Abstract
Eruptive xanthoma (EX) is a very rare dermatosis mostly occurring due to high levels of serum triglycerides or uncontrolled diabetes mellitus. When EX is encountered, it is important to keep in mind that it could be a sign of severe underlying metabolic derangements. Early recognition can help avoid serious complications such as pancreatitis. After treatment of the underlying metabolic disorders, lesions mostly disappear without leaving scars. We present a case of a 55-year-old woman who presented with solely EX lesions and who was eventually diagnosed with diabetes mellitus and severe hypertriglyceridaemia.
Background
Eruptive xanthoma (EX) is a rare type of xanthomas mostly occurring due to high levels of serum triglycerides or uncontrolled diabetes mellitus. The risk of developing EX is higher if the patient has both of these conditions simultaneously.1 2 Patients have high risk for coronary artery disease and pancreatitis due to severe hypertriglyceridaemia.1–3 EX may be an early warning sign of underlying hypertriglyceridaemia and uncontrolled diabetes mellitus. In our case, EX was the first and only symptom of diabetes mellitus and hypertriglyceridaemia. Recognising EX as being part of a serious metabolic disorder and being aware of the fact that EX may be the sole and first symptom of diabetes and severe concomitant hypertriglyceridaemia are important to prevent serious complications such as coronary artery disease and pancreatitis.
Case presentation
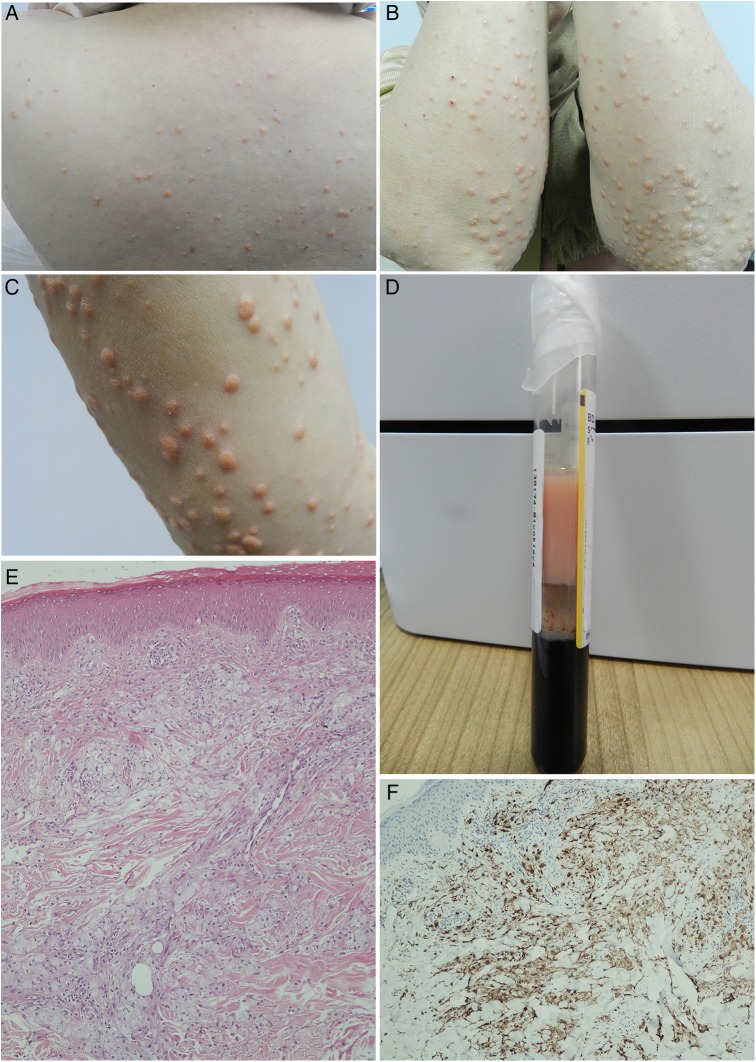
A 55-year-old woman presented with sudden-onset itchy lesions on her arms and legs for almost 20 days. She denied personal or family history for similar lesions. On dermatological examination, there were yellowish, non-follicular papules with erythematous borders, concentrated on both elbows and knees and spreading to the extensor surfaces of the extremities and back (figure 1A–C).
Figure 1.
(A) Yellowish papules on the patient's back. (B) Yellowish papules on forearms. (C) Closer appearance of the lesions. (D) The appearance of the patient's whole blood in tube. (E) Xanthoma cell nests in the dermis (H&E ×100). (F) CD68 positivity for histiocytes (Immunoperoxidase ×200).
