Abstract
Introduction
The interstate commerce of unpasteurized fluid milk, also known as raw milk, is illegal in the United States, and intrastate sales are regulated independently by each state. However, U.S. Food and Drug Administration regulations allow the interstate sale of certain types of cheeses made from unpasteurized milk if specific aging requirements are met. We describe characteristics of these outbreaks, including differences between outbreaks linked to cheese made from pasteurized or unpasteurized milk.
Methods
We reviewed reports of outbreaks submitted to the Foodborne Disease Outbreak Surveillance System during 1998–2011 in which cheese was implicated as the vehicle. We describe characteristics of these outbreaks, including differences between outbreaks linked to cheese made from pasteurized versus unpasteurized milk.
Results
During 1998–2011, 90 outbreaks attributed to cheese were reported; 38 (42%) were due to cheese made with unpasteurized milk, 44 (49%) to cheese made with pasteurized milk, and the pasteurization status was not reported for the other eight (9%). The most common cheese–pathogen pairs were unpasteurized queso fresco or other Mexican-style cheese and Salmonella (10 outbreaks), and pasteurized queso fresco or other Mexican-style cheese and Listeria (6 outbreaks). The cheese was imported from Mexico in 38% of outbreaks caused by cheese made with unpasteurized milk. In at least five outbreaks, all due to cheese made from unpasteurized milk, the outbreak report noted that the cheese was produced or sold illegally. Outbreaks caused by cheese made from pasteurized milk occurred most commonly (64%) in restaurant, delis, or banquet settings where cross-contamination was the most common contributing factor.
Conclusions
In addition to using pasteurized milk to make cheese, interventions to improve the safety of cheese include limiting illegal importation of cheese, strict sanitation and microbiologic monitoring in cheese-making facilities, and controls to limit food worker contamination.
Introduction
Pasteurization of milk is considered one of the most effective public health interventions of the 20th century. Before pasteurization and other controls in the dairy industry, milk product–borne illnesses, including typhoid fever, scarlet fever, tuberculosis, and septic sore throat, were widespread in the United States (Bryan, 1983). The interstate commerce of unpasteurized fluid milk, also known as raw milk, is illegal in the United States, and intrastate sales are regulated independently by each state (Food and Drug Administration, 2011). However, the Code of Federal Regulations provides identity and aging standards that allow the interstate sale of certain types of cheeses made from unpasteurized milk if specific requirements are met. For example, hard cheeses (e.g., cheddar), semisoft cheeses (e.g., Gouda), and soft ripened cheeses (e.g., Camembert), can be made with unpasteurized milk if they are aged (cured) at a temperature of not less than 35°F for not less than 60 days (Food and Drug Administration, 2012). There are no aging standards for soft uncured (or fresh) cheeses for interstate commerce; these cheeses must be made from pasteurized milk. However, soft uncured cheeses made from unpasteurized milk can be manufactured and sold within states that permit sales of unpasteurized dairy products, although standards and regulations vary by state.
Factors influencing pathogen survival and growth in cheese include acidity, preservatives, temperature, competing flora, water activity, and salt concentration (Food and Drug Administration, 2013). Pasteurization should effectively eliminate pathogenic microorganisms from milk used to make cheese. In addition, cheese can become contaminated with pathogens by contamination during cheese-making, through contact with contaminated equipment or other foods, or via handling by infected food workers.
We reviewed foodborne disease outbreaks attributed to cheese reported to the Centers for Disease Control and Prevention (CDC) during 1998–2011. Our objective was to describe characteristics of these outbreaks, including differences between outbreaks linked to cheese made from pasteurized or unpasteurized milk.
Methods
A foodborne disease outbreak is defined as the occurrence of two or more cases of a similar illness resulting from ingestion of a common food (Gould et al., 2013). CDC conducts surveillance for foodborne disease outbreaks investigated and reported by local, state, and territorial health departments in the United States through the Foodborne Disease Outbreak Surveillance System (http://www.cdc.gov/foodsafety/fdoss/). The information collected for each outbreak includes year, month, state, number of illnesses, hospitalizations and deaths, etiology, implicated food, settings where food was prepared, and contributing factors (Bryan et al., 1997). For outbreaks attributed to dairy products, information is collected on whether the product was made from pasteurized or unpasteurized milk.
