Abstract
Whereas the study of the interactions between the immune system and the central nervous system (CNS) has often focused on pathological conditions, the importance of neuroimmune communication in CNS homeostasis and function has become clear over that last two decades. Here we discuss the progression of our understanding of the interaction between the peripheral immune system and the CNS. We examine the notion of immune privilege of the CNS in light of both earlier findings and recent studies revealing a functional meningeal lymphatic system that drains cerebrospinal fluid (CSF) to the deep cervical lymph nodes, and consider the implications of a revised perspective on the immune privilege of the CNS on the etiology and pathology of different neurological disorders.
Introduction
The central nervous system (CNS) monitors and coordinates internal organ function and responds to changes in the environment. Being an essential system, it needs to be protected from endogenous and exogenous threats. Anatomically the CNS is protected by the cerebrospinal fluid (CSF) and the meninges that surround the brain and the spinal cord. The meninges are composed of the pia matter that intimately covers the parenchyma, a non-vascularized arachnoid matter, and a heavily vascularized dura matter, that is attached to the skull. The sub-arachnoid space lies between the arachnoid and the dura matter and contains the cerebrospinal fluid (CSF). The CNS is protected from the entry of pathogens, circulating immune cells, and factors within the blood by a physical blood-brain barrier (BBB) jointly maintained by tight junctions between brain endothelial cells, the basal lamina of these cells, and astrocyte endfeet processes (reviewed in [1–4]). Therefore, potentially damaging agents cannot readily gain access to the CNS. On the other hand, the meninges are more accessible and populated by various immune cells (reviewed in [5–7]). Although immune cells patrol the meninges[8,9], the mechanism by which these cells and antigens from the CNS trigger immune responses has remained unclear.
Experiments in the mid 20th century gave rise to the concept of the brain as a site of immune privilege[10]. Several physiological characteristics of the CNS, in addition to the presence of the BBB, were thought to underlie the slow immune reactions in the brain. For example, there is an absence of professional antigen presenting cells in the brain parenchyma, low MHC class I and II expression, and the apparent absence of classical lymphatic drainage from the CNS, all of which limit the capacity for an immune response to CNS-derived antigens. Despite these physical barriers, interactions between the CNS and the immune system occur and are not limited to pathology, but also extend to homeostatic functions. Since the initial studies from the beginning of the last century, a substantial progress has been made in our understanding of neuroimmune interactions. It has been demonstrated that (i) CNS-derived antigens induce an immune response in the deep cervical lymph nodes[11,12]; (ii) the immune response in the CNS has both beneficial and detrimental effects on brain function[13–15]; and (iii) that the CNS possesses a functional lymphatic system within the meninges that drains cellular and soluble constituents from the CSF into the deep cervical lymph nodes[16–18]. We discuss these findings here, and in this context we examine the progression of our understanding of the concept of CNS immune privilege.
Immune privilege of the CNS
Early studies of tumors[19,20] or fetal tissue[21] transplanted into the brain parenchyma showed successful growth of heterologous tumors or development of embryonic tissue, suggesting that the brain might be an appropriate transplantation site for the study of embryonic and tumor development. The tolerance of these transplants compared to their rejection in the periphery suggested that the brain was immunologically unique. In the 1940s, Medawar performed seminal experiments where adult rabbit skin was grafted into the brain parenchyma and observed that the rejection rate of the graft in the rabbit brain was lower than that of a similar graft on the chest, suggesting that the brain is a tolerogenic organ, unable to induce or support an immune response. In contrast, when skin from the same donor was first grafted peripherally and then grafted into the brain, it was rejected as rapidly as grafts in the peripheral organs, suggesting that the immune system, once peripherally activated, can enter the brain and cause graft rejection[10]. These experiments, by indicating that the brain fails to mount an efficient immune response against an allogeneic graft, gave rise to the concept of this organ’s immune privilege[10,22].
To this day, the CNS is still considered immune privileged or immunologically unique, but as our knowledge of the complex neuroimmune interactions occurring under homeostatic and pathological conditions expands, the mechanisms of immune privilege are being refined. One of the mechanisms suggested early on to underlie, at least in part, immune privilege was the perceived absence of classical lymphatic drainage of CNS antigens. Although soluble constituents from the parenchyma and the CSF drain into the deep cervical lymph nodes, the proposed route was via the cribriform plate and nasal mucosa lymphatics and through the classical lymphatic drainage[11,23]. The importance of the deep cervical lymph nodes and lymphatic vessels of higher mammals (cats and dogs) was demonstrated when all cervical lymph nodes were resected and the lymphatic vessels in the neck were ligated. Several neurological abnormalities were reported, including increased CSF pressure, neuropathologic abnormalities such as edema formation in ventricle and the pia mater, hydrocephalus, enlarged peri-capillar spaces around blood vessels, swollen axons, degeneration of a ganglion, prolife ration of glia, injury to the optic nerve, pupil edema, delayed reflexes upon reward, and finally increased sensitivity to barbiturates[24].
What role are the deep cervical lymph nodes and the lymphatic vessels playing in CNS drainage?
Drainage from the CNS
In addition to blood, the CNS contains CSF and interstitial fluid (ISF). CSF is produced mainly in the ventricles of the brain by the epithelial cells of the choroid plexus and circulates from the lateral ventricles to the third and then the fourth ventricle, finally reaching the subarachnoid space in the meninges. The ISF circulates within the brain parenchyma. Drainage of the two fluids, though connected, supposedly occurs in different ways[25,26]
In peripheral tissues, circulating ISF is recycled into the local lymphatic system, thereby cleaning the tissue and preventing accumulation of potentially toxic compounds, such as cellular metabolites or debris from damaged or necrotic cells[27]. Macromolecules and immune cells are then delivered to the lymph nodes and toxic compounds are removed through the blood. In the brain and spinal cord parenchyma the clearance of ISF is different, due to the unique tissue architecture and the lack of a classical lymphatic vasculature and depends on the size and properties of the compounds that are drained. Diffusion across the BBB and into the CSF is relatively unrestricted for small molecules, hydrophobic compounds, and transporter molecules expressed on the BBB[28–30]. For larger molecules, simple diffusion is not efficient enough to drain molecules from the deep brain parenchyma into the CSF[28].
