Abstract
Objective
New clinical guidelines endorse the use of low-dose computed tomography (LDCT) for lung cancer screening among selected heavy smokers while recommending patients be counseled about the potential benefits and harms. We developed and field tested a brief, video-based patient decision aid about lung cancer screening.
Methods
Smokers in a cancer center tobacco treatment program aged 45 to 75 years viewed the video online between November 2011 and September 2012. Acceptability, knowledge, and clarity of values related to the decision were assessed.
Results
Fifty-two patients completed the study (mean age=58.5 years; mean duration smoking=34.8 years). Acceptability of the aid was high. Most patients (78.8%) indicated greater interest in screening after viewing the aid. Knowledge about lung cancer screening increased significantly as a result of viewing the aid (25.5% of questions answered correctly before the aid, and 74.8% after; P<.01) although understanding of screening eligibility remained poor. Patients reported being clear about which benefits and harms of screening mattered most to them (94.1% and 86.5%, respectively).
Conclusions
Patients have high information needs related to lung cancer screening. A video-based decision aid may be helpful in promoting informed decision-making, but its impact on lung cancer screening decisions needs to be explored.
Keywords: Decision Making, Lung Neoplasms, Early Detection of Cancer, Oncology, Cancer
INTRODUCTION
Lung cancer is the second most common cancer and the leading cause of cancer deaths in the US and worldwide [1–2]. Because of its strong link to tobacco use, lung cancer is the most preventable form of cancer death.
In June 2011, the National Lung Screening Trial (NLST) published its primary result: among persons 55-to-74 years of age who previously or currently smoke heavily, 20% fewer lung cancer deaths were observed among those who received low-dose computed tomography (LDCT) rather than standard chest x-rays for screening [3]. These findings have led many professional medical societies to endorse annual LDCT screening for lung cancer for individuals meeting NLST eligibility [4–6]. Yet, lung cancer screening with LDCT is associated with potential harms, including radiation exposure and a high false-positive rate leading to subsequent follow-up and invasive testing with its own associated harms [7]. In addition to the physical harms associated with LDCT screening, there is the risk of overtreatment for possibly nonfatal cancers, psychological harms (anxiety, depression), and real or perceived financial strain [8]. Because of these potential harms, many organizations highlight the need for informed decision making. For example, The American Cancer Society’s (ACS) evidence-based guideline and US Preventive Services Task Force recommendation emphasize the importance of patients having the opportunity to weigh the harms and benefits when making a decision about screening for lung cancer with their healthcare provider [5–6].
Patient decision aids can play an important role in promoting shared decisions about lung cancer screening. These interventions are designed to help people think about the choices they face by describing where and why a choice exists. Decision aids provide information about options, help people deliberate by considering relevant attributes of the options, support people in forecasting how they might feel about outcomes associated with the outcomes, and support their constructing preferences for the options [9]. Compared with usual care interventions, patient decision aids significantly improve knowledge, result in more accurate risk perceptions, help patients become more assured about their decisions, decrease passive participation in decision making, and result in decisions consistent with patients’ values [7].
In response to new evidence and potential misconceptions about the benefits and harms of LDCT screening for lung cancer, we developed a video-based patient decision aid to promote informed screening decisions. Here we report on field testing of the decision aid among current and former smokers
METHODS
Development of the Patient Decision Aid
The video “Lung Cancer Screening: Is It Right for Me?” was designed to be used in primary care settings by candidates for lung cancer screening (the final video was approximately 6 minutes long), but the format allows the aid to be used in other settings as well. A video-format was selected to maximize its potential use with patients having low health literacy. The content was written at the 8th-grade reading level. The aid was tested for comprehension with patients and modified during development. Features of the aid include an on-screen narrator, information about lung cancer and its risk factors, footage of a patient undergoing a scan, animations communicating the magnitude of harms and benefits of LDCT screening, and an implicit values clarification component that depicts trade-offs between potential harms and benefits. A unique feature of the aid is the use of animated pictographs to depict the likelihood of benefit from LDCT screening and the false-positive rate associated with testing (Figure 1).
