Abstract
To investigate and monitor the progression of scoliosis and other spinal deformities in patients following idiopathic scoliosis (IS), non-invasive and radiation-free techniques are recommended because of the need for repeated radiographs. In a clinical setting, spine parameters can be quickly, cheaply and easily assessed using rasterstereography (RS). To assess the validity of the radiation-free technique RS based on surface topography compared with radiographs. MEDLINE, the Cochrane Library and EMBASE were systematically searched for studies which investigate the validity of rasterstereography compared with x-ray measurements. Studies published between January 1, 1990 and July 31, 2013 in English, German and French were included. Studies dealing with magnetic resonance imaging were excluded. Twelve studies with 570 patients were included; these articles were published between 1990 and 2013. The majority of studies investigated patients with IS, but other spinal pathologies included were thoracic hyperkyphosis and Scheuermann’s disease. With regard to the quality assessment criteria for the included studies, three out of twelve studies were evaluated using a twelve point scale and two used a scale with eleven points. We conclude that RS facilitates clinical practice by analysing the spinal column. It is completely radiation-free and could help to monitor scoliosis progression.
Key words: Scoliosis, spinal deformities, rasterstereography, surface topography, x-ray measurement
Introduction
Various subjective and objective methods have been developed to analyze and quantify scoliosis and other spinal deformities.1-5 To evaluate the degree of deformity in the diagnosis and treatment of scoliosis and other spinal deformities examinations such as roentgenograms or computed tomography are frequently used.4,6,7 The use of two-dimensional anterior-posterior (a.p.) full-length spine radiologic investigation is accepted as the mainstay to attest the medical diagnosis of idiopathic scoliosis, despite providing data only in two dimensions.8 The obvious disadvantage of such instrumental assessment method is the fear of increased carcinogenic risk and infertility from repeated exposure to ionizing radiation.9-12
The reason for the repeated radiographs is the requirement to measure the type, the flexibility and progression of the spinal curvatures in follow-up examinations in definite time intervals, which is obtained from two-dimensional a.p. spine radiographs.8 In the study of Nash and colleagues teenage girls with idiopathic scoliosis received over a treatment period of three years 22 roentgenograms.11 One alternative examination suitable for this purpose is the light-sectioning method rasterstereography (RS), which is a precise, radiation-free and inexpensive and that is in routine clinical use in many scoliosis centers throughout the world.13 The method, which was developed by Drerup and Hierholzer in the 1980s, has been confirmed to be reliable both in pre- and postsurgical scoliosis patients for supplementing radiological and clinical examinations.14-18 By detecting anatomical landmarks with characteristic shape parameters – the vertebra prominens and the two spina iliaca posterior superior – coordinate data of back surface points and the line of symmetry can be determined.19 RS provides a reliable method for three-dimensional back shape analysis and reconstruction of spinal deformities.20,21 Several studies have evaluated the validity of RS compared with X-ray.22-25 Therefore, the aim of the present research was to evaluate the validity and accuracy of RS compared with X-ray in a systematic literature review.
Inclusion criteria and study identification
A systematic review of the literature was conducted in July 2013 using the PubMed data base of the National Library of Medicine, Embase and the Cochrane library for relevant trials indexed between January 1, 1990, and July 31, 2013. To be included in the literature review, articles had to meet the following criteria: i) original studies that investigated the validity of RS compared with X-ray measurement and ii) published between January 1, 1990, and July 31, 2013, in the English, French or German language. The following search items were used: rasterstereography, rasterstereographic AND X-ray, rasterstereography OR rasterstereographic. Studies were also excluded if they lacked standard X-ray measurement of the spine, e.g. MR tomography or a lack of evaluation of spine parameters or if they analysis of difference in leg length or pelvic obliquity.
Those papers satisfying these criteria were retrieved and included in the review.
Data abstraction
An abstraction form was created. Data were extracted independently on the basis of their full text by one reviewer, and verified by a second. The reviewers were not blinded to the journal or the author’s name. The accuracy of the data abstraction was randomly confirmed in 10% of cases by the initial reviewer, as well as the second reviewer. The data abstraction form included: author’s name, year of publication, investigated parameters, study population, x-ray measurement, statistical methods, outcomes and the QUADAS tool.
