is the same for both groups. Of note, patients in the ALIF group were significantly older (49 vs. 35, P<0.001), and a higher percentage (97.6%) of patients in the ADR group had degenerative disc disease as the primary indication versus 72.2% of patients in the ALIF group (P<0.001).23 A prospective study examining the incidence of RE after ALIF compared the rates of RE using a questionnaire versus quantitative testing using postejaculatory urine analysis and concluded that RE was overestimated when a questionnaire was used versus laboratory analysis (41.7% vs 9.5%). Additionally, the study did not show a statistical difference in RE rates between the group receiving rhBMP-2 and the group not receiving rhBMP-2 (P>0.80).24 Importantly, these studies have also not assessed stand alone cage ALIF versus anterior plate with cage constructs, which could potentially affect the rates of RE.
A 10-year follow-up cohort-controlled study demonstrated a statistically significant (P=0.0012) higher incidence of RE in patients with exposure to rhBMP-2 (6.3%) versus those patients without exposure (0.9%).25 Unfortunately, many of the studies examining the effect of rhBMP-2 use on RE employed questionnaires without laboratory testing for RE, thus placing their results into question. Due to conflicting results from numerous studies, Mroz et al.,26 Siemionow et al.,27 Tannoury et al.,28 as well the authors of this review believe that the matter of whether rhBMP-2 use is an independent risk factor for RE is still up for debate without a proven definitive causative effect.
Experience of approach surgeon
General surgeons or vascular surgeons have been used to provide surgical exposure during anterior lumbar surgery. A study by Smith et al. showed statistically lower values of estimated blood loss, operative time, and hospital stay time (P=0.0007, P=0.0003, P=0.0006, respectively) when the approach is performed by general or vascular surgeons. Retrograde ejaculation in two patients was a complication only of the group using an access surgeon.29
Total disc replacement vs anterior lumbar interbody fusion vs posterior lumbar interbody fusion
A randomized controlled trial comparing total disc replacement (TDR) to posterior lumbar interbody fusion (PLIF) using the ODI (Oswestry Disability Index) item 8, Table 2,30 found a significant increase in sex life quality (P<0.001) when either method was used with this improvement in sex life quality most correlated with decreased back pain (r=0.71).10
Table 2.
The Oswestry Disability Index item 8.
| Statement | Corresponding score |
|---|---|
| My sex life is normal and causes no extra pain. | 0 |
| My sex life is normal but causes some extra pain. | 1 |
| My sex life is nearly normal but is very painful. | 2 |
| My sex life is severely restricted by pain. | 3 |
| My sex life is nearly absent because of pain. | 4 |
| Pain prevents any sex life at all | 5 |
For each ODI item, a statement is picked and the corresponding score is given.30
Interventions: a guide to early management and appropriate referral
Medications
Early interventions may help maximize sexual and reproductive function in spinal cord injury patients. Intracorporeal (IC) therapy is an important option to assist SCI men to achieve erection. Intracorporeal therapy often includes using papaverine – direct smooth muscle inhibition – and phentolamine – alpha-adrenergic blocker leading to smooth muscle relaxation and prostaglandin E1. Many studies have supported the efficacy of these IC medications,31,32 but complications such as bleeding at the injection site and scaring of the tunica albuginea causing curvature may prohibit their use.31 The release of sildenafil in 1998 made oral therapy an option. Sildenafil works by blocking phosphodiesterase 5 leading to slower catabolism of cGMP. A prospective study examining 41 SCI patients identified 93% of patients as having penile rigidity adequate for sexual intercourse and a statistically significant increase in erectile function and intercourse satisfaction using the International Index of Erectile Function (IIEF) questionnaire after using sildenafil (P<0.05). Patients had to have an intact sacral spinal reflex segment leading to reflexive erections caused by direct somesthetic stimulation. Patients could also have psychogenic erections caused by extrinsic visual, auditory, chemosensory input or erotic thoughts. They found no significant improvement in orgasm or ejaculatory function.33
Psychosocial therapy
The Consortium for Spinal Cord Medicine clinical practice guidelines state that sexual education in spinal cord injury patients should focus not only about the mechanics and practicalities of sexual activity, but also integrate a person’s personal needs, questions, life views, and life context as these relate to sexuality. Sexuality should be understood in the context of a person’s life rather than as a separate and distinct entity.34 A questionnaire of 190 SCI individuals found sufficient levels of sexual counseling resulted in higher sex life satisfaction (Mann-Whitney, P=0.004).15 It is a valuable adjunct to the various other forms of treatment.
