Abstract
Postoperative spinal wound infection is a potentially devastating complication after operative spinal procedures. Despite the utilization of perioperative prophylactic antibiotics in recent years and improvements in surgical technique and postoperative care, wound infection continues to compromise patients’ outcome after spinal surgery. In the modern era of pending health care reform with increasing financial constraints, the financial burden of post-operative spinal infections also deserves consideration. The aim of our work is to give to the reader an updated review of the latest achievements in prevention, risk factors, diagnosis, microbiology and treatment of postoperative spinal wound infections. A review of the scientific literature was carried out using electronic medical databases Pubmed, Google Scholar, Web of Science and Scopus for the years 1973-2012 to obtain access to all publications involving the incidence, risk factors, prevention, diagnosis, treatment of postoperative spinal wound infections. We initially identified 119 studies; of these 60 were selected. Despite all the measures intended to reduce the incidence of surgical site infections in spine surgery, these remain a common and potentially dangerous complication.
Key words: Spine, infections, surgery, orthopedic
Introduction
Postoperative spinal wound infection is a potentially devastating complication after operative spinal procedures. Despite the utilization of prophylactic antibiotics, improvements in surgical technique and postoperative care, wound infections continue to compromise patients’ outcome after spinal surgery.1-7
Patients with a spinal wound infection have longer hospital lengths of stay, higher mortality, and higher re-operation rates.8 In the modern era of pending health care reform with increasing financial constraints, the financial burden of post operative spinal infections also deserves consideration. One estimate that quantified the associated increase in cost was performed by Thalgott et al. who reported an increase of $200,000 per patient.9
The aim of our work is to give to the reader an updated review of the latest achievements in prevention, risk factors, diagnosis, microbiology and treatment of postoperative spinal wound infections.
Search strategies and criteria
A review of the scientific literature was carried out using electronic medical databases Pubmed, Google Scholar, Web of Science and Scopus for the years 1973-2012 to obtain access to all publications involving postoperative spinal wound infections. Searches were restricted to the English literature only. The search terms were: postoperative spinal wound infections, postoperative wound infections of the spine, perioperative infections of the spine, surgical site infection after spine surgery, spinal infections. All available publications from the past 30 years, primarily from high-volume surgical centers, were considered.
Articles were selected if the abstract contained, according to the investigators’ experience, relevant information about, incidence, risk factors, prevention, diagnosis, treatment of postoperative spinal wound infections. The reference lists of these articles were also reviewed to find additional candidate studies. All articles selected for full text review were distributed to 2 reviewers, who independently decided on inclusion/exclusion and independently abstracted the study data. Two independent reviewers, G.E. and P.P., assessed the level of evidence quality using The levels of evidence for primary research question as adopted by the North American Spine Society, and disagreements were resolved by consensus.
Results
Using the earlier mentioned search strategy, 119 studies were initially identified. Of these 60 were selected (Figure 1).
Figure 1.
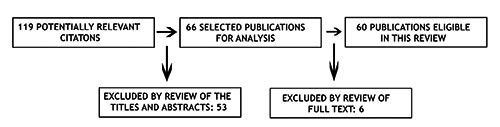
Study sample.
Incidence of postoperative spine infections
Surgical site infection (SSI) is the most common hospital acquired infection that occurs in the early postoperative period.10 The reported incidence of post-operative spinal infection has varied widely from 0.7% to 16%.1,4,7,8,10-18 The main reason for this wide range is that different types of intervention on the spine have different risks for postoperative infection. These studies have reported on heterogeneous patients populations in which the invasiveness of each type of procedure, for instance, was very different.
The most recent National Nosocomial Infections Surveillance Summary System, by the Centers for Disease Control and Prevention, reported rates of surgical site infection, from individual institutions, have ranged from 0% to 15%, depending on the indication to surgery, site, approach, and the use of instrumentation.10-14,19,20 One series, that may reflect a more accurate incidence for commonly performed spinal procedures was reported by Olsen et al.20 and demonstrated an incidence of surgical site infections following orthopedic spinal operations to be 2.0% (46 of 2316 cases presented).