We reviewed reports of foodborne disease outbreaks during 1998–2011 where cheese was the implicated food or where a food containing cheese was implicated and the cheese was known to be the contaminated ingredient (e.g., blue cheese dressing). Outbreaks where both milk and cheese were reported as vehicles were included in the analysis; outbreaks exclusively associated with milk and those associated with other dairy products were excluded. We analyzed characteristics of outbreaks attributed to cheese overall and by pasteurization status of the milk used to make the cheese. Information on the source of implicated cheeses was not available for all outbreaks; we used information on the setting where the cheese was prepared when the source was unknown. Additional details on outbreaks (e.g., adherence to 60-day aging period) were obtained, when possible, by following up with state health departments reporting outbreaks and by an online search. Data on the legal status of unpasteurized milk sales in each state was obtained from the National Association of State Departments of Agriculture (National Association of State Departments of Agriculture, 2011). Chi-square tests were used for comparisons of categorical variables; the Wilcoxon rank-sum test was used to assess differences in medians. Data were analyzed using Microsoft Excel and SAS version 9.3 (SAS Institute).
Results
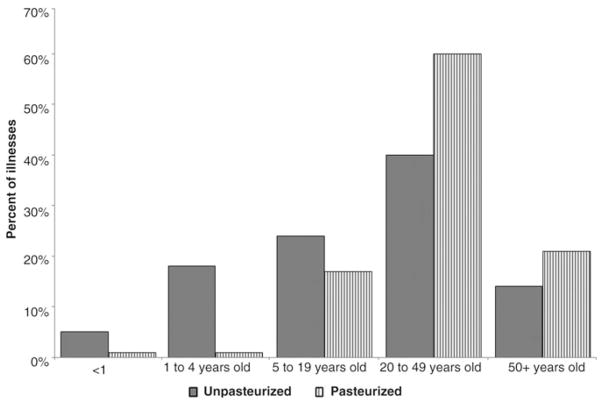
During 1998–2011, 90 outbreaks where cheese was the implicated food were reported to the CDC. These outbreaks resulted in 1882 illnesses, 230 hospitalizations, and 6 deaths. A median of 6.5 outbreaks (range, 3–10) was reported each year, with no discernible pattern in the number of outbreaks overall or by pasteurization status (Fig. 1). The pasteurization status of the milk used to make the cheese was reported for 82 (91%) outbreaks; 38 (46%) were caused by cheese made from unpasteurized milk and 44 (54%) by cheese made from pasteurized milk. Further analyses include only the outbreaks where the pasteurization status of the milk used to make the cheese was known.
FIG. 1.
Number of foodborne disease outbreaks attributed to cheese, by year and pasteurization status, 1998–2011.
Outbreaks due to cheese made from unpasteurized milk had more illnesses than those due to cheese made from pasteurized milk, but this difference was not statistically significant (unpasteurized: median = 12 illnesses, interquartile range [IQR] 7–29; pasteurized: median = 7.5 illnesses, IQR 3–17). Twenty-one percent of outbreak-associated illnesses in outbreaks caused by cheese made from unpasteurized milk resulted in hospitalization versus 6% in outbreaks due to cheese made from pasteurized milk ( p < 0.01) (Table 1).
Table 1.
Characteristics of Foodborne Disease Outbreaks Due to Cheese, by Pasteurization Status, Foodborne Disease Outbreak Surveillance System, 1998–2011a
| Milk used to make cheese
|
||
|---|---|---|
| Unpasteurized | Pasteurized | |
| Outbreaks, no. | 38 | 44 |
| Illnesses, no. | 816 | 987 |
| Hospitalizations, no. | 168 | 61 |
| Deaths, no. | 3 | 3 |
|
| ||
| Etiology | N = 38 n (%) | N = 33 n (%) |
|
| ||
| Salmonellab | 13 (34) | 6 (18) |
| Campylobacter | 10 (26) | 1 (3) |
| Brucella | 5 (13) | 0 (0) |
| Shiga toxin–producing Escherichia colic | 4 (11) | 1 (3) |
| Listeria monocytogenes | 4 (11) | 8 (24) |
| Shigella | 2 (5) | 1 (3) |
| Bacillus cereus | 0 (0) | 1 (3) |
| Norovirus | 0 (0) | 13 (39) |
| Other virus | 0 (0) | 1 (3) |
| Staphylococcus aureus | 0 (0) | 1 (3) |
|
| ||
| Cheese source or setting of preparation | N = 34 n (%) | N = 44 n (%) |
|
| ||
| Imported from Mexico | 13 (38) | 0 (0) |
| Private home | 7 (21) | 4 (14) |
| Dairy or farm | 7 (21) | 3 (7) |
| Restaurant, deli, or banquet | 1 (3) | 28 (64) |
| Commercial product without further preparation | 1 (3) | 7 (16) |
| Otherd | 5 (15) | 2 (5) |
An additional 8 outbreaks with 79 illnesses, 1 hospitalization, and no deaths in which the pasteurization status was unknown were reported.
Salmonella serotypes in outbreaks due to cheese made from unpasteurized milk were Typhimurium (6 outbreaks), Newport (2 outbreaks), Bovismorbificans (1 outbreak), Meleagridis and Newport (1 outbreak), serotyping only identified Group B (1 outbreak), not reported (2 outbreaks). Salmonella serotypes in outbreaks due to cheese made from pasteurized milk were Montevideo (2 outbreaks), Java, Newport, Typhimurium (1 outbreak each), not reported (1 outbreak).