Methodological quality assessment
The studies included in this review were independently appraised for quality by two authors using the 14-item QUADAS appraisal tool.26,27 It was developed to assess the diagnostic accuracy of primary diagnostic studies used in systematic reviews.26
Using this tool, two reviewers (MM and SS) independently assessed the methodological quality of each included paper. Any disagreement in respect of study eligibility, data extraction or methodological quality assessment was settled through discussion between the reviewers. If no agreement was reached, a third reviewer (AS) acted as an adjudicator to determine the consensus.
Study identification
An appropriate search strategy was constructed to ensure that all relevant trials published during the study period were identified (Table 1). A total of 62 citations were identified through the literature search. All full-text articles were assessed for eligibility. Twelve studies were included in the review after this procedure (Figure 1).22-25,28-34
Table 1.
Medline, Cochrane library and EMBASE were checked in July 2013 for appropriate material following the in- and exclusion criteria of this systematic review. The same keywords were used in all three databases.
| Keywords | Medline | Cochrane | EMBASE |
|---|---|---|---|
| Rasterstereography | 40 | 1 | 50 |
| Rasterstereography OR rasterstereographic | 46 | 1 | 51 |
| Rasterstereographic AND x-ray | 13 | 0 | 2 |
| Total | 99 | 2 | 103 |
Limits: publication date (1990-2013); “humans”; language (English, French. German).
Figure 1.
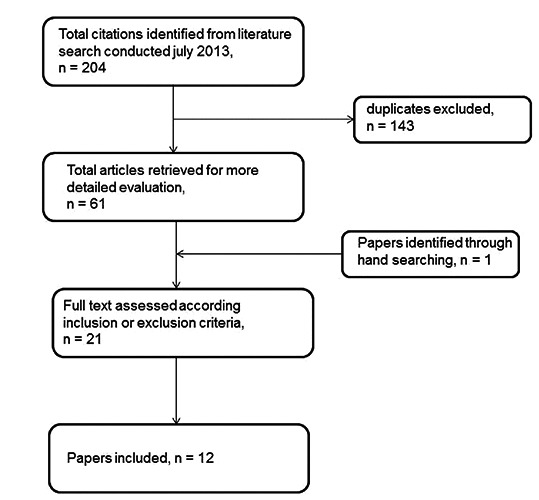
Flow of the studies through the systematic review.
Investigated parameters
The vertebral rotation was measured radiographically in nine studies out of the twelve investigated and compared with the rasterstereographic surface rotation respectively.14,15,22-25,28-40 The lateral deviation was the second most frequent parameter mentioned in three out of four studies by Hackenberg et al. with five mentions altogether.22-24 Kyphotic angle and lumbar lordosis were investigated triply. Torso overhang, apex height, lumbar scoliosis, thoracic scoliosis and pelvic position were recorded once each. Liljenqvist et al. investigated the highest number of parameters in their study (Table 2).25
Table 2.
Parameters investigated in the primary studies.
| Vertebral rotation - surface rotation | Cobb angle | Torso overhang | Pelvic balance | Lateral deviation of spine | Kyphosis angle | Lumbar lordosis angle | Thoracic scoliosis | Apex height | Lumbar scoliosis | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Drerup et al.34 | 1 | 1 | 1 | 1 | 4 | ||||||
| Liljenqvist et al.25 | 1 | 1 | 1 | 1 | 1 | 1 | 6 | ||||
| Hackenberg et al.30 | 1 | 1 | |||||||||
| Hackenberg et al.22 | 1 | 1 | 2 | ||||||||
| Hackenberg et al.23 | 1 | 1 | 2 | ||||||||
| Hackenberg et al.24 | 1 | 1 | 2 | ||||||||
| Schulte et al.29 | 1 | 1 | |||||||||
| Schulte et al.28 | 1 | 1 | 1 | 3 | |||||||
| Weiss et al.31 | 1a | 1 | |||||||||
| Crawford et al.40 | 1b | 1 | |||||||||
| Frerich et al.33 | 1 | 1 | 1 | 1 | 4 | ||||||
| Mangone et al.32 | 1c | 1 | |||||||||
| Total | 9 | 3 | 1 | 1 | 5 | 3 | 3 | 1 | 1 | 1 |
Study population
All studies investigated patients with spinal pathologies, e.g. idiopathic scoliosis (Table 3)14,15,22-25,28-40
Table 3.
