Abstract
Few examples of interprofessional collaboration by chiropractors and other healthcare professionals are available. This case report describes an older adult with complex low back pain and longstanding tobacco use who received collaborative healthcare while enrolled in a clinical trial. This 65 year-old female retired office worker presented with chronic back pain. Imaging findings included disc extrusion and spinal stenosis. Multiple co-morbidities and the complex nature of this case substantiated the need for multidisciplinary collaboration. A doctor of chiropractic and a doctor of osteopathy provided collaborative care based on patient goal setting and supported by structured interdisciplinary communication, including record sharing and telephone consultations. Chiropractic and medical interventions included spinal manipulation, exercise, tobacco reduction counseling, analgesic use, nicotine replacement, dietary and ergonomic recommendations, and stress reduction strategies. Collaborative care facilitated active involvement of the patient and resulted in decreased radicular symptoms, improvements in activities of daily living, and tobacco use reduction.
Keywords: chiropractic, integrative medicine, interdisciplinary communication, low back pain, patient-centered care, radiculopathy, spinal manipulation, tobacco use cessation
Abstract
Il y a peu d’exemples de collaboration interprofessionnelle entre les chiropraticiens et d’autres professionnels de la santé. Cette étude de cas décrit une personne âgée souffrant d’une lombalgie complexe et de tabagisme de longue date qui a reçu des soins de santé en collaboration pendant qu’elle participait à un essai clinique. Cette employée de bureau à la retraite âgée de 65 ans souffrait d’une lombalgie chronique. Les examens d’imagerie ont révélé des extrusions discales et une sténose rachidienne. Des comorbidités multiples et la nature complexe de ce cas ont justifié la nécessité d’une collaboration multidisciplinaire. Un chiropraticien et un ostéopathe ont fourni des soins en collaboration selon les objectifs établis pour la patiente et soutenus par une communication interdisciplinaire structurée, y compris le partage du dossier et des consultations téléphoniques. Les interventions chiropratiques et médicales étaient notamment axées sur la manipulation vertébrale, l’exercice, des conseils sur la réduction de l’usage du tabac, l’utilisation d’analgésiques, le remplacement de la nicotine, des recommandations diététiques et ergonomiques, et des stratégies de réduction du stress. Les soins en collaboration ont facilité la participation active de la patiente et ont entraîné une diminution des symptômes radiculaires, des améliorations dans les activités de la vie quotidienne, et la réduction de l’usage du tabac.
Keywords: chiropratique, médecine intégrative, communication interdisciplinaire, lombalgie, soins centrés sur le patient, radiculopathie, manipulation vertébrale, cessation du tabagisme
Introduction
Older adults with low back pain (LBP) often represent a complex clinical picture due to the inherent challenges of treating LBP especially when combined with multiple co-morbidities.1–4 Given the potential for such complexity, it is important for clinicians and patients to consider these elements as management plans are designed and implemented.2,5 Multidisciplinary collaborative care including care coordination among providers is one possible approach to the management of complex LBP.1,2,6,7
Boon and colleagues defined collaborative care as “an interprofessional process for communication and decision making that enables the separate and shared knowledge and skills of health providers to synergistically influence patient care.”8,9 Successful collaboration requires patient interest and involvement10–12, mutual respect9,10,12, maintenance of professional autonomy8,13,14, understanding each team members’ practice scope9,13,15–17, goal setting9,10,13, and an openness to discussion and consensus building processes13. Communication models that may support interprofessional collaboration include telephone consultations10,18–20 or face-to-face meetings10,16,18,21, job shadowing experiences9,16,20, use of electronic medical records9,14,18, and confirming understanding among team members12,19,21.
This case presentation describes a collaborative effort between healthcare providers and a patient enrolled in a clinical trial on interdisciplinary co-management of older adults with LBP.20,22 The trial randomly allocated eligible participants to receive 12-weeks of LBP care under 1 of 3 professional practice models: medical care; concurrent medical and chiropractic care; or collaborative care involving the patient and a medical and chiropractic co-management team. The co-management team collaborated through scheduled phone consultations and a secure, web-based, electronic communication system to share health records between the different health systems involved.20 The interprofessional practice model emphasized patient goal setting; provider discussions of diagnoses, complicating factors and challenges to treatment; a cooperative treatment approach; monitoring patient status and care challenges; and ongoing support of the patient’s treatment goals.20 The co-managing practitioners in this case were a doctor of chiropractic (DC) working at a chiropractic research center and a doctor of osteopathy (DO) completing a residency in family medicine. This case report discusses the collaboration process of a DC, DO, and patient engaged in the management of complex LBP in an older adult.