Physical aids
Vacuum erection devices (VED) uses vacuum to cause corporal filling. A cost-utility analysis deemed VED an acceptable and appropriate solution to a challenging problem.35 A series of cases looking at 20 SCI men found that at 6 months 60% of men and 42% of their female partners found that the device had improved their sexual relationship. Petechiae and penile skin edema were reported as the most frequent complications.36 In spinal cord injured men who cannot ejaculate, penile vibratory stimulation (PVS) or rectal probe electroejaculation (EEJ) can be used to induce ejaculation. PVS is considered the less invasive of the two methods and results in higher semen quality.37 A more cranial level of injury is correlated with a higher success rate of PVS. The highest rate of ejaculation was obtained using a 2.5 mm amplitude vibrator.38 In patients not responding to PVS, the 1-adrenergic agonist midodrine was shown to help 64.6% of the 102 SCI men achieve antegrade or retrograde ejaculation. Better responses were seen in patients with complete (ASIA A) UMN lesions above T10.39
Surgical intervention
Surgically implanted prosthetic devices are also an option for SCI patients, especially those who have failed pharmacological and mechanical treatment. The devices are often rigid, semi-rigid, or inflatable penile implants. Common risks include colonization and infection of the device.40 The implants can also be useful for fitting urinary condoms and a study in 37 SCI men showed 41% of patients reporting benefit to their marital life.41
Summary
Sexual and reproductive health are important factors which can affect the quality of life of patients suffering from spinal cord injury. A sound understanding of pathogenesis, common impairments, and treatment of sexual and reproductive issues associated with SCI can help spine practitioners counsel, treat, and refer their patients. Several effective psychological, pharmacological, surgical, and mechanical treatments are available for patients with SCI-related sexual dysfunction. Importantly, most of the available literature on the sexual and reproductive complications of spinal injury and spine surgery is low level evidence, most commonly level III or level IV studies, thus further research is required to refine our understanding of these problems.
References
- 1.Anderson KD. Targeting recovery: priorities of the spinal cord-injured population. J Neurotrauma 2004;21:1371-83. [DOI] [PubMed] [Google Scholar]
- 2.Courtois FJ, Charvier KF, Leriche A, Raymond DP. Sexual function in spinal cord injury men. I. Assessing sexual capability. Paraplegia 1993;31:771-84. [DOI] [PubMed] [Google Scholar]
- 3.Kreuter M, Taft C, Siösteen A, Biering-Sørensen F. Women’s sexual functioning and sex life after spinal cord injury. Spinal Cord 2010;49:154-60. [DOI] [PubMed] [Google Scholar]
- 4.Singh A, Tetreault L, Kalsi-Ryan S, et al. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol 2014;6:309-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siösteen A, Lundqvist C, Blomstrand C, et al. Sexual ability, activity, attitudes and satisfaction as part of adjustment in spinal cord-injured subjects. Paraplegia 1990;28:285-95. [DOI] [PubMed] [Google Scholar]
- 6.Kreuter M, Sullivan M, Siösteen A. Sexual adjustment and quality of relationships in spinal paraplegia: a controlled study. Arch Phys Med Rehabil 1996;77:541-8. [DOI] [PubMed] [Google Scholar]