Risk factors for postoperative spine infections
There are numerous influences on the development of postoperative infection that may be divided into two categories: i) unchangeable strictly patient-related, and ii) changeable or procedure-related.7,21-24
Patient’s related risk factors
The so-called unchangeable risk factors include patient age (older than 70), American Society of Anesthesiologists (ASA) score and medical conditions of which the most important are diabetes mellitus, cardiovascular disease, obesity, smoking, malignancy, steroid use, previous lumbar surgery, nutritional status, chronic obstructive pulmonary disease, immunologic competency.1-3,7,9,20,21,24,25 Further -more, the immunocompromized state related to diabetes predisposes patients to becoming infected with uncommon organisms.26-28 The nutritional status of the patient should be considered as a stand-alone risk, malnoutrished patients are 15 times more likely to acquire an infection after spinal procedures.9,21,22,29 Many authors consider a low blood level of albumin and a low number of white blood cells as a marker of a weak immune system and therefore a risk factor for infection.
Procedure related risk factors
Duration of surgery, estimated blood loss, blood transfusion, use of instrumentation, multiple staged intervention, number of levels fused, time the patient remains in the postoperative care unit, and prolonged preoperative hospital stay are the most important changeable risk factors.7,24,25,29,30 In fact, less invasive interventions, such as discectomy, have been reported to have a lower incidence of postoperative infection as opposed to more invasive techniques, as an instrumented fusion which have the highest reported rates of postoperative infection.1,17,24,31-33 The rate of infection for non-instrumented fusions has been reported to range from less than 1% up to 5%, whereas the rate with the addition of instrumentation increases to 1% to 7%.1,11,34-38 Along with instrumentation, a posterior approach has been shown to be a risk factor for postoperative infection.34,39-41 In theory, instrumentation may cause local soft tissue irritation leading to inflammation and seroma formation, which subsequently provides a fertile breeding ground for microorganisms to growth. Adherence of bacteria to the surface of implants is promoted by glycocalyx, a polysaccharide biofilm, that acts as barrier against the host immune response and antibiotic penetration.31,42,43 Finally, metallosis from micromotion of the instrumentation may lead to granuloma formation, another medium for bacterial colonization.31,44 A higher surgical case order has been proposed as a risk factor for SSI by Gruskay et al.45 Koutsoumbelis et al.7 reported that a greater number of people in the operating room during the surgical procedure, and specifically the number of nurses, was identified as an independent risk factor for infection. According to Memtsoudis et al.18 an anterior approach in more likely to be complicated by a local complication (including site infection) than a posterior approach; in their analysis of a national registry (NIS-National Inpatient Sample) they found that the highest rate of local morbidity was seen in fusion surgeries performed by an anterior-posterior combined approach (ALIF, TLIF, PLIF), which can be explained by longer surgical times, more blood loss, and increased surgical complexity. Although the approach is often dictated by the individual patient’s condition, newer access methods using the retroperitoneal space, thus avoiding intra abdominal structures, and thoracoscopic exploration may be considered to reduce morbidity and mortality whenever feasible.18 Although it may not be realistic to eliminate all potential risk factors for infection and a finite rate of infection may in fact be an intrinsic part of surgical intervention, however, preoperative modification of the changeable risk factors may lead to a minimization of a patient’s overall risk and may improve outcome and in turn lower costs.24,46
Prevention of postoperative spine infections
Risk factors reduction
Prevention of SSI in spine surgery may be focused on the changeable risk factors discussed previously. First of all it is clear that, concerning the risk of postoperative infections, the choice of the kind of intervention is crucial; therefore, when applicable, a less invasive method should be encouraged. The same attitude should be adopted with regard to the use of instrumentation. It is recommended that all distant site infections (e.g. pulmonary system, urinary system, gastro-intestinal tract) be aggressively treated in the perioperative period to reduce SSI.23
Fundamentally, to prevent spinal infections, sterile technique in the operating room is extremely important to prevent the initial inoculation of the wound. For a clinical infection to occur at the surgical site, bacteria must be present at the operative/procedural site in substantial quantity (105 organisms).17 It is widely recognized that most post-procedural infections are a consequence of direct inoculation and thus meticulous sterile handling in the OR is paramount.31,47