Investigations
Laboratory results were as follows: triglyceride 1788 mg/dL, total cholesterol level 324 mg/dL, high-density lipoprotein level 21 mg/dL, fasting glucose level 373 mg/dL, glycated haemoglobin 12% and C reactive protein 12.4 mg/L. The patient denied alcohol or drug use, or any systemic disease, and had no personal or family history of hypertriglyceridaemia or hyperlipoproteinaemia. The patient's hepatitis B surface antigen was positive. Other routine laboratory tests including complete blood counts, aspartate aminotransferase, alanine aminotransferase, creatinine and thyroid-stimulating hormone were within normal ranges. The patient's body mass index was 34.1 kg/m2. Centrifugation of the blood of the patient revealed lipemic plasma with a creamy supernatant in the tube (figure 1D). Her lipoprotein electrophoresis findings were compatible with acquired type V hyperlipoproteinaemia as β lipoprotein was 37.3%, pre-β lipoprotein 39.2%, α lipoprotein 19.2% and chylomicrons was 4.3%. She had no systemic symptoms of any kind. She had not undergone a medical check-up in recent years, so was not aware of her diabetes mellitus. She did not have any common symptoms of diabetes mellitus, such as xerostomia, weight changes, polyuria and polydipsia. A biopsy sample was taken from a lesion on the right elbow. Histopathological examination showed multiple nests of large, pale staining, lipid-laden histiocytes (foamy cells) in the dermis (figure 1E). These cells stained positive for CD68 (figure 1F). Abdominal ultrasound revealed grade 2 hepatosteatosis.
Differential diagnosis
Molluscum contagiosum, juvenile xanthogranuloma, necrobiotic xanthogranuloma, lichen planus and papular granuloma annulare are among the gamut of differential diagnosis of EX.2 4 5 The diagnosis can easily be made with typical appearance and spread of the lesions, but biopsy may be required to confirm the diagnosis in selected cases. Histopathological examination demonstrates macrophages with a foamy cytoplasm and dermal extracellular lipids.5
Treatment
On the basis of the clinical and histopathological findings, the patient was diagnosed as EX. She was referred to an endocrinologist for treatment and further follow-up. Gemfibrozil 600 mg two times per day, cholestyramine 9 g two times per day, insulin glargine 1×22 IU and insulin aspart 3×6 IU were started.
Outcome and follow-up
Subsequently, the patient's biochemical values returned to normal range and the EX lesions fully resolved with slight hyperpigmentation within a month, without dermatological treatment (figure 2A, B).
Figure 2.
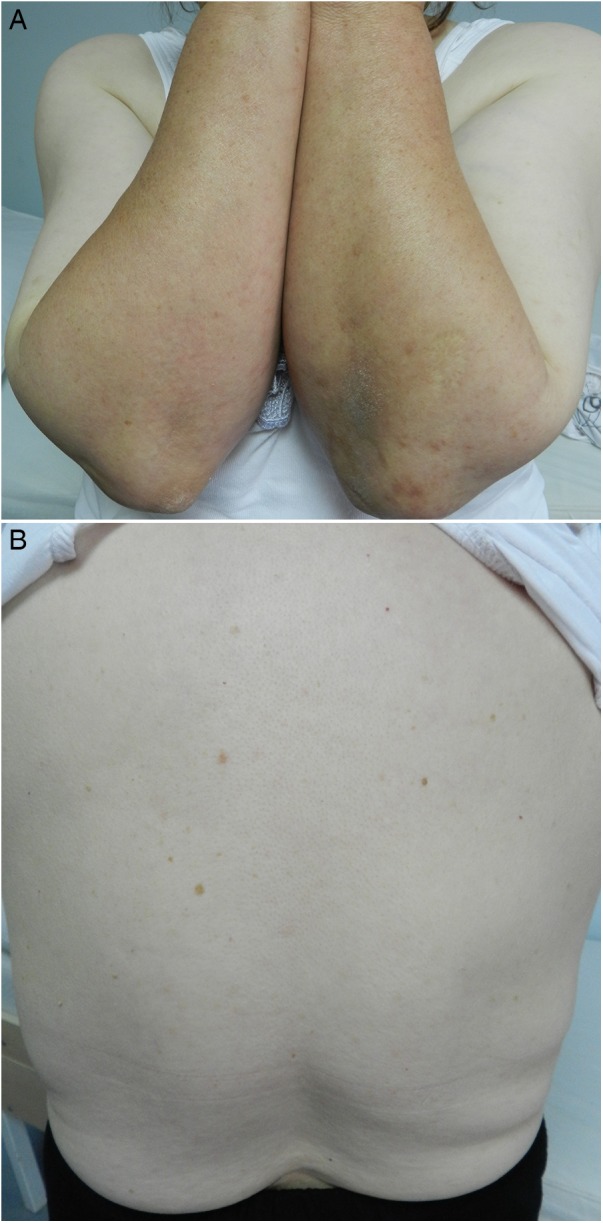
Appearance of the patient's forearms (A) and back (B) 1 month after the first visit.