During the 1980s, studies by Grady et al.[31,32] and Cserr et al.[11] showed that tracers injected into the CSF accumulate around small blood vessels that penetrate the brain, suggesting that a physical connection exists between the CSF and the perivascular spaces around the brain vasculature[31–33]. Recent studies by Nedergaard et al., extended that model by demonstrating the presence of a system, which was termed the ‘glymphatic system’, that allows interstitial solutes to be cleared from the brain via exchange of CSF and of ISF along the canals made between the walls of the veins and astrocytic endfeet[34,35]. Using confocal and intravital imaging, tracers injected into the cisterna magna of adult mice were visualized in the para-arterial spaces within 10 min of injection and reached the paravenous spaces more than 30 min later, suggesting a diffusion of the CSF from the periarterial spaces to the perivenous spaces through the brain parenchyma[34]. When injected directly into the brain parenchyma the tracers accumulate in the paravenous spaces, confirming that this could be an exit path for brain solutes[34]. The glymphatic system allows the efflux of both hydrophilic and lipophilic compounds, as well as of proteins such as Aβ, suggesting that dysfunction of this system may play etiological role in Alzheimer’s disease[34,36–38]. Both the efficiency of tracer infiltration into the brain parenchyma and its clearance from the brain are dependent on the maintenance of arteriole pulsatility[39] and CSF pressure[40,41]. Interestingly, the glymphatic system appears to be impaired in mice deficient in water-channel aquaporin-4 (Aqp4), suggesting a role for this molecule, which is expressed on astrocyte end-feet[42], in the bulk diffusion of water in the brain[34,40,41]. Also of interest is the fact that Aqp4−/− mice were still able to clear some of the tracer from the parenchyma, suggesting that other molecules may mediate water diffusion in addition to Aqp4. The precise mechanism by which compounds are diffused across the astrocyte end-feet remains unknown. Notably, the glymphatic space increases during sleep[37]. In sleeping mice, the clearance of endogenous proteins such as Aβ from the brain is indeed enhanced[37]. This phenomenon, which appears to be dependent on adrenergic receptor inhibition, is one of the first indicators of scientific evidence for a particular function of sleep, namely to facilitate clearance of the brain parenchyma[37]. Thus, the glymphatic system provides a way for ISF and macromolecules from within the brain parenchyma to reach the CSF. The question whether immune cells can leave the brain parenchyma through the same path remains unknown, and a recent study suggested a potential specific path for immune cells to leave the brain parenchyma via the rostral migratory stream[43].
CSF is produced by choroid plexus epithelial cells and flows vectorially through the ventricular system before draining into the subarachnoid spaces through a number of apertures. In these spaces the CSF flows between two meningeal membranes, the arachnoid and the pia matter. Physically the CSF provides the brain with buoyancy, while physiologically it provides a route by which neurotransmitters, hormones and cytokines travel over wide areas of the CNS and waste materials are extruded[44]. The production, flow and drainage of CSF are tightly regulated, enabling CSF pressure maintenance. Drainage of CSF into the major venous sinuses through arachnoid villi and granulations was the first described path for CSF drainage[45–48] (Figure 1). In humans, arachnoid villi are primarily associated with the superior sagittal sinus and the transverse sinuses[49,50]. In sheep and rodents these granulations appear to be significantly smaller[12,51]. The arachnoid villi allow the CSF to flow out through channels of the arachnoid cap of the granulation before it reaches the venous endothelium[47,52]. While this system is efficient for the excretion of water and small compounds into the bloodstream, larger compounds (macromolecules and especially immune cells) are unlikely to be transferred though this route.
Figure 1. Paths of CSF fluid drainage.
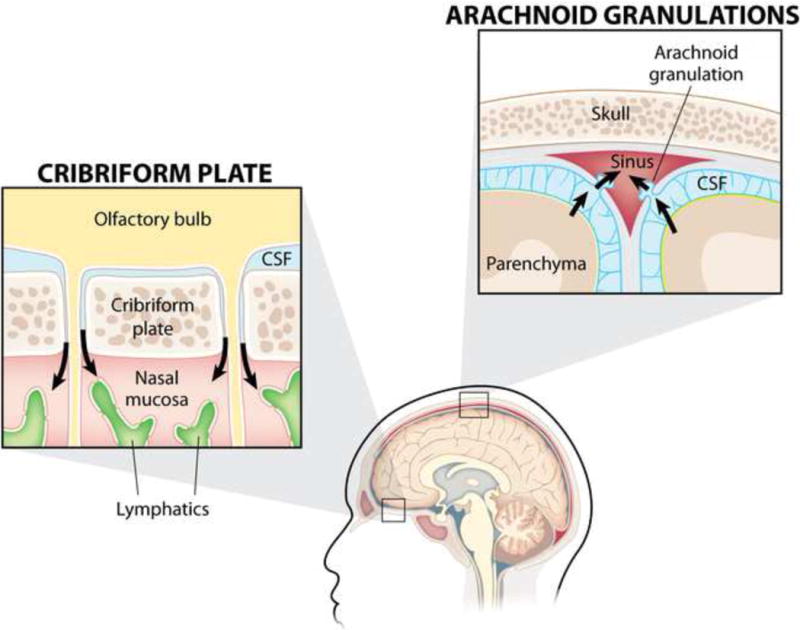
The CSF, flowing between the arachnoid and the pia matter of the meninges, can drain into the blood stream through the arachnoid granulations located along the superior sagittal sinus and the transverse sinuses, or reach the lymphatic vasculature of the nasal mucosa by crossing the cribriform plate, localized under the olfactory bulbs, along the olfactory nerves.
In a large variety of mammals and also in humans, injection of tracers revealed a second path of CSF drainage from the subarachnoid spaces into the inferior aspect of the olfactory bulbs[12,53–55]. The relative contribution of each CSF-drainage pathway in humans and larger mammals probably differs from that in smaller animals[25,56,57].
