Abstract
Background:
Low back pain is a common symptom arising from many possible sources and includes the possibility of the contribution of remote pathology. This report describes a patient with bilateral osteonecrosis of the femoral heads presenting with a primary symptom of low back pain.
Case presentation:
A 37-year-old male presented for evaluation of dominant pain that existed for approximately 6–12 months and was located in the right low back. Milder pain was also reported in the right hip. Low back and hip pain were both aggravated by weight-bearing activities. An evidence-based diagnostic evaluation revealed little indication for a primary pain source originating from low back structures. Radiographs revealed bilateral osteonecrosis with evidence of left femoral head collapse.
Conclusion:
Hip osteonecrosis may have contributed to an atypical presentation of low back pain due to aberrant localization of pain and/or combined with altered biomechanical loading of musculoskeletal structures.
Keywords: low back pain, hip joint, osteonecrosis, diagnosis, chiropractic, avascular necrosis
Abstract
Historique :
La lombalgie est un symptôme commun découlant de nombreuses sources possibles et comprend la possibilité de la contribution d’une pathologie distante. Cette étude décrit un patient atteint d’ostéonécrose bilatérale des têtes fémorales présentant un symptôme primaire de lombalgie.
Exposé de cas :
Un homme de 37 ans s’est présenté pour l’évaluation d’une douleur dominante dans le bas du dos, côté droit, qui existait depuis environ 6 à 12 mois. Une douleur plus légère a également été signalée à la hanche droite. Ces deux douleurs s’aggravaient pendant des activités où il fallait porter une charge. Une évaluation diagnostique fondée sur des preuves a révélé peu d’indication d’une source de douleur primaire provenant de structures lombaires. Les radiographies ont révélé une ostéonécrose bilatérale avec une constatation de l’effondrement de la tête fémorale gauche.
Conclusion :
L’ostéonécrose de la hanche pourrait avoir contribué à une présentation atypique de douleurs lombaires en raison de la localisation aberrante de la douleur ou de la combinaison avec la charge biomécanique altérée des structures musculosquelettiques.
Keywords: douleur lombaire, articulation de la hanche, ostéonécrose, diagnostic, chiropratique, nécrose avasculaire
Background
Low back pain (LBP) is a common symptom arising from many potential anatomic sources such as nerve roots, myofascial structures, bone, joints, intervertebral discs, and organs within the abdominal cavity.1,2 Symptoms can also spawn from aberrant neurological pain processing3,4 and are influenced substantially by psychosocial elements5–10. Thus, the diagnostic evaluation of patients with LBP often requires complex clinical decision-making.11
LBP can also be caused by remotely located or concurrent conditions.12–15 An example of LBP remotely generated from the hip was reported by Ben-Galim et al., who studied 25 patients diagnosed with hip osteoarthritis and concomitant LBP. Patients underwent total hip arthroplasty and experienced both a reduction in hip and LBP sustained for at least 2 years following surgery.16 Similarly, Sembrano et al. studied 368 patients with LBP originating from a combination of spine and hip (8%) and spine and sacroiliac joint (7.5%) pathology. LBP was reported by patients with pathology identified only in the hip region in 2.5% of cases.17
LBP generated from hip pathology is likely due to the functional interdependence of related regions18,19 and has been labeled hip-spine syndrome20. Briefly, this syndrome describes altered spinal alignment with changes in transmitted forces and muscle length in the presence of hip pathology. Indirect evidence for this concept is demonstrated by patients with LBP who also exhibit reduced ROM, strength, and muscular endurance in the hip21–23 and by those who achieve measurable clinical improvement in LBP symptoms following treatment directed at the hip region24,25.
Osteonecrosis (ON), or avascular necrosis, of the hip is characterized by disruption or loss of nutrient blood supply to the femoral head resulting in progressive osseus breakdown, often leading to structural failure of the cortical surface.26 Estimates suggest that up to 20,000 new cases of hip ON are diagnosed each year in the United States alone27,28 and up to 60% occur bilaterally29. ON etiology can be categorized as traumatic by direct injury to the hip, or non-traumatic by factors such as collagen vascular disease, sickle cell hemoglobinopathy, and possibly long-term exposure to corticosteroid drugs.30–33 Non-traumatic ON most commonly occurs between the 3rd and 5th decade34 exhibiting variable progression, though many cases develop femoral head collapse within 3 years following diagnosis35. In addition to hip pain, patients with ON report concomitant pain in the low back, buttock, groin, thigh, and knee.36–38
This case report describes an adult male with chronic low back pain who presented for an eligibility examination before enrollment in a clinical trial involving chiropractic care for patients with LBP.39 The case presented in this article was unique in that our in-office evaluation revealed little diagnostic evidence for a symptom source located in the lumbar region. Radiographic imaging, however, revealed bilateral osteonecrosis of the femoral heads.