All 4 outbreaks due to cheese made from unpasteurized milk were caused by E. coli O157:H7. Three non-O157 Shiga toxin–producing E. coli serogroups were isolated in the outbreak due to cheese made from pasteurized milk.
Other settings for outbreaks with cheese made from unpasteurized milk were street vendor (2 outbreaks), grocery store (2 outbreaks), and fair or festival (1 outbreak). For pasteurized cheeses: grocery store (1 outbreak) and school (1 outbreak).
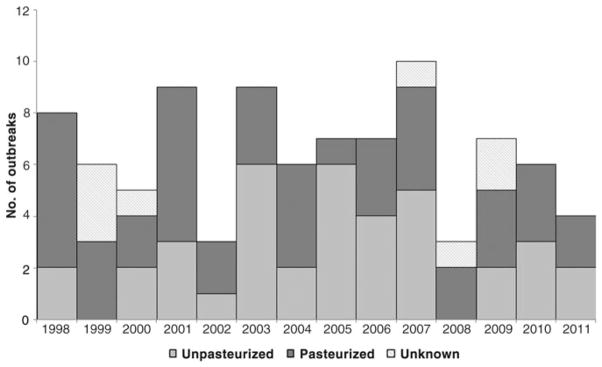
In outbreaks due to cheese made from unpasteurized milk, 56% of illnesses were among females, compared with 47% in outbreaks due to pasteurized cheese (p < 0.01). In outbreaks due to cheese made from unpasteurized milk, more illnesses were among children and adolescents than in outbreaks due to cheese made from pasteurized milk (Fig. 2, p < 0.0001). In outbreaks caused by cheese made from pasteurized milk, more illnesses were among persons aged 20–49 years old and those ≥ 50 years old than in outbreaks from cheese made from unpasteurized milk ( p < 0.001 and p = 0.001, respectively).
FIG. 2.
Age distribution of illnesses in outbreaks attributed to cheese, by pasteurization status, 1998–2011. Information was available for 34 outbreaks and 631 illnesses in outbreaks caused by unpasteurized milk and 35 outbreaks and 565 illnesses in outbreaks caused by pasteurized milk.
Outbreaks due to cheese made from unpasteurized milk were most often caused by Salmonella (34%), Campylobacter (26%), Brucella (13%), and Shiga toxin–producing Escherichia coli (11%). In contrast, outbreaks due to cheeses made from pasteurized milk were most often caused by norovirus (39%) and Listeria (24%) (Table 1). The three deaths in outbreaks due to cheeses made from unpasteurized milk were caused by Listeria (two deaths) and Salmonella serotype Typhimurium; the three deaths in outbreaks due to cheeses made from pasteurized milk were caused by Listeria.
The type of cheese was reported for 36 outbreaks caused by cheese made from unpasteurized milk and 36 caused by cheese made from pasteurized milk. Queso fresco was the most common type of cheese reported (26% of all outbreaks), including 18 outbreaks due to unpasteurized and 1 due to pasteurized cheese (Table 2). An additional seven outbreaks (two unpasteurized, five pasteurized) reported an unspecified type of soft Mexican-style cheese. “Homemade” cheese was the second most common type reported among outbreaks due to cheese made from unpasteurized milks (seven outbreaks, 19%). Three outbreaks (one caused by Gouda, one caused by blue, and one caused by multiple types of soft, aged cheeses) involved cheese made from unpasteurized milk and aged > 60 days; two of these outbreaks were caused by E. coli O157:H7 and one by Listeria. Recalls of the implicated cheese were reported for 11 outbreaks (7 outbreaks due to cheeses made from pasteurized milk, and 4 due to cheeses made from unpasteurized milk).
Table 2.
Types of Cheese Implicated in Foodborne Disease Outbreaks Due to Cheese, by Cheese Category and Pasteurization Status, 1998–2011
| Cheese category and type | Milk used to make cheese
|
|
|---|---|---|
| Unpasteurized N = 36 n (%) | Pasteurized N = 36 n (%) | |
| Soft or semisoft, unripened (fresh) | ||
| Queso fresco | 18 (50) | 1 (3) |
| Other Mexican-style cheesea | 2 (6) | 5 (14) |
| Goat, chevre | 1 (3) | 0 (0) |
| Italian-style (mozzarella, ricotta, and basket) | 1 (3) | 0 (0) |
| Mozzarella | 0 (0) | 4 (11) |
| Cottage | 0 (0) | 1 (3) |
| Cream | 0 (0) | 1 (3) |
| Chive and ackwai | 0 (0) | 1 (3) |
| Soft or semisoft, mold ripened | ||
| Blue | 1 (3)b | 0 (0) |
| Soft or semisoft, aged | ||
| Soft, multiple types | 1 (3)b | |
| Hard or semihard, ripened | ||
| Cheddar | 1 (3) | 3 (8) |
| Gouda | 1 (3)b | 0 (0) |
| Swiss | 0 (0) | 3 (8) |
| Processed | ||
| American | 0 (0) | 1 (3) |
| Other or unspecified | ||
| “Homemade” | 7 (19) | 0 (0) |
| Curds | 2 (6) | 1 (3) |
| Goat, unspecified type | 1 (3) | 0 (0) |
| Sheep’s milk | 0 (0) | 1 (3) |
| Multiple or cheese tray | 0 (0) | 6 (17) |
| Dip, sauce, or fondue | 0 (0) | 3 (8) |
| Other | 0 (0) | 5 (14)c |
Specific type of Mexican-style cheese was not specified.