Case presentation
Clinical history
A 65 year-old female retired office worker presented with LBP and constant radiation to the left gluteal and posterior thigh regions with occasional radiation to the great toe. The LBP first occurred 30 years prior when the patient acquired a flexed and twisted trunk position causing immediate and severe pain. Daily activities became progressively affected, albeit gradually over 30 years.
This patient’s healthcare seeking for her LBP depicted a common fragmented patient care history of being ‘in the system.’23 This fragmented care included multiple primary care evaluations, specialist referrals, repeated imaging studies, minimal attention to co-morbid conditions potentially complicating her LBP, consultations with complementary and alternative providers, and an overall lack of care coordination.
Thirty-four months prior to examination in our clinic, the patient underwent a lumbar magnetic resonance imaging (MRI) scan and an orthopaedic evaluation, which included lumbar radiographs. She then received corticosteroid injections that relieved the pain extending below the knee. Subsequently, the patient received chiropractic care with another provider 6 months prior to our examination. Care from medical and chiropractic providers resulted in partial, temporary improvement. At our initial evaluation, symptoms were severe enough to cause sleep interruption and interfere substantially with activities of daily living (ADL).
Examination
The patient reported her LBP at a level of 6 of 10 on the 0–10 numeric rating scale for pain. Examination findings included limited lumbar extension, radiating pain to the left posterior thigh with Valsalva’s maneuver and during a brief walking test24, and a positive straight leg raise test with radiation to the posterior thigh.
Imaging
Lumbar radiographs obtained from the prior orthopaedic evaluation demonstrated disc narrowing at L4-5 and L5-S1, endplate osteophytosis in the lower thoracic region and throughout the lumbar spine, a 21° left lumbar convexity, mild osteoporosis, arteriosclerotic calcification of the abdominal aorta, calcification within the pelvis consistent with a uterine fibroid, and evidence of abdominal surgery consistent with a history of bariatric surgery and cholecystectomy (Figures 1 and 2). Previous lumbar MRI demonstrated L5-S1 left para-central disc extrusion with slight displacement of the left S1 nerve root and severe bilateral neural foraminal stenosis. At L4-5 there was mild/moderate central canal stenosis, a small central disc protrusion and bilateral foraminal stenosis.
Figure 1.
Lateral lumbar spine x-ray: showing arteriosclerotic calcification of the abdominal aorta (short arrow), osteophytes throughout the lumbar spine, and advanced disc degeneration at L4-5, L5-S1 (long arrows).
Figure 2.
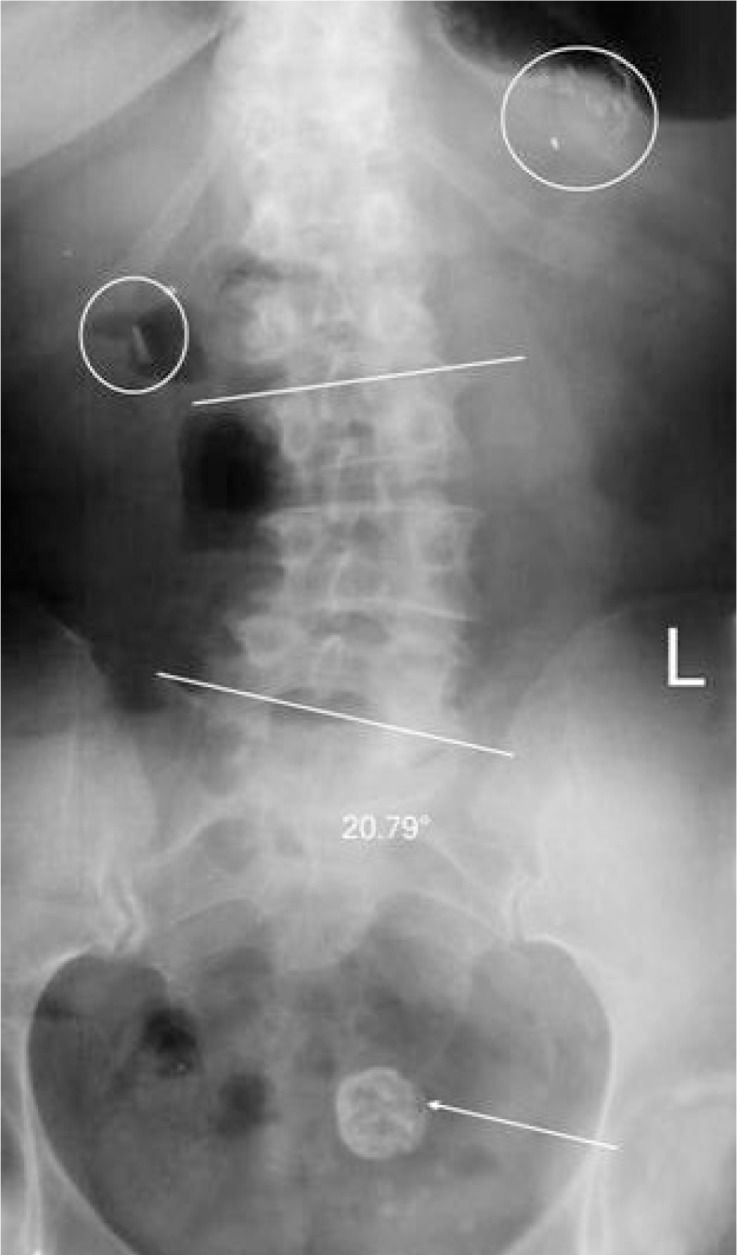