Case presentation
Clinical history
A 37-year-old African-American male with a varied work history reported LBP which he first experienced upon waking approximately 6–12 months before evaluation at our clinic. No traumatic incident or injury was reported prior to symptom onset. At exam, his most severe pain, rated at 5/10 on a numerical rating scale, was located over the right posterior iliac crest. Milder pain was also reported in the anterior right hip region. Both the low back and hip pain were sharp in quality and exhibited varying intensity. Walking, twisting the torso, and initiating movements such as rising from a chair provoked both hip and low back symptoms. Palliative activities included lying down and sitting. The patient denied any previous evaluation or treatment for these symptoms. Health history included childhood onset asthma, a 4-pack/year smoking history, one acute asthma hospitalization with corticosteroid therapy (1 year prior), and a recent frostbite injury to the left foot. Alcohol consumption of ≥ 4 drinks per day reportedly occurred 9 times in the past year with an average of 2 drinks per week. Current medication consisted only of the bronchodilator albuterol, as needed, for asthma symptoms.
Examination
Clinical evaluation was conducted using an evidence-based diagnostic classification system for LBP developed by Vining et al.40 The system incorporates a checklist tool to aid practitioners in synthesizing and organizing the historical and examination information to confirm or rule out diagnoses. Briefly, the checklist includes between 1 and 6 criteria supporting a specific diagnosis for LBP and a screening category indicating the need for additional evaluation or referral. When a criterion is met, a checkbox is marked indicating evidence for a particular diagnosis. Evidence is demonstrated by meeting clinical prediction rules or multiple criteria within a category. Conversely, evidence against a diagnosis is demonstrated by failing to meet a sufficient number of criteria within a category. An example of the diagnostic checklist tool is provided in Appendix 1.
Gait observation revealed a slight stiff-legged limp guarding the left lower extremity, attributed by the patient to plantar foot surface sensitivity persisting since his frostbite injury. Pulse, respiration, blood pressure, and temperature were within normal limits as were active and passive lumbar and hip ranges of motion. Pain did not centralize on repeated lumbar end range loading. Likewise, thigh thrust, sacral thrust, iliac compression, anterior superior iliac spine compression, and the lumbar extension-rotation test did not reproduce pain. Achilles and patellar deep tendon reflexes were normally symmetrical and responsive. Muscle strengths of the tibialis anterior, extensor hallicus longus and peroneus were +5 and symmetrical. The Leeds Assessment for Neuropathic Symptoms and Signs score was 0 indicating pain was arising from a nociceptive instead of a neuropathic source.41
Only 3 examination maneuvers mildly reproduced the patient’s LBP: Gaenslen’s test on the right, femoral nerve stretch on the right, and active lumbar extension. Patrick’s test and passive external rotation of the right hip produced right hip pain. No examination procedures produced pain in the left hip. Lumbar segmental hypomobility and mild paraspinal hypertonicity were also noted.
The health history and symptom characteristics combined with few and mild examination findings (described above) did not result in evidence suggesting locally-generated LBP. Likewise, there was no historical, symptomatic, or examination evidence for neuropathic pain.5,40 Two examination maneuvers resulted in hip pain creating some suspicion for hip pathology. Lumbar pathology was still considered possible due to chronicity, failure to meet any diagnostic criteria, and lack of an event that initiated symptoms. Thus, the decision was made to conduct a radiographic examination of the lumbar spine and pelvis.
Imaging and diagnosis
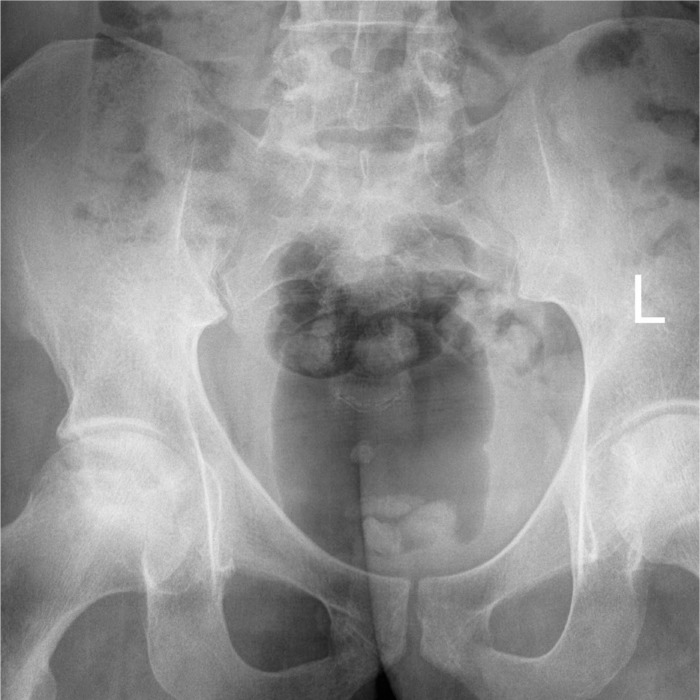
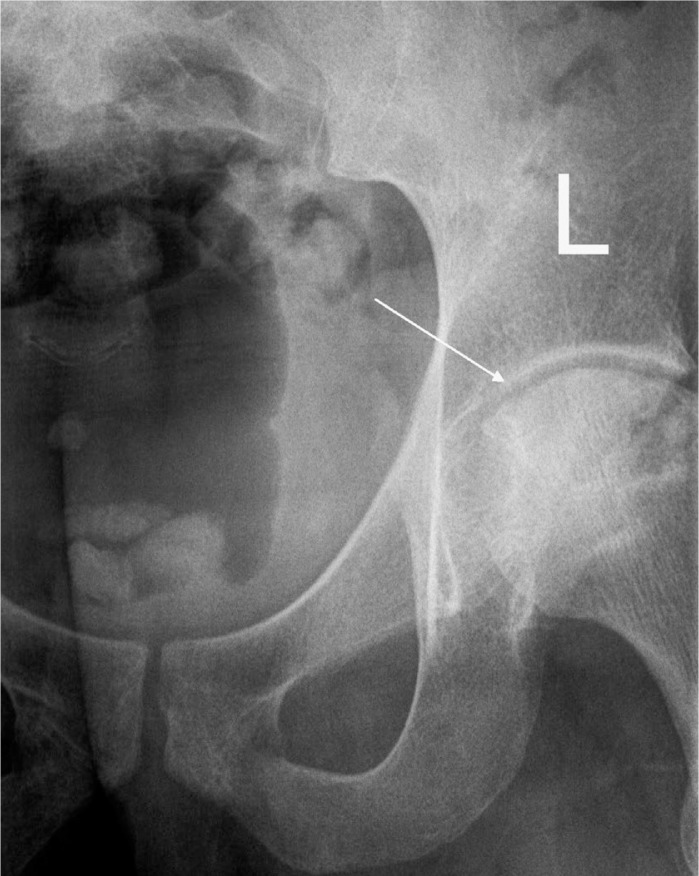
Radiographic examination revealed a slight left lumbar convexity without notable degenerative change in the lumbar spine or sacroiliac joints. Right and left femoral heads showed a mixed sclerotic pattern (See Figure 1). The left femoral head demonstrated a mild loss of sphericity, indicating early cortical collapse (See Figure 2). Altered density in the femoral head(s) accompanied by collapse of the femoral cortical surface (impaction fracture) are findings consistent with a diagnosis of osteonecrosis.42