The invasiveness and complexity of the procedure is directly related to the post-procedural infections’ rate. In regard to this Gelalis et al.17 took microbial samples for culture from surgical wounds during surgery at regular intervals and reported no significant difference in the intraoperative contamination rate of the wound between shorter procedures, usually less invasive, and longer interventions, usually more complex. It is a very common practice to prepare the skin before surgery by shaving the skin at the site of incision. Celik et al.48 questioned whether skin shaving of the incision site could decrease the risk of infection and they demonstrated that, in a cohort of 789 patients who received pre-surgical skin shaving had a higher infection rate than patients who didn’t. One potential mechanisms for this finding is that shaving may cause a change in or loss of protective skin flora at the incision line, and micro trauma of the shaved area may increase bacterial colonization, both of these hazards may increase the risk of infection.48
Local chemical agents and drains
In the perspective of reducing the incidence of postoperative infections different adjunctive measures have been reported, for example the use of chemical agents, as local antibiotics and disinfectants, or physical agents as prophylactic drains.1,6,49-52
The use of powdered vancomycin locally administrated during surgery, as a prophylactic measure in an attempt to reduce the incidence of postoperative spinal wound infections, has been reported to be effective.49 Cheng et al. reported the efficacy of dilute betadine solution irrigation in the prevention of postoperative infection of spinal surgery.6 The use of prophylactic drains is common in orthopedics.50,51 The theoretical advantages of postoperative drain use include the evacuation of the post-operative hematoma and seroma, thereby decreasing the risk of infection and wound breakdown.50-52 In contrast to this commonly accepted principle Brown et al.50 studied the role of closed wound suction drainage in the prevention of deep infection and found no difference between patients in which a drain was placed vs patients without a drain. The use of drains is not recommended as a means to reduce infection rates after single-level surgical procedures by the North American Spine Society’s evidence-based guidelines for antibiotic prophylaxis in spine surgery.53
Perioperative antibiotic prophylaxis
The use of perioperative antibiotic prophylaxis to prevent infections is widespread and has resulted in an estimated reduction of post-operative spinal infections to less than 6%.24 Generally, a first-generation cephalosporin is used for prophylaxis; the reason of this choice is because of the activity of this kind of antibiotic against the methilicillin-susceptible Staphylococcus Aureus, Staphylococcus Epidermidis and most of the Enterobacteriacae. These are the most frequent microorganism responsible of infection of the surgical sites.15,54 Additional considerations are the low cost and the good soft-tissue and bone penetration of this antibiotics. It should be given intravenous before incision and repeated when the operation exceeds 4 hours. The antibiotic is continued postoperatively for no longer than 24 hours.5
Patients with previous history methicillin-resistant Staphylococcus aureus (MRSA) infection, institutions with high rate of MRSA (>10%) and methicillin-resistant Staphylococcus epidermidis (MRSE) (>20%) surgical site infections (SSIs), and patients colonized with MRSA, MRSA should undergo to perioperative prophylaxis with vancomycin.
Vancomycin has adequate activity against the most common high-resistant pathogens involved in orthopedic procedures, and it reaches high concentrations in the bone, synovia, and muscle within minutes after administration. A routine use of vancomycin should be discouraged since its routinely prophylactic use is associated with vancomycin-resistant Enterococcus Enterococcus colonization and infection.
Rubistein et al.54 evaluated, in a double blinded placebo-controlled randomized trial, the efficacy of a preoperative single dose Cephazolin in the prevention of SSI in lumbar spine. They reported that the use of perioperative prophylactic dose of Cephazolin in spinal surgery doesn’t reduce the incidence of postoperative infections but instead reduces the severity of the infection.
In the penicillin allergic patients, vancomycin, clindamycin, or ciprofloxacin are potential alternatives.1,4,8,43,53 Perioperative antibiotics have been shown in some studies to decrease the risk for postoperative infection nearly 10 times after discectomy.1,12,50,55
Patients with instrumented fusions have a decreased infection rate with the use of prophylaxis compared with patients having surgery without prophylaxis.1,8,12,53,54
Classification of postoperative spine infections
From an anatomical point of view SSIs are commonly classified as superficial or deep. Superficial infections are limited only to the skin or subcutaneous tissues without fascial involvement.1,19,24,31 Deep infections involve the fascia and/or paraspinal musculature in close proximity to the spine and neural elements.