Study population, X-ray measurement and statistical methods
| Study | Study population | X-ray measurement | Statistical methods 1 |
|---|---|---|---|
| Drerup et al.34 | 113 patients with Cobb angles below 52 degrees | Anterior-posterior radiographs | RMS, standard deviation |
| Liljenqvist et al.25 | 95 patients with idiopathic scoliosis or scoliotic posture and 18 patients with thoracic hyperkyphosis and Scheuermann’s disease | Anterior-posterior radiography in standing posture, vertebral rotation according to Perdriolle 197937 | RMS, mean |
| Hackenberg et al.30 | 31 patients with thoracic, thoracolumbar and lumbar idiopathic scoliosis | Anterior-posterior radiography in standing posture, sagital curvature according to Cobb 1948 andvertebral rotation according to Perdriolle 197937,39 | Wilcoxon sign rank test, mean, standard deviation, minimum, maximum |
| Hackenberg et al.22 | 25 patients with severe idiopathic scoliosis (Cobb angle of 57° on average) | Standard anterior-posterior radiographs were digitized according to Drerup14,15 | RMS |
| Hackenberg et al.23 | 52 patients with thoracic, thoracolumbar und lumbar idiopathic scoliosis | Anterior-posterior radiography in standing posture, digitized according to the method of Drerup14,15 | RMS |
| Hackenberg et al.24 | 25 patients with idiopathic scoliosis | Anterior-posterior radiography in relaxed standing posture, digitized according to the method of Drerup14,15 | RMS, range |
| Schulte et al.29 | 43 patients with idiopathic scoliosis | Digital radiometric rotation according to Drerup anterior-posterior radiographs, relaxed standing posture14,15 | Wilcoxon sign rank test, mean, median, minimum, maximum, standard deviation |
| Schulte et al.28 | 16 patients with idiopathic right convex scoliosis | Radiographs digitized in accordance with Drerup’s method14,15 | RMS, maximum, correlation coefficient r2 |
| Weiss et al.31 | 53 patients (26 with Scheuermann’s disease, 3 with thoracolumbar kyphosis, 15 with idiopathic kyphosis. 9 with kyphosis other origin) |
Lateral x-ray | Mean, standard deviation, Pearson correlation, t-test. |
| Crawford et al.40 | 10 patients prepared for lumbar spine surgery | Relaxed clavicle position with hands placed over ipsilateral clavicles, standardized erect lateral x-ray positioning guide, lordodic angle via the modified Cobb-method using the superior endplates of L1 and S1 for reference | Nonparametric correlation coefficient Spearman’s rho, mean, standard deviation, coefficient of variations |
| Frerich et al.33 | 64 patients with adolescent idiopathic scoliosis (A1S). Cobb angle between 10-50 degrees | Standard anterior-posterior radiograph | Correlation coefficient, average difference, range of difference |
| Mangone et al.32 | 25 patients with diagnosis of A1S | Vertebral rotation (Raimondi method regolo)33 | Kolmogorov-Smirrnov test, one way ANOVA intra-class-correlation coefficient (ICC), paired t-test, Spearman’s correlation coefficient by rank (rs) |
| Total | 570 patients |
SD, Standard deviation; RMS, root mean square.
Statistics
The root mean square (RMS) was used for data evaluation in six studies. Mean values were also found in five studies. Weiss 2008, Schulte 2008, Frerich 2012 and Magone 2013 et al. used correlation coefficients for statistical comparison of the parameters (Table 3).28,31-33
X-ray methods
Full-length radiographs of spines on two planes were made by Liljenqvist et al.25 and Hackenberg et al.30 These two authors were the only ones who determined vertebral rotation using the Perdriolle method (Table 3).
Study outcomes
The studies produced different results. The highest RMS for vertebral rotation was measured at 7.9 degrees. Smaller values for this parameter were found by Hackenberg et al. and Drerup et al.22-24,34 Crawford et al.40 illustrated a nonsignificant association between the two methods using a t-test. Weiss et al.31 produced a significant difference which will be discussed later (Table 4).22-25,28-33,40
Table 4.