- 7.Kirshblum SC, Burns SP, Biering-Sorensen F, et al. International standards for neurological classification of spinal cord injury (Revised 2011). J Spinal Cord Med 2011;34:535-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krassioukov A, Biering-Sørensen F, Donovan W, et al. International standards to document remaining autonomic function after spinal cord injury. J Spinal Cord Med 2012;35:201-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hart RA, Pro SL, Gundle KR, Marshall LM. Lumbar stiffness as a collateral outcome of spinal arthrodesis: a preliminary clinical study. Spine J 2013;13:150-6. [DOI] [PubMed] [Google Scholar]
- 10.Berg S, Fritzell P, Tropp H. Sex life and sexual function in men and women before and after total disc replacement compared with posterior lumbar fusion. Spine J 2009;9:987-94. [DOI] [PubMed] [Google Scholar]
- 11.Andersson KE, Wagner G. Physiology of penile erection. Physiol Rev 1995;75:191. [DOI] [PubMed] [Google Scholar]
- 12.Giuliano F, Clément P. Physiology of ejaculation: emphasis on serotonergic control. Eur Urol 2005;48:408-17. [DOI] [PubMed] [Google Scholar]
- 13.Kim HS, Kim NH, Lee HM, et al. Sexual dysfunction in men with paraparesis in lumbar burst fractures. Spine 2000;25:2187-90. [DOI] [PubMed] [Google Scholar]
- 14.Biering-Sørensen F, Sønksen J. Penile erection in men with spinal cord or cauda equina lesions. Semin Neurol 1992;12:98-105. [DOI] [PubMed] [Google Scholar]
- 15.Valtonen K, Karlsson AK, Siösteen A, et al. Satisfaction with sexual life among persons with traumatic spinal cord injury and meningomyelocele. Disabil Rehabil 2006;28:965-76. [DOI] [PubMed] [Google Scholar]
- 16.Biering-Sørensen I, Hansen RB, Biering-Sørensen F. Sexual function in a traumatic spinal cord injured population 10-45 years after injury. J Rehabil Med 2012;44:926-31. [DOI] [PubMed] [Google Scholar]
- 17.Jackson AB, Wadley V. A multicenter study of women’s self-reported reproductive health after spinal cord injury. Arch Phys Med Rehabil 1999;80:1420–8. [DOI] [PubMed] [Google Scholar]
- 18.Hart RA, Marshall LM, Hiratzka SL, et al. Functional limitations due to stiffness as a collateral impact of instrumented arthrodesis of the lumbar spine. Spine (Phila Pa 1976) 2014;39:E1468-74. [DOI] [PubMed] [Google Scholar]
- 19.Jefferys A, Siassakos D, Wardle P. The management of retrograde ejaculation: a systematic review and update. Fertil Steril 2012;97:306-12. [DOI] [PubMed] [Google Scholar]
- 20.Sasso RC, Burkus JK, LeHuec JC. Retrograde ejaculation after anterior lumbar interbody fusion: transperitoneal versus retroperitoneal exposure. Spine (Phila Pa 1976) 2003;28:1023-6. [DOI] [PubMed] [Google Scholar]
- 21.Burkus JK, Dryer RF, Peloza JH. Retrograde ejaculation following single-level anterior lumbar surgery with or without recombinant human bone morphogenetic protein-2 in 5 randomized controlled trials: clinical article. J Neurosurg Spine 2013;18:112-21. [DOI] [PubMed] [Google Scholar]
- 22.Carragee EJ, Mitsunaga KA, Hurwitz EL, Scuderi GJ. Retrograde ejaculation after anterior lumbar interbody fusion using rhBMP-2: a cohort controlled study. Spine J 2011;11:511-6. [DOI] [PubMed] [Google Scholar]
- 23.Lindley EM, McBeth ZL, Henry SE, et al. Retrograde ejaculation after anterior lumbar spine surgery. Spine (Phila Pa 1976) 2012;37:1785-9. [DOI] [PubMed] [Google Scholar]
- 24.Tepper G, Rabbani R, Yousefzadeh M, Prince D. Quantitative Assessment of retrograde ejaculation using semen analysis, comparison with a standardized qualitative questionnaire, and investigating the impact of rhBMP-2. Spine (Phila Pa 1976) 2013;38:841-5. [DOI] [PubMed] [Google Scholar]