Superficial wound infections may present with the four cardinal signs of infection pain (dolor), redness (rubor), swelling (tumor), and warmth (calor). Wound drainage may also be present and while the infection remains localized, bacteremia and systemic signs and symptoms may not be present.5,19,24,31 Diskitis, osteomyelitis and/or epidural abscess may occur as a deep infection may spread to the intervertebral disk, bone, and/or epidural space.31
Chronologically SSIs may be classified as early (within 4 weeks of a procedure), or delayed (more than 4 weeks later).5,23,24,31 Another consideration is the pathogen(s) producing the infection as pointed out by Thalgott et al.,9 who classified infections into group i) presence of a single microogranism type, group ii), presence of multiple organisms and group iii), multiple microorganisms with associated myonecrosis. Additionally, patients may be divided into group A, B and C on the basis of the functional status of the patient, as normal, with local or multiple systemic disease, and immunocompromized, respectively. The aim of the above classification is to facilitate the choice of treatment on the basis of infection severity, considered from a strictly microbiological point of view, and of the immune response of the host.
Microbiology of postoperative spine infections
The most frequent microorganism found in spinal surgical site infections is Staphyloococcus Aureus.1,7,15,23,32,54,55 Staphylococcus epidermidis and Enterococcus species have also been noted with increasing frequency in postoperative infections.1,54 Patients with compromised immune system may also present with a surgical wound infected by less virulent microorganisms.56
There has been a relative increase in other causative organisms over the last few years, particularly gram-negative bacteria.54 Several authors maintain that the routine use of prophylactic antibiotics has altered the spectrum of the reported organisms caused by postoperative spinal infections.20,24,53-55
Diagnosis
Clinical presentation
A suspect of infection should always arise in front of patients presenting back pain (especially at the surgical site), fever, and elevated white blood cell (WBC) count, elevated ESR and CRP.
Back pain is the most reliable symptom and is present in 83% to 100% of patients in the general population.56 Fever is the least reliable symptom and is present in 16% to 65% of patients in the general population.26 Fluctuance can indicate hematoma or an infectious collection. Typically, a sterile hematoma is not associated with increased pain or rubor.
Laboratory tests
Blood cultures should be drawn at the peak of temperature spikes. Several laboratory tests can be used to help establish the diagnosis of postprocedural infection. Initial blood work should consist of a complete blood count (CBC) with a differential, erythrocyte sedimentation rate (ESR), C-Reactive protein (CRP), and blood cultures.31 Leukocyte elevation with a definite shift toward polymorphonuclear cells is an indication of postoperative infection. Although the ESR is elevated immediately after surgery, it peaks by 4 days and usually returns to normal levels by 14 days.22,31 At 2 weeks, values should be less than 30, and at 6 weeks the ESR should be less than 20. A rising ESR after the fourth postoperative day is highly suggestive of an infectious process. CRP levels usually peak on postoperative day 2 and quickly return to preoperative levels. Infection can cause a persistently elevated CRP, or a second peak after surgery. If a fluctuance is present, multiple aspirations after sterile preparation of the skin can be considered. The fluid should be analyzed by Gram staining, aerobic and anaerobic cultures, and antibiotic sensitivities.22,31
Imaging
Usually plain film radiography is the first imaging requested but is unlikely to be helpful in the diagnosis of an acute postoperative infection. In case of delayed infections, lucency around grafts, hardware, or within the vertebrae is suggestive. Plain radiographs are helpful in inspecting surgical implants.22,31 Second level modalities such as computed tomography (CT) and magnetic resonance imaging (MRI) normally show dramatic changes after surgery. Edema, seroma, and hematoma are difficult to differentiate from infection. Thus, the diagnosis more heavily relies on appearance of the wound, laboratory studies, and clinical judgment. CT-guided biopsy may be of utility in the presence of a suspicious lesion or fluid collection.