Discussion
EX is characterised by numerous sudden-onset yellow papules, 1–4 mm in diameter, surrounded by an erythematous halo; they are usually observed on the extensor surfaces of the extremities.3 6 They may be itchy and Koebner phenomenon may be positive in some.2 After treatment for the underlying disease, these lesions usually heal without leaving scars.2 3
EX occurs due to familial hyperchylomicronaemia, or because of conditions leading to hypertriglyceridaemia, such as obesity, hypothyroidism, alcohol abuse, systemic oestrogen replacement or retinoid or corticosteroid therapy.1–3 6 It most commonly develops in type V hyperlipidaemia.7 Type V hyperlipoproteinaemia is a relatively rare form of hyperlipoproteinaemia, and is accompanied by an increase in very low-density lipoprotein and chylomicron according to Fredrickson's classification.8 Samples of lipemic plasma show a creamy supernatant, indicating the presence of chylomicrons, when serum is allowed to stand for 24 h at 4°C. Type V hyperlipoproteinaemia may be congenital or acquired secondary to uncontrolled diabetes mellitus, alcohol consumption or oestrogen treatment.7 8
In conclusion, it is important to keep in mind that EX may be a harbinger of an underlying uncontrolled metabolic condition and completely disappears with its treatment.
Learning points.
Eruptive xanthoma (EX) may be an early warning sign of underlying hypertriglyceridaemia and uncontrolled diabetes mellitus.
Recognising EX as being part of a serious metabolic disorder and being aware of the fact that EX may be the sole and first symptom of diabetes and severe concomitant hypertriglyceridaemia are important to prevent serious complications such as coronary artery disease and pancreatitis.
After treatment of the underlying metabolic abnormality, the lesions usually heal without leaving scars.
Footnotes
Contributors: All the authors read and approved the manuscript. BS performed the dermatological examination and wrote the manuscript. ROK captured the images and performed the literature review. SBA followed up on the patient’s metabolic disorders and contributed to the manuscript. MK carried out the histopathological examination.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Digby M, Belli R, McGraw T et al. Eruptive xanthomas as a cutaneous manifestation of hypertriglyceridemia: a case report. J Clin Aesthet Dermatol 2011;4:44–6. [PMC free article] [PubMed] [Google Scholar]
- 2.Loeckermann S, Braun-Falco M. Eruptive xanthomas in association with metabolic syndrome. Clin Exp Dermatol 2010;35:565–6. 10.1111/j.1365-2230.2009.03477.x [DOI] [PubMed] [Google Scholar]
- 3.Parker F. Xanthomas and hyperlipidemias. J Am Acad Dermatol 1985;13:1–30. 10.1016/S0190-9622(85)70139-9 [DOI] [PubMed] [Google Scholar]
- 4.Villalón G, Martín JM, Monteagudo C et al. [Eruptive xanthomas after onset of diabetes mellitus]. Actas Dermosifiliogr 2008;99:426–7. 10.1016/S0001-7310(08)74712-4 [DOI] [PubMed] [Google Scholar]
- 5.Holsinger JM, Campbell SM, Witman P. Multiple erythematous-yellow, dome-shaped papules. Am Fam Physician 2010;82:517–20. [PubMed] [Google Scholar]
- 6.Ladizinski B, Lee KC. Eruptive xanthomas in a patient with severe hypertriglyceridemia and type 2 diabetes. CMAJ 2013;185:1600–50. 10.1503/cmaj.130148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park JR, Jung TS, Jung JH et al. A case of hypothyroidism and type 2 diabetes associated with type V hyperlipoproteinemia and eruptive xanthomas. J Korean Med Sci 2005;20:502–5. 10.3346/jkms.2005.20.3.502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gotoda T, Shirai K, Ohta T et al. Diagnosis and management of type I and type V hyperlipoproteinemia. J Atheroscler Thromb 2012;19:1–12. 10.5551/jat.10702 [DOI] [PubMed] [Google Scholar]