Made from unpasteurized milk and aged > 60 days.
Includes 2 outbreaks with a shredded cheese and 1 outbreak associated with each of the following preparation methods: ball, spread, sticks.
Three of the outbreaks due to unpasteurized and all six of the outbreaks due to pasteurized queso fresco or other Mexican-style cheese were caused by Listeria. Other cheese–pathogen pairs causing at least 3 outbreaks were unpasteurized queso fresco or other Mexican-style cheese and Salmonella (10 outbreaks), unpasteurized “homemade” cheese and Campylobacter (4 outbreaks), and unpasteurized queso fresco or other Mexican-style cheese and Brucella (3 outbreaks). Four of the outbreaks of norovirus infections were attributed to cheese trays or other arrangements with multiple cheeses.
Many of the cheeses made from unpasteurized milk were soft unaged cheeses imported from Mexico (13 outbreaks, 38%). Other common places of cheese preparation in outbreaks due to cheese made from unpasteurized milk were private homes (seven outbreaks, 21%), and dairies or farms (seven outbreaks, 21%) (Table 1). The most common setting for outbreaks due to pasteurized cheese was a restaurant, deli, or banquet facility (28 outbreaks, 64%). In five outbreaks, all due to cheese made from unpasteurized milk, the outbreak report noted that the cheese was produced or sold illegally. In two of these outbreaks, the cheese was sold by a street vendor; in one, the cheese was imported into the United States illegally and sold; in one, homemade cheese was made from illegally obtained unpasteurized milk; and in one, the cheese was produced and sold on an unlicensed dairy farm.
Among the 33 outbreaks due to cheese made from unpasteurized milk where cases were reported from a single state, most (91%) occurred in states where the intrastate sale of unpasteurized dairy products was legal. Three outbreaks occurred in states (Michigan, North Carolina, and Virginia) where the intrastate sale of unpasteurized dairy products was illegal. Nine outbreaks (five caused by cheese made from pasteurized milk and four caused by cheese made from unpasteurized milk) had cases reported from multiple states. The products implicated in multistate outbreaks caused by cheeses made from pasteurized milk were Mexican-style cheese (four outbreaks) and shredded pasteurized cheese. The products implicated in multistate outbreaks caused by cheeses made from unpasteurized milk were a homemade cheese, Italian-style soft cheeses (mozzarella, ricotta, “basket” cheese) (McCarthy et al., 2002), Gouda cheese, blue cheese, and several types of cow, goat, and sheep’s milk soft cheeses produced at the same facility.
The most common contributing factor in outbreaks caused by cheese made from unpasteurized milk was contamination of raw product or ingredient by pathogens from animals or the environment (62%, Table 3); this factor was rarely reported for outbreaks caused by cheese made from pasteurized milk. The common contributing factors in outbreaks caused by cheese made from pasteurized milk were related to worker health and hygiene, including bare-handed contact by food workers (35%) or handling by an infected person or carrier of a pathogen (31%); these factors were not reported for any of the outbreaks caused by cheese made from unpasteurized milk.
Table 3.
Contributing Factors Reported in Foodborne Disease Outbreaks Associated With Cheese, by Pasteurization Status, 1998–2011
| Contributing factor description | Milk used to make cheese
|
|
|---|---|---|
| Unpasteurized (n = 26) n (%)a | Pasteurized (n = 26) n (%)a | |
| Raw product/ingredient contaminated by pathogens from animal or environment | 16 (62) | 2 (8) |
| Ingestion of contaminated raw products | 11 (42) | 1 (4) |
| Insufficient time and/or temperature during cooking/heat processing or reheating | 10 (38) | 1 (4) |
| Inadequate processing (acidification, water activity, fermentation) | 2 (8) | 0 (0) |
| Allowing foods to remain at room or warm outdoor temperature for several hours, preparing foods a half day or more before serving | 2 (8) | 1 (4) |
| Cross-contamination from raw ingredient of animal origin | 1 (4) | 4 (15) |
| Inadequate cleaning of processing/preparation equipment/utensil | 1 (4) | 5 (19) |
| Improper cooling or cold-holding | 1 (4) | 5 (19) |
| Bare-handed contact by handler/worker/preparer | 0 (0) | 9 (35) |
| Handling by an infected person or carrier of pathogen | 0 (0) | 8 (31) |
| Storage in contaminated environment | 0 (0) | 6 (23) |
| Glove-handed contact by handler/worker/preparer | 0 (0) | 5 (19) |
More than one contributing factor could be selected for each outbreak, so numbers may total more than 100%.