Studies performed in the early 20th century demonstrated that CSF drains into the deep cervical lymph[24], although the path that macromolecules within the CSF take to reach the nodes was not completely understood[24]. Later works demonstrated the pathway was via the cribriform plate into the lymphatic system of the nasal mucosa[12,58,54,59,53] (Figure 1) and then to the deep cervical lymph nodes. Immune cells from the meningeal spaces were proposed to drain similarly[60–62]. Antigenpresenting cells (APCs) and lymphocytes were shown to reach the nasal lymphatics by crawling along the olfactory nerves[43,60,61]. Based on these data, the cribriform plate was viewed as a path for soluble molecules from the CSF and immune cells to exit the CNS.
The meningeal lymphatic system
Recent findings have revealed the presence of a conventional and functional lymphatic system, which is located in the meninges (in the dura matter) and enables fluid, macromolecules and immune cells to drain from the CNS into the deep cervical lymph nodes[16,17] (Figure 2). Dural lymphatics had been previously mentioned in the literature[18] but their role in CSF drainage remained unaddressed. Using both a newly established dissection of mouse meninges[16] and lymphatic cell reporter mice[16,17], conventional lymphatic vessels expressing hallmarks of lymphatic endothelial cells (CD31, LYVE-1, podoplanin, VEGFR3 and the chemokine CCL21) were seen to be lining the dural sinuses and exiting the CNS at the base of the skull[16,17]. Although apparently less well developed than the peripheral lymphatic network[16], they possess scattered lymphatic valves[17] (near the base of the skull only) and respond to exogenous VEGF-c like peripheral lymphatics[16]. Tracers and macromolecules injected into the brain and/or the CSF were shown to drain primarily into the deep cervical lymph nodes, confirming the previous observation of a drainage path[16,17]. Surgical ligation of the lymphatic vessels[16] and the use of mice lacking meningeal lymphatics[17] (along with other peripheral lymphatics[63]) showed that the drainage in the deep cervical lymph nodes was dependent on the presence of meningeal lymphatic vessels. Interestingly, ligation of the lymphatic vessels that reach to the deep cervical lymph nodes induced a lymphedema-like phenomenon on meningeal lymphatics suggesting a physical connection between the meningeal lymphatic vessels and the deep cervical lymph nodes[16]. Importantly, immune cells (T cells, B cells, and dendritic cells) were present in the meningeal lymphatic vessels under normal conditions[16], suggesting that the meningeal lymphatics participate in the trafficking of immune cells out of the CNS in the steady state.
Figure 2. The meningeal lymphatics enable the drainage of macromolecules and immune cells.

While the CSF fluid drains back to the bloodstream, the macromolecules and immune cells localized within the CSF drain primarily through the meningeal lymphatic vessels to reach the deep cervical lymph nodes.
In transgenic mice lacking in meningeal lymphatic vessels, drainage of macromolecules into the deep cervical lymph nodes was abrogated, but most importantly, the drainage from the brain parenchyma into the CSF (through the glymphatic system) was also impaired, without affecting CSF pressure[17]. These findings demonstrate that the fluid exchange between the CSF and the peripheral blood occurs via different conduits than the drainage of macromolecules and immune cells from the CSF, which exit through the meningeal lymphatic vessels.
As we discuss in the next chapter, lymphatic endothelial cells of meningeal lymphatic vessels may be equipped with unique molecular arsenal to maintain anergy of CNS-reactive T cells within the meningeal spaces. Failure of such a mechanism, if exists, may underlie the etiology of autoimmune attack on the brain, as seen in MS. Therefore, the discovery of CNS lymphatics does not challenge the immune privilege status of the CNS but may rather offer new mechanisms underlying this unique immunological environment. It also provides new hypotheses for unresolved questions in a variety of settings with neuroimmune components.
Potential role of CNS lymphatics in health and disease
Experimental autoimmune encephalomyelitis (EAE) is an animal model for multiple sclerosis (MS), where immune cells specific to CNS antigens damage the CNS, resulting in paralysis[64–73]. Autoimmune T cells traffic to the brain and cross the BBB and causes damage[74], thus preventing T cell migration to the CNS is a therapeutic target. Indeed, Natalizumab or Tysabri®, a monoclonal antibody that targets α4β1 integrin (VLA-4) on T cells and prevents their extravasation into the tissue and has been shown to be effective in MS[75–78]. Although MS is known to be associated with reduced activity of regulatory T cells, there appears to be no difference in autoimmune T-cell repertoire between MS-prone and healthy patients[79]. What then triggers an autoimmune attack? As discussed in Box 1, meningeal lymphatic vessels may be playing a central role in maintaining tolerance of autoimmune T cells similar to what has been demonstrated in tumors, where MHCI/II expression of lymphatic endothelial cells anergizes tumor-specific CD4+ and CD8+ T cells[80–85] Meningeal lymphatic endothelial cells may directly tolerize T cells and, therefore, lymphatic drainage of CNS antigens may contribute to tolerance to these self-antigens. Thus, an inflammatory trigger, such as a viral infection, may activate the self reactive T cells leading to attacks in the CNS.
BOX I. What is the role of meningeal lymphatic vessels in neurological disorders?
Understanding the function of meningeal lymphatic vessels on a molecular level in their regulation of immune responses in the meninges and the CNS parenchyma, will be necessary to address their role in CNS disorders. Even more work will be needed to take these discoveries to the clinic.
Theoretically, lymphatic vessels may affect brain immunity in numerous ways. Meningeal lymphatic vessels are likely an important route for APCs and soluble factors from the brain to reach the deep cervical lymph nodes[16,17] in addition to the previously described routes[25,26]. Thus, does enhanced APC trafficking result in a greater potential for self-reactive T cells to be primed against brain antigens and thus result in an autoimmune attack? Likewise, drainage of tumor antigens (within the APCs or as soluble macromolecules) from the brain may alter the process of tumor rejection. Although brain tumors very rarely metastasize, the route for metastases could be via the meningeal lymphatic vessels.
