Abstract
Accidental ingestion of a denture is an acute emergency, and the denture is usually removed on the same day it is discovered. We present a patient who had a seizure while asleep, during which his denture broke; he accidentally swallowed a major part of it, which had a clasp attached. He was unaware that he had ingested the denture, since he was asymptomatic, but he started developing symptoms after 5 days and presented to us on the eighth day of ingestion. With much difficulty, the impacted section of the denture in the distal oesophagus was removed with the combined effort of flexible endoscopy and a rigid oesophagoscopy. Post-procedure, the patient developed mediastinitis, which was managed conservatively; he is doing well on follow-up.
Background
The diagnosis of the presence of old and forgotten foreign bodies in the oesophagus requires a high index of clinical suspicion. The removal of such foreign bodies may also be difficult. There is no standardised management protocol and the procedure should be tailored to suit individual cases. Interdisciplinary cooperation may be required for successful management of the situation and also for complications that may arise. Doctors managing the emergency room should be aware of the intricacies of diagnosis and management of this potentially risky condition.
Case presentation
A 55-year-old man presented with the symptoms of difficulty in swallowing, a feeling of tightness of the chest and cough for the last 2 days. He had seizure disorder since childhood and was on regular anticonvulsants. Seven days prior to the presentation, he had experienced one episode of seizure while asleep with his denture on. During the seizure, the denture broke, and he accidentally ingested a major part of it, which had a clasp. The next day, when the patient awakened, he found a piece of his denture lying on the floor. He searched for the remaining part but could not find it and, since he was completely asymptomatic, he thought that the remaining part of the denture was missing and continued his routine. After 5 days, he started developing difficulty in swallowing, with food being caught in his mid-chest along with a cough and chest tightness. The symptoms gradually worsened and, on the eighth day, he presented to the gastroenterology department. A chest X-ray was taken, which showed the clasp of the denture lying in the distal oesophagus (figure 1). An upper gastrointestinal (UGI) endoscopy was performed under general anaesthesia after securing the airway, which showed the denture lying vertically in the oesophagus, 32 cm from the incisors. One edge of the denture was impacted into the wall of the oesophagus and the clasp was not seen clearly since it was on the other side of the denture (figure 2).
Figure 1.
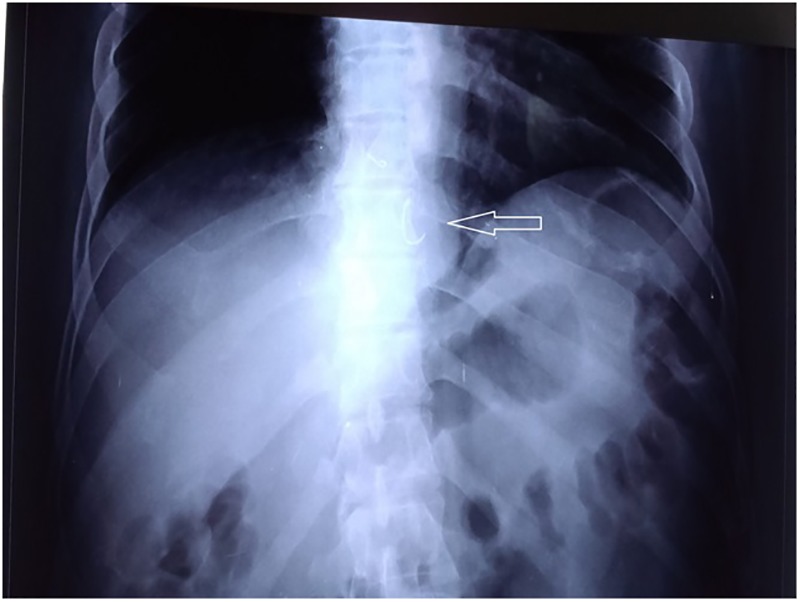
X-ray showing radiopaque clasp of the denture at the distal end of the oesophagus (white arrow).
Figure 2.
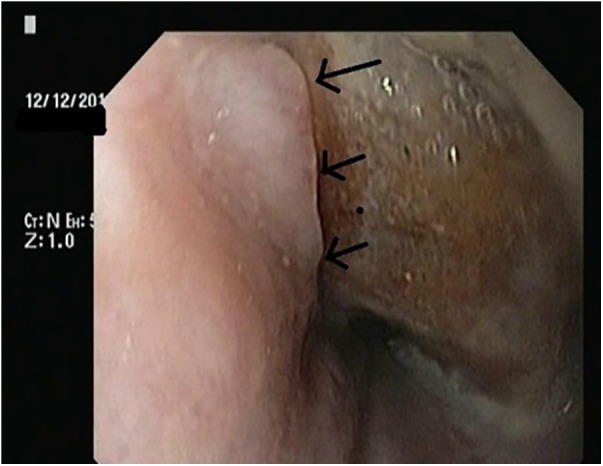
Endoscopic picture showing impacted (black arrows) denture at the lower end of the oesophagus.