Discussion
Outbreaks caused by cheese made from unpasteurized milk resulted in more hospitalizations than outbreaks caused by cheese made from pasteurized milk, and often involved cheeses imported into the United States from Mexico or made in a private home. Nearly half of the illnesses in outbreaks caused by cheese made from unpasteurized milk were in children. Americans eat an estimated 10 billion pounds of cheese (33.2 pounds per capita) each year (United States Department of Agriculture, 2012). The proportion of this that is made from unpasteurized milk is unknown, but is estimated to be < 1%, emphasizing that the risk of illnesses may be orders of magnitude higher for unpasteurized than pasteurized dairy products (Langer et al., 2012).
Nearly 40% of the outbreaks caused by cheese made from unpasteurized milk were linked with soft cheeses imported from Mexico. Although outbreak reports only noted that the implicated cheeses were illegal in a few of the outbreaks, it is possible that more of these cheeses were not for legal sale in the United States. Commercial importation of cheese made from unpasteurized milk from Mexico is illegal unless the cheese has met specific aging standards (Food and Drug Administration, 2012; USDA APHIS, 2012). Travelers can bring in limited amounts of cheese made from unpasteurized milk for personal use (Kinde et al., 2007; U.S. Customs and Border Protection, 2012); however, cheese made from unpasteurized milk is often imported for “personal use,” often on a large scale, and subsequently illegally sold in the United States. This practice has repeatedly resulted in outbreaks associated with queso fresco and other Mexican-style cheeses made from unpasteurized milk (Linnan et al., 1988; Altekruse et al., 1998; Cody et al., 1999; Villar et al., 1999; MacDonald et al., 2005; Centers for Disease Control and Prevention, 2008). One study found that 46% of cheese samples imported from Mexico were contaminated with Salmonella, E. coli O157:H7, or Listeria, in addition to frequent contamination by debris and insects (Torres-Vitela et al., 2012). Surveys of imported cheeses have found higher levels of pathogens in cheeses imported from Mexico and Central America than other regions (D’Amico and Donnelly, 2011). Outbreaks caused by homemade cheeses made with unpasteurized milk were also common. Because food safety regulations are difficult or impossible to enforce in private homes, additional consumer education is needed about proper sanitary procedures for cheese-making.
More recently, some soft cheeses made from pasteurized milk, particularly Mexican-style cheeses such as queso fresco, have also been implicated in outbreaks of Listeria infections in the United States (Linnan et al., 1988; Jackson et al., 2011), Canada (Gaulin et al., 2012), and Europe (Fretz et al., 2010; Koch et al., 2010). Because Listeria is common in the processing environment, cheese made with pasteurized milk can become contaminated during cheese-making and aging (D’Amico et al., 2008; Centers for Disease Control and Prevention, 2013). Soft cheeses can support the growth of Listeria introduced after processing, regardless of whether the milk used for the cheese was pasteurized or not (D’Amico et al., 2008). Because Listeria can grow and survive at refrigerated temperatures, even in cheeses aged more than 60 days (D’Amico et al., 2008), strict adherence to controls to avoid postpasteurization contamination with Listeria is required.
Three of the outbreaks included in this series—two caused by E. coli O157:H7 and one caused by Listeria—involved cheeses made from unpasteurized milk that had been aged for longer than 60 days, providing additional evidence that this aging requirement is insufficient to render cheese pathogen free. In one outbreak, facility records indicated that at least some of the lots of implicated cheese had been packaged and released for sale before completion of the 60-day aging period (McCollum et al., 2012). Several studies have found that pathogens can survive in cheese for longer than 60 days, both experimentally (Campbell and Gibbard, 1944; Schlesser et al., 2006; D’Amico et al., 2010) and in outbreak settings (Wade and Shere, 1928; Tucker et al., 1946; Honish et al., 2005). Viable E. coli O157, Mycobacterium bovis, and Salmonella have been found in laboratory-produced and inoculated cheeses made from unpasteurized milk as long as a year after production (Mitscherlich and Marth, 1984; Reitsma and Henning, 1996; D’Amico et al., 2010).