A-P lumbar x-ray: showing a 21° lumbar curvature, surgical clips (circled) and a 2.6 cm diameter density consistent with uterine fibroid (arrow).
Diagnosis
DC evaluation revealed a diagnosis of non-compressive lumbar radiculopathy and neurogenic claudication.25 The examining DO documented a diagnosis of chronic LBP due to a previous injury. Though a straight leg raise test produced symptoms in the posterior thigh, examination by both providers revealed no conclusive evidence for the clinical presentation of compressive radiculopathy despite MRI evidence of nerve root displacement and foraminal stenosis. Table 1 presents the patient’s clinical history and concurrent conditions. Notably, there was a 45-year smoking history (1.5–2 packs of cigarettes/ day), obesity, physical inactivity, and significant ADL impairment.
Table 1.
Clinical history and concurrent conditions
| Diagnosis | Health History and Current Status |
|---|---|
| Spinal conditions | |
| Activities of daily living impairments |
|
| Tobacco dependence |
|
| Obesity |
|
| Mental health conditions |
|
| Benign positional vertigo |
|
| Cardiovascular conditions |
|
Case management
LBP management
Treatment goals were determined jointly at the first chiropractic visit by the DC and patient as: 1) reduction of LBP, 2) improved psychological management of chronic pain and 3) improved ability to perform ADLs. Specifically, the patient hoped to participate in gardening activities with less pain. Goal 1 was addressed by manual lumbar distraction, gentle high velocity manipulation at the left sacroiliac joint26–29, and manual ischemic compression of associated hypertonic muscles30,31. Goal 2 was supported by the recommendation of a mindfulness meditation technique as a strategy to help manage stress and assist with pain reduction.32 Goal 3 was supported by the in-office chiropractic treatments and home exercise recommendations consisting of gentle stretching exercises with trunk motions and brisk walking to tolerance.33,34 The DC advised tobacco cessation, although this was not a high priority for the patient at first.
The DO initiated a similar goal-setting process, identifying short-term pain management as an objective. To achieve this goal, the DO recommended acetaminophen, emphasizing appropriate dosing and side effects. Weight reduction through physical activity was explored, but no acceptable options were identified as exercise increased the patient’s LBP. The patient agreed to attempt weight reduction through diet modification. The DO also recommended continuation of chiropractic care.
Tobacco cessation
During the initial DO visit, the patient expressed that her addiction to tobacco was troubling because she was aware it worsened her LBP recovery prognosis. These concerns motivated her and the DO to initiate a trial of nicotine replacement therapy to facilitate smoking reduction. After a review of previous medication use for smoking cessation and prior side effects, a nicotine patch was prescribed.