Figure 1.
Radiographic image showing bilateral mixed or patchy sclerosis represented by areas of non-uniform density in the superior femoral heads extending toward but not into the femoral necks.
Figure 2.
Radiographic image of left hip. Subtle flattened area (Arrow) on the superior medial cortical surface of the femur represents impaction fracture of underlying necrotic bone.
Outcomes
The patient was informed of the diagnosis and that he was ineligible for the clinical trial because he needed a surgical evaluation and a condition causing the LBP originating from the low back region could not be confirmed.39 The doctor of chiropractic discussed the potential detrimental health effects of alcohol consumption due to reported levels that categorized him with a slight risk for dependence or abuse.43 The patient was then referred to a primary care provider to further evaluate ON etiology and to facilitate a surgical consultation. An orthopedic surgeon concurred with the diagnosis of bilateral ON and considered the most likely etiology to be that of prior corticosteroid use, possibly in combination with prior alcohol consumption. Bilateral total hip arthroplasty was recommended. Chiropractic treatment (i.e. palliative manipulative therapies, exercises designed to relieve LBP and/or hip symptoms, and/or activity modifications that reduce weight-bearing on the affected joints) was not pursued because care at our clinic is not available for patients outside those enrolled in ongoing clinical trials. At the time this manuscript was submitted for publication, the patient had not undergone corrective surgery due to an elective decision to postpone.
Discussion
In this case, the patient’s clinical history and examination did not indicate a primary source of LBP originating from low back structures and imaging revealed no latent pathology in the lumbar spine. Hip examination findings were only mildly suggestive of several potential conditions, such as femoroacetabular impingement and osteoarthritis44,45 which require more advanced testing to confirm a diagnosis46–49. Radiographic imaging demonstrated bilateral ON with the left hip showing greater structural deterioration despite normal examination findings and the absence of symptoms on that side. Incongruity between the severity of imaging findings and symptoms is not uncommon in many musculoskeletal conditions.50,51
Bilateral ON was visible with standard radiography because the condition had reached a level of progression demarcated by relatively advanced bony disorganization and collapse. Had ON been strongly suspected without radiographic evidence, we likely would have recommended magnetic resonance imaging because it is a more sensitive diagnostic tool capable of detecting early ON pathology.52,53
Though there is no definitive method available to confirm the dominant source of pain, the lack of evidence supporting a local LBP diagnosis in conjunction with the radiographic evidence compelled us to theorize the symptom contribution in this case. We posit hip ON contributed to an atypical presentation of LBP most likely due to altered biomechanical loading of pelvic and low back structures or combined with referred pain or aberrant localization.
Risk factors for non-traumatic ON include corticosteroid use, alcohol abuse, sickle cell disease, systemic lupus erythematosus, renal failure and hematologic disorders.35,52 More than 90% of non-traumatic hip ON cases are estimated to occur secondary to alcohol and corticosteroid use54 possibly via mechanisms that result in fatty infiltration of bone marrow leading to intraosseus hypertension, vascular compression, and diminished vascularity to the femoral head55,56. However, the causal relationships between ON and alcohol and corticosteroid use is unclear because it is difficult to separate pharmacologic side-effects from underlying disease.57 The patient described here had a relatively recent history of short-term corticosteroid use. The suspected mechanisms by which corticosteroids can cause ON suggest that long-term use, instead of short-term, is necessary for increasing risk.58 Therefore, corticosteroids may not have contributed to the development of ON in this case. Likewise, the quantity of prior alcohol use did not suggest long-term abuse and may not have played a contributing role. No other substantial risk factors were identified.