Factors contributing to cheese-associated outbreaks differed depending on whether the milk used to make the cheese was pasteurized or not. Not surprisingly, because unpasteurized milk used to make cheese originates in the dairy farm environment, contamination at the point of processing, typically due to contamination by pathogens from animals or the environment, was the most common contributing factor in outbreaks caused by cheese made from unpasteurized milk. Contamination at the point of processing was uncommon in outbreaks due to pasteurized cheeses: in one, an outbreak of Campylobacter infections was linked to cheese curds labeled as pasteurized produced by a local dairy that had repeated production issues resulting in inadequate pasteurization; hence, this product cannot be considered pasteurized. In two outbreaks, the cheese was contaminated with Listeria. The most common factor contributing to outbreaks caused by pasteurized cheese was deficiencies in worker health and hygiene, consistent with the large number of outbreaks caused by norovirus and the finding that norovirus outbreaks often involved cheese trays or other arrangements involving multiple types of cheese commonly found in restaurants (Langer et al., 2012).
There are several limitations to foodborne disease outbreak surveillance data (Gould et al., 2013). First, foodborne disease outbreak reporting is voluntary and not all foodborne disease outbreaks are reported to the CDC. Even when outbreaks are reported, states are allowed to edit reports if new data become available. Information on whether cheese implicated in an outbreak had been aged for > 60 days was not available for all outbreaks because health departments were sometimes unable to obtain it and because this information is not explicitly collected by the outbreak report form. Similarly, information on whether a cheese was produced and sold legally or not is also not explicitly collected; it is possible that more outbreaks, particularly those due to cheeses made from unpasteurized milk, were caused by illegally produced cheeses. The outbreak report form also does not collect information to categorize the point of contamination for all outbreaks (e.g., during processing, at retail). Not all variables were reported for each outbreak; we contacted state health departments reporting outbreaks to complete any missing data. Contributing factor data help to provide insights into factors influencing foodborne disease outbreaks (Bryan et al., 1997); however, the definitions of these factors are subject to interpretation. For some outbreaks, it is possible that the contributing factors reported represented general deficiencies noted during an outbreak investigation rather than specific factors contributing to the outbreak.
Nearly all of the outbreaks due to cheeses made from unpasteurized milk occurred in states where intrastate sales of unpasteurized milk were legal. Regulations limiting the sale of unpasteurized dairy products have a marked impact on the incidence of outbreaks. A previous study found that states where intrastate sales of unpasteurized dairy products was legal had nearly six times the rate of outbreaks caused by cheese made from unpasteurized milk than states where sales were illegal (Langer et al., 2012). Currently, 30 states allow some sort of legal sale of unpasteurized milk (National Association of State Departments of Agriculture, 2011). Even in states where sales of unpasteurized dairy products are illegal, loopholes like cow-share programs provide means for consumers to acquire unpasteurized milk. Legalization of the sale of unpasteurized milk in additional states might result in an increasing number of outbreaks and illnesses.
Understanding the sources and routes of contamination can help to improve the safety of cheese. In addition to using pasteurized milk, soft-cheese-making facilities need to ensure strict sanitation and microbiologic monitoring. Labeling of cheese should include whether the milk used to make it was pasteurized or unpasteurized, whether the cheese was aged and for how long, and the license number of the production facility. Efforts to reduce production and sale of illegally manufactured cheeses as well as continued binational collaborations are needed to address the issue of illegal cheese importation. Restaurant owners and public health practitioners should continue to educate foodworkers on the importance of not preparing food while ill.
These findings reemphasize the risks of consuming unpasteurized dairy products. Additionally, persons at higher risk for listeriosis, including older adults, pregnant women, and persons with immunocompromising conditions, should be aware that certain soft cheeses made with unpasteurized milk, or made under unsanitary conditions (whether or not the milk was pasteurized), have been shown to cause severe illness. These soft cheeses include fresh (unripened) cheeses, such as queso fresco (Centers for Disease Control and Prevention, 2013), and soft-ripened cheeses. Some public health agencies, including the European Centre for Disease Control and Prevention (http://www.ecdc.europa.eu/en/healthtopics/listeriosis/factsheet-general-public/Pages/factsheet-general-public.aspx) and the Public Health Agency of Canada (http://www.phac-aspc.gc.ca/fs-sa/fs-fi/listerios-eng.php), recommend that persons in high-risk groups avoid all soft cheeses to reduce the risk of listeriosis. Information about unpasteurized dairy products and prevention resources for higher-risk groups can be found online (http://www.cdc.gov/foodsafety/rawmilk/raw-milk-index.html).
Acknowledgments
Funding for this report was provided by the Centers for Disease Control and Prevention. The funding agencies did not have a role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Disclosure Statement
No competing financial interests exist.
The findings and conclusions in this report are those of the authors and do not necessarily represent those of the Centers for Disease Control and Prevention.