During a subsequent visit, the DC recommended an additional supportive measure of a Personal Quit Plan (PQP), developed during a 30-minute consultation that included the association of smoking and chronic LBP.35 The PQP was developed for use by DCs,36 based on the American Cancer Society’s Guide to Quit Smoking37. The written PQP included reasons for tobacco cessation, financial implications, a plan for support by family and friends, and a quit date. Additional suggestions included replacements for social cues of tobacco use, stress reduction through breathing and meditation techniques, and behavioral changes, such as removing cigarettes and ashtrays, increased engagement in enjoyable activities such as gardening and constructing puzzles, and drinking water. The patient’s PQP was shared with the DO through the secure health record website. Collaborative communications between the patient and providers confirmed the smoking reduction goal and reinforced team member roles. A summary of interprofessional communications is provided in Table 2.
Table 2.
Interprofessional communications during case co-management
| Week | Communication Type | Patient Goals | Interprofessional Communication Summary |
|---|---|---|---|
| 1 | Treatment summary/DC |
|
|
| 3 | Treatment summary/DO |
|
|
| 4 | Phone call summary/DO Phone call summary/DC |
|
|
| 5 | Health records/DC |
|
|
| 6 | Treatment summary/DC |
|
|
| 12 | Phone call summary/DO Phone call summary/DC |
Future recommendations
|
|
| 14 | Treatment summary/DC |
|
|
Outcomes
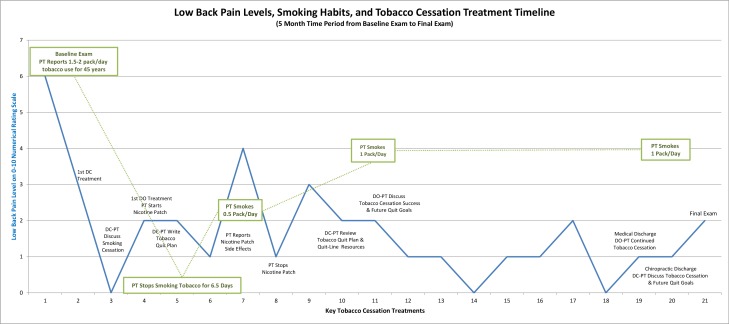
Figure 3 depicts the patient’s LBP outcomes, smoking habits, and tobacco cessation efforts during the trial. The patient rated her LBP at 1–2 on the 0–10 numerical rating scale at the end of the 12-week intervention, down from 6/10 at baseline. She reported performing some gardening activity, yard-work, and housework with less pain and a reduced amount of pain medication. Both providers made final recommendations, which included continued walking and exercises to improve core stability, acetaminophen for pain relief, limited heavy lifting and twisting motions, and chiropractic and/or medical care as needed.
Figure 3.
Low Back Pain Levels, Smoking Habits, and Tobacco Cessation Treatment Timeline
The patient ceased smoking for 6.5 consecutive days. She discontinued the nicotine patch and resumed tobacco use after experiencing increased psychological stress, LBP, and a side effect of skin irritation. At a subsequent visit to the DO, the patient expressed frustration that “her quitting efforts had been a failure.” The DO congratulated the patient, stating “this was a victory and not a defeat.” The patient considered further smoking cessation efforts, but expressed concern over dealing with life and family stressors without smoking as a coping mechanism. Both providers encouraged continued smoking cessation efforts following discharge.
Discussion
While best practices for chiropractic care recommend multidisciplinary management when appropriate2, there are few examples available in the scientific literature of interprofessional collaboration that describe chiropractic patients of any age7,9,17,38, much less for older adults with complex LBP2,17,39. This 65-year old female patient exhibited chronic LBP diagnosed as non-compressive lumbar radiculopathy and neurogenic claudication complicated by spinal curvature and degeneration, obesity, physical inactivity, impaired ADLs, life stresses, cardiovascular disease, and long standing tobacco use.