Classification and management options
Clinical and radiographic findings can be grouped in stages to help diagnose and track the progress of ON. The Ficat-Arlet classification system categorizes ON based on pathological progression. Table 1 lists common imaging findings associated with each classification stage.59 In cases where cortical collapse occurs and/or hip degeneration is present causing pain or compromised articulation (Ficat-Arlet stage III or IV), total hip arthroplasty is likely the only treatment option that will allow patients to remain ambulatory in the long-term.60
Table 1.
Radiographic imaging findings associated with Ficat-Arlet stages of osteonecrosis of the hip
| Stage | Radiographic Findings |
|---|---|
| 0 Preclinical | Normal or near-normal |
| I Preradiographic | Normal or near-normal |
| II Prior to head collapse or sequestrum formation |
|
| III Collapse |
|
| IV Degenerative |
|
Conservative early-interventional (pre-cortical collapse) approaches include activity and lifestyle modifications that significantly limit weight-bearing, and therefore, compressive loading of the femoral head.35,54 Encouraging patients to reduce alcohol consumption and supporting smoking cessation may also be helpful.61 Other conservative treatments intended to stimulate revascularization and bone regrowth include extracorporeal shockwave therapy, pulsed electromagnetic field therapy, and hyperbaric oxygen therapy.34,35 Pharmacotherapy options include bisphosphonate compounds which treat ON by depressing osteoclast activity and inducing apoptosis, thereby delaying trabecular collapse. However, in a review of therapies for non-traumatic ON, Lee et al. concluded that sufficient evidence is not currently present to support the routine use of pharmacologic agents.34 Two surgical procedures designed to prevent collapse and stimulate regrowth are core decompression and vascularized bone grafts. No clear evidence points to either procedure as a more effective approach, perhaps due in part to the heterogeneity of specific presentations and co-morbid conditions contributing to ON.35,57
Following cortical collapse, total hip arthroplasty or femoral head resurfacing may be recommended. Unfortunately, evidence indicating either procedure as most appropriate or predictive of outcomes also appears mixed.60,62,63 In this case, only 1 femoral head demonstrated collapse, and bilateral total hip arthroplasty was recommended.
Conclusion
This report describes a patient with bilateral hip ON possibly contributing to atypical LBP via referred pain or altered biomechanical loading of pelvic and low back tissues. The case demonstrates the value of performing an evidenced-based diagnostic investigation for patients with LBP, including substance use exposure and detailed health history, and having a working knowledge of clinical management options for those identified with ON. ON can occur in combination with other conditions commonly treated by manual therapy practitioners, and similar cases present opportunities to co-manage patients and collaborate with other healthcare professionals.
Acknowledgments
We are grateful to the participant for consenting to the publication of this report. The authors wish to acknowledge the principal investigators of the clinical trial, Ting Xia and Christine Goertz, the National Center for Complementary and Alternative Medicine, National Institutes of Health, Grant Number 5U19AT004663, and the ability to conduct the trial in a facility constructed with support from Research Facilities Improvement Grant Number C06 RR15433 from the National Center for Research Resources, National Institutes of Health.
Appendix 1. Diagnostic classification checklist for patients with chronic low back pain. Reprinted with permission from the Journal of the Canadian Chiropractic Association [40].
| Screening | ||
|---|---|---|
| Is there evidence of progressive neurological deficit? ............................................................................. | ❑ No | ❑ Yes |
| Is there evidence of pathologic fracture, infection or malignancy? ......................................................... | ❑ No | ❑ Yes |
| Are there gait difficulties, spasticity or other signs of myelopathy?........................................................ | ❑ No | ❑ Yes |
| Recent history of unplanned or unexplained weight loss?....................................................................... | ❑ No | ❑ Yes |
| Is there evidence of seronegative spondyloarthropathy? ......................................................................... | ❑ No | ❑ Yes |
| Nociceptive Pain | ||
|---|---|---|
| Discogenic Pain | ||
| Centralization with repeated motion ........................................................................................................ | ❑ No | ❑ Yes |
| Any two: (Centralization w/ repeated motion, vulnerable/apprehensive when stooped, & exten. loss). | ❑ No | ❑ Yes |
| SI Joint Pain (3 or more of 6 tests) | ||
| Three or more of 6 + SI Joint tests without centralization with repeated motion .................................... (Gaenslen’s L & R, Thigh Thrust [symptom side], Distraction, Iliac Compression, Sacral Thrust) |
❑ No | ❑ Yes |
| Zygapophyseal (Facet) Joint Pain (3 or more) | ||
| Age > 50 ................................................................................................................................................... | ❑ No | ❑ Yes |
| Pain relieved when walking ..................................................................................................................... | ❑ No | ❑ Yes |
| Pain relieved when sitting ........................................................................................................................ | ❑ No | ❑ Yes |
| Onset of pain was paraspinal ................................................................................................................... | ❑ No | ❑ Yes |
| Positive Extension-Rotation test .............................................................................................................. | ❑ No | ❑ Yes |
| Myofascial Pain | ||
| Ache-type pain with aggravation by use of involved muscle .................................................................. | ❑ No | ❑ Yes |
| Trigger point in muscle with possible radiation ....................................................................................... | ❑ No | ❑ Yes |
| Neuropathic Pain | ||
|---|---|---|
| Compressive Radiculopathy | ||