On the other hand, meningeal lymphatic vessels may account for the suppression of brain-specific immune responses. For example, tumor-associated lymphatic vessels have been shown to express MHC molecules, presenting tumor associated antigens and thus anergize T cells in order to suppress an anti-tumor immune response[85]. A similar function may be attributed to the meningeal lymphatics; thus, if these vessels fail to anergize T cells, they may become activated in response to self-antigens and attack the brain. A failure of local lymphatic vessels to induce T cell tolerance could possibly underlie autoimmune attacks in MS. On the other hand, meningeal lymphatic vessels that overly suppress self-reactive T cells may diminish the population of circulating immune cells in the meninges leading to cognitive impairments[9,101,104].
Finally, aggregated Aβ may be released from the CNS parenchyma via the glymphatic system[34,39,41], but it is unlikely that macromolecules would be removed from the CSF through the blood vasculature. Protein aggregates are most likely to be removed from the CSF via the meningeal lymphatic vessels into the periphery. With aging, however, these vessels may become less efficient, resulting in the deposition of protein aggregates (as seen with Aβ aggregates on the brain’s blood vasculature), which will then clog the lymphatic vessels and prevent aggregate removal. It is thus possible that Alzheimer’s disease pathology is preceded by breakdown in the pathways that remove Aβ, including the meningeal lymphatic vessels. In such a case, pharmacological expansion of the vessels may be a viable therapeutic approach. Restoring the function of meningeal lymphatics by viral therapy, by physical abstraction, or pharmacologically may alter the immune response in the meninges as well as the drainage of cells and macromolecules, thereby beneficially affecting neurological disorders, in which meningeal lymphatic vessel function and/or meningeal immunity are impaired.
Protective and pathogenic T cell responses also occur in response to infection. In several models of viral encephalitis, the inoculation of virus into the brain parenchyma leads to a lethal encephalitis[86] The pathway by which viral antigens were able to exit the CNS to prime T cell responses in the periphery has remained unclear[87–89]. The drainage of viral antigens from the parenchyma by the glymphatic system to the CSF and the subsequent drainage via lymphatic vessels to the deep cervical lymph node may account for the ability of these viruses to prime T cell responses. In addition, several pathogens establish chronic infections of the CNS, including cytomegalovirus, JC virus, herpes simplex virus, and Toxoplasma gondii. Ongoing immune responses are required to prevent lethal reactivation of these diseases, yet the mechanisms by which antigens from these pathogens were able to maintain a continuous peripheral immune response has not been determined[89–92]. The CNS lymphatics may be centrally involved in the maintenance of the immune response to these opportunistic pathogens of the CNS.
Immune response within the CNS is not always detrimental, as evidenced by CNS injury, where the immediate and physiological response of immune cells is to limit secondary degeneration[93–97]. CNS injury results in T cell proliferation and activation, primarily in the deep cervical lymph nodes[98], suggesting that the drainage of macromolecules and/or cells from the injury site induces an immune response. Elimination of these T cells, or of the lymph nodes as a whole, results in impaired neuronal survival, suggesting that their spontaneous response is beneficial. However, it is still poorly understood how immune cells become activated in the deep cervical lymph nodes after injury and what damaged tissue-derived molecular mediators and/or antigens are inducing this neuroprotective response[98].
T cells also support cognition under physiological conditions. Deficiency in the T cell compartment results in impaired performance in spatial learning and memory tasks[99–101]. Interestingly, not only T cell deficiency, but also acute depletion of T cells from wild-type mice or even inhibition of their migration into CNS tissue (by anti-VLA4 antibodies) resulted in impaired performance of mice in cognitive tasks[102,103]. Moreover, no immune infiltrates were observed within the parenchyma of mice that learned the task, but immune activity was noticed in the meninges. A crucial question remains regarding the signal that induces the recruitment of T cells into the meninges during a cognitive task. Changes in CSF composition, local activation, and drainage of meningeal immune cells could potentially provide signal to the periphery to induce T cell recruitment. Drainage from the CNS into the periphery might therefore be an important component to maintain higher brain function.
Concluding remarks
The immune system functions in the CNS in a way that is unique from peripheral tissues. Our understanding of immune privilege continues to be refined as new discoveries are made. Originally thought to be immunologically pristine, it is now accepted that immune cells are present in the meninges and provide immune surveillance of the CNS. Likewise, classical lymphatic vessels were discovered in the CNS meninges. The new findings provide a mechanism by which large particles and immune cells can drain from the brain and interface directly with the peripheral immune system. The unique properties of these vessels, including their location and size, may explain why immune responses to CNS antigens are often slower than in peripheral tissues. Moreover, this discovery suggests that the deep cervical lymph nodes may be intimately involved in both the tolerance to self-antigens and immune responses against foreign antigens. Lymphatic endothelial cells of meningeal lymphatic vessels may be molecularly uniquely equipped to ensure tolerance of T cells reactive to CNS-derived antigens. When the mechanisms of lymphatic endothelial cell-mediated tolerance fail, autoimmunity may develop. Therefore, the classical lymphatic vessels draining the CNS may in fact be fundamental in ensuring CNS immune privilege. As the immune system is involved in both the normal function of the brain and in neurological diseases and disorders, there is a continued need to understand the basic tenets of immune privilege, as it is still clear that the CNS remains immunologically unique.
TRENDS BOX.
Meningeal space of the brain is enriched in variety of innate and adaptive immune cells, which are communicating with and circulating through the deep cervical lymph nodes.
Sufficient meningeal immunity is necessary for higher brain function – elimination of T cells results in cognitive deficiency in mice. T cells that are responsible for this beneficial cross-talk are presumably specific to CNS self – antigens.
Close examination of the dura matter revealed presence of functional classic lymphatic vessels that drain macromolecules and immune cells from the meninges and the CSF.
Obstruction (surgical) or elimination (transgenic mice) of meningeal lymphatic vessels abrogates glymphatic flow and abolishes drainage to the deep cervical lymph nodes without affecting CSF pressure.
Outstanding questions.
Why are immune responses to CNS antigens slow to develop? What mechanisms underlie these responses, and how do they relate to autoimmune responses to other tissues?