Some clinical guidelines support comprehensive multidisciplinary approaches for LBP management, with collaboration encouraged between practitioners40, while others note the effectiveness of such treatments has not been compared to less intensive programs41. Although chiropractic may be delivered concurrently with medical services42, care coordination or collaboration between patients and providers may not occur13,19,43. Co-management, referral, and health record sharing between medical doctors and DCs is often limited7,42,44–48 and may result in care fragmentation9. Patients and providers may not discuss the concurrent use of conventional and complementary medicine43, which precludes the opportunity for integrated care and may impact “efficiency, quality, and patient safety in health care delivery systems”44. Collaborative care can be essential in expediting timely referral for complicated geriatric conditions.49,50
In the case reported here, tobacco cessation was a main focus of care coordination. The Council on Chiropractic Education urges chiropractors to provide information and resources to every patient who smokes and indicates a willingness to attempt smoking cessation.51 Both providers evaluated this patient’s tobacco use history, reviewed the relationship between LBP and smoking, and encouraged tobacco cessation both as a pain management strategy and as beneficial for overall health.35,37,52–55 The patient successfully refrained from cigarette smoking for 6.5 days, the longest reported cessation in her 45-year smoking history.
This case supports the concept of improving the effectiveness of health care for chronic LBP in older adults by information sharing and coordinated decision making between practitioners and by incorporating the patient as an active member of the treatment team.10,11 A recent focus group study demonstrated older adults’ interest in LBP co-management by chiropractors and medical physicians.19 Indicators of successful co-management valued by older adults in the study included “patient-centered communication, collegial interdisciplinary interactions between these providers, and health record sharing”.19 Another qualitative study on treatment coordination in primary care models reported that while continuity and information sharing is important, they are not adequate to provide care coordination for complex health conditions, and patient participation in decision-making must also be incorporated.9–11,14
Conclusion
This case report demonstrated interprofessional collaboration in the treatment of an older adult with complex low back pain and tobacco use by a DC and a DO. Collaboration may improve the treatment effectiveness of musculoskeletal disorders which are often multifactorial in causation. Effective collaboration encompassed interactions between diverse health practitioners and the patient’s opinions and preferences. This healthcare team used a patient-centered approach that included the patient’s participation in goal setting and attainment, health record sharing, structured interdisciplinary communications, and cooperative treatment plans. For successful implementation, a collaborative care model must be specifically selected and tailored for the practice settings involved.
Acknowledgments
The authors extend appreciation to the patient for actively participating and expressing opinions regarding her health care plan to her providers and for her willingness to share her experience in this case report. We also thank the Genesis Family Medical Center osteopathic physician who co-managed the care of this patient and fostered a team approach as well as Christine Goertz DC, PhD, principal investigator for the clinical trial, and the clinic staff at the Palmer Center for Chiropractic Research who coordinated study activities.
Footnotes
Disclaimers:
No conflicts of interest and no disclaimers to declare.
Consent:
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review.
Funding support:
This work was funded through a grant from the U.S. Department of Health and Human Services, Health Resources Services Administration; grant number R18-HP-15126. This project was conducted in a facility constructed with support from Research Facilities Improvement Grant Number C06 RR15433 from the National Center for Research Resources, National Institutes of Health.
Trial registration:
References