References
- Altekruse SF, Timbo BB, Mowbray JC, Bean NH, Potter ME. Cheese-associated outbreaks of human illness in the United States, 1973 to 1992: Sanitary manufacturing practices protect consumers. J Food Prot. 1998;61:1405–1407. doi: 10.4315/0362-028x-61.10.1405. [DOI] [PubMed] [Google Scholar]
- Bryan FL. Epidemiology of milk-borne diseases. J Food Prot. 1983;46:637–649. doi: 10.4315/0362-028X-46.7.637. [DOI] [PubMed] [Google Scholar]
- Bryan FL, Guzewich JJ, Todd ECD. Surveillance of foodborne disease. III. Summary and presentation of data on vehicles and contributory factors: Their value and limitations. J Food Prot. 1997;60:701–714. doi: 10.4315/0362-028X-60.6.701. [DOI] [PubMed] [Google Scholar]
- Campbell A, Gibbard J. The survival of E. Typhosa in cheddar cheese manufactured from infected raw milk. J Pub Health. 1944;35:158–164. [Google Scholar]
- Centers for Disease Control and Prevention. Outbreak of multi-drug-resistant Salmonella enterica serotype Newport infections associated with consumption of unpasteurized Mexican-style aged cheese—Illinois, March 2006-April 2007. MMWR. 2008;57:432–435. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Vital signs: Listeria illnesses, deaths, and outbreaks—United States, 2009–2011. MMWR. 2013;62:448–452. [PMC free article] [PubMed] [Google Scholar]
- Cody SH, Abbott SL, Marfin AA, et al. Two outbreaks of multidrug-resistant Salmonella serotype Typhimurium DT104 infections linked to raw-milk cheese in Northern California. JAMA. 1999;281:1805–1810. doi: 10.1001/jama.281.19.1805. [DOI] [PubMed] [Google Scholar]
- D’Amico DJ, Donnelly CW. FDA’s domestic and imported cheese compliance program results: January 1, 2004–December 31, 2006. Food Protection Trends. 2011;31:216–226. [Google Scholar]
- D’Amico DJ, Druart MJ, Donnelly CW. 60-day aging requirement does not ensure safety of surface-mold-ripened soft cheeses manufactured from raw or pasteurized milk when Listeria monocytogenes is introduced as a postprocessing contaminant. J Food Prot. 2008;71:1563–1571. doi: 10.4315/0362-028x-71.8.1563. [DOI] [PubMed] [Google Scholar]
- D’Amico DJ, Druart MJ, Donnelly CW. Behavior of Escherichia coli O157:H7 during the manufacture and aging of Gouda and stirred-curd cheddar cheeses manufactured from raw milk. J Food Prot. 2010;73:2217–2224. doi: 10.4315/0362-028x-73.12.2217. [DOI] [PubMed] [Google Scholar]
- Food and Drug Administration. Code of Federal Regulations, Title 21, Part 133, Cheeses and Related Cheese Products. Volume 2012.
- Food and Drug Administration. Grade “A” Pasteurized Milk Ordinance. 2011 [Google Scholar]
- Food and Drug Administration. Evaluation and Definition of Potentially Hazardous Foods—Chapter 3. Factors that Influence Microbial Growth. 2013 [Google Scholar]
- Fretz R, Sagel U, Ruppitsch W, et al. Listeriosis outbreak caused by acid curd cheese Quargel, Austria and Germany 2009. Euro Surveill. 2010;15 pii:19477. [PubMed] [Google Scholar]
- Gaulin C, Ramsay D, Bekal S. Widespread listeriosis outbreak attributable to pasteurized cheese, which led to extensive cross-contamination affecting cheese retailers, Quebec, Canada, 2008. J Food Prot. 2012;75:71–78. doi: 10.4315/0362-028X.JFP-11-236. [DOI] [PubMed] [Google Scholar]
- Gould LH, Walsh KA, Vieira AR, et al. Surveillance for foodborne disease outbreaks—United States, 1998–2008. MMWR Surveill Summaries. 2013;62(Suppl 2):1–34. [PubMed] [Google Scholar]
- Honish L, Predy G, Hislop N, et al. An outbreak of E. coli O157:H7 hemorrhagic colitis associated with unpasteurized gouda cheese. Can J Public Health. 2005;96:182–184. doi: 10.1007/BF03403686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KA, Biggerstaff M, Tobin-D’Angelo M, et al. Multi-state outbreak of Listeria monocytogenes associated with Mexican-style cheese made from pasteurized milk among pregnant, Hispanic women. J Food Prot. 2011;74:949–953. doi: 10.4315/0362-028X.JFP-10-536. [DOI] [PubMed] [Google Scholar]