Figure 1. Screen shots from the patient decision aid video.
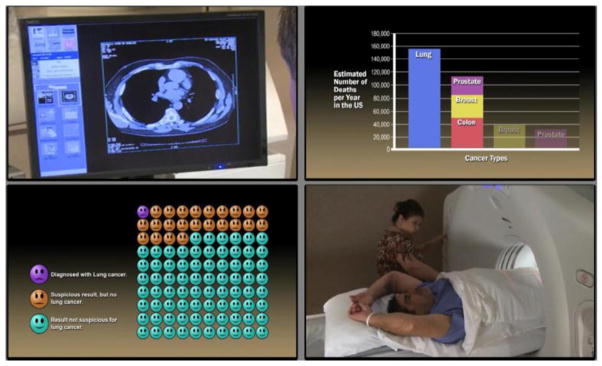
Clockwise from top left: LDCT image on a monitor; deaths due to lung cancer compared to other cancers; icon array showing likelihood of a positive LDCT result; and an LDCT scan procedure. Subjects were cancer center patients in a tobacco treatment program who participated in the study between November 2011 and September 2012.
Subjects and Procedures
An uncontrolled, before-after design was used to evaluate the decision aid. These designs are typically used as part of a systematic development process for patient decision aids, where the aid is field tested with patients to determine acceptability of the tool and gain initial indicators of the tool’s effectiveness in promoting informed decisions [10]. Eligible subjects were patients from a tobacco treatment program at a large cancer center who were English speakers and had no history of lung cancer. Current and former patients were mailed invitation letters (n=500) and recruitment fliers were included in new patient packets (n=60). Interested patients were given a link to an online survey where they completed a pre-intervention assessment, viewed the decision aid video, and completed a post-intervention assessment. The project was approved by the Institutional Review Board at The University of Texas MD Anderson Cancer Center.
Measures and Analysis
The usability of the patient decision aid was tested using the Ottawa Acceptability Measures,[11] general ratings of the quality of the aid, and the perceived impact of the aid on screening decisions. The effectiveness of the decision aid in promoting informed screening decisions was assessed using two of the decision aid evaluation criteria defined by the International Patient Decision Aid Collaboration: being informed and feeling clear about values [12]. We used an 11-item measure of lung cancer screening knowledge and the values clarity subscale of the Decisional Conflict Scale [13]. We also included 3 knowledge items specific to risks and benefits presented in the aid for a subset of the sample. The Decisional Conflict Scale values clarity subscale questions were compared with standards for the scale [13].
At the time of the study, new guidelines had not yet been released and screening with LDCT was not being reimbursed by insurance. Posthoc analyses comparing patients (n=14) who met both age and pack-year history eligibility for LDCT screening and those who did not (n=38) showed all screen-eligible patients rated the length as about right, while 6 (15.8%) of the remaining patients indicated the video should have been longer. No other differences were observed, and the combined data is reported below.
RESULTS
Of the 52 participants in the field testing, 23 (44.2%) were current smokers and the remainder were former smokers. The average smoking history was 30 pack-years, and the average time smoking was 34.8 years. The age range was 45 to 75 years (mean age=58.5 years), and 34 (65.4%) were female. Ten (19.2%) of the participants identified themselves as African American and 3 (6%) as Hispanic; the remainder were Caucasian. Seventeen (32.7%) of the participants had a high school degree or less.
More than 94% of patients viewed the entire video, would recommend it to others, felt it held their interest, and wanted to view similar videos about health care decisions. Ratings of the amount of information in the aid, length, and clarity were highly favorable. Most patients (78.8%) believed that people would be more interested in screening after viewing the decision aid.