- 1.Dougherty P, Hawk C, Weiner D, Gleberzon B, Andrew K, Killinger L. The role of chiropractic care in older adults. Chiropr Man Therap. 2012;20:3. doi: 10.1186/2045-709X-20-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hawk C, Schneider M, Dougherty P, Gleberzon BJ, Killinger LZ. Best practices recommendations for chiropractic care for older adults: results of a consensus process. J Manipulative Physiol Ther. 2010;33:464–473. doi: 10.1016/j.jmpt.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 3.Killinger LZ. Diagnostic challenges in the older patient. Chiropr Man Therap. 2012;20:28. doi: 10.1186/2045-709X-20-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van den Bussche H, Koller D, Kolonko T, Hansen H, Wegscheider K, Glaeske G, et al. Which chronic diseases and disease combinations are specific to multimorbidity in the elderly? Results of a claims data based cross-sectional study in Germany. BMC Public Health. 2011;11:101. doi: 10.1186/1471-2458-11-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guiding principles for the care of older adults with multimorbidity: an approach for clinicians: American Geriatrics Society Expert Panel on the Care of Older Adults with Multimorbidity. J Am Geriatr Soc. 2012;60:E1–E25. doi: 10.1111/j.1532-5415.2012.04188.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mior S, Barnsley J, Boon H, Ashbury FD, Haig R. Designing a framework for the delivery of collaborative musculoskeletal care involving chiropractors and physicians in community-based primary care. J Interprof Care. 2010;24:678–689. doi: 10.3109/13561821003608757. [DOI] [PubMed] [Google Scholar]
- 7.Mior S, Gamble B, Barnsley J, Cote P, Cote E. Changes in primary care physician’s management of low back pain in a model of interprofessional collaborative care: an uncontrolled before-after study. Chiropr Man Therap. 2013;21:6. doi: 10.1186/2045-709X-21-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boon H, Verhoef M, O’Hara D, Findlay B. From parallel practice to integrative health care: a conceptual framework. BMC Health Serv Res. 2004;4:15. doi: 10.1186/1472-6963-4-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riva JJ, Muller GD, Hornich AA, Mior SA, Gupta A, Burnie SJ. Chiropractors and collaborative care: An overview illustrated with a case report. J Can Chiropr Assoc. 2010;54:147–154. [PMC free article] [PubMed] [Google Scholar]
- 10.Banfield M, Gardner K, McRae I, Gillespie J, Wells R, Yen L. Unlocking information for coordination of care in Australia: a qualitative study of information continuity in four primary health care models. BMC Fam Pract. 2013;14:34. doi: 10.1186/1471-2296-14-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parsons S, Harding G, Breen A, Foster N, Pincus T, Vogel S, et al. Will shared decision making between patients with chronic musculoskeletal pain and physiotherapists, osteopaths and chiropractors improve patient care? Fam Pract. 2012;29:203–212. doi: 10.1093/fampra/cmr083. [DOI] [PubMed] [Google Scholar]
- 12.Levinson W, Lesser CS, Epstein RM. Developing physician communication skills for patient-centered care. Health Aff (Millwood) 2010;29:1310–1318. doi: 10.1377/hlthaff.2009.0450. [DOI] [PubMed] [Google Scholar]
- 13.Boon HS, Mior SA, Barnsley J, Ashbury FD, Haig R. The difference between integration and collaboration in patient care: results from key informant interviews working in multiprofessional health care teams. J Manipulative Physiol Ther. 2009;32:715–722. doi: 10.1016/j.jmpt.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 14.King G, O’Donnell C, Boddy D, Smith F, Heaney D, Mair FS. Boundaries and e-health implementation in health and social care. BMC Med Inform Decis Mak. 2012;12:100. doi: 10.1186/1472-6947-12-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eisenberg DM, Buring JE, Hrbek AL, Davis RB, Connelly MT, Cherkin DC, et al. A model of integrative care for low-back pain. J Altern Complement Med. 2012;18:354–362. doi: 10.1089/acm.2011.0408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Riva JJ, Lam JM, Stanford EC, Moore AE, Endicott AR, Krawchenko IE. Interprofessional education through shadowing experiences in multi-disciplinary clinical settings. Chiropr Osteopat. 2010;18:31. doi: 10.1186/1746-1340-18-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gleberzon BJ. Chiropractic care of the older person: developing an evidence-based approach. J Can Chiropr Assoc. 2001;45:156–171. [Google Scholar]