Treatment of postoperative spine infections
Surgical site infections in spine surgery can be difficult to manage and often necessitate prolonged hospitalization, extended use of antibiotic therapy, wound debridement and irrigation or instrumentation removal.10,56
The traditional protocol treatment of SSI is early recognition, debridement, irrigation and culture-specific antibiotic administration. Usually as soon as the diagnosis of deep wound infection is done the patient is brought to the OR where the wound is thoroughly debrided and irrigated under general anesthetic; if the tissue has no necrosis and results clean at the end of the debridement the wound is closed over suction drain.1,11,23,31,56-58 If after the debridement the tissue looks questionable, the wound is packed open and re-debrided in 2 to 4 days. In cases of infection with a delayed onset, more than 37 weeks, the instrumentation can be removed because the arthrodesis may be solid.11,23,58
Surgical management of deep wound infections is commonly treated by long term antibiotic therapy.1,11,23,57-60 Many authors agree that it is useful to obtain a microbial culture of the infected wound to start a specific intravenous (i.v.) antibiotic therapy but it is vital to start a broad-spectrum antibiotic until the culture results and sensitivities are available.1,2,59 Weinstein et al.1 suggested that definitive treatment depends on the culture results but generally they consider infections with anaerobes as polymicrobial therefore to be treated with broad-spectrum antibiotics, as vancomycin or metronidazole, administered i.v. for 6 weeks. A suppressive antibiotic therapy is usually suggested consisting of oral administration of sulfamethoxazole thrimethroprim or doxycyline. The suppressive antibiotic therapy is different for anaerobes that can be treated with oral administration at suppressive dose of amoxicillin.1,2,59 To support the wound healing process recently the use of vacuum assisted closure (VAC) dressings and closed suction irrigation systems is becoming more popular in the clinical management of infected wounds.57,58,60 Rohmiller et al.60 assert that the advent of negative pressure suction devices has changed dramatically the management of postoperative wound infections. They reported a series of 28 postoperative deep wound infections treated with debridement, irrigation and placement of a CSIS with the use of a sterile saline normal solution for a mean period of 4 days. No antibiotic was added to the solution. All of the infected wounds healed without any additional measures. In opposition to this study we found interesting the work of Labler et al.57 They sustain that the drainage of an open wound under negative pressure VAC dressing is more efficient than local irrigation systems by continuously removing the wound fluid which inhibits mitosis, protein synthesis and fibroblast collagen synthesis and prevents its stasis in the wound. The drainage of extracellular fluid also reduces the interstitial pressure, increases blood flow and thus the local nutrition as well; they reported good results in a series of 15 post operative wound infections of the dorsal spine treated with serial debridement, irrigation, i.v. antibiotic therapy and placement of VAC dressing. Also Mehbod et al. proposed the application of a VAC device is a useful method to decrease the number of visits to the OR for debridement.58 They reported an average number of visits to the OR of 2.2 after the application of the VAC dressing against a literature average varying between 2.7 and 4.7.
Abbey et al.36 developed a treatment algorithm that may be considered a good treatment strategy. They suggest that the instrumentation should be removed only when multiple debridements and long period antibiotic therapy have failed; on the contrary Picada et al. state that instrumentation removal is not necessary in acute infections and that the instrumentation should remain in place until achieving the desired immobilization for arthrodesis.11
Conclusions
Despite all the measures intended to reduce the incidence of SSI in spine surgery these remain a common and potentially dangerous complication. Prevention is the best way to solve the problem. An improved understanding of the risk factors will allow improved preventative measures.
In both the short and long postsurgical period, surveillance by the surgeon is vital to make an early diagnosis. Once the infection is diagnosed a treatment strategy can be set up. The key principles of treatment are aggressive surgical treatment and targeted antibiotic therapy to eradicate the infection and limit damage to local tissues and the neural elements.