Comparison between x-ray measurement and rasterstereography
| Study | Outcomes |
|---|---|
| Drerup et al.34 | RMS deviation of the spinal midline (frontal) 3.6 mm (4.6 mm), RMS deviation of rotation 2,7 degrees (3.1°), SD of lateral curve amplitude 4.0 mm, SD of rotation amplitude 2.5, difference in apex height –4.6 mm, SD of Cobb angle 7.9° |
| Liljenqvist et al.25 | Cobb angle: double-major scoliosis upper curvature 7.1° RMS, lower curvature 8.2°, thoracic scoliosis 7.8° RMS. thoracic and lumbar scoliosis 6.9° RMS, scoliotic malposition 7.4° RMS. Thoracic kyphosis with Scheuermann’s disease 5.6° RMS. Lumbar lordosis with Scheuermann’s disease 14.0° RMS. Torso overhang mean statistical spread 1.07 cm. Pelvic balance mean statistical spread 0.65 cm. Rotation of apical vertebra on average 7.9° RMS (depends on type of scoliosis) |
| Hackenberg et al.30 | Radiography apical vertebral rotation 29.2° preoperatively, 16.7° postoperatively, rasterstereographic max. surface rotation 16.5° preoperatively, 10.8° postoperatively, RMS preoperatively 14.8C |
| Hackenberg et al.22 | Average RMS difference of lateral deviation 5.8 mm, for vertebral and surface rotation curves 4.4° |
| Hackenberg et al.23 | Lateral deviation RMS difference 6.4 mm preoperatively, 3.4 mm postoperatively. Vertebral rotation (VR) without correction of trunk torsion RMS difference 5.3° preoperatively, 4.1° postoperatively, with correction of trunk torsion the RMS difference 4.5° preoperatively, 3.2° postoperatively |
| Hackenberg et al.24 | Lateral deviation RMS difference 5.8 mm preoperatively, 4.5 mm postoperatively. Vertebral rotation without correction of torsion RMS difference of 5.5° preoperatively, 5.2° without correction of torsion postoperatively, vertebral rotation with correction of torsion RMS 4.8° preoperatively, 4.3°with correction of torsion RMS postoperatively. |
| Schulte et al.29 | Group 1: Radiography maximum thoracic vertebral rotation 12.7° preoperatively, 6.8° follow-up. Secondary lumbar curve rotation 12.7° preoperatively, 10.9° at follow-up. Rasterstereography thoracic vertebral derotation 19.5° preoperatively, 10.4° follow-up. Secondary lumbar curve 9.6° preoperatively, 4.9° follow-up. Group 2: Radiography maximum lumbar vertebral rotation 21.9° preoperatively, 9.0° follow-up. Secondary thoracic curve vertebral rotation 5.0° preoperatively, 6.5° follow-up. Rasterstereography lumbar vertebral rotation 15.5° preoperatively, 6.0° postoperatively, secondary thoracic curve rotation 8.5° preoperatively, 11.3° postoperatively. |
| Schulte et al.28 | RMS differences 3.2 mm for vertebral lateral deviation and 2.5 degrees for vertebral rotation. Correlation coefficient Cobb angle radiography and lateral deviation RMS 0.7 rasterstereography and rotation RMS 0.5 rasterstereography. |
| Weiss et al.31 | Average kyphosis angle radiography 49°, SD 17°, rasterstereography 63°, SD 13°, Pearson correlation of 0.78, significant difference of 14 degrees in the t test (t 9.6 P<0.001). |
| Crawford et al.40 | Lumbar lordosis radiography at baseline mean 56.4°, SD 10.7° preoperatively, mean 53.5°, SD 12.1° six week follow-up. Lumbar lordosis rasterstereography baseline mean preoperatively 46.2°, SD 11.5, mean postoperatively 6-week follow up 43.1°, SD 7.6. Lumbar lordosis rasterstereography and radiography correlation preoperatively, P=0.28 (not significant), postoperatively, P=0.26 (not significant). |
| Frerich et al.33 | Lumbar curve average difference 9.40 degrees, range of difference 0-22, r=0.758 Thoracic curve average difference 7.00 degrees, range of difference 0-19, r=0.872, Thoracic kyphosis average difference 10.6 degrees, range of difference 1-24, r=0.799, Lumbar lordosis average difference 8 degrees, range of difference 0-21, r=0.813 |
| Mangone et al.32 | Ventral rotation (VR) by x-ray mean 9.93, SD 5.38, mean by RS 4.99, SD 3.50, t-test significant (t=10.48, P<0.0001. Lumbar VR by x-ray mean ± SD 9.18, SD 3.33, by RS mean 5.52, SD 3.01. Thoracic VR by x-ray mean 10.18, SD 5.90, by RS mean 4.82, SD 3.65. r=0.52 entire spine, r=0.47, Cobb angle <30° (subgroup) r=0.42 Cobb angle >30° (subgroup) r=0.30 lumbar ventral rotation (subgroup) r=0.47 thoracic ventral rotation (subgroup) |
SD, Standard deviation; RMS, root mean square.