- Kinde H, Mikolon A, Rodriguez-Lainz A, et al. Recovery of Salmonella, Listeria monocytogenes, and Mycobacterium bovis from cheese entering the United States through a noncommercial land port of entry. J Food Prot. 2007;70:47–52. doi: 10.4315/0362-028x-70.1.47. [DOI] [PubMed] [Google Scholar]
- Koch J, Dworak R, Prager R, et al. Large listeriosis outbreak linked to cheese made from pasteurized milk, Germany, 2006–2007. Foodborne Pathog Dis. 2010;7:1581–1584. doi: 10.1089/fpd.2010.0631. [DOI] [PubMed] [Google Scholar]
- Langer AJ, Ayers T, Grass J, Lynch M, Angulo FJ, Mahon BE. Nonpasteurized dairy products, disease outbreaks, and state laws-United States, 1993–2006. Emerg Infect Dis. 2012;18:385–391. doi: 10.3201/eid1803.111370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linnan MJ, Mascola L, Lou XD, et al. Epidemic listeriosis associated with Mexican-style cheese. N Engl J Med. 1988;319:823–828. doi: 10.1056/NEJM198809293191303. [DOI] [PubMed] [Google Scholar]
- MacDonald PD, Whitwam RE, Boggs JD, et al. Outbreak of listeriosis among Mexican immigrants as a result of consumption of illicitly produced Mexican-style cheese. Clin Infect Dis. 2005;40:677–682. doi: 10.1086/427803. [DOI] [PubMed] [Google Scholar]
- McCarthy T, Phan Q, Mshar P, Mshar R, Howard R, Hadler JL. Outbreak of multidrug-resistant Salmonella Newport associated with consumption of Italian-style soft cheese, Connecticut. International Conference on Emerging Infectious Diseases; Atlanta, GA. 2002. [Google Scholar]
- McCollum J, Williams N, Beam S, et al. Multistate outbreak of Escherichia coli O157:H7 infections associated with in-store sampling of an aged raw-milk Gouda cheese, 2010. J Food Prot. 2012;75:1759–1765. doi: 10.4315/0362-028X.JFP-12-136. [DOI] [PubMed] [Google Scholar]
- Mitscherlich E, Marth EH. Microbial Survival in the Environment: Bacteria and Rickettsiae Important in Human and Animal Health. Berlin, New York: Springer-Verlag; 1984. [Google Scholar]
- National Association of State Departments of Agriculture. [accessed October 16, 2012];Raw Milk Survey. Available at: www.nasda.org/file.aspx?id=3916.
- Reitsma CJ, Henning DR. Survival of enterohemorrhagic Escherichia coli O157:H7 during the manufacture and curing of cheddar cheese. J Food Prot. 1996;59:460–464. doi: 10.4315/0362-028X-59.5.460. [DOI] [PubMed] [Google Scholar]
- Schlesser JE, Gerdes R, Ravishankar S, Madsen K, Mowbray J, Teo AY. Survival of a five-strain cocktail of Escherichia coli O157:H7 during the 60-day aging period of cheddar cheese made from unpasteurized milk. J Food Prot. 2006;69:990–998. doi: 10.4315/0362-028x-69.5.990. [DOI] [PubMed] [Google Scholar]
- Torres-Vitela MR, Mendoza-Bernardo M, Castro-Rosas J, et al. Incidence of Salmonella, Listeria monocytogenes, Escherichia coli O157:H7, and staphylococcal enterotoxin in two types of Mexican fresh cheeses. J Food Prot. 2012;75:79–84. doi: 10.4315/0362-028X.JFP-11-258. [DOI] [PubMed] [Google Scholar]
- Tucker GB, Cameron GM, et al. Typhimurium food infection from Colby cheeseSalmonella. JAMA. 1946;131:1119. doi: 10.1001/jama.1946.02870310015005. [DOI] [PubMed] [Google Scholar]
- U.S. Customs and Border Protection. [accessed October 16, 2012];Travelers bringing food into the U.S. for personal use. 2012 Available at: https://help.cbp.gov/app/answers/detail/a_id/82/~/travelers-bringing-food-into-the-u.s.-for-personal-use.
- United States Department of Agriculture. Food Availability, Dairy Products. 2012 [Google Scholar]
- USDA APHIS. Importing into the United States. Milk and Milk Products. 2012;2012 [Google Scholar]
- Villar RG, Macek MD, Simons S, et al. Investigation of multidrug-resistant Salmonella serotype Typhimurium DT104 infections linked to raw-milk cheese in Washington State. JAMA. 1999;281:1811–1816. doi: 10.1001/jama.281.19.1811. [DOI] [PubMed] [Google Scholar]
- Wade EM, Shere L. Longevity of typhoid bacilli in cheddar cheese: A study following an outbreak of typhoid fever traced to cheese. Am J Public Health Nation’s Health. 1928;18:1480–1488. doi: 10.2105/ajph.18.12.1480. [DOI] [PMC free article] [PubMed] [Google Scholar]