Can immune cells (perivascular macrophages in healthy brain and other myeloid cells during CNS inflammation) exit the brain parenchyma to the CSF? If yes, what route do these cells take? What are the mechanisms ensuring tolerance to these antigens? If no, what mechanism retains antigens presenting cells within the borders of parenchyma?
Do patients afflicted with MS and/or AD exhibit specific changes in meningeal lymphatic vessels? If so, could these changes be indicative/predictive of disease?
Acknowledgments
We would like to thank Shirley Smith for editing the manuscript and Anita Impagliazzo for figure artwork. This work was primarily supported by a grant from the National Institute on Aging, NIH (AG034113 award to J. K).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
All authors declare no conflict of interests.
References
- 1.Ransohoff RM, et al. Three or more routes for leukocyte migration into the central nervous system. Nat Rev Immunol. 2003;3:569–581. doi: 10.1038/nri1130. [DOI] [PubMed] [Google Scholar]
- 2.Engelhardt B, Ransohoff RM. Capture, crawl, cross: the T cell code to breach the blood-brain barriers. Trends Immunol. 2012;33:579–589. doi: 10.1016/j.it.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 3.Takeshita Y, Ransohoff RM. Inflammatory cell trafficking across the blood-brain barrier: chemokine regulation and in vitro models. Immunol Rev. 2012;248:228–239. doi: 10.1111/j.1600-065X.2012.01127.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bentivoglio M, Kristensson K. Tryps and trips: cell trafficking across the 100-year-old blood-brain barrier. Trends Neurosci. 2014;37:325–333. doi: 10.1016/j.tins.2014.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Russi AE, Brown MA. The meninges: new therapeutic targets for multiple sclerosis. Transl Res J Lab Clin Med. 2015;165:255–269. doi: 10.1016/j.trsl.2014.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weller RO. Microscopic morphology and histology of the human meninges. Morphol Bull Assoc Anat. 2005;89:22–34. doi: 10.1016/s1286-0115(05)83235-7. [DOI] [PubMed] [Google Scholar]
- 7.Decimo I, et al. Meninges: from protective membrane to stem cell niche. Am J Stem Cells. 2012;1:92–105. [PMC free article] [PubMed] [Google Scholar]
- 8.Ransohoff RM, Engelhardt B. The anatomical and cellular basis of immune surveillance in the central nervous system. Nat Rev Immunol. 2012;12:623–635. doi: 10.1038/nri3265. [DOI] [PubMed] [Google Scholar]
- 9.Kipnis J, et al. Pro-cognitive properties of T cells. Nat Rev Immunol. 2012;12:663–669. doi: 10.1038/nri3280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Medawar PB. Immunity to homologous grafted skin; the fate of skin homografts transplanted to the brain, to subcutaneous tissue, and to the anterior chamber of the eye. Br J Exp Pathol. 1948;29:58–69. [PMC free article] [PubMed] [Google Scholar]
- 11.Cserr HF, et al. Drainage of brain extracellular fluid into blood and deep cervical lymph and its immunological significance. Brain Pathol Zurich Switz. 1992;2:269–276. doi: 10.1111/j.1750-3639.1992.tb00703.x. [DOI] [PubMed] [Google Scholar]
- 12.Kida S, et al. CSF drains directly from the subarachnoid space into nasal lymphatics in the rat. Anatomy, histology and immunological significance. Neuropathol Appl Neurobiol. 1993;19:480–488. doi: 10.1111/j.1365-2990.1993.tb00476.x. [DOI] [PubMed] [Google Scholar]
- 13.Steinman L. Elaborate interactions between the immune and nervous systems. Nat Immunol. 2004;5:575–581. doi: 10.1038/ni1078. [DOI] [PubMed] [Google Scholar]
- 14.Walsh JT, et al. Regulatory T cells in central nervous system injury: a double-edged sword. J Immunol Baltim Md 1950. 2014;193:5013–5022. doi: 10.4049/jimmunol.1302401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schwartz M, Raposo C. Protective Autoimmunity: A Unifying Model for the Immune Network Involved in CNS Repair. Neurosci Rev J Bringing Neurobiol Neurol Psychiatry. 2014;20:343–358. doi: 10.1177/1073858413516799. [DOI] [PubMed] [Google Scholar]
- 16.Louveau A, et al. Structural and functional features of central nervous system lymphatic vessels. Nature. 2015 doi: 10.1038/nature14432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aspelund A, et al. A dural lymphatic vascular system that drains brain interstitial fluid and macromolecules. J Exp Med. 2015;212:991–999. doi: 10.1084/jem.20142290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andres KH, et al. Nerve fibres and their terminals of the dura mater encephali of the rat. Anat Embryol (Berl) 1987;175:289–301. doi: 10.1007/BF00309843. [DOI] [PubMed] [Google Scholar]
- 19.Shirai Y. Transplantation of the rat sarcoma in adult heterogenous animals. Japn Med World 1921 [Google Scholar]
- 20.Murphy JB, Sturm E. Conditions determining the transplantability of tissues in the brain. J Exp Med. 1923 doi: 10.1084/jem.38.2.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Willis RA. Experiments on the intracerebral implantation of embryo tissues in rats. Proc R Soc Lond Ser B 1935 [Google Scholar]
- 22.Widner H, Brundin P. Immunological aspects of grafting in the mammalian central nervous system. A review and speculative synthesis. Brain Res. 1988;472:287–324. doi: 10.1016/0165-0173(88)90010-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harling-Berg C, et al. Role of cervical lymph nodes in the systemic humoral immune response to human serum albumin microinfused into rat cerebrospinal fluid. J Neuroimmunol. 1989;25:185–193. doi: 10.1016/0165-5728(89)90136-7. [DOI] [PubMed] [Google Scholar]
- 24.Foldi M, et al. Uber Wirkungen der Unterbindung der Lymphgefasse und Lymphknoten des Halses auf das Zentralnervensystem im Tierversuch. 1963;137:483–510. [PubMed] [Google Scholar]