References
- 1.Weinstein MA, McCabe JP, Cammisa FP., Jr Postoperative spinal wound infection: a review of 2,391 consecutive index procedures. J Spinal Disord 2000;13:422-6. [DOI] [PubMed] [Google Scholar]
- 2.Pappou IP, Papadopoulos EC, Sama AA, et al. Postoperative infections in interbody fusion for degenerative spinal disease. Clin Orthop Relat Res 2006;444:120-8. [DOI] [PubMed] [Google Scholar]
- 3.Deyo RA, Cherkin DC, Loeser JD, et al. Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am 1992;74:536-43. [PubMed] [Google Scholar]
- 4.Pullter Gunne AF, Cohen DB. Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine (Phila Pa 1976) 2009;34:1422-8. [DOI] [PubMed] [Google Scholar]
- 5.Sasso RC, Garrido BJ. Postoperative spinal wound infections. J Am Acad Orthop Surg 2008;16:330-7. [DOI] [PubMed] [Google Scholar]
- 6.Cheng MT, Chang MC, Wang ST, et al. Efficacy of dilute betadine solution irrigation in the prevention of postoperative infection of spinal surgery. Spine (Phila Pa 1976) 2005;30:1689-93. [DOI] [PubMed] [Google Scholar]
- 7.Koutsoumbelis S, Hughes AP, Girardi FP, et al. Risk factors for postoperative infection following posterior lumbar instrumented arthrodesis. J Bone Joint Surg Am 2011;93:1627-33. [DOI] [PubMed] [Google Scholar]
- 8.Veeravagu A, Patil CG, Lad SP, Boakye M. Risk factors for postoperative spinal wound infections after spinal decompression and fusion surgeries. Spine (Phila Pa 1976) 2009;34:1869-72. [DOI] [PubMed] [Google Scholar]
- 9.Thalgott JS, Cotler HB, Sasso RC, et al. Postoperative infections in spinal implants. Classification and analysis: a multicenter study. Spine (Phila Pa 1976) 1991;16:981-4. [DOI] [PubMed] [Google Scholar]
- 10.Horan TC, Culver DH, Gaynes RP, et al. Nosocomial infections in surgical patients in the United States, January 1986-June 1992. National Nosocomial Infections Surveillance (NNIS) System. Infect Control Hosp Epidemiol 1993;14:73-80. [DOI] [PubMed] [Google Scholar]
- 11.Picada R, Winter RB, Lonstein JE, et al. Postoperative deep wound infection in adults after posterior lumbosacral spine fusion with instrumentation: incidence and management. J Spinal Disord 2000;13:42-5. [DOI] [PubMed] [Google Scholar]
- 12.Barker FG 2nd. Efficacy of prophylactic antibiotic therapy in spinal surgery: a meta-analysis. Neurosurgery 2002;51:391-401. [PubMed] [Google Scholar]
- 13.Beiner JM, Grauer J, Kwon BK, Vaccaro AR. Postoperative wound infections of the spine. Neurosurg Focus 2003;15:E14. [DOI] [PubMed] [Google Scholar]
- 14.Gaynes RP, Culver DH, Horan TC, et al. Surgical site infection (SSI) rates in the United States, 1992-1998: the National Nosocomial Infections Surveillance System basic SSI risk index. Clin Infect Dis 2001;33:S69-77. [DOI] [PubMed] [Google Scholar]
- 15.Fang A, Hu SS, Endres N, Bradford DS. Risk factors for infection after spinal surgery. Spine (Phila Pa 1976) 2005;30:1460-5. [DOI] [PubMed] [Google Scholar]
- 16.Smith JS, Shaffrey CI, Sansur CA, et al. Rates of infection after spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976) 2011;36:556-63. [DOI] [PubMed] [Google Scholar]
- 17.Gelalis ID, Arnaoutoglou CM, Politis AN, et al. Bacterial wound contamination during simple and complex spinal procedures. A prospective clinical study. Spine J 2011;11:1042-8. [DOI] [PubMed] [Google Scholar]
- 18.Memtsoudis SG, Vougioukas VI, Ma Y, et al. Perioperative morbidity and mortality after anterior, posterior, and anterior/posterior spine fusion surgery. Spine (Phila Pa 1976) 2011;36:1867-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.National Nosocomial Infections Surveillance System. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June. 2004, issued October 2004. Am J Infect Control 2004;32:470-85. [DOI] [PubMed] [Google Scholar]
- 20.Olsen MA, Nepple JJ, Riew KD, et al. Risk factors for surgical site infection following orthopaedic spinal operations. J Bone Joint Surg Am 2008;90:62-9. [DOI] [PubMed] [Google Scholar]