| Absent ankle/knee reflex .......................................................................................................................... | ❑ No | ❑ Yes |
| Leg pain worse than back pain? ............................................................................................................... | ❑ No | ❑ Yes |
| Dermatome distribution (cough, sneeze, strain) ...................................................................................... | ❑ No | ❑ Yes |
| Paresis (extremity motor strength loss).................................................................................................... | ❑ No | ❑ Yes |
| Finger floor distance during flexion >25cm ............................................................................................. | ❑ No | ❑ Yes |
| LANSS score >12 .................................................................................................................................... | ❑ No | ❑ Yes |
| Non-compressive Radiculopathy | ||
| LANSS score >12 .................................................................................................................................... | ❑ No | ❑ Yes |
| Compressive Radiculopathy criteria are satisfied .................................................................................... | ❑ No | ❑ Yes |
| Neurogenic Claudication | ||
| Score of 7 or more on clinical prediction rule ......................................................................................... | ❑ No | ❑ Yes |
| ABI greater than 0.9 (if indicated) ........................................................................................................... | ❑ No | ❑ Yes |
| Central Pain | ||
| Pain disproportionate to injury/pathology ............................................................................................... | ❑ No | ❑ Yes |
| Disproportionate, non-mechanical, unpredictable pattern of aggravating/relieving factors .................... | ❑ No | ❑ Yes |
| Strong association with maladaptive psychosocial factors ...................................................................... (neg. emotions, poor self efficacy, maladaptive beliefs & pain behaviors, conflicts [family, work…]) | ❑ No | ❑ Yes |
| Diffuse or non-anatomic distribution of tenderness to palpation ............................................................. | ❑ No | ❑ Yes |
| Functional Instability (Lumbar Segmental Instability) | ||
|---|---|---|
| Prone passive lumbar extension positive ................................................................................................. | ❑ No | ❑ Yes |
| One or more lumbar hypermobile segment(s) ......................................................................................... | ❑ No | ❑ Yes |
| One or more lumbar hypomobile segments ............................................................................................. | ❑ No | ❑ Yes |
| Other diagnoses | ||
|---|---|---|
| Evidence for other diagnoses (Thoracolumbar syndrome, Piriformis syndrome, Hip pain) ................... | ❑ No | ❑ Yes |
| Leeds Assessment of Neuropathic Symptoms and Signs (LANSS Pain Scale) | |
| Does the pain feel like strange unpleasant sensations on the skin (e.g. pricking, tingling, pins/needles)? .................... 5 | |
| Does skin in the painful area(s) look different (mottled, more red or pink than usual)? ................................................ 5 | |
| Is the skin in the painful area abnormally sensitive to touch? (e.g. lightly stroked, tight clothes) ................................ 3 | |
| Does your pain come on suddenly? (e.g. electric shocks, jumping, or bursting) ........................................................... 2 | |
| Does the pain feel as if the skin temperature in the painful area has changed abnormally (e.g. hot, burning)? ............ 1 | |
| Exam: Does stroking the painful area of skin with cotton produce pain? ...................................................................... 5 | |
| Exam: Does a pinprick at the painful area feel different than a pinprick in an area of normal skin? ............................. 3 | |
| 0 – 12 = likely nociceptive, Score > 12 likely neuropathic | Total: ................................................................ ______ |
| Adapted from: Bennett, M.I. (2001). The LANSS Pain Scale: The Leeds assessment of neuropathic symptoms and signs. Pain, 92(1–2), 147–157. | |
| Neurogenic Claudication Clinical Prediction Rule (Score of ≥ 7) |
| Age 60–70 ........................................................................................................................................................................ 2 |
| Age >70 ........................................................................................................................................................................... 3 |
| Onset over 6 months ....................................................................................................................................................... 1 |
| Symptoms improve when bending forward .................................................................................................................... 2 |
| Symptoms improve when bending backward ............................................................................................................... −2 |
| Symptoms exacerbated while standing ........................................................................................................................... 2 |
| Intermittent claudication symptoms (symptoms while walking and relieved by rest) ................................................... 1 |
| Urinary incontinence ....................................................................................................................................................... 1 |
| Total ....................................................................................................................................................................... _____ |
| Adapted from: Sugioka T, Hayashino Y, Konno S, Kikuchi S, Fukuhara S. Predictive value of self-reported patient information for the identification of lumbar spinal stenosis. Fam Pract 2008;25:237–244. |
Footnotes
Funding support: This work was funded through a grant from the U.S. Department of Health and Human Services, Health Resources Services Administration; grant number 5U19AT004663. This project was conducted in a facility constructed with support from Research Facilities Improvement Grant Number C06 RR15433 from the National Center for Research Resources, National Institutes of Health.