- 25.Weller RO, et al. Lymphatic drainage of the brain and the pathophysiology of neurological disease. Acta Neuropathol (Berl) 2009;117:1–14. doi: 10.1007/s00401-008-0457-0. [DOI] [PubMed] [Google Scholar]
- 26.Laman JD, Weller RO. Drainage of cells and soluble antigen from the CNS to regional lymph nodes. J Neuroimmune Pharmacol Off J Soc NeuroImmune Pharmacol. 2013;8:840–856. doi: 10.1007/s11481-013-9470-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alitalo K. The lymphatic vasculature in disease. Nat Med. 2011;17:1371–1380. doi: 10.1038/nm.2545. [DOI] [PubMed] [Google Scholar]
- 28.Syková E, Nicholson C. Diffusion in brain extracellular space. Physiol Rev. 2008;88:1277–1340. doi: 10.1152/physrev.00027.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Groothuis DR, et al. Efflux of drugs and solutes from brain: the interactive roles of diffusional transcapillary transport, bulk flow and capillary transporters. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metab. 2007;27:43–56. doi: 10.1038/sj.jcbfm.9600315. [DOI] [PubMed] [Google Scholar]
- 30.Verkman AS. Diffusion in the extracellular space in brain and tumors. Phys Biol. 2013;10:045003. doi: 10.1088/1478-3975/10/4/045003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rennels ML, et al. Evidence for a “paravascular” fluid circulation in the mammalian central nervous system, provided by the rapid distribution of tracer protein throughout the brain from the subarachnoid space. Brain Res. 1985;326:47–63. doi: 10.1016/0006-8993(85)91383-6. [DOI] [PubMed] [Google Scholar]
- 32.Rennels ML, et al. Rapid solute transport throughout the brain via paravascular fluid pathways. Adv Neurol. 1990;52:431–439. [PubMed] [Google Scholar]
- 33.Szentistványi I, et al. Drainage of interstitial fluid from different regions of rat brain. Am J Physiol. 1984;246:F835–844. doi: 10.1152/ajprenal.1984.246.6.F835. [DOI] [PubMed] [Google Scholar]
- 34.Iliff JJ, et al. A Paravascular Pathway Facilitates CSF Flow Through the Brain Parenchyma and the Clearance of Interstitial Solutes, Including Amyloid β. Sci Transl Med. 2012;4:147ra111–147ra111. doi: 10.1126/scitranslmed.3003748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang L, et al. Evaluating glymphatic pathway function utilizing clinically relevant intrathecal infusion of CSF tracer. J Transl Med. 2013;11:107. doi: 10.1186/1479-5876-11-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thrane VR, et al. Paravascular microcirculation facilitates rapid lipid transport and astrocyte signaling in the brain. Sci Rep. 2013;3 doi: 10.1038/srep02582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xie L, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342:373–377. doi: 10.1126/science.1241224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kress BT, et al. Impairment of paravascular clearance pathways in the aging brain. Ann Neurol. 2014;76:845–861. doi: 10.1002/ana.24271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Iliff JJ, et al. Cerebral Arterial Pulsation Drives Paravascular CSF–Interstitial Fluid Exchange in the Murine Brain. J Neurosci. 2013;33:18190–18199. doi: 10.1523/JNEUROSCI.1592-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Plog BA, et al. Biomarkers of Traumatic Injury Are Transported from Brain to Blood via the Glymphatic System. J Neurosci. 2015;35:518–526. doi: 10.1523/JNEUROSCI.3742-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iliff JJ, et al. Impairment of Glymphatic Pathway Function Promotes Tau Pathology after Traumatic Brain Injury. J Neurosci. 2014;34:16180–16193. doi: 10.1523/JNEUROSCI.3020-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Potokar M, et al. Regulation of AQP4 surface expression via vesicle mobility in astrocytes. Glia. 2013;61:917–928. doi: 10.1002/glia.22485. [DOI] [PubMed] [Google Scholar]
- 43.Mohammad MG, et al. Immune cell trafficking from the brain maintains CNS immune tolerance. J Clin Invest. 2014;124:1228–1241. doi: 10.1172/JCI71544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Whedon JM, Glassey D. CEREBROSPINAL FLUID STASIS AND ITS CLINICAL SIGNIFICANCE. Altern Ther Health Med. 2009;15:54–60. [PMC free article] [PubMed] [Google Scholar]
- 45.Kido DK, et al. Human spinal arachnoid villi and granulations. Neuroradiology. 1976;11:221–228. doi: 10.1007/BF00328377. [DOI] [PubMed] [Google Scholar]
- 46.Go KG, et al. Fluid secretion in arachnoid cysts as a clue to cerebrospinal fluid absorption at the arachnoid granulation. J Neurosurg. 1986;65:642–648. doi: 10.3171/jns.1986.65.5.0642. [DOI] [PubMed] [Google Scholar]
- 47.Upton ML, Weller RO. The morphology of cerebrospinal fluid drainage pathways in human arachnoid granulations. J Neurosurg. 1985;63:867–875. doi: 10.3171/jns.1985.63.6.0867. [DOI] [PubMed] [Google Scholar]
- 48.Mawera G, Asala SA. The function of arachnoid villi/granulations revisited. Cent Afr J Med. 1996;42:281–284. [PubMed] [Google Scholar]
- 49.Leach JL, et al. Normal appearance of arachnoid granulations on contrast-enhanced CT and MR of the brain: differentiation from dural sinus disease. AJNR Am J Neuroradiol. 1996;17:1523–1532. [PMC free article] [PubMed] [Google Scholar]
- 50.Roche J, Warner D. Arachnoid granulations in the transverse and sigmoid sinuses: CT, MR, and MR angiographic appearance of a normal anatomic variation. AJNR Am J Neuroradiol. 1996;17:677–683. [PMC free article] [PubMed] [Google Scholar]
- 51.Boulton M, et al. Drainage of CSF through lymphatic pathways and arachnoid villi in sheep: measurement of 125I-albumin clearance. Neuropathol Appl Neurobiol. 1996;22:325–333. doi: 10.1111/j.1365-2990.1996.tb01111.x. [DOI] [PubMed] [Google Scholar]