- 25.Comer GC, Smith MW, Hurwitz EL, et al. Retrograde ejaculation after anterior lumbar interbody fusion with and without bone morphogenetic protein-2 augmentation: a 10-year cohort controlled study. Spine J 2012;12:881-90. [DOI] [PubMed] [Google Scholar]
- 26.Mroz TE, Abdullah KG, Benzel EC. Commentary: retrograde ejaculation and the use of rhBMP-2 for anterior lumbar interbody fusion: what does the evidence say to surgeons and to patients? Spine J 2012;12:891-3. [DOI] [PubMed] [Google Scholar]
- 27.Siemionow K, Sundberg E, Tyrakowski M, et al. Point-counter-point debate: the association between recombinant human bone morphogenetic protein utilization and complications in spine surgery. Curr Rev Musculoskelet Med 2014;7:200-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tannoury CA, An HS. Complications with the use of bone morphogenetic protein 2 (BMP-2) in spine surgery. Spine J 2014;14:552-9. [DOI] [PubMed] [Google Scholar]
- 29.Smith MW, Rahn KA, Shugart RM, et al. Comparison of perioperative parameters and complications observed in the anterior exposure of the lumbar spine by a spine surgeon with and without the assistance of an access surgeon. Spine J 2011;11:389-94. [DOI] [PubMed] [Google Scholar]
- 30.Fairbank JCT, Pynsent PB. The oswestry disability index. Spine 2000;25:2940-53 [DOI] [PubMed] [Google Scholar]
- 31.Watanabe T, Chancellor MB, Rivas DA, et al. Epidemiology of current treatment for sexual dysfunction in spinal cord injured men in the USA model spinal cord injury centers. J Spinal Cord Med 1996;19:186-9. [DOI] [PubMed] [Google Scholar]
- 32.Purvis K, Egdetveit I, Christiansen E. Intracavernosal therapy for erectile failure: impact of treatment and reasons for drop-out and dissatisfaction. Int J Impot Res 1999;11:287-99. [DOI] [PubMed] [Google Scholar]
- 33.Schmid DM, Schurch B, Hauri D. Sildenafil in the treatment of sexual dysfunction in spinal cord-injured male patients. Eur Urol 2000;38:184-93. [DOI] [PubMed] [Google Scholar]
- 34.Consortium for Spinal Cord Medicine. Sexuality and reproductive health in adults with spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med 2010;33:281-336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mittmann N, Craven B, Gordon M, et al. Erectile dysfunction in spinal cord injury: a cost-utility analysis. J Rehabil Med 2005;37:358-64. [DOI] [PubMed] [Google Scholar]
- 36.Denil J, Ohl DA, Smythe C. Vacuum erection device in spinal cord injured men: patient and partner satisfaction. Arch Phys Med Rehabil 1996;77:750-3. [DOI] [PubMed] [Google Scholar]
- 37.Brackett NL, Padron OF, Lynne CM. Semen Quality of spinal cord injured men is better when obtained by vibratory stimulation versus electroejaculation. J Urol 1997;157:151-7. [PubMed] [Google Scholar]
- 38.Brackett NL. Semen retrieval by penile vibratory stimulation in men with spinal cord injury. Hum Reprod Update 1999;5:216-22. [DOI] [PubMed] [Google Scholar]
- 39.Soler JM, Previnaire JG, Plante P, et al. Midodrine improves ejaculation in spinal cord injured men. J Urol 2007;178:2082-6. [DOI] [PubMed] [Google Scholar]
- 40.Gross AJ, Sauerwein DH, Kutzenberger J, Ringert RH. Penile prostheses in paraplegic men. Br J Urol 1996;78:262-4. [DOI] [PubMed] [Google Scholar]
- 41.Iwatsubo E, Tanaka M, Takahashi K, Akatsu T. Non-inflatable penile prosthesis for the management of urinary incontinence and sexual disability of patients with spinal cord injury. Paraplegia 1986;24:307-10. [DOI] [PubMed] [Google Scholar]