The mean percentage of correct responses to the 11-item lung cancer knowledge measure increased significantly for all 11 items from 25.5% (SD=20.7) before the decision aid was viewed to 74.8% (SD=20.2) after the aid was viewed (P<.01 for each item, see Table 1). For the 3-item knowledge subset related to risks and benefits (n=22), the mean percentage of correct responses significantly increased from 18.2% (SD=9.1) to 72.7% (SD=28.4) (P<.01, Table 1). Despite the intervention, three quarters of patients continued to have difficulty correctly answering the question about whether all current and former smokers should be screened for lung cancer (Question 10).
Table 1.
Knowledge Questions Answered Correctly Before and After Viewing of the Patient Lung Cancer Screening Decision Aid (N=52)*
| Question (answer) | Before % |
After % |
|---|---|---|
| 1. Is lung cancer the second leading cause of cancer death in the US? (no) | 11.8 | 53.8 |
| 2. Is smoking responsible for more than half of all lung cancer deaths in US? (yes) | 71.2 | 94.2 |
| 3. Does having a low-dose CT decrease your chances of getting lung cancer? (no) | 25.5 | 82.4 |
| 4. Does having a low-dose CT decrease your chances of dying from lung cancer? (yes) | 21.2 | 74.5 |
| 5. If nothing is found on your CT scan should you repeat the scan in 6 months? (no) | 11.5 | 70.6 |
| 6. Is radiation exposure one of the harms of screening? (yes) | 37.3 | 86.3 |
| 7. Can a low-dose CT show that you have a tumor when you do not? (yes) | 13.5 | 84.6 |
| 8. Can a low-dose CT miss a tumor in your lungs? (yes) | 25.5 | 86.5 |
| 9. Will all tumors found in the lungs grow to be life threatening? (no) | 48.1 | 88.5 |
| 10. Should all current and former smokers be screened for lung cancer? (no) | 3.8 | 23.1 |
| 11. Can a low-dose CT find heart disease? (yes) | 13.5 | 86.3 |
| 12. Does a low-dose CT lower your chances of dying from lung cancer by 40%? (yes)** | 9.1 | 40.9 |
| 13. Will most people with suspicious cancer results actually be diagnosed with lung cancer? (no)** | 27.3 | 95.5 |
| 14. Will about a quarter of people screened with low-dose CT have a result that is suspicious for lung cancer? (yes)** | 18.2 | 81.8 |
The correct response to each question is given in parentheses. All before-and-after comparisons are significant at P<.01 using paired samples t-tests.
Subjects were cancer center patients in a tobacco treatment program who participated in the study between November 2011 and September 2012.
Risk questions administered in a subset of 22 participants.
After viewing the decision aid, most patients reported that they felt clear about which benefits of screening for lung cancer mattered most (94.1%), and about which harms mattered most (86.5%). The mean overall Decisional Conflict Scale values clarity subscale score was 7.84 (SD=23.18), which compares favorably to a threshold score of 25 or below out of 100 for feeling ready to make a decision[13].
DISCUSSION
This field test of a video-based patient decision aid for lung cancer screening with LDCT showed that the aid was well received by current and former smokers. Many of the participants in this study believed that the aid would increase interest in LDCT for lung cancer screening.
General knowledge of lung cancer and LDCT screening was initially poor among this group. The patient decision aid significantly improved the overall rate of correct answers, highlighting the important informational function of the tool. In addition, similar to observations with other decision aids [14], our video helped the study participants better understand their values regarding the potential harms and benefits of LDCT screening for lung cancer. However, the patients continued to have difficulty with the question about whether all smokers should undergo screening, suggesting ongoing confusion about eligibility for LDCT screening.
The study was limited to current and former smokers who were patients in a tobacco treatment program at a large cancer center. We did not track patients’ subsequent use of LDCT for screening, although at the time of this study, patients would have had to pay for the service themselves.
CONCLUSION
Lung cancer screening with LDCT joins a growing list of cancer screening services for which guidelines strongly endorse patients making informed decisions in consultation their health care providers. Patient demand for this service will likely increase as will the need for balanced, high quality information about the harms and benefits of LDCT screening to ensure that patients are making informed decisions. Large, comparative trials are needed to assess the impact of the aid on informed decisions and outcomes long term.
Highlights.
Screening with low-dose CT lowers lung cancer mortality in heavy smokers.
Patients should be counseled about the benefits and harms of screening with CT.
We field tested a video-based decision aid about lung cancer screening.
Large gains in knowledge were observed; interest in screening increased.
Decision aids prepare heavy smokers to make informed screening decisions.
Acknowledgments
We acknowledge the support of Bonnie Nelson for patient recruitment, Elizabeth Hess, ELS(D), MA, for editing the manuscript, and the Tobacco Treatment Program at The University of Texas MD Anderson Cancer Center. Dr. Volk had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
CONFLICT OF INTEREST
The authors declare that there are no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Cancer Society. Cancer facts & figures 2012. Secondary Cancer facts & figures 2012. 2012 http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-031941.pdf.
- 2.Khan N, Afaq F, Mukhtar H. Lifestyle as risk factor for cancer: Evidence from human studies. Cancer Letters. 2010;293(2):133–43. doi: 10.1016/j.canlet.2009.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aberle DR, Adams AM, Berg CD, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. New England Journal of Medicine. 2011;365(5):395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bach PB, Mirkin JN, Oliver TK, et al. Benefits and harms of CT screening for lung cancer: a systematic review. JAMA. 2012;307(22):2418–29. doi: 10.1001/jama.2012.5521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wender R, Fontham ET, Barrera E, Jr, et al. American Cancer Society lung cancer screening guidelines. CA Cancer J Clin. 2013 doi: 10.3322/caac.21172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moyer VA. Screening for Lung Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2013 doi: 10.7326/M13-2771. [DOI] [PubMed] [Google Scholar]
- 7.Stacey D, Bennett CL, Barry MJ, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2011;(10):CD001431. doi: 10.1002/14651858.CD001431.pub3. [DOI] [PubMed] [Google Scholar]
- 8.Harris RP, Sheridan SL, Lewis CL, et al. The Harms of Screening: A Proposed Taxonomy and Application to Lung Cancer Screening. JAMA internal medicine. 2013 doi: 10.1001/jamainternmed.2013.12745. [DOI] [PubMed] [Google Scholar]
- 9.Volk RJ, Llewellyn-Thomas H, Stacey D, Elwyn G. Ten years of the International Patient Decision Aid Standards Collaboration: evolution of the core dimensions for assessing the quality of patient decision aids. BMC Medical Informatics and Decision Making. 2013;12(Suppl 2:S1) doi: 10.1186/1472-6947-13-S2-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coulter A, Stilwell D, Kryworuchko J, Mullen P, Ng C, van der Weijden T. A systematic development process for patient decision aids. BMC Medical Informatics and Decision Making. 2013;12(Suppl 2:S2) doi: 10.1186/1472-6947-13-S2-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Connor A, Cranney A. User Manual - Acceptability. Secondary User Manual - Acceptability 2002. 1996 http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Acceptability.pdf.
- 12.Sepucha KR, Borkhoff CM, Lally J, et al. Establishing the effectiveness of patient decision aids: key constructs and measurement instruments. BMC Medical Informatics and Decision Making. 2013;12(Suppl 2:S12) doi: 10.1186/1472-6947-13-S2-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O’Connor A. Decisional conflict scale user manual. Secondary Decisional conflict scale user manual. 2010 http://decisionaid.ohri.ca/eval_dcs.html.
- 14.Schwartz LM, Woloshin S, Fowler FJ, Jr, Welch HG. Enthusiasm for cancer screening in the United States. JAMA. 2004;291(1):71–8. doi: 10.1001/jama.291.1.71291/1/71. [DOI] [PubMed] [Google Scholar]