- 21.Levin R, Bono CM, Garfin SR. Vertebral discitis and osteomyelitis. Vaccaro AR, ed. Spine: core knowledge in orthopaedics. Philadephia: Mosby; 2005. pp. 212-225. [Google Scholar]
- 22.Bono CM, Kauffman CP, Garfin SR. Postoperative cervical spine infections. In: The cervical spine. 4th Ed. Benzel E, Eismont F, Currier BL, et al. eds. Philadelphia: LWW; 2005. pp 1170-1178. [Google Scholar]
- 23.Dipaola CP, Saravanja DD, Boriani L, et al. Postoperative infection treatment score for the spine (PITSS): construction and validation of a predictive model to define need for single versus multiple irrigation and debridement for spinal surgical site infection. Spine J 2012;12:218-30. [DOI] [PubMed] [Google Scholar]
- 24.Christodoulou AG, Givissis P, Symeonidis PD, et al. Reduction of postoperative spinal infections based on an etiologic protocol. Clin Orthop Relat Res 2006;444:107-13. [DOI] [PubMed] [Google Scholar]
- 25.Dick J, Boachie-Adjei O, Wilson M. One-stage versus two-stage anterior and posterior spinal reconstruction in adults. Comparison of outcomes including nutritional status, complications rates, hospital costs, and other factors. Spine(Phila Pa 1976) 1992;17:S310-6. [DOI] [PubMed] [Google Scholar]
- 26.Carragee EJ. Pyogenic vertebral osteomyelitis. J Bone Joint Surg Am 1997;79:874-80. [DOI] [PubMed] [Google Scholar]
- 27.Gupta RK, Khan ZU, Nampoory MR, et al. Cutaneous cryptococcosis in a diabetic renal transplant recipient. J Med Microbiol 2004;53:445-9. [DOI] [PubMed] [Google Scholar]
- 28.Khurram IM, Khan SA, Khwaja AA, et al. Risk factors for clinical infection in patients colonized with methicillin resistant Staphylococcus aureus (MRSA). J Pak Med Assoc 2004;54:408-12. [PubMed] [Google Scholar]
- 29.Klein JD, Hey LA, Yu CS, et al. Perioperative nutrition and postoperative complications in patients undergoing spinal surgery. Spine (Phila Pa 1976) 1996;21:2676-82. [DOI] [PubMed] [Google Scholar]
- 30.Carreon LY, Puno RM, Dimar JR 2nd, et al. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am 2003;85A:2089-92. [DOI] [PubMed] [Google Scholar]
- 31.Chaudhary SB, Vives MJ, Basra SK, Reiter MF. Postoperative spinal wound infections and postprocedural diskitis. J Spinal Cord Med 2007;30:441-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heller JG. Postoperative infections of the spine. In: Rothman RH, Simeone FA, eds. The spine. Philadelphia: WB Saunders; 1992. pp 1817-1837. [Google Scholar]
- 33.Massie JB, Heller JG, Abitbol JJ, et al. Postoperative posterior spinal wound infections. Clin Orthop Relat Res 1992:99-108. [PubMed] [Google Scholar]
- 34.Levi AD, Dickman CA, Sonntag VK. Management of postoperative infections after spinal instrumentation. J Neurosurg 1997;86:975-80. [DOI] [PubMed] [Google Scholar]
- 35.Lonstein J, Winter R, Moe J, Gaines D. Wound infection with Harrington instrumentation and spine fusion for scoliosis. Clin Orthop Relat Res 1973:222-33. [PubMed] [Google Scholar]
- 36.Abbey DM, Turner DM, Warson JS, et al. Treatment of postoperative wound infections following spinal fusion with instrumentation. J Spinal Disord 1995;8:278-83. [DOI] [PubMed] [Google Scholar]
- 37.Glassman SD, Dimar JR, Puno RM, Johnson JR. Salvage of instrumental lumbar fusions complicated by surgical wound infection. Spine (Phila Pa 1976) 1996;21:2163-9. [DOI] [PubMed] [Google Scholar]
- 38.Hodges SD, Humphreys SC, Eck JC, et al. Low postoperative infection rates with instrumented lumbar fusion. South Med J 1998;91:1132-6. [DOI] [PubMed] [Google Scholar]
- 39.Olsen MA, Mayfield J, Lauryssen C, et al. Risk factors for surgical site infection in spinal surgery. J Neurosurg 2003;98:149-55. [PubMed] [Google Scholar]
- 40.Wimmer C, Gluch H, Franzreb M, Ogon M. Predisposing factors for infection in spine surgery: a survey of 850 spinal procedures. J Spinal Disord 1998;11:124-8. [PubMed] [Google Scholar]
