Abstract
Persistent gastrocutaneous fistula (GCF) is a difficult to manage complication following gastrostomy tube removal, with leakage resulting in distressing sequelae including cutaneous injury, infection and dehydration. Many such patients are high-risk for invasive surgery and, to date, endoscopic closure techniques, including clipping systems, have limitations. We present the case of a 62-year-old woman with persistently leaking GCF 6 months postgastrostomy tube removal, despite maximal antisecretory therapy and postpyloric feeding, and describe failed attempted endoscopic closure with conventional clips. Treatment options were discussed and informed consent was given for an attempt at endoscopic closure using a novel radial closure device (‘Padlock clip’) combined with surgical de-epithelialisation, with the understanding that this device has never previously been used in this setting. At follow-up 2 weeks postprocedure, the patient was asymptomatic with complete healing of the GCF. This approach has advantages over other endoscopic closure techniques and can be considered as an alternative approach to GCF closure.
Background
Chronic gastrocutaneous fistulae (GCF) are a difficult to manage complication following percutaneous gastrostomy tube removal, with an estimated incidence of around 4.5%.1 The duration of gastrostomy use (>6 months duration) and resultant epithelialisation of the tract are critical factors in the development of GCF,2–4 hence de-epithelialisation may be important in treating refractory cases. While the majority of gastrostomy sites close spontaneously within 1–3 months,4 some of those that become chronic may respond to conservative measures to optimise healing including drugs such as proton pump inhibitors and somatostatin analogues to minimise gastric secretions, prokinetics to increase gastric emptying and postpyloric feeding.5 Defects that prove refractory to these measures and continue to discharge large volumes of gastric output can cause considerable morbidity to these patients, with recognised complications including cutaneous injury, risk of infection, dehydration, electrolyte disturbance and requirement for frequent dressings and stoma bags. Traditionally, prior to advances in gastrointestinal (GI) endoscopy, such patients would have ultimately required surgical closure via laparotomy with de-epithelialisation of the GCF tract, gastric repair and fascial closure. However, given that many gastrostomy fed patients have multiple co-morbidities rendering them poor surgical candidates, the emergence of less-invasive endoscopic options has been an important development. Successful outcomes have been reported for GCF with endoscopic clip closure6–12 and endoscopically assisted suturing techniques.13–15 A combined approach to de-epithelialise the tract in addition to mechanical endoscopic closure has been advocated in the majority of published cases,6 7 10 13 15 thereby mimicking the surgical approach, with good results, albeit limited to small series and case reports. Given that endoscopic clip closure is less invasive than endoscopically assisted suturing, it is often the first-line approach. Whereas conventional endoscopic clips were limited in terms of the amount of GCF tissue that can be entrapped and held, making the procedures technically difficult and cumbersome, over-the-scope clips with a ‘bear-claw’ design, which are now widely available, have been an advance and are felt to be superior in this regard.8–9 11 The Padlock clip (Diagmed Healthcare Ltd, North Yorkshire, UK) is a novel over-the-scope clip that has been developed with a radial closure design to ensure greater ability to approximate and circumferentially entrap tissue for a more robust closure of perforations, surgical gastrostomies and fistulae. The Padlock clip has been shown to be effective for gastrostomy closure in preclinical animal model studies,16 17 but, to our knowledge, has never been attempted for GCF closure until the present case.