Treatment
Our plan was to initially attempt to disimpact the denture endoscopically with the available accessories and then, if successful, to remove the denture endoscopically. The ear, nose and throat (ENT) surgeon and cardiothoracic surgeon on call were alerted, so that if we faced a problem they would be on hand to help. The denture was grasped with alligator forceps, but since it was deeply impacted and because of the shape of the denture and the difficult positioning, it slipped several times on this attempt. After much difficulty, the denture was disimpacted, but it again slipped back into the oesophagus while we were trying to remove it. It was again snagged, this time with a polypectomy snare, and brought up to the cricopharynx, but it was difficult to remove from the cricopharynx because of poor vision and the fact that the clasp was on the other side of the denture and not seen clearly. Since a suitable overtube was not available, the section of the denture was again placed in the upper oesophagus and, with the help of the ENT surgeon, using a rigid oesophagoscopy, it was removed (figure 3). Following the procedure, the patient developed subcutaneous emphysema around the neck. He also developed a fever the next morning, with an elevated white cell count, and hence started on antibiotics; a contrast-enhanced CT (CECT) of the thorax was performed to rule out perforation. CECT of the thorax revealed mediastinitis (localised air collection adjacent to the upper third of the oesophagus), with left-sided pleural effusion, however, there was no leak seen on giving oral contrast (figure 4). Hence the patient was kept nil per oral, and antibiotics were continued. With conservative treatment he gradually improved and was fed orally after 10 days. There were no further complications and he was discharged after 2 days of starting oral feeding.
Figure 3.
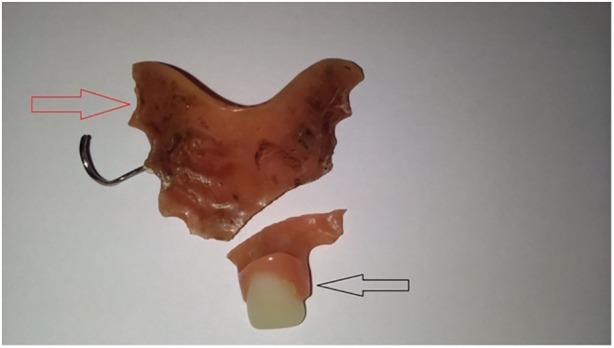
Picture showing the removed partial denture (red arrow) along with the remaining part of the denture that was not swallowed (black arrow).
Figure 4.
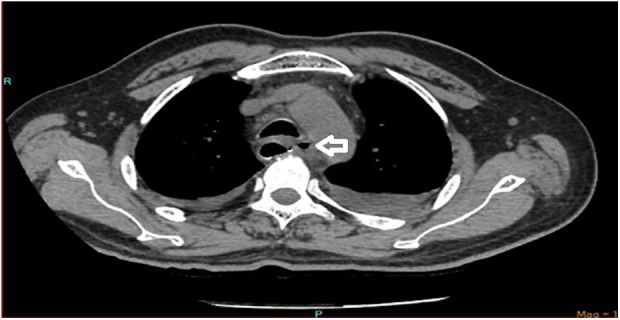
CT of the thorax showing free air in the mediastinum (white arrow).
Outcome and follow-up
The patient has been followed up for the past 4 months and is doing well, with no difficulty swallowing. He was advised a dental implant instead of a removable denture and is following up for this in the dental department.