References
- 1.Dagenais S, Tricco AC, Haldeman S. Synthesis of recommendations for the assessment and management of low back pain from recent clinical practice guidelines. Spine J. 2010;10:514–529. doi: 10.1016/j.spinee.2010.03.032. [DOI] [PubMed] [Google Scholar]
- 2.Manchikanti L, Singh V, Pampati V, Damron KS, Barnhill RC, Beyer C, et al. Evaluation of the relative contributions of various structures in chronic low back pain. Pain Physician. 2001;4:308–316. [PubMed] [Google Scholar]
- 3.Smart KM, Blake C, Staines A, Thacker M, Doody C. Mechanisms-based classifications of musculoskeletal pain: part 1 of 3: symptoms and signs of central sensitisation in patients with low back (+/− leg) pain. Man Ther. 2012;17:336–344. doi: 10.1016/j.math.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 4.Garland EL. Pain processing in the human nervous system: a selective review of nociceptive and biobehavioral pathways. Prim Care. 2012;39:561–571. doi: 10.1016/j.pop.2012.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murphy DR, Hurwitz EL. Application of a diagnosis-based clinical decision guide in patients with low back pain. Chiropr Man Therap. 2011;19:26. doi: 10.1186/2045-709X-19-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pincus T, Kent P, Bronfort G, Loisel P, Pransky G, Hartvigsen J. Twenty-five years with the biopsychosocial model of low back pain-is it time to celebrate? A report from the twelfth international forum for primary care research on low back pain. Spine (Phila Pa 1976) 2013;38:2118–2123. doi: 10.1097/BRS.0b013e3182a8c5d6. [DOI] [PubMed] [Google Scholar]
- 7.O’Sullivan P. Diagnosis and classification of chronic low back pain disorders: maladaptive movement and motor control impairments as underlying mechanism. Man Ther. 2005;10:242–255. doi: 10.1016/j.math.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Weiner BK. Spine update: the biopsychosocial model and spine care. Spine (Phila Pa 1976) 2008;33:219–223. doi: 10.1097/BRS.0b013e3181604572. [DOI] [PubMed] [Google Scholar]
- 9.Nicholas MK, George SZ. Psychologically informed interventions for low back pain: an update for physical therapists. Phys Ther. 2011;91:765–776. doi: 10.2522/ptj.20100278. [DOI] [PubMed] [Google Scholar]
- 10.Foster NE, Delitto A. Embedding psychosocial perspectives within clinical management of low back pain: integration of psychosocially informed management principles into physical therapist practice – challenges and opportunities. Phys Ther. 2011;91:790–803. doi: 10.2522/ptj.20100326. [DOI] [PubMed] [Google Scholar]
- 11.Amirdelfan K, McRoberts P, Deer TR. The differential diagnosis of low back pain: a primer on the evolving paradigm. Neuromodulation. 2014;17(Suppl 2):11–17. doi: 10.1111/ner.12173. [DOI] [PubMed] [Google Scholar]
- 12.Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344:363–370. doi: 10.1056/NEJM200102013440508. [DOI] [PubMed] [Google Scholar]
- 13.Spitzer WO LFDM. Scientific approach to the assessment and management of activity-related spinal disorders. A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine (Phila Pa 1976) 1987;12:S1–59. [PubMed] [Google Scholar]
- 14.Chou R, Qaseem A, Snow V, Casey D, Cross JT, Jr, Shekelle P, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 15.Jordan KP, Hayward RA, Blagojevic-Bucknall M, Croft P. Incidence of prostate, breast, lung and colorectal cancer following new consultation for musculoskeletal pain: a cohort study among UK primary care patients. Int J Cancer. 2013;133:713–720. doi: 10.1002/ijc.28055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ben-Galim P, Ben-Galim T, Rand N, Haim A, Hipp J, Dekel S, et al. Hip-spine syndrome: the effect of total hip replacement surgery on low back pain in severe osteoarthritis of the hip. Spine (Phila Pa 1976) 2007;32:2099–2102. doi: 10.1097/BRS.0b013e318145a3c5. [DOI] [PubMed] [Google Scholar]
- 17.Sembrano JN, Polly DW., Jr How often is low back pain not coming from the back? Spine (Phila Pa 1976) 2009;34:E27–E32. doi: 10.1097/BRS.0b013e31818b8882. [DOI] [PubMed] [Google Scholar]
- 18.Wainner RS, Whitman JM, Cleland JA, Flynn TW. Regional interdependence: a musculoskeletal examination model whose time has come. J Orthop Sports Phys Ther. 2007;37:658–660. doi: 10.2519/jospt.2007.0110. [DOI] [PubMed] [Google Scholar]
- 19.Redmond JM, Gupta A, Nasser R, Domb BG. The hip-spine connection: understanding its importance in the treatment of hip pathology. Orthopedics. 2015;38:49–55. doi: 10.3928/01477447-20150105-07. [DOI] [PubMed] [Google Scholar]
- 20.Offierski CM, MacNab I. Hip-spine syndrome. Spine (Phila Pa 1976) 1983;8:316–321. doi: 10.1097/00007632-198304000-00014. [DOI] [PubMed] [Google Scholar]
- 21.Reiman MP, Weisbach PC, Glynn PE. The hips influence on low back pain: a distal link to a proximal problem. J Sport Rehabil. 2009;18:24–32. doi: 10.1123/jsr.18.1.24. [DOI] [PubMed] [Google Scholar]