QUADAS
Three studies scoring 12 points and two studies scoring 11 points on the QUADAS scale were evaluated; one study received four out of 14 possible points (Table 5).22-25,28-33,40
Discussion
Our systematic review of twelve studies evaluating the validity of RS shows that the accuracy of this method varies. Liljenqvist reported an unacceptably high root-mean-square difference for a vertebral rotation of 7.9 degrees.25 The RMS difference of vertebral rotation comparing digitized x-rays and rasterstereography was considerably lower in other studies.23,24,30,34 Postoperatively, Hackenberg et al. state problems when recording radiographic vertebral rotation according to the Perdriolle method.30 A source of inaccuracy of vertebral rotation could occur due to metallic implants hiding the contours of the vertebral bodies and pedicles.29
In some cases the patients had an idiopathic scoliosis located in the thoracic, thoracolumbar and lumbar parts of the spinal column. The highest Cobb angle of the scoliosis amounted to 92 degrees in Hackenberg.30 Other spinal pathologies were hyperkyphoses and Morbus Scheuermann. Healthy volunteers were not examined.
Some authors investigated more than the parameters in Table 2. But they didn’t match them with the radiographic or rasterstereographic correlate because some parameters are not directly comparable.
The statistical methods diverged. The RMS was frequently used as a statistical method. By calculating the RMS the square results were extracted; these have a smoothing effect on the absolute values.
Another problem when comparing absolute values became apparent in the study by Weiss.31 When the rasterstereographic kyphotic angle was compared to the radiometric kyphotic angle, a correlation of 0.78 according to Pearson was found. A t-test revealed a significant difference of 14 degrees (P<0.001) between the two methods, attributed to the fact that the radiometric kyphotic angle was measured from Th4 to Th12, but the rasterstereographic kyphotic angle was measured from Thl to Th12.
The most studies scored seven or more of possible 14 points on the QUADAS scale, which means that these studies minimum have sufficient methodological quality.
However, quantitative evaluation of the validity of RS is difficult because RS is based on external measurements of the outer contour. RS will reference outer contours formed by spinous processes. Furthermore, it is influenced by overlying subcutaneous tissue that may affect the evaluation of parameters related to the internal morphology e.g. the surrounding soft tissue rotates less than the spine itself. In contrast, radiographic measures are derived directly from the internal morphology and consider variability of the spine.32,40
Mohokum et al. however were able to show that a higher body mass index has no influence on the reliability of the method when used on healthy test volunteers.20
To be able to further improve research, it is important to standardise all applied statistical methods. Useful and suitable methods, in addition to mean values, standard deviation, scattering etc., would be a continuous evaluation of the correlation coefficient (e.g. Pearson) and the RMS. Ideally, in diagnostic studies involving rasterstereography, i.e. during an evaluation if the method appropriately detects spinal disorders according to current standards, a statement about the sensitivity and specificity should be made. Questions about influential factors such as the thickness of skin folds, body weight, body height, scars, etc. should be systematically included in further study designs.
Conclusions
Rasterstereography facilitates clinical practice by examining the spinal column. Further, it is completely radiation free and could help to monitor scoliosis progression. It can be used for screening examinations as well as for follow-ups and a diagnostic method for spinal scoliosis.