Case presentation
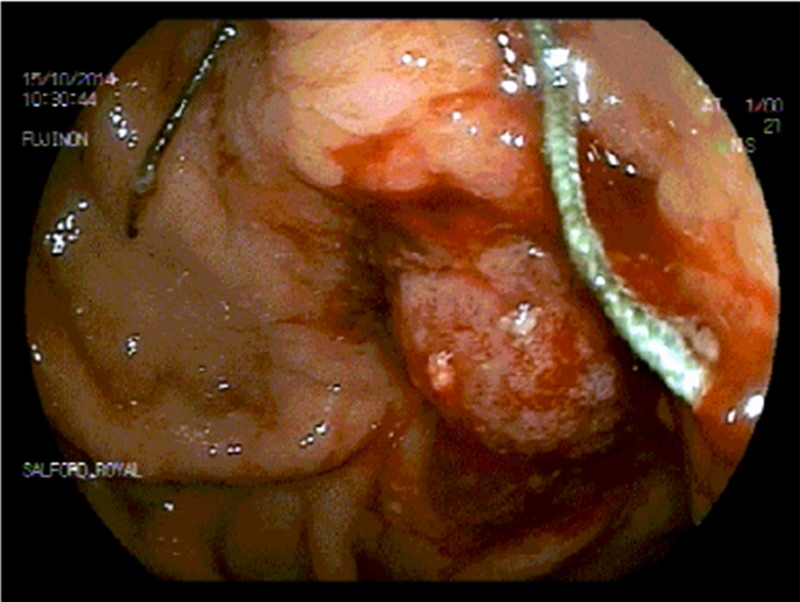
A 62-year-old woman had a long-standing history of complex nutritional problems following multiple previous abdominal surgeries including caesarean section, oophorectomies for ovarian cysts, hysterectomy and subsequent small bowel resection and sigmoid resection due to obstruction secondary to extensive adhesions with subsequent reversal of transverse colostomy. She was under long-term follow-up in the tertiary advanced nutrition and gastroenterology service at Salford Royal Foundation Trust. From a nutritional point of view, her symptoms included features of postoperative short bowel syndrome and delayed gastric emptying, and she had required postpyloric enteral feeding via a radiologically placed percutaneous gastrojejunostomy feeding tube for over 10 years. Long-term oral intake had been limited to oral fluids during this time. Jejunal feeding had been well tolerated and maintained her nutritional requirements, with periodic tube changes via the same gastrostomy tract. Unfortunately, over a period of several months, the patient had noticed increasing amounts of peristomal leakage of gastric contents at the exit site, leading to cutaneous injury and requirement of frequent dressings. This problem remained despite prokinetic and antisecretory medications. Ultimately, a decision was made to remove this feeding tube and resite it at a new gastrostomy site. However, the earlier gastrostomy site continued to leak large volumes of gastric content, with ongoing symptoms at the exit site, which failed to heal at 3 months post-tube removal. This was despite postpyloric feeding and optimal medical therapy. Given the situation, an attempt was made to close the defect endoscopically, initially with conventional endoscopic clips (Resolution Clip, Boston Scientific, Massachusetts, USA). Unfortunately, this was also unsuccessful, and the leaking defect and its associated symptoms persisted (figure 1).
Figure 1.

Leaking gastrocutaneous fistula preprocedure.
Treatment
At a subsequent outpatient review, the patient was offered the choice of either referral to upper GI surgeons for surgical closure, endoscopically assisted suturing15 or an attempt at closure using an over-the-scope endoscopic clip (OTSC). Understandably, given the patients extensive surgical history, she was not keen to pursue a further operation at this stage. When discussing endoscopic closure and OTSC systems with the patient, we introduced the possibility of using a novel radial closure device (Padlock clip, Diagmed Healthcare Ltd, North Yorkshire, UK) (figure 2) and explained its potential advantages over similar previously used concept systems with a ‘bear-claw’ design, which have been successfully used according to several reports in the literature.8 9 11 The patient made an informed decision to have an attempted endoscopic closure with the Padlock clip. Informed consent was obtained, with the patient understanding that this particular device had not, to our knowledge, been previously used in this specific clinical setting. The procedure was performed 6 months after removal of the feeding tube. Diagnostic upper GI endoscopy was performed using a standard diagnostic endoscope with the patient under general anaesthesia. The radial closure device cap was mounted to the tip of the endoscope prior to the procedure. The fistula was identified at the internal gastric end via a thin plastic catheter (figure 3). The external opening of the fistula epithelium was then excised and freshened surgically. After removal of the plastic catheter, the internal fistula opening and surrounding mucosa were suctioned endoscopically into the radial closure device cap and the device was deployed (figure 4).
Figure 2.

The Padlock clip.
Figure 3.

Endoscopic view showing the gastrocutaneous fistula with plastic cannula in its lumen encircled by the radial closure device cap attached to the endoscope.
Figure 4.
Endoscopic view after deployment of the radial closure Padlock clip device.
A ‘leak test’ with water applied externally during internal air insufflation confirmed an air tight seal. The small external skin defect was then closed with a suture. The patient was given intravenous antibiotics for 48 h, then discharged home on oral antibiotics. She resumed oral fluids the day following the procedure.
Outcome and follow-up
At outpatient clinic follow-up 2 weeks postprocedure, there were no complications and complete healing of the GCF (figure 5) was confirmed, with complete resolution of all symptoms at the exit site. Given that the GCF site had completely healed, the sutures were removed during this visit. The patient was extremely pleased with the outcome of this minimally invasive approach. Outpatient clinic review at 10 months postprocedure confirmed long-term success of the procedure, with the patient remaining asymptomatic with a healthy, healed appearance at the former GCF site.
Figure 5.