Discussion
Denture ingestion is a commonly encountered problem and accounts for about 11.5% of impacted tracheal or oesophageal foreign bodies, according to a study by Abdullah et al.1 In adults, denture ingestion usually occurs after trauma, intoxication, loss of consciousness or during sleep.2 Ill-fitting and damaged dentures can also be accidentally ingested while eating food and drinking water. Seizure patients have an increased risk of denture ingestion during episodes of seizure and hence selection of a suitable denture for them is important. Removable acrylic dentures are not routinely advised for seizure patients since the denture can get dislodged and can either get ingested accidentally or cause considerable local trauma during episodes of seizure. Hence for these reasons, though costly, non-removable fixed prostheses (implants or bridge) are the better option.3
Sharp-pointed objects lodged in the oesophagus are a medical emergency.4 Ingested dentures with sharp clasps impacted in the oesophagus have to be removed as early as possible, as the prognosis depends on how early one recognises the problem and deals with it. However, delayed presentation of denture ingestion is not uncommon and presentations as late as 6 months have been reported.5 Complications of denture ingestion include obstruction and perforation of the oesophagus, mediastinitis, pneumothorax, pneumopericardium, tracheo-oesophageal, aorto-oesophageal and even oesophagobronchoaortic fistulas, aortic erosion, enterocolonic fistulas and colonic perforation; these complications are more commonly seen in delayed presentations.6
There are many problems in identifying and diagnosing denture ingestion. First, patients may not be fully aware that they have swallowed a denture, especially in cases of accidental ingestion of ill-fitting and damaged dentures during the process of eating and drinking, and while sleeping, or if unconscious. Second, most dentures are radiolucent and hence radiological identification is difficult. To make things worse, patients may be totally asymptomatic in the initial few days, hence only a high index of suspicion and thorough initial ENT examination is essential, and, if required, an UGI endoscopy may also be performed before ruling out the possibility of denture ingestion. Patients with denture ingestion may present with various symptoms, including neck pain, dysphonia, dysphagia, excessive salivation, sore throat, choking sensation, retrosternal pain, fever, haemoptysis, regurgitation of undigested food and odynophagia.7 In one of the largest series of impacted dentures, the cervical section of the oesophagus was the commonest site of impaction, and dysphagia and tracheal tenderness were the most consistent features of denture impaction in the upper oesophagus.8 Our patient was totally asymptomatic in the initial 4 days, and hence did not seek medical attention. The usual site of impaction of foreign bodies corresponds to the physiological site of narrowing, and any impaction away from the sites of natural constriction should arouse suspicion of pathological narrowing of the lumen or penetration of the wall of the oesophagus at that site. The lumen should be inspected after removal of the foreign body, to exclude such probabilities. In our case, the site of impaction was quite unusual, and impaction was mainly due to penetration of the denture into the oesophagus. Repeat endoscopy was not carried out in our patient since the oral contrast study was normal and the patient was completely asymptomatic on follow-up.
There is no standard protocol followed for the removal of the ingested dentures in the oesophagus as it usually depends on the type of denture, its location, and availability of expertise accessories. The choice between flexible and rigid endoscopy for removal of oesophageal foreign bodies remains controversial. Rigid endoscopy gives a much better view of the cervical oesophagus, whereas a flexible endoscope gives an excellent view of the thoracic oesophagus and oesophagogastric junction.9 However, this has to be ideally performed using a multidisciplinary approach involving a gastroenterologist, ENT surgeon and a cardiothoracic surgeon. Small dentures without a sharp clasp can be removed by a flexible endoscope with the help of foreign body forceps or a polypectomy snare with or without an overtube, irrespective of the denture's position in the oesophagus. In the upper oesophagus, large dentures and dentures with a sharp clasp can be removed by a rigid oesophagoscope since vision is good, and, if required, they can be broken and the pieces removed. However, they can also be removed by a flexible endoscopy, if suitable accessories are available. If they are in the mid or distal oesophagus, treatment has to be individualised, and it is always better to initially make an attempt with a flexible endoscope and an overtube, as these are extremely useful in such cases. Care should be taken while the denture is being negotiated through the cricopharynx, because it may not be performed under vision and there is a high chance of injury and perforation, especially in the presence of a clasp. While retrieving, if it is not possible to negotiate it across the cricopharynx, the denture can be left in the upper oesophagus and removed with a rigid oesophagoscope, as was done in our case. In the case of an impacted denture, it is extremely difficult to remove it endoscopically and, again, the protocol has to be individualised. Gentle disimpaction can be achieved endoscopically, as was done in our case, but if the impaction is deeper and if the attempt to disimpact is unsuccessful, or if the patient develops any immediate procedural complications requiring surgery, the patient has to be operated on by a cardiothoracic surgeon. The literature regarding management of impacted dentures in the oesophagus is sparse, and there are few reports on failures in the first attempt; in some cases, where repeated attempts of endoscopic removal had failed and sharp ends were impacted or had penetrated the wall of the oesophagus, some sort of improvisation of the procedure or oesophagotomy had been needed for removal of the foreign body.10–12 The success of endoscopic removal in such cases mainly depends on the duration of impaction, with increased failure rate corresponding to longer duration of impaction. The need for surgical intervention is also greater in these cases when compared to cases of dentures presenting without impaction.