- 18.Ganz DA, Fung CH, Sinsky CA, Wu S, Reuben DB. Key elements of high-quality primary care for vulnerable elders. J Gen Intern Med. 2008;23:2018–2023. doi: 10.1007/s11606-008-0808-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lyons KJ, Salsbury SA, Hondras MA, Jones ME, Andresen AA, Goertz CM. Perspectives of older adults on co-management of low back pain by doctors of chiropractic and family medicine physicians: a focus group study. BMC Complement Altern Med. 2013;13:225. doi: 10.1186/1472-6882-13-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goertz CM, Salsbury SA, Vining RD, Long CR, Andresen AA, Jones ME, et al. Collaborative care for older adults with low back pain by family medicine physicians and doctors of chiropractic (COCOA): study protocol for a randomized controlled trial. Trials. 2013;14:18. doi: 10.1186/1745-6215-14-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maiers MJ, Westrom KK, Legendre CG, Bronfort G. Integrative care for the management of low back pain: use of a clinical care pathway. BMC Health Serv Res. 2010;10:298. doi: 10.1186/1472-6963-10-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goertz C, Lyons SS, Andresen A, Hondras M, Jones M, Killinger LZ, et al. Collaborative care for older adults (COCOA), Palmer College of Chiropractic. J Allied Health. 2010;39(Suppl 1):e135–e136. [PubMed] [Google Scholar]
- 23.Walker J, Holloway I, Sofaer B. In the system: the lived experience of chronic back pain from the perspectives of those seeking help from pain clinics. Pain. 1999;80:621–628. doi: 10.1016/S0304-3959(98)00254-1. [DOI] [PubMed] [Google Scholar]
- 24.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 25.Vining R, Potocki E, Seidman M, Morgenthal AP. An evidence-based diagnostic classification system for low back pain. J Can Chiropr Assoc. 2013;57:189–204. [PMC free article] [PubMed] [Google Scholar]
- 26.Cox JM. Low Back Pain Mechanism, Diagnosis, and Treatment. 7th ed. Wolters Kluwer/Lippincott Williams and Wilkins; 2001. [Google Scholar]
- 27.Murphy DR, Hurwitz EL, Gregory AA, Clary R. A non-surgical approach to the management of lumbar spinal stenosis: a prospective observational cohort study. BMC Musculoskelet Disord. 2006;7:16. doi: 10.1186/1471-2474-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Snow GJ. Chiropractic management of a patient with lumbar spinal stenosis. J Manipulative Physiol Ther. 2001;24:300–304. doi: 10.1067/mmt.2001.114359. [DOI] [PubMed] [Google Scholar]
- 29.Hondras MA, Long CR, Cao Y, Rowell RM, Meeker WC. A randomized controlled trial comparing 2 types of spinal manipulation and minimal conservative medical care for adults 55 years and older with subacute or chronic low back pain. J Manipulative Physiol Ther. 2009;32:330–343. doi: 10.1016/j.jmpt.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 30.Moraska AF, Hickner RC, Kohrt WM, Brewer A. Changes in blood flow and cellular metabolism at a myofascial trigger point with trigger point release (ischemic compression): a proof-of-principle pilot study. Arch Phys Med Rehabil. 2013;94:196–200. doi: 10.1016/j.apmr.2012.08.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Iglesias-Gonzalez JJ, Munoz-Garcia MT, Rodrigues-de-Souza DP, Alburquerque-Sendin F, Fernandez-de-las-Penas C. Myofascial trigger points, pain, disability, and sleep quality in patients with chronic nonspecific low back pain. Pain Med. 2013;14:1964–1970. doi: 10.1111/pme.12224. [DOI] [PubMed] [Google Scholar]
- 32.Esmer G, Blum J, Rulf J, Pier J. Mindfulness-based stress reduction for failed back surgery syndrome: a randomized controlled trial. J Am Osteopath Assoc. 2010;110:646–652. [PubMed] [Google Scholar]
- 33.Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005;142:776–785. doi: 10.7326/0003-4819-142-9-200505030-00014. [DOI] [PubMed] [Google Scholar]
- 34.Shnayderman I, Katz-Leurer M. An aerobic walking programme versus muscle strengthening programme for chronic low back pain: a randomized controlled trial. Clin Rehabil. 2013;27:207–214. doi: 10.1177/0269215512453353. [DOI] [PubMed] [Google Scholar]
- 35.Alkherayf F, Agbi C. Cigarette smoking and chronic low back pain in the adult population. Clin Invest Med. 2009;32:E360–E367. doi: 10.25011/cim.v32i5.6924. [DOI] [PubMed] [Google Scholar]
- 36.Gordon JS, Istvan J, Haas M. Tobacco cessation via doctors of chiropractic: results of a feasibility study. Nicotine Tob Res. 2010;12:305–308. doi: 10.1093/ntr/ntp203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wai EK, Rodriguez S, Dagenais S, Hall H. Evidence-informed management of chronic low back pain with physical activity, smoking cessation, and weight loss. Spine J. 2008;8:195–202. doi: 10.1016/j.spinee.2007.10.024. [DOI] [PubMed] [Google Scholar]