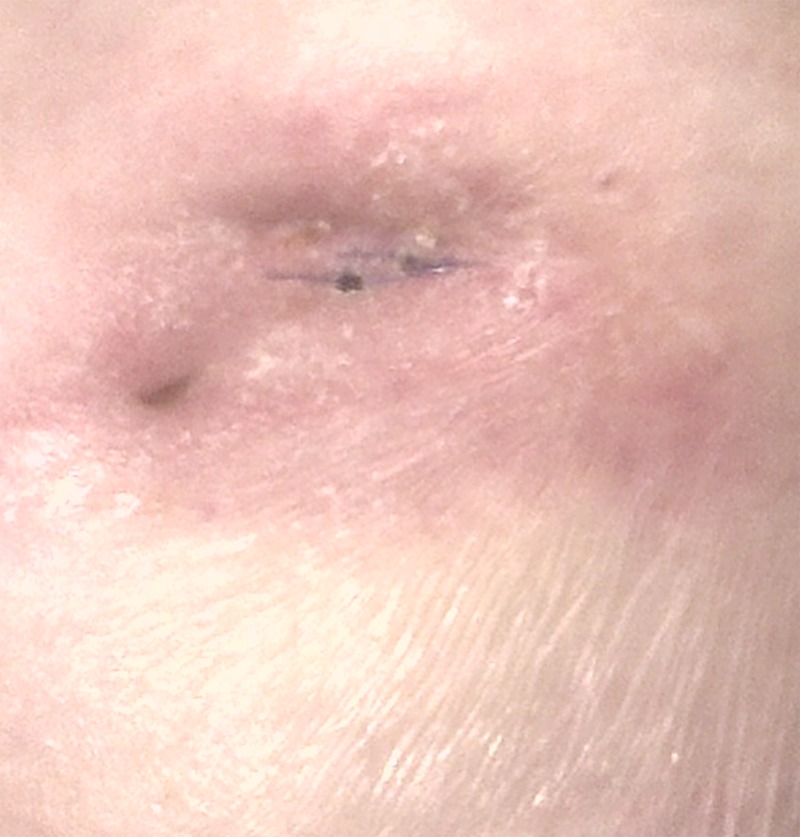
Abdominal image taken at follow-up 2 weeks postprocedure confirming healing of the fistula site.
Discussion
To our knowledge this is the first use of the Padlock clip for closure of a refractory GCF. Our experience would suggest that this device is easy to use in these circumstances, is less invasive than suturing approaches and could be considered as an alternative approach to this rare but troublesome complication of percutaneous gastrostomy tubes. Advantages of this system compared to the OTSC with a ‘bear claw’ design8 9 11 pertain to the circumferential compression and ability to grasp more tissue, providing a more robust closure. These factors, along with the promising data in animal models16 17and the patients decision to proceed with it ahead of alternatives such as OTSC with ‘bear-claw’ design, previously described in this setting, strongly influenced our decision to recommend this device as a therapeutic option.
The aetiology of this GCF in the present case was likely secondary to epithelialisation of the tract, given the chronicity of gastrostomy use, and contributed to it by delayed gastric emptying. Therefore, our decision to combine the endoscopic closure procedure with surgical de-epithelialisation may have contributed to the successful outcome. Other non-surgical options for de-epithelialisation in the literature have included electro and chemical cautery, argon beam photocoagulation and biopsy removal6 7 10 13 15; these could potentially be used in conjunction with the Padlock clip as an alternative to surgical excision.
This novel technique has added to the growing number of endoscopic approaches available for closure of GCFs. Randomised clinical trials are now required to determine the most effective approach and evaluate the added benefit of a combined de-epithelialisation procedure.
Learning points.
Clinicians should be aware of gastrocutaneous fistula (GCF) as a rare but difficult to manage complication post gastrostomy removal, associated with considerable morbidity.
If conservative management fails, an endoscopic closure procedure should be considered, particularly in poor surgical candidates, as there are several endoscopic options now available.
The earlier endoscopic clips for GCF closure have limited ability to grasp tissue, making procedures technically challenging, with variable success.
Here we describe the first ever use of the Padlock clip for GCF closure and report a successful outcome. This system has an advantageous radial design compared with previously used clips.
Combining endoscopic mechanical closure with de-epithelialisation may be important in achieving successful closure.
Acknowledgments
The authors would like to acknowledge Mrs Susan Wood for administrative support and Mr John Bolton, senior clinical photographer at Salford Royal NHS Foundation Trust.