- 22.Cibulka MT, Sinacore DR, Cromer GS, Delitto A. Unilateral hip rotation range of motion asymmetry in patients with sacroiliac joint regional pain. Spine (Phila Pa 1976) 1998;23:1009–1015. doi: 10.1097/00007632-199805010-00009. [DOI] [PubMed] [Google Scholar]
- 23.Vad VB, Bhat AL, Basrai D, Gebeh A, Aspergren DD, Andrews JR. Low back pain in professional golfers: the role of associated hip and low back range-of-motion deficits. Am J Sports Med. 2004;32:494–497. doi: 10.1177/0363546503261729. [DOI] [PubMed] [Google Scholar]
- 24.Burns SA, Mintken PE, Austin GP, Cleland J. Short-term response of hip mobilizations and exercise in individuals with chronic low back pain: a case series. J Man Manip Ther. 2011;19:100–107. doi: 10.1179/2042618610Y.0000000007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lejkowski PM, Poulsen E. Elimination of intermittent chronic low back pain in a recreational golfer following improvement of hip range of motion impairments. J Bodyw Mov Ther. 2013;17:448–452. doi: 10.1016/j.jbmt.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 26.Stevens K, Tao C, Lee SU, Salem N, Vandevenne J, Cheng C, et al. Subchondral fractures in osteonecrosis of the femoral head: comparison of radiography, CT, and MR imaging. AJR Am J Roentgenol. 2003;180:363–368. doi: 10.2214/ajr.180.2.1800363. [DOI] [PubMed] [Google Scholar]
- 27.Mankin HJ. Nontraumatic necrosis of bone (osteonecrosis) N Engl J Med. 1992;326:1473–1479. doi: 10.1056/NEJM199205283262206. [DOI] [PubMed] [Google Scholar]
- 28.Roshan A, Ram S. The neglected femoral neck fracture in young adults: review of a challenging problem. Clin Med Res. 2008;6:33–39. doi: 10.3121/cmr.2008.752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Min BW, Song KS, Cho CH, Lee SM, Lee KJ. Untreated asymptomatic hips in patients with osteonecrosis of the femoral head. Clin Orthop Relat Res. 2008;466:1087–1092. doi: 10.1007/s11999-008-0191-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Griffith JF, Antonio GE, Kumta SM, Hui DS, Wong JK, Joynt GM, et al. Osteonecrosis of hip and knee in patients with severe acute respiratory syndrome treated with steroids. Radiology. 2005;235:168–175. doi: 10.1148/radiol.2351040100. [DOI] [PubMed] [Google Scholar]
- 31.Iida S, Harada Y, Shimizu K, Sakamoto M, Ikenoue S, Akita T, et al. Correlation between bone marrow edema and collapse of the femoral head in steroid-induced osteonecrosis. AJR Am J Roentgenol. 2000;174:735–743. doi: 10.2214/ajr.174.3.1740735. [DOI] [PubMed] [Google Scholar]
- 32.Marti-Carvajal AJ, Sola I, Agreda-Perez LH. Treatment for avascular necrosis of bone in people with sickle cell disease. Cochrane Database Syst Rev. 2009:CD004344. doi: 10.1002/14651858.CD004344.pub3. [DOI] [PubMed] [Google Scholar]
- 33.Liu YF, Chen WM, Lin YF, Yang RC, Lin MW, Li LH, et al. Type II collagen gene variants and inherited osteonecrosis of the femoral head. N Engl J Med. 2005;352:2294–2301. doi: 10.1056/NEJMoa042480. [DOI] [PubMed] [Google Scholar]
- 34.Lee MS, Hsieh PH, Shih CH, Wang CJ. Non-traumatic osteonecrosis of the femoral head – from clinical to bench. Chang Gung Med J. 2010;33:351–360. [PubMed] [Google Scholar]
- 35.Rajpura A, Wright AC, Board TN. Medical management of osteonecrosis of the hip: a review. Hip Int. 2011;21:385–392. doi: 10.5301/HIP.2011.8538. [DOI] [PubMed] [Google Scholar]
- 36.Carabelli RA, Goldman M. Avascular necrosis. A case report. Phys Ther. 1987;67:542–544. doi: 10.1093/ptj/67.4.542. [DOI] [PubMed] [Google Scholar]
- 37.Pajaczkowski JA. The stubborn hip: idiopathic avascular necrosis of the hip. J Manipulative Physiol Ther. 2003;26:107. doi: 10.1067/mmt.2003.13. [DOI] [PubMed] [Google Scholar]
- 38.Karim R, Goel KD. Avascular necrosis of the hip in a 41-year-old male: a case study. J Can Chiropr Assoc. 2004;48:137–141. [PMC free article] [PubMed] [Google Scholar]
- 39.Xia T, Wilder DG, Gudavalli MR, DeVocht JW, Vining RD, Pohlman KA, et al. Study protocol for patient response to spinal manipulation – a prospective observational clinical trial on physiological and patient-centered outcomes in patients with chronic low back pain. BMC Complement Altern Med. 2014;14:292. doi: 10.1186/1472-6882-14-292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vining R, Potocki E, Seidman M, Morgenthal AP. An evidence-based diagnostic classification system for low back pain. J Can Chiropr Assoc. 2013;57:189–204. [PMC free article] [PubMed] [Google Scholar]
- 41.Bennett M. The LANSS Pain Scale: the Leeds assessment of neuropathic symptoms and signs. Pain. 2001;92:147–157. doi: 10.1016/s0304-3959(00)00482-6. [DOI] [PubMed] [Google Scholar]
- 42.Marchiori D. Clinical Imaging: With Skeletal, Chest and Abdomen Pattern Differentials. 2 ed. Elsevier Health Sciences; 2004. [Google Scholar]
- 43.U.S.Department of Health & Human Services, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism Helping Patients Who Drink Too Much, A Clinician’s Guide, Updated 2005 Edition. 2005.