References
- 1.Luk KD, Lee CF, Cheung KM, et al. Clinical effectiveness of school screening for adolescent idiopathic scoliosis: a large population-based retrospective cohort study. Spine (Phila Pa 1976) 2010;35:1607-14. [DOI] [PubMed] [Google Scholar]
- 2.Corona J, Sanders JO, Luhmann SJ, et al. Reliability of radiographic measures for infantile idiopathic scoliosis. J Bone Joint Surg Am 2012;94:e86. [DOI] [PubMed] [Google Scholar]
- 3.Klos SS, Liu XC, Lyon RM, et al. Reliability of a functional classification system in the monitoring of patients with idiopathic scoliosis. Spine (Phila Pa 1976) 2007;32:1662-6. [DOI] [PubMed] [Google Scholar]
- 4.Hierholzer E, Hackenberg L. Three-dimensional shape analysis of the scoliotic spine using MR tomography and rasterstereography. Stud Health Technol Inform 2002;91:184-9. [PubMed] [Google Scholar]
- 5.Malmstrom EM, Karlberg M, Melander A, Magnusson M. Zebris versus Myrin: a comparative study between a three-dimensional ultrasound movement analysis and an inclinometer/compass method: intradevice reliability, concurrent validity, intertester comparison, intratester reliability, and intraindividual variability. Spine (Phila Pa 1976) 2003;28:E433-40. [DOI] [PubMed] [Google Scholar]
- 6.Cui G, Watanabe K, Nishiwaki Y, et al. Loss of apical vertebral derotation in adolescent idiopathic scoliosis: 2-year follow-up using multi-planar reconstruction computed tomography. Eur Spine J 2012;21:1111-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuklo TR, Potter BK, Schroeder TM, O’Brien MF. Comparison of manual and digital measurements in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2006;31:1240-6. [DOI] [PubMed] [Google Scholar]
- 8.Amzallag-Bellenger E, Uyttenhove F, Nectoux E, et al. Idiopathic scoliosis in children and adolescents: assessment with a biplanar X-ray device. Insights Imaging 2014;5:571-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ronckers CM, Land CE, Miller JS, et al. Cancer mortality among women frequently exposed to radiographic examinations for spinal disorders. Radiat Res 2010;174:83-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Levy AR, Goldberg MS, Hanley JA, et al. Projecting the lifetime risk of cancer from exposure to diagnostic ionizing radiation for adolescent idiopathic scoliosis. Health Phys 1994;66:621-33. [DOI] [PubMed] [Google Scholar]
- 11.Nash CL, Jr., Gregg EC, Brown RH, Pillai K. Risks of exposure to X-rays in patients undergoing long-term treatment for scoliosis. J Bone Joint Surg Am 1979;61:371-4. [PubMed] [Google Scholar]
- 12.Goldberg MS, Mayo NE, Levy AR, et al. Adverse reproductive outcomes among women exposed to low levels of ionizing radiation from diagnostic radiography for adolescent idiopathic scoliosis. Epidemiology 1998;9:271-8. [PubMed] [Google Scholar]
- 13.Drerup B. Rasterstereographic measurement of scoliotic deformity. Scoliosis 2014;9:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Drerup B. Principles of measurement of vertebral rotation from frontal projections of the pedicles. J Biomech 1984;17:923-35. [DOI] [PubMed] [Google Scholar]
- 15.Drerup B. Improvements in measuring vertebral rotation from the projections of the pedicles. J Biomech 1985;18:369-78. [DOI] [PubMed] [Google Scholar]
- 16.Drerup B, Hierholzer E. Automatic localization of anatomical landmarks on the back surface and construction of a body-fixed coordinate system. J Biomech 1987;20:961-70. [DOI] [PubMed] [Google Scholar]
- 17.Hierholzer E, Luxmann G. Three-dimensional shape analysis of the scoliotic spine using invariant shape parameters. J Biomech 1982;15:583-98. [DOI] [PubMed] [Google Scholar]
- 18.Hierholzer E, Schier F. Rasterstereography in the measurement and postoperative follow-up of anterior chest wall deformities. Z Kinderchir 1986;41:267-71. [DOI] [PubMed] [Google Scholar]
- 19.Lippold C, Moiseenko T, Drerup B, et al. Spine deviations and orthodontic treatment of asymmetric malocclusions in children. BMC Musculoskelet Disord 2012;13:151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mohokum M, Mendoza S, Udo W, et al. Reproducibility of rasterstereography for kyphotic and lordotic angles, trunk length, and trunk inclination: a reliability study. Spine (Phila Pa 1976) 2010;35:1353-8. [DOI] [PubMed] [Google Scholar]