- 52.Tripathi BJ, Tripathi RC. Vacuolar transcellular channels as a drainage pathway for cerebrospinal fluid. J Physiol. 1974;239:195–206. doi: 10.1113/jphysiol.1974.sp010563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Johnston M, et al. Evidence of connections between cerebrospinal fluid and nasal lymphatic vessels in humans, non-human primates and other mammalian species. Cerebrospinal Fluid Res. 2004;1:2. doi: 10.1186/1743-8454-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Johnston M, et al. Subarachnoid injection of Microfil reveals connections between cerebrospinal fluid and nasal lymphatics in the nonhuman primate. Neuropathol Appl Neurobiol. 2005;31:632–640. doi: 10.1111/j.1365-2990.2005.00679.x. [DOI] [PubMed] [Google Scholar]
- 55.Koh L, et al. Integration of the subarachnoid space and lymphatics: is it time to embrace a new concept of cerebrospinal fluid absorption? Cerebrospinal Fluid Res. 2005;2:6. doi: 10.1186/1743-8454-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Weller RO, et al. Pathophysiology of the lymphatic drainage of the central nervous system: Implications for pathogenesis and therapy of multiple sclerosis. Pathophysiol Off J Int Soc Pathophysiol ISP. 2010;17:295–306. doi: 10.1016/j.pathophys.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 57.Johanson CE, et al. Multiplicity of cerebrospinal fluid functions: New challenges in health and disease. Cerebrospinal Fluid Res. 2008;5:10. doi: 10.1186/1743-8454-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nagra G, et al. Quantification of cerebrospinal fluid transport across the cribriform plate into lymphatics in rats. Am J Physiol Regul Integr Comp Physiol. 2006;291:R1383–1389. doi: 10.1152/ajpregu.00235.2006. [DOI] [PubMed] [Google Scholar]
- 59.Zhang ET, et al. Directional and compartmentalised drainage of interstitial fluid and cerebrospinal fluid from the rat brain. Acta Neuropathol (Berl) 1992;83:233–239. doi: 10.1007/BF00296784. [DOI] [PubMed] [Google Scholar]
- 60.Goldmann J, et al. T cells traffic from brain to cervical lymph nodes via the cribroid plate and the nasal mucosa. J Leukoc Biol. 2006;80:797–801. doi: 10.1189/jlb.0306176. [DOI] [PubMed] [Google Scholar]
- 61.Kaminski M, et al. Migration of monocytes after intracerebral injection at entorhinal cortex lesion site. J Leukoc Biol. 2012;92:31–39. doi: 10.1189/jlb.0511241. [DOI] [PubMed] [Google Scholar]
- 62.Harris MG, et al. Immune privilege of the CNS is not the consequence of limited antigen sampling. Sci Rep. 2014;4:4422. doi: 10.1038/srep04422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Thomas SN, et al. Impaired humoral immunity and tolerance in K14-VEGFR-3-Ig mice that lack dermal lymphatic drainage. J Immunol Baltim Md 1950. 2012;189:2181–2190. doi: 10.4049/jimmunol.1103545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wekerle H, Sun D. Fragile privileges: autoimmunity in brain and eye. Acta Pharmacol Sin. 2010;31:1141–1148. doi: 10.1038/aps.2010.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zamvil S, et al. T-cell clones specific for myelin basic protein induce chronic relapsing paralysis and demyelination. Nature. 1985;317:355–358. doi: 10.1038/317355a0. [DOI] [PubMed] [Google Scholar]
- 66.Chen Y, et al. Regulatory T cell clones induced by oral tolerance: suppression of autoimmune encephalomyelitis. Science. 1994;265:1237–1240. doi: 10.1126/science.7520605. [DOI] [PubMed] [Google Scholar]
- 67.Kawakami N, et al. Live imaging of effector cell trafficking and autoantigen recognition within the unfolding autoimmune encephalomyelitis lesion. J Exp Med. 2005;201:1805–1814. doi: 10.1084/jem.20050011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Prat A, et al. Migration of multiple sclerosis lymphocytes through brain endothelium. Arch Neurol. 2002;59:391–397. doi: 10.1001/archneur.59.3.391. [DOI] [PubMed] [Google Scholar]
- 69.Prat A, et al. Heterogeneity of T-lymphocyte function in primary progressive multiple sclerosis: relation to magnetic resonance imaging lesion volume. Ann Neurol. 2000;47:234–237. [PubMed] [Google Scholar]
- 70.Steinman L, Zamvil SS. Virtues and pitfalls of EAE for the development of therapies for multiple sclerosis. Trends Immunol. 2005;26:565–571. doi: 10.1016/j.it.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 71.Liblau RS, et al. Neurons as targets for T cells in the nervous system. Trends Neurosci. 2013;36:315–324. doi: 10.1016/j.tins.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 72.Siffrin V, et al. In vivo imaging of partially reversible th17 cell-induced neuronal dysfunction in the course of encephalomyelitis. Immunity. 2010;33:424–436. doi: 10.1016/j.immuni.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 73.Zipp F, et al. Identification of inflammatory neuronal injury and prevention of neuronal damage in multiple sclerosis: hope for novel therapies? JAMA Neurol. 2013;70:1569–1574. doi: 10.1001/jamaneurol.2013.4391. [DOI] [PubMed] [Google Scholar]
- 74.Baxter AG. The origin and application of experimental autoimmune encephalomyelitis. Nat Rev Immunol. 2007;7:904–912. doi: 10.1038/nri2190. [DOI] [PubMed] [Google Scholar]
- 75.McCormack PL. Natalizumab: a review of its use in the management of relapsing-remitting multiple sclerosis. Drugs. 2013;73:1463–1481. doi: 10.1007/s40265-013-0102-7. [DOI] [PubMed] [Google Scholar]
- 76.Steinman L. Blocking adhesion molecules as therapy for multiple sclerosis: natalizumab. Nat Rev Drug Discov. 2005;4:510–518. doi: 10.1038/nrd1752. [DOI] [PubMed] [Google Scholar]
- 77.Theien BE, et al. Discordant effects of anti-VLA-4 treatment before and after onset of relapsing experimental autoimmune encephalomyelitis. J Clin Invest. 2001;107:995–1006. doi: 10.1172/JCI11717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Steinman L. Immunology of relapse and remission in multiple sclerosis. Annu Rev Immunol. 2014;32:257–281. doi: 10.1146/annurev-immunol-032713-120227. [DOI] [PubMed] [Google Scholar]