- 41.Pull ter Gunne AF, van Laarhoven CJ, Cohen DB. Surgical site infection after osteotomy of the adult spine: does type of osteotomy matter? Spine (Phila Pa 1976) 2009;34:1422-8.19478664 [Google Scholar]
- 42.Bassewitz HL, Fischgrund JS, Herkowitz HN. Postoperative spine infections. Semin Spine Surg 2000;12:203-11. [Google Scholar]
- 43.Wilson SC, Skinner HB. Orthopedic infections. Skinner HB, ed. Current diagnosis & treatment in orthopedics. 4th Ed. New York: McGraw-Hill; 2006. Chapter 8. [Google Scholar]
- 44.Clark CE, Shufflebarger HL. Late-developing infection in instrumented idiopathic scoliosis. Spine (Phila Pa 1976) 1999;24:1909-12. [DOI] [PubMed] [Google Scholar]
- 45.Gruskay J, Kepler C, Smith J, et al. Is surgical case order associated with increased infection rate after spine surgery? Spine (Phila Pa 1976). 2012;37:1170-4. [DOI] [PubMed] [Google Scholar]
- 46.Schuster JM, Rechtine G, Norvell DC, Dettori JR. The influence of perioperative risk factors and therapeutic interventions on infection rates after spine surgery: a systematic review. Spine (Phila Pa 1976) 2010;35:S125-37. [DOI] [PubMed] [Google Scholar]
- 47.Cruse PJ, Foord R. A five-year prospective study of 23,649 surgical wounds. Arch Surg 1973;107:206-10. [DOI] [PubMed] [Google Scholar]
- 48.Celik SE, Kara A. Does shaving the incision site increase the infection rate after spinal surgery? Spine (Phila Pa 1976) 2007;32:1575-7. [DOI] [PubMed] [Google Scholar]
- 49.Molinari RW, Khera OA, Molinari WJ 3rd. Prophylactic intraoperative powdered vancomycin and postoperative deep spinal wound infection: 1512 consecutive surgical cases over a 6-year period. Eur Spine J 2012;21:S476-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Brown MD, Brookfield KF. A randomized study of closed wound suction drainage for extensive lumbar spine surgery. Spine (Phila Pa 1976) 2004;29:1066-8. [DOI] [PubMed] [Google Scholar]
- 51.Payne DH, Fischgrund JS, Herkowitz HN, et al. Efficacy of closed wound suction drainage after single-level lumbar laminectomy. J Spinal Disord 1996;9:401-3. [PubMed] [Google Scholar]
- 52.Beer KJ, Lombardi AV, Jr, Mallory TH, Vaughn BK. The efficacy of suction drains after routine total joint arthroplasty. J Bone Joint Surg Am 1991;73:584-7. Erratum in: J Bone Joint Surg Am 1991;73:791. [PubMed] [Google Scholar]
- 53.Watters WC 3rd, Baisden J, Bono CM, et al. Antibiotic prophylaxis in spine surgery: an evidence-based clinical guideline for the use of prophylactic antibiotics in spine surgery. Spine J 2009;9:142-6. [DOI] [PubMed] [Google Scholar]
- 54.Rubinstein E, Findler G, Amit P, Shaked I. Perioperative prophylactic cephazolin in spinal surgery. A double-blind placebo-controlled trial. J Bone Joint Surg Br 1994;76:99-102. [PubMed] [Google Scholar]
- 55.Horwitz NH, Curtin JA. Prophylactic antibiotics and wound infections following laminectomy for lumber disc herniation. J Neurosurg 1975;43:727-31. [DOI] [PubMed] [Google Scholar]
- 56.Cunningham ME, Girardi F, Papadopoulos EC, Cammisa FP. Spinal infections in patients with compromised immune systems. Clin Orthop Relat Res 2006;444:73-82. [DOI] [PubMed] [Google Scholar]
- 57.Labler L, Keel M, Trentz O, Heinzelmann M. Wound conditioning by vacuum assisted closure (V.A.C.) in postoperative infections after dorsal spine surgery. Eur Spine J 2006;15:1388-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mehbod AA, Ogilvie JW, Pinto MR, et al. Postoperative deep wound infections in adults after spinal fusion: management with vacuum-assisted wound closure. J Spinal Disord Tech 2005;18:14-7. [DOI] [PubMed] [Google Scholar]
- 59.Abbey DM, Turner DM, Warson JS, et al. Treatment of postoperative wound infections following spinal fusion with instrumentation. J Spinal Disord 1995;8:278-83. [DOI] [PubMed] [Google Scholar]
- 60.Rohmiller MT, Akbarnia BA, Raiszadeh K, et al. Closed suction irrigation for the treatment of postoperative wound infections following posterior spinal fusion and instrumentation. Spine (Phila Pa 1976) 2010;35: -642-6. [DOI] [PubMed] [Google Scholar]