Monitoring of the patient after the removal of the ingested denture is, again, important, and it is always safer to exclude any complications before starting oral feeding. In our case, the patient had a fever the day following surgery, and a CECT with oral contrast performed the subsequent day showed mediastinitis with left-sided pleural effusion, with no obvious leak of contrast outside the oesophagus. Two possibilities were considered, namely, an iatrogenic microperforation during the rigid oesophagoscope, or a microperforation secondary to impaction of the denture. In situations such as this, a subcutaneous emphysema in the neck following the procedure along with localised air collection surrounding the cervical part of the oesophagus on imaging usually favours a perforation in the cervical oesophagus as a complication related to use of a rigid oesophagoscope, while a localised air collection surrounding the part of oesophagus at the site of impaction without a subcutaneous emphysema of the neck might favour a complication secondary to the deep impaction or a complication related to disimpaction of the denture.6 In our case, there was subcutaneous emphysema immediately following the removal of the denture, and localised air collection was seen adjacent to the upper third of the oesophagus, favouring the possibility of a cervical oesophageal microperforation. However, with conservative measures, the patient improved and was eventually discharged in a healthy state. To conclude, denture ingestion is a medical emergency, and removal of the denture, if impacted in the oesophagus, has to be carried out using a multidisciplinary approach, with careful monitoring of the patient after the procedure.
Learning points.
Removable acrylic dentures should generally be avoided in patients with seizure disorders and, instead, a non-removable fixed prosthesis is a better option especially to avoid complication such as accidental denture ingestion.
Large dentures with a clasp are extremely difficult to remove from the oesophagus, and present a high rate of complications, hence requiring a multidisciplinary approach.
Accidental denture ingestion may very rarely be asymptomatic for the initial few days, hence it is extremely important to rule out the possibility of denture ingestion by thorough investigations, when in doubt.
Mediastinitis following removal of a denture from the oesophagus can be managed conservatively if there is no leak on oral contrast study.
Acknowledgments
The authors would like to acknowledge Professor Ananthakrishnan, from the Department of General Surgery, for playing a major role in helping us manage this patient.
Footnotes
Twitter: Follow Vinoth Boopathy at @drbvinoth
Contributors: VB was the interventional endoscopist. SSB was the ENT specialist involved in removal of the denture. VB prepared the main manuscript. SSB and SD helped in the literature review. PB helped in providing the radiological pictures and edited the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Abdullah BJ, Teong LK, Mahadevan J et al. Dental prosthesis ingested and impacted in the esophagus and orolaryngopharynx. J Otolaryngol 1998;27:190–4. [PubMed] [Google Scholar]
- 2.Firth AL, Moor J, Goodyear PWA et al. Dentures may be radiolucent. Emerg Med J 2003;20:562–3. 10.1136/emj.20.6.562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karolyhazy K, Kivovics P, Fejerdy P et al. Prosthodontic status and recommended care of patients with epilepsy. J Prosthet Dent 2005;93:177–82. 10.1016/j.prosdent.2004.11.008 [DOI] [PubMed] [Google Scholar]
- 4.Ikenberry SO, Jue TL, Anderson MA et al. , ASGE Standards of Practice Committee. Management of ingested foreign bodies and food impactions. Gastrointest Endosc 2011;73:1085–91. 10.1016/j.gie.2010.11.010 [DOI] [PubMed] [Google Scholar]
- 5.Rathore PK, Raj A, Sayal A et al. Prolonged foreign body impaction in the esophagus. Singapore Med J 2009;50:e53–54. [PubMed] [Google Scholar]
- 6.Kulendra KN, Skilbeck CJ, Blythe J et al. Delayed presentation of a swallowed partial denture. BMJ Case Rep 2010;2010:pii: bcr10.2009.2401 10.1136/bcr.10.2009.2401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haidary A, Leider JS, Silbergleit R. Unsuspected swallowing of a partial denture. AJNR Am J Neuroradiol 2007;28:1734 10.3174/ajnr.A0658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bandyopadhyay SN, Das S, Das SK et al. Impacted dentures in the oesophagus. J Laryngol Otol 2014;128:468–74. 10.1017/S002221511400070X [DOI] [PubMed] [Google Scholar]
- 9.Lam HC, Woo JK, van Hasselt CA. Management of ingested foreign bodies: a retrospective review of 5240 patients. J Laryngol Otol 2001:115:954–7. [DOI] [PubMed] [Google Scholar]
- 10.Yadav R, Mahajan G, Mathur RM. Denture plate foreign body of esophagus. IJTCVS 2008;24:191–4. [Google Scholar]
- 11.Fang R, Sun J, Hu Y et al. Endoscopic removal of esophageal impacted dentures. Ann Otol Rhinol Laryngol 2010;119:249–51. 10.1177/000348941011900407 [DOI] [PubMed] [Google Scholar]
- 12.Adobamen PO, Ediale J. Diagnostic and therapeutic strategies in denture removal after ingestion in a developing and emerging country—Nigeria. Arch Clin Exp Surg 2013;2:97–100. (cited 7 August 2015) 10.5455/aces.20120725025451 [DOI] [Google Scholar]