- 79.Sospedra M, Martin R. Immunology of Multiple Sclerosis*. Annu Rev Immunol. 2005;23:683–747. doi: 10.1146/annurev.immunol.23.021704.115707. [DOI] [PubMed] [Google Scholar]
- 80.Cohen JN, et al. Tolerogenic properties of lymphatic endothelial cells are controlled by the lymph node microenvironment. PloS One. 2014;9:e87740. doi: 10.1371/journal.pone.0087740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rouhani SJ, et al. Roles of lymphatic endothelial cells expressing peripheral tissue antigens in CD4 T-cell tolerance induction. Nat Commun. 2015;6:6771. doi: 10.1038/ncomms7771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tewalt EF, et al. Lymphatic endothelial cells induce tolerance via PD-L1 and lack of costimulation leading to high-level PD-1 expression on CD8 T cells. Blood. 2012;120:4772–4782. doi: 10.1182/blood-2012-04-427013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Malhotra D, et al. Transcriptional profiling of stroma from inflamed and resting lymph nodes defines immunological hallmarks. Nat Immunol. 2012;13:499–510. doi: 10.1038/ni.2262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lund AW, et al. VEGF-C promotes immune tolerance in B16 melanomas and cross-presentation of tumor antigen by lymph node lymphatics. Cell Rep. 2012;1:191–199. doi: 10.1016/j.celrep.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 85.Shields JD, et al. Induction of lymphoidlike stroma and immune escape by tumors that express the chemokine CCL21. Science. 2010;328:749–752. doi: 10.1126/science.1185837. [DOI] [PubMed] [Google Scholar]
- 86.Swanson PA, McGavern DB. Viral diseases of the central nervous system. Curr Opin Virol. 2015;11:44–54. doi: 10.1016/j.coviro.2014.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Marten NW, et al. Kinetics of virus-specific CD8+ -T-cell expansion and trafficking following central nervous system infection. J Virol. 2003;77:2775–2778. doi: 10.1128/JVI.77.4.2775-2778.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bergmann CC, et al. Coronavirus infection of the central nervous system: host-virus stand-off. Nat Rev Microbiol. 2006;4:121–132. doi: 10.1038/nrmicro1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.McGavern DB, Kang SS. Illuminating viral infections in the nervous system. Nat Rev Immunol. 2011;11:318–329. doi: 10.1038/nri2971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Tan IL, et al. HIV-associated opportunistic infections of the CNS. Lancet Neurol. 2012;11:605–617. doi: 10.1016/S1474-4422(12)70098-4. [DOI] [PubMed] [Google Scholar]
- 91.Landrith TA, et al. Characteristics and critical function of CD8+ T cells in the Toxoplasma-infected brain. Semin Immunopathol. 2015;37:261–270. doi: 10.1007/s00281-015-0487-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Torti N, et al. Non-hematopoietic cells in lymph nodes drive memory CD8 T cell inflation during murine cytomegalovirus infection. PLoS Pathog. 2011;7:e1002313. doi: 10.1371/journal.ppat.1002313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Gadani SP, et al. Dealing with Danger in the CNS: The Response of the Immune System to Injury. Neuron. 2015;87:47–62. doi: 10.1016/j.neuron.2015.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Walsh JT, et al. T cells in the central nervous system: messengers of destruction or purveyors of protection? Immunology. 2014;141:340–344. doi: 10.1111/imm.12187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Shechter R, et al. Infiltrating blood-derived macrophages are vital cells playing an anti-inflammatory role in recovery from spinal cord injury in mice. PLoS Med. 2009;6:e1000113. doi: 10.1371/journal.pmed.1000113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kroner A, et al. TNF and increased intracellular iron alter macrophage polarization to a detrimental M1 phenotype in the injured spinal cord. Neuron. 2014;83:1098–1116. doi: 10.1016/j.neuron.2014.07.027. [DOI] [PubMed] [Google Scholar]
- 97.Evans TA, et al. High-resolution intravital imaging reveals that blood-derived macrophages but not resident microglia facilitate secondary axonal dieback in traumatic spinal cord injury. Exp Neurol. 2014;254:109–120. doi: 10.1016/j.expneurol.2014.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Walsh JT, et al. MHCII-independent CD4+ T cells protect injured CNS neurons via IL-4. J Clin Invest. 2015;125:699–714. doi: 10.1172/JCI76210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Brynskikh A, et al. Adaptive immunity affects learning behavior in mice. Brain Behav Immun. 2008;22:861–869. doi: 10.1016/j.bbi.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 100.Derecki NC, et al. Regulation of learning and memory by meningeal immunity: a key role for IL-4. J Exp Med. 2010;207:1067–1080. doi: 10.1084/jem.20091419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Radjavi A, et al. Brain antigen-reactive CD4+ T cells are sufficient to support learning behavior in mice with limited T cell repertoire. Brain Behav Immun. 2014;35:58–63. doi: 10.1016/j.bbi.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Derecki NC, et al. Regulation of learning and memory by meningeal immunity: a key role for IL-4. J Exp Med. 2010;207:1067–1080. doi: 10.1084/jem.20091419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wolf SA, et al. CD4-positive T lymphocytes provide a neuroimmunological link in the control of adult hippocampal neurogenesis. J Immunol Baltim Md 1950. 2009;182:3979–3984. doi: 10.4049/jimmunol.0801218. [DOI] [PubMed] [Google Scholar]
- 104.Marin I, Kipnis J. Learning and memory … and the immune system. Learn Mem Cold Spring Harb N. 2013;20:601–606. doi: 10.1101/lm.028357.112. [DOI] [PMC free article] [PubMed] [Google Scholar]