- 21.Schulein S, Mendoza S, Malzkorn R, et al. Rasterstereographic evaluation of interobserver and intraobserver reliability in post-surgical adolescent idiopathic scoliosis patients. J Spinal Disord Tech 2013;26:E143-9. [DOI] [PubMed] [Google Scholar]
- 22.Hackenberg L, Hierholzer E. 3D back surface analysis of severe idiopathic scoliosis by rasterstereography: comparison of rasterstereographic and digitized radiometric data. Stud Health Technol Inform 2002;88:86-9. [PubMed] [Google Scholar]
- 23.Hackenberg L, Hierholzer E, Potzl W, et al. Rasterstereographic back shape analysis in idiopathic scoliosis after posterior correction and fusion. Clin Biomech (Bristol, Avon) 2003;18:883-9. [DOI] [PubMed] [Google Scholar]
- 24.Hackenberg L, Hierholzer E, Potzl W, et al. Rasterstereographic back shape analysis in idiopathic scoliosis after anterior correction and fusion. Clin Biomech (Bristol, Avon) 2003;18:1-8. [DOI] [PubMed] [Google Scholar]
- 25.Liljenqvist U, Halm H, Hierholzer E, et al. [3-dimensional surface measurement of spinal deformities with video rasterstereography]. Z Orthop Ihre Grenzgeb 1998;136:57-64. [Article in German] [DOI] [PubMed] [Google Scholar]
- 26.Whiting P, Rutjes AW, Reitsma JB, et al. The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res Methodol 2003;3:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whiting PF, Weswood ME, Rutjes AW, et al. Evaluation of QUADAS, a tool for the quality assessment of diagnostic accuracy studies. BMC Med Res Methodol 2006;6:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schulte TL, Hierholzer E, Boerke A, et al. Raster stereography versus radiography in the long-term follow-up of idiopathic scoliosis. J Spinal Disord Tech 2008;21:23-8. [DOI] [PubMed] [Google Scholar]
- 29.Schulte TL, Liljenqvist U, Hierholzer E, et al. Spontaneous correction and derotation of secondary curves after selective anterior fusion of idiopathic scoliosis. Spine (Phila Pa 1976) 2006;31:315-21. [DOI] [PubMed] [Google Scholar]
- 30.Hackenberg L, Liljenqvist U, Hierholzer E, Halm H. [Scanning stereographic surface measurement in idiopathic scoliosis after VDS (ventral derotation spondylodesis)]. Z Orthop Ihre Grenzgeb. 2000;138:353-9. [Article in German] [DOI] [PubMed] [Google Scholar]
- 31.Weiss HR, Elobeidi N. Comparison of the kyphosis angle evaluated by video rasterstereography (VRS) with x-ray measurements. Stud Health Technol Inform 2008;140:137-9. [PubMed] [Google Scholar]
- 32.Mangone M, Raimondi P, Paoloni M, et al. Vertebral rotation in adolescent idiopathic scoliosis calculated by radiograph and back surface analysis-based methods: correlation between the Raimondi method and rasterstereography. Eur Spine J 2013;22:367-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Frerich JM, Hertzler K, Knott P, Mardjetko S. Comparison of radiographic and surface topography measurements in adolescents with idiopathic scoliosis. Open Orthop J 2012;6:261-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Drerup B, Hierholzer E. Back shape measurement using video rasterstereography and three-dimensional reconstruction of spinal shape. Clin Biomech (Bristol, Avon) 1994;9:28-36. [DOI] [PubMed] [Google Scholar]
- 35.Drerup B, Hierholzer E. Evaluation of frontal radiographs of scoliotic spines. Part II. Relations between lateral deviation, lateral tilt and axial rotation of vertebrae. J Biomech 1992;25:1443-50. [DOI] [PubMed] [Google Scholar]
- 36.Drerup B, Hierholzer E. Evaluation of frontal radiographs of scoliotic spines. Part I. Measurement of position and orientation of vertebrae and assessment of clinical shape parameters. J Biomech 1992;25:1357-62. [DOI] [PubMed] [Google Scholar]
- 37.Perdriolle R. La Scoliose. Paris: Maloine, SA; 1979. [Google Scholar]
- 38.Weiss HR. Measurement of vertebral rotation: Perdriolle versus Raimondi. Eur Spine J 1995;4:34-8. [DOI] [PubMed] [Google Scholar]
- 39.Cobb JR. Outline for the study of Scoliosis. Instructional Course Lectures 5. Ann Arbor; J.W. Edwards: 1948. pp 261-275. [Google Scholar]
- 40.Crawford RJ, Price RI, Singer KP. The effect of interspinous implant surgery on back surface shape and radiographic lumbar curvature. Clin Biomech (Bristol, Avon) 2009;24:467-72. [DOI] [PubMed] [Google Scholar]
- 41.Stagnara P, De Mauroy JC, Dran G, et al. Reciprocal angulation of vertebral 409 bodies in a sagittal plane: approach to references for the evaluation of kyphosis and 410 lordosis. Spine (Phila Pa 1976) 1982;7:335-42. [DOI] [PubMed] [Google Scholar]