Footnotes
Contributors: AA and DHV contributed equally to this work and should be considered as joint first authors. We confirm that all the authors met the authorship criteria for BMJ case reports by being involved in the concept and design of the procedure reported and its presentation, and drafting of the manuscript including critical reviews for intellectual content; all the authors approved the final version of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bratu I, Bharmal A. Incidence and predictors of gastrocutaneous fistula in the pediatric patient. ISRN Gastroenterol 2011;2011:686803 10.5402/2011/686803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Papavramidis TS, Mantzoukis K, Michalopoulos N. Confronting gastrocutaneous fistulas. Ann Gastroenterol 2011;24:16–19. [PMC free article] [PubMed] [Google Scholar]
- 3.Gordon JM, Langer JC. Gastrocutaneous fistula in children after removal of gastrostomy tube: incidence and predictive factors. J Pediatr Surg 1999;34:1345–6. 10.1016/S0022-3468(99)90008-8 [DOI] [PubMed] [Google Scholar]
- 4.El-Rifai N, Michaud L, Mention K et al. Persistence of gastrocutaneous fistula after removal of gastrostomy tubes in children: prevalence and associated factors. Endoscopy 2004;36:700–4. 10.1055/s-2004-825662 [DOI] [PubMed] [Google Scholar]
- 5.Vasant DH, Lal S, Blackett BD et al. Closure of a large high-output gastrocutaneous fistula with combined postpyloric feeding and aggressive medical therapy. BMJ Case Rep 2012;2012:pii: bcr2012007267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duddempudi S, Ghevariya V, Singh M et al. Treatment of persistently leaking post PEG tube gastrocutaneous fistula in elderly patients with combined electrochemical cautery and endoscopic clip placement. South Med J 2009;102:585–8. 10.1097/SMJ.0b013e3181a5a6a2 [DOI] [PubMed] [Google Scholar]
- 7.Hameed H, Kalim S, Khan YI. Closure of a nonhealing gastrocutanous fistula using argon plasma coagulation and endoscopic hemoclips. Can J Gastroenterol 2009;23:217–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kothari TH, Haber G, Sonpal N et al. The over-the-scope clip system—a novel technique for gastrocutaneous fistula closure: the first North American experience. Can J Gastroenterol 2012;26:193–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kouklakis G, Zezos P, Liratzopoulos N et al. Endoscopic treatment of a gastrocutaneous fistula using the over-the-scope-clip system: a case report. Diagn Ther Endosc 2011;2011:384143 10.1155/2011/384143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Teitelbaum JE, Gorcey SA, Fox VL. Combined endoscopic cautery and clip closure of chronic gastrocutaneous fistulas. Gastrointest Endosc 2005;62:432–5. 10.1016/j.gie.2005.04.047 [DOI] [PubMed] [Google Scholar]
- 11.Turner JK, Hurley JJ, Ketchell I et al. Over-the-scope clip to close a fistula after removing a percutaneous endoscopic gastrostomy tube. Endoscopy 2010;42(Suppl 2):E197–8. 10.1055/s-0030-1255693 [DOI] [PubMed] [Google Scholar]
- 12.Peter S, Geyer M, Beglinger C. Persistent gastrocutaneous fistula after percutaneous gastrostomy tube removal. Endoscopy 2006;38:539–40. 10.1055/s-2006-925245 [DOI] [PubMed] [Google Scholar]
- 13.Eskaros S, Ghevariya V, Krishnaiah M et al. Percutaneous endoscopic suturing: an effective treatment for gastrocutaneous fistula. Gastrointest Endosc 2009;70:768–71. 10.1016/j.gie.2009.05.002 [DOI] [PubMed] [Google Scholar]
- 14.Tasaki T, Arakaki Y, Murakami K et al. Closure of persistent gastrocutaneous postpercutaneous endoscopic gastrostomy fistula by simple percutaneous suturing with endoscopic assist. Gastrointest Endosc 2012;76:699–700. 10.1016/j.gie.2012.03.1404 [DOI] [PubMed] [Google Scholar]
- 15.Vasant DH, Abraham A, Paine PA. Endoscopically assisted suturing of a persistent gastrocutaneous fistula by using a site closure device. Gastrointest Endosc 2013;78:553–4. 10.1016/j.gie.2013.04.001 [DOI] [PubMed] [Google Scholar]
- 16.Desilets DJ, Romanelli JR, Earle DB et al. Gastrotomy closure with the lock-it system and the Padlock-G clip: a survival study in a porcine model. J Laparoendosc Adv Surg Tech A 2010;20:671–6. 10.1089/lap.2010.0076 [DOI] [PubMed] [Google Scholar]
- 17.Romanelli JR, Desilets DJ, Earle DB. Natural orifice transluminal endoscopic surgery gastrotomy closure in porcine explants with the Padlock-G clip using the Lock-It system. Endoscopy 2010;42:306–10. 10.1055/s-0029-1243950 [DOI] [PubMed] [Google Scholar]