- 44.Gerhardt MB, Romero AA, Silvers HJ, Harris DJ, Watanabe D, Mandelbaum BR. The prevalence of radiographic hip abnormalities in elite soccer players. Am J Sports Med. 2012;40:584–588. doi: 10.1177/0363546511432711. [DOI] [PubMed] [Google Scholar]
- 45.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis – what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 46.Martin HD, Kelly BT, Leunig M, Philippon MJ, Clohisy JC, Martin RL, et al. The pattern and technique in the clinical evaluation of the adult hip: the common physical examination tests of hip specialists. Arthroscopy. 2010;26:161–172. doi: 10.1016/j.arthro.2009.07.015. [DOI] [PubMed] [Google Scholar]
- 47.Rahman LA, Adie S, Naylor JM, Mittal R, So S, Harris IA. A systematic review of the diagnostic performance of orthopedic physical examination tests of the hip. BMC Musculoskelet Disord. 2013;14:257. doi: 10.1186/1471-2474-14-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reiman MP, Goode AP, Hegedus EJ, Cook CE, Wright AA. Diagnostic accuracy of clinical tests of the hip: a systematic review with meta-analysis. Br J Sports Med. 2013;47:893–902. doi: 10.1136/bjsports-2012-091035. [DOI] [PubMed] [Google Scholar]
- 49.Maslowski E, Sullivan W, Forster HJ, Gonzalez P, Kaufman M, Vidal A, et al. The diagnostic validity of hip provocation maneuvers to detect intra-articular hip pathology. PM R. 2010;2:174–181. doi: 10.1016/j.pmrj.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 50.van Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Spinal radiographic findings and nonspecific low back pain. A systematic review of observational studies. Spine (Phila Pa 1976) 1997;22:427–434. doi: 10.1097/00007632-199702150-00015. [DOI] [PubMed] [Google Scholar]
- 51.Reis AC, Rabelo ND, Pereira RP, Polesello G, Martin RL, Garcia Lucareli PR, et al. Radiological examination of the hip – clinical indications, methods, and interpretation: a clinical commentary. Int J Sports Phys Ther. 2014;9:256–267. [PMC free article] [PubMed] [Google Scholar]
- 52.Etienne G, Mont MA, Ragland PS. The diagnosis and treatment of nontraumatic osteonecrosis of the femoral head. Instr Course Lect. 2004;53:67–85. [PubMed] [Google Scholar]
- 53.Malizos KN, Karantanas AH, Varitimidis SE, Dailiana ZH, Bargiotas K, Maris T. Osteonecrosis of the femoral head: etiology, imaging and treatment. Eur J Radiol. 2007;63:16–28. doi: 10.1016/j.ejrad.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 54.Amanatullah DF, Strauss EJ, Di Cesare PE. Current management options for osteonecrosis of the femoral head: part 1, diagnosis and nonoperative management. Am J Orthop (Belle Mead NJ) 2011;40:E186–E192. [PubMed] [Google Scholar]
- 55.Cui Q, Wang Y, Saleh KJ, Wang GJ, Balian G. Alcohol-induced adipogenesis in a cloned bone-marrow stem cell. J Bone Joint Surg Am. 2006;88(Suppl 3):148–154. doi: 10.2106/JBJS.F.00534. [DOI] [PubMed] [Google Scholar]
- 56.Zalavras CG, Lieberman JR. Osteonecrosis of the femoral head: evaluation and treatment. J Am Acad Orthop Surg. 2014;22:455–464. doi: 10.5435/JAAOS-22-07-455. [DOI] [PubMed] [Google Scholar]
- 57.Lieberman JR, Berry DJ, Mont MA, Aaron RK, Callaghan JJ, Rajadhyaksha AD, et al. Osteonecrosis of the hip: management in the 21st century. Instr Course Lect. 2003;52:337–355. [PubMed] [Google Scholar]
- 58.Gebhard KL, Maibach HI. Relationship between systemic corticosteroids and osteonecrosis. Am J Clin Dermatol. 2001;2:377–388. doi: 10.2165/00128071-200102060-00004. [DOI] [PubMed] [Google Scholar]
- 59.Ficat RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg Br. 1985;67:3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 60.Mont MA, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: ten years later. J Bone Joint Surg Am. 2006;88:1117–1132. doi: 10.2106/JBJS.E.01041. [DOI] [PubMed] [Google Scholar]
- 61.Kaushik AP, Das A, Cui Q. Osteonecrosis of the femoral head: An update in year 2012. World J Orthop. 2012;3:49–57. doi: 10.5312/wjo.v3.i5.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mont MA, Rajadhyaksha AD, Hungerford DS. Outcomes of limited femoral resurfacing arthroplasty compared with total hip arthroplasty for osteonecrosis of the femoral head. J Arthroplasty. 2001;16:134–139. doi: 10.1054/arth.2001.28722. [DOI] [PubMed] [Google Scholar]
- 63.Springer BD, Connelly SE, Odum SM, Fehring TK, Griffin WL, Mason JB, et al. Cementless femoral components in young patients: review and meta-analysis of total hip arthroplasty and hip resurfacing. J Arthroplasty. 2009;24:2–8. doi: 10.1016/j.arth.2009.04.032. [DOI] [PubMed] [Google Scholar]