- 38.Rubis LM, Rubis D, Winchester B. A collaborative approach between chiropractic and dentistry to address temporomandibular dysfunction: a case report. J Chiropr Med. 2014;13:55–61. doi: 10.1016/j.jcm.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Paeck T, Ferreira ML, Sun C, Lin CW, Tiedemann A, Maher CG. Are older adults missing from low back pain clinical trials? – A systematic review and meta-analysis. Arthritis Care Res (Hoboken) 2013;66(8):1220–1226. doi: 10.1002/acr.22261. [DOI] [PubMed] [Google Scholar]
- 40.Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15(Suppl 2):S192–S300. doi: 10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chou R. Low back pain (chronic) BMJ Clin Evid (Online) 2010;2010:1116. [PMC free article] [PubMed] [Google Scholar]
- 42.Weigel PA, Hockenberry JM, Bentler SE, Kaskie B, Wolinsky FD. Chiropractic episodes and the co-occurrence of chiropractic and health services use among older Medicare beneficiaries. J Manipulative Physiol Ther. 2012;35:168–175. doi: 10.1016/j.jmpt.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kaczorowski J, Patterson C, Arthur H, Mith KS, Mills DA. Complementary therapy involvement of physicians: implications for practice and learning. Complement Ther Med. 2002;10:134–140. doi: 10.1016/s0965229902000857. [DOI] [PubMed] [Google Scholar]
- 44.Greene BR, Smith M, Allareddy V, Haas M. Referral patterns and attitudes of primary care physicians towards chiropractors. BMC Complement Altern Med. 2006;6:5. doi: 10.1186/1472-6882-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Greene BR, Smith M, Haas M, Allareddy V. How often are physicians and chiropractors provided with patient information when accepting referrals? J Ambul Care Manage. 2007;30:344–346. doi: 10.1097/01.JAC.0000290403.89284.e0. [DOI] [PubMed] [Google Scholar]
- 46.Smith M, Greene BR, Haas M, Allareddy V. Intra-professional and inter-professional referral patterns of chiropractors. Chiropr Osteopat. 2006;14:12. doi: 10.1186/1746-1340-14-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smith M, Green B, Haas M, Liao J. First report on a US project analyzing chiropractic and medical interprofessional relationships. J Interprof Care. 2004;18:320–321. doi: 10.1080/13561820410001731368. [DOI] [PubMed] [Google Scholar]
- 48.Hawk C, Long CR, Boulanger KT, Morschhauser E, Fuhr AW. Chiropractic care for patients aged 55 years and older: report from a practice-based research program. J Am Geriatr Soc. 2000;48:534–545. doi: 10.1111/j.1532-5415.2000.tb05000.x. [DOI] [PubMed] [Google Scholar]
- 49.Wong JJ, Dufton J, Mior SA. Spontaneous conus medullaris infarction in a 79 year-old female with cardiovascular risk factors: a case report. J Can Chiropr Assoc. 2012;56:58–65. [PMC free article] [PubMed] [Google Scholar]
- 50.Marchand AA, Wong JJ. Conservative management of idiopathic anterior atlantoaxial subluxation without neurological deficits in an 83-year-old female: A case report. J Can Chiropr Assoc. 2014;58:76–84. [PMC free article] [PubMed] [Google Scholar]
- 51.Evans MW, Jr, Rupert R. The Council on Chiropractic Education’s new wellness standard: a call to action for the chiropractic profession. Chiropr Osteopat. 2006;14:23. doi: 10.1186/1746-1340-14-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shiri R, Karppinen J, Leino-Arjas P, Solovieva S, Viikari-Juntura E. The association between smoking and low back pain: a meta-analysis. Am J Med. 2010;123:87–35. doi: 10.1016/j.amjmed.2009.05.028. [DOI] [PubMed] [Google Scholar]
- 53.Fishbain DA, Lewis JE, Cutler R, Cole B, Steele RR, Rosomoff HL. Does smoking status affect multidisciplinary pain facility treatment outcome? Pain Med. 2008;9:1081–1090. doi: 10.1111/j.1526-4637.2007.00306.x. [DOI] [PubMed] [Google Scholar]
- 54.Wu HL, Ding WY, Shen Y, Zhang YZ, Guo JK, Sun YP, et al. Prevalence of vertebral endplate modic changes in degenerative lumbar scoliosis and its associated factors analysis. Spine (Phila Pa 1976) 2012;37:1958–1964. doi: 10.1097/BRS.0b013e31825bfb85. [DOI] [PubMed] [Google Scholar]
- 55.Kauppila LI. Atherosclerosis and disc degeneration/low-back pain – a systematic review. Eur J Vasc Endovasc Surg. 2009;37:661–670. doi: 10.1016/j.ejvs.2009.02.006. [DOI] [PubMed] [Google Scholar]