Abstract
Home blood pressure (HBP) monitoring is recommended for assessing the effects of antihypertensive treatment, but it is not clear how the treatment-induced changes in HBP compare with the changes in clinic BP (CBP). We searched PubMed using the terms “home or self-measured blood pressure,” and selected articles in which the changes in CBP and HBP (using the upper arm oscillometric method) induced by antihypertensive drugs were presented. We performed a systematic review of 30 articles published before March 2008 that included a total of 6794 subjects. As there was significant heterogeneity in most of the outcomes, a random effects model was used for the meta-analyses. The mean changes (± standard error) in CBP and HBP (systolic/diastolic) were -15.2±0.03/-10.3±0.03 mmHg and -12.2±0.04/-8.0±0.04 mmHg respectively, although there were wide varieties of differences in the reduction between HBP and CBP. The reductions in CBP were correlated with those of HBP (systolic BP; r=0.66, B=0.48, diastolic BP; r=0.71, B=0.52, P<0.001). In 7 studies that also included 24-hour BP monitoring, the reduction of HBP was greater than that of 24-hr BP in systolic (HBP; -12.6±0.06 mmHg, 24-hr BP; -11.9±0.04 mmHg, P<0.001). In 5 studies that included daytime and nighttime systolic BP separately, HBP decreased 15% more than daytime ambulatory BP and 30% more than nighttime ambulatory BP. In conclusion, HBP falls about 20% less than CBP with antihypertensive treatments. Daytime systolic BP falls 15% less and nighttime systolic BP falls 30% less than home systolic BP.
Keywords: Home blood pressure, self-measured blood pressure, clinic blood pressure, meta-analysis
Introduction
The reduction of blood pressure (BP) levels by antihypertensive drug treatment is associated with decreased risks of cardiovascular events independently of the antihypertensive drug classes used to cause the reduction.1 In most of the studies investigating this effect BP has been evaluated using mercury or aneroid sphygmomanometers in a clinic or office setting. There is now increasing evidence that BP measurements made in “out-of-office” settings (using both home and ambulatory monitoring) are better predictors of cardiovascular events.2 The most widely used measure in these studies has been the twenty-four hour average ambulatory BP, which has been demonstrated to be a better predictor of cardiovascular events in patients taking antihypertensive medication.3 In a meta-analysis by Mancia and Parati,4 it was reported that the reduction of 24-hr average BP with antihypertensive medications (14.6 / 9.2 mmHg) was about 60 % of the reduction measured by clinic BP (24.9 / 14.5 mmHg).
Recently, devices for the self-measurement of home BP have become widely available, and their use for the evaluation of the effects of antihypertensive treatment has been endorsed by national and international guidelines,5-7 which recommend that BP should be measured both in the morning and at night. Like 24-hr ambulatory BP, home BPs also have greater predictive value for cardiovascular events than clinic BPs.8, 9 Home BP monitoring is less expensive and more suited to long-term repeated use than 24-hr ambulatory BP monitoring,10 and can assess the effectiveness of antihypertensive medication on BP control at different times of the day. Verberk et al.11 reported in the meta-analysis of home BP monitoring that the average reductions of clinic BP (20.1/13.6 mmHg) produced by antihypertensive medications were larger than the reductions of home BP (13.9/9.1 mmHg), but the number of studies available for this analysis was small (6 articles).
The purpose of this study was to compare, in a meta-analysis, the changes in home and clinic BP produced by different antihypertensive drugs, including the changes in both morning and evening BP levels.
Methods
Identification of papers
We performed a systematic review of home BP monitoring in PubMed at the end of December 2007. We used the key words “home blood pressure,” and “self-measured blood pressure” to search for candidate articles. Additional papers were collected from reference lists of the identified articles and reviews, and a follow-up search for more recent publications (through March 2008). There were no available articles in the Cochrane library.
Paper selection
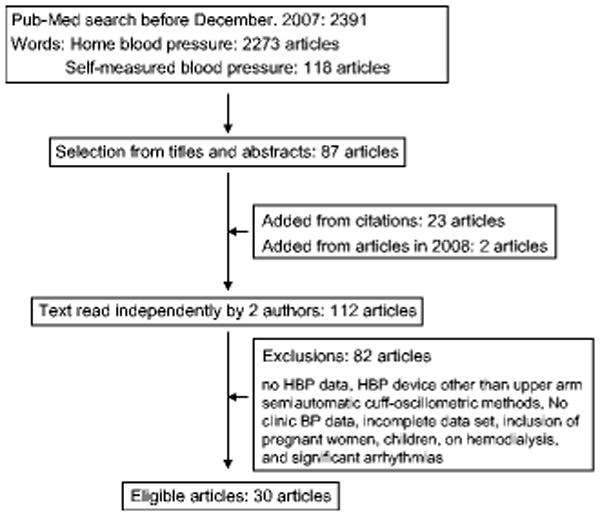
A flow chart summarizing the paper selection process is shown in Figure 1.12-41 The full text of those papers identified as potentially relevant on the basis of their titles and abstracts was reviewed by 2 independent investigators (JI and DJC). The criteria for papers to be included in the present meta-analysis were as follows: (1) study evaluated the effect(s) of at least one antihypertensive drug therapy, (2) results published for both home BP and clinic BP, pre- and post-treatment, (3) home BP measured using a semiautomatic or automatic upper-arm cuff oscillometric device, and (4) home BP measured in the morning and/or evening according to the guidelines.5-7 Studies were excluded from our analysis if they included: (1) pregnant women, (2) children, (3) patients on hemodialysis, and (4) patients with severe arrhythmia. We included 2 articles in which home BPs were measured only in the morning31, 36 (the morning home BPs were used as the average home BPs in these studies) and one article where BP was measured in the morning, at noon, and in the evening.16 We included some articles in which the method of clinic BP measurements was not clearly described,15, 19, 24, 30, 31, 33, 35-37 and/or in which clinic BP was measured only once per clinic visit,31 but we repeated our analyses excluding these articles. Rater differences in the selection of articles were discussed, and the last author (TGP) resolved any remaining discrepancies concerning article eligibility.
Figure 1. Flow chart of paper selection.
Data extraction
The averages of age, percentage of males, body mass index, antihypertensive medication use, dose and timing of antihypertensive drugs, and the methods of clinic and home BP measurements for each study were all abstracted as background data. The levels and changes of the clinic and home BPs and their standard deviations (SD) during the antihypertensive treatment periods were also collected. One article40 published data only for mean BP and pulse pressure, but the systolic and diastolic BP could be obtained from the original database, because the first author of this meta-analysis was a co-author of the article. In 7 articles,18, 20, 22, 25, 26, 32, 39 24-hr ambulatory BP data were also available, which we included in our analysis.
Data synthesis
The changes in clinic and home BPs were extracted for each of the eligible studies, excluding data for the placebo and control groups,14, 40 and also excluding 9 articles in which the method of clinic BP measurements were not described.15, 19, 24, 30, 31, 33, 35-37 The exclusion criteria of the 9 articles were as follows: 1) the technique and/or device of clinic BP measurements were not written, 2) the clinic BP was measured only once, and 3) the clinic BP was not measured by physicians or nurses. There were 13 articles in which home BP data were described separately for the morning and evening BP.12-15, 18, 20, 23, 25, 30, 37, 38, 40, 41 We also evaluated the changes in clinic, morning, and evening BP depending on whether the antihypertensive medication was taken in the morning12-15, 18, 20, 23, 25, 30, 41 or in the evening.12, 37, 38, 40 The effects of different antihypertensive drug classes on the changes in clinic and home BP (using morning dosing) were evaluated for calcium channel blockers (6 studies),12, 16, 17, 25, 35, 37 angiotensin converting enzyme inhibitors (5 studies),13, 14, 18, 21, 22 and angiotensin II receptor blockers (7 studies).18, 20-22, 24, 33, 41 Finally, we were able to compare the reductions of home BP with those of 24-hr BP in 7 articles18, 20, 22, 25, 26, 32, 39, and with daytime BP and nighttime BP in 5 articles. 22, 25, 26, 32, 39
Statistical analysis
The changes in BP measured before and after antihypertensive treatment periods are shown as mean ± standard error (SE), and the BPs measured at baseline are shown as mean ± SD. In the data sets in which standard deviations after the treatment periods were unavailable, it was assumed that the SDs of the BP before and after treatment were the same. As most of the accepted articles did not show SDs of the changes in clinic and home BP, the SDs were calculated using the formula42: [(SD at baseline)2 + (SD at follow-up)2 − 2 r (SD at baseline) (SD at follow-up)](0.5) . The r values of changes in clinic and home BPs were estimated from a study in which all variables were available (i.e. clinic systolic BP 0.50, clinic diastolic BP 0.32, home systolic BP 0.56, home diastolic BP 0.75, morning systolic BP 0.61, morning diastolic BP 0.78, evening systolic BP 0.54, evening diastolic BP 0.72).40 Before we evaluated the changes in clinic and home BP, we performed a heterogeneity test. The estimates of change in clinic and home BP exhibited significant heterogeneity across articles, and data synthesis was therefore performed using an unstandardized random effects model. Simple correlations between the reductions of BP were evaluated using Pearson's test weighted by the number of subjects enrolled in the studies. The differences in the change in clinic and home BP were calculated in all data sets, and meta-analyzed using a random effects model, except for the differences between home and 24-hr or daytime diastolic BP. These differences were analyzed using a fixed effects model because there was no significant heterogeneity. Additionally, the treatment induced BP changes corrected for the level of BP were calculated using the Oldham's correction43 (corrected BP change = actual change divided by the average of pre- and post-treatment BPs). The mean pre- and post-treatment BPs were meta-analyzed using a random effects model. All statistical analyses were performed using Excel-based (Microsoft Corp. USA) meta-analysis worksheets (developed by JES and JI) and SPSS (version 14.0, SPSS Inc. Chicago, Illinois, USA).
Results
The methods of clinic and home BP measurements in the selected studies are shown in Table 1.12-41 The baseline characteristics in the selected studies are shown in the Supplemental Table (S1) (please see http://hyper.ahajournals.org). The baseline levels and treatment-induced reductions in clinic and home BP, and the antihypertensive medications used, are shown in Table 2. 12-41 The baseline levels and treatment-induced BP reductions including in morning and evening and 24-hr BP, and the details of antihypertensive medications in the selected studies are shown in the Supplemental Table (S2) (please see http://hyper.ahajournals.org). The changes in clinic and home BP are shown in Figure 2. The reductions of home BP (-12.2/-8.0 mmHg) were 20% less for systolic and 22% less for diastolic BP than the reductions of clinic BP (-15.2/-10.3 mmHg, P<0.001, N=6794). When we excluded data sets in which the methods of clinic BP measurement were not clearly described,15, 19, 24, 30, 31, 33, 35, 36 the reductions of clinic and home BP were similar: -14.7 ± 0.04 / -10.7 ± 0.03 mmHg and -11.8 ± 0.04 / -8.1 ± 0.05 mmHg (P<0.001 for the both differences, N=6322). Scatter plots of the study-specific average changes in clinic and home systolic and diastolic BPs, and their correlations (weighted by the numbers of enrolled subjects) are shown in Figure 3. Additionally, scatter plots of study-specific average baseline BP levels and the BP reduction, and the correlations weighted by numbers of enrolled subjects are shown in Figure 4. The treatment induced BP changes corrected for the level of BP by using the Oldham's correction were 10.2 for clinic systolic BP, 11.5 % for clinic diastolic BP, 10.7 % for home systolic BP, and 9.2 % for home diastolic BP.
Table 1. Blood pressure measurement methods of 30 collected papers.
| Clinic BP | HBP measurements | |||||
|---|---|---|---|---|---|---|
| First author | N. Sub. | Clinic BP devices | Home BP devices | N. HBP | Time | Dur. |
| Mengden T12 | 19 | Sphg. | Visomat OZ1 | ? | ME | 2 w |
| Chatellier G13 | 816 | Sphyg. | UA751, A&D | 3 | ME | 4 d |
| Vaur L14 | 24 | Mercury sphyg. | A&D UA751 | 3 | ME | 7 d |
| Bailey B15 | 31 | Sphyg. | Omron HEM 706 | ? | ME | ? |
| Fernandez-G16 | 1395 | Omron HEM-705CP | Omron HEM-705CP | 2 | ME, noon | ? |
| Leeman MJ17 | 760 | Mercury or Aneroid Sphyg. | Omron HEM-705CP | 2 | ME | 8 d |
| Ragot S18 | 199 | Mercury sphyg. | UA751, A&D | 3 | ME | 7 d |
| Broege PA19 | 20 | Sphyg. | Omron HEM-702 | 3 | ME | ? |
| Mancia G20 | 215 | Sphyg, | Pressolink-T | 3 | ME | 7 d |
| 211 | Sphyg, | Pressolink-T | 3 | ME | 7d | |
| Ragot S21 | 217 | Omron HEM-705CP | Omron HEM-705CP | 3 | ME | 7 d |
| 218 | Omron HEM-705CP | Omron HEM-705CP | 3 | ME | 7 d | |
| Stergiou GS22 | 33 | Sphyg. | Omron HEM-705CP | 2 | ME | 5 d |
| Suzuki H23 | 113 | Sphyg. | Omron HEM 401C | 1 | ME | 2 d |
| Mengden T24 | 53 | Usual device | TensioPhone 2 | ≥1 | ME | ? |
| Mion D25 | 65 | Omron IC | Omron IC | 3 | ME | 7 d |
| Staessen JA26 | 197 | Shyg. ? | Omron HEM-705CP | 3 | ME | 7 d |
| 203 | Shyg. ? | Omron HEM-705CP | 3 | ME | 7 d | |
| Girerd X27 | 171 | TensioPhone | TensioPhone | 3 | ME | 4 d |
| Halme L28 | 113 | Omron M4 | Omron M4 | 2 | ME | 7 d |
| Borie G29 | 227 | Sphyg. or Electronical device | Tensio Day Monitor | 3 | ME | 5 d |
| 222 | Sphyg. or Electronical device | Tensio Day Monitor | 3 | ME | 5 d | |
| Hashimoto J30 | 76 | NA | Omron HEM701C, 703C, 747IC, 747IC-N | 1 | ME | 5 d |
| Kamoi K31 | 50 | FT-200 | Semiautomatic arm-cuff oscillometric | 1 | M | ? |
| Niiranen TJ32 | 56 | Sphyg. | Omron M4, HEM-722C | 2 | ME | 7 d |
| Ewald S33 | 53 | NA | TensioPhone 2 | ≥1 | ME | ? |
| Karotsis AK34 | 185 | A&D767 | A&D767 | ? | ME | 3 d |
| Yamagishi T35 | 54 | NA | Omron HEM401C | 1 | ME | ? |
| 54 | NA | Omron HEM401C | 1 | ME | ? | |
| Yamagishi T36 | 43 | NA | Automatic arm-cuff device | 1 | M | ? |
| 15 | NA | Automatic arm-cuff device | 1 | M | ? | |
| Ashizawa N37 | 23 | NA | Automatic arm-cuff device | ? | ME | ? |
| Ikeda T38 | 49 | Omron, HEM907 | Omron HEM-737 | 2 | ME | ? |
| Verberk WJ39 | 214 | Omron, HEM705CP | Omron, HEM705CP | 3 | ME | 7 d |
| Eguchi K40 | 308 | Omron, HEM705IT | Omron, HEM705IT | 2 | ME | 3 d |
| Nakamoto H41 | 21 | Omron, HEM705IT | Omron, HEM705IT | ≥1 | ME | ? |
| 19 | Omron, HEM705IT | Omron, HEM705IT | ≥1 | ME | Tel | |
NA indicates not applicable; N. Sub., Number of enrolled subjects; Sphyg., sphygmomanometer; N. HBP, number of home blood pressure measurements in one occasions; ME, morning and evening; M, morning; w, weeks; d, days; Tel, telemedicine. In the paper of Girerd X et al. home blood pressure was measured in the standing position.
Table 2. Changes in blood pressures and baseline blood pressure levels.
| Anti-HTN treatments | Reduction of systolic / diastolic BPs (mmHg) | Baseline level of systolic / diastolic BPs (mmHg) | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| First author | N | Drug name | CBP | HBP | CBP | HBP |
| Mengden T12 | 19 | Amlodipine | 13 / 8 | 11.5 / 6.5 | 158 / 103 | 151 / 97.5 |
| 19 | Amlodipine | 12 / 5 | 7 / 4 | 158 / 103 | 151 / 97.5 | |
| Chatellier G13 | 816 | Trandpril | 21.8 / 15.3 | 13.8 / 8.7 | 166.4 / 101.4 | 153.2 / 93.8 |
| Vaur L14 | 24 | Trandpril | 10.2 / 8.3 | 10.7 / 5.8 | 163 / 101 | 146 / 94 |
| Bailey B15 | 31 | Perindopril or Indapamide | 8 / 4 | 8 / 4 | 156 / 93 | 146 / 88.5 |
| Fernandez-G16 | 1395 | Verapamil SR | 20.1 / 13.0 | 16.8 / 11.0 | 165.9 / 97.8 | 158.7 / 93.3 |
| Leeman MJ17 | 760 | Diltiazem SR | 20 / 13 | 11 / 8 | 162 / 99 | 155 / 95 |
| Ragot S18 | 105 | Losartan | 17.5 / 14.3 | 8.8 / 4.3 | 160.0 / 99.7 | 144.0 / 88.6 |
| 94 | Trandpril | 16.9 / 12.7 | 9.6 / 5.2 | 160.2 / 99.8 | 144.3 / 90.5 | |
| Broege PA19 | 20 | Cholrthalidone Prinivil *3 | -3 / -5 | 2 / 0 | 153 / 78 | 140 / 77 |
| Mancia G20 | 215 | Valsartan | 10 / 7.3 | 8.2 / 4.9 | 158 / 100.8 | 149.5 / 95.8 |
| 211 | Irbesartan | 16.2 / 10.5 | 11.1 / 6.9 | 159.3 / 100.7 | 140.0 / 95.5 | |
| Ragot S21 | 217 | Telmisartan | 13.9 / 8.9 | 12.3 / 6.6 | 157.9 / 97.6 | 151.6 / 94.2 |
| 218 | Perindopril | 10.9 / 6.6 | 8.9 / 5.2 | 158.9 / 97.9 | 152.2 / 94.8 | |
| Stergiou GS22 | 33 | Lisinopril | 15 / 10.5 | 17 / 10.1 | 144 / 95.6 | 145 / 93.2 |
| 33 | Losartan | 8.3 / 5.9 | 8.3 / 4.5 | 144 / 95.6 | 145 / 93.2 | |
| Suzuki H23 | 113 | Amlodipine Benazepril | 19 / 20 | 20.5 / 16 | 148 / 89.0 | 155 / 91.0 |
| Mengden T24 | 53 | Olmesartan | 27.6 / 16.0 | 9.2 / 6.7 | 162.6 / 96.3 | 149.8 / 85.7 |
| Mion D25 | 65 | Amlodipine | 2 / 5 | 6.5 / 1 | 164 / 99 | 160 / 93.5 |
| Staessen JA26 | 197 | Lisinopril, HCZ, Amlodipine, or Prazosin *1 | 22 / 14 | 16 / 10.2 | 159.1 / 101.5 | 146.4 / 92.2 |
| 203 | Lisinopril, HCZ, Amlodipine, or Prazosin *2 | 15.3 / 10.5 | 11.1 / 7.3 | 160.8 / 101.8 | 146.8 / 92.0 | |
| Girerd X27 | 171 | Valsartan HCZ | 6 / 4 | 6 / 4 | 157 / 91 | 152 / 87 |
| Halme L28 | 113 | Any | 12.7 / 7.1 | 7.8 / 3.1 | 159.5 / 94.1 | 143.1 / 85.3 |
| Borie G29 | 227 | Valsartan HCZ | 11.8 / 6.9 | 10.6 / 7.4 | 153 / 90 | 149 / 89 |
| 222 | Irbesartan HCZ | 15 / 8.6 | 13 / 9.5 | 153 / 91 | 149 / 90 | |
| Hashimoto J30 | 76 | Indapamide | 9 / 5 | 12 / 6 | 145 / 86 | 142.5 / 83 |
| Kamoi K31 | 50 | Doxazosin | 9 / 4 | 18 / 5 | 151 / 87 | 164 / 85 |
| Niiranen TJ32 | 56 | Candesartan HCZ *3 Felodipine *3 | 18.5 / 10.3 | 17.1 / 10.0 | 149.3 / 94.4 | 143.4 / 90.5 |
| Ewald S33 | 53 | Olmesartan | 29.1 / 16.5 | 9.2 / 6.7 | 162.6 / 96.3 | 147.8 / 85.7 |
| Karotsis AK34 | 185 | Chlorthalidone Felodipine, Lisinopril, or Valsartan | 21.6 / 7.7 | 14.7 / 5.7 | 158.6 / 86.1 | 150.3 / 83.0 |
| Yamagishi T35 | 54 | Azelnidipine | 28.2 / 17.2 | 23.5 / 14.2 | 165.5 / 99.1 | 160.1 / 97.5 |
| 54 | Amlodipine | 23.2 / 14.1 | 20.5 / 12.2 | 157.3 / 96.0 | 154.8 / 95.4 | |
| Yamagishi T36 | 43 | Cilnidipine | 15.5 / 9.1 | 11.9 / 6.7 | 146.3 / 87.5 | 146.2 / 88.7 |
| 15 | Cilnidipine | 29.9 / 19.0 | 19 / 12.1 | 163.7 / 99.5 | 150.3 / 95.1 | |
| Ashizawa N37 | 23 | Cilnidipine | 6.9 / 1.9 | 11.75 / 3.9 | 144.3 / 84.1 | 143.1 / 81.6 |
| Ikeda T38 | 49 | Doxazosin | 1.6 / 2.5 | 7.2 / 4.4 | 137.9 / 87.7 | 137.3 / 85.7 |
| Verberk WJ39 | 214 | NA | 22 / 11.7 | 21.8 / 11.9 | 166.2 / 97.1 | 156.1 / 92.8 |
| Eguchi K40 | 308 | Doxazosin, Atenolol *3 | 12.4 / 9.8 | 10.3 / 7.1 | 157 / 83 | 146 / 79 |
| Nakamoto H41 | 21 | Telmisartan | 19 / 9 | 10 / 10 | 167 / 97 | 144 / 93 |
| 19 | Amlodipine | 14 / 10 | 8 / 6 | 164 / 95 | 143 / 91 | |
CBP indicates clinic blood pressure; HBP, home blood pressure; HCZ, Hydrochlorothiazide; Anti-HTN, anti-hypertensive.
was treated based on clinic blood pressure level, and
was treated based on home blood pressure level.
indicate added antihypertensive drugs when the subjects did not achieved target blood pressure levels.
Figure 2. Changes in home and clinic blood pressures.
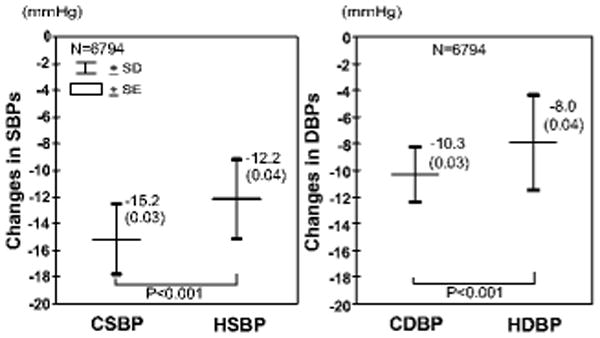
Data were collected from 30 articles (6794 subjects), and analyzed using a random effects model. Data are shown as mean (standard error). CSBP indicates clinic systolic blood pressure; CDBP, clinic diastolic blood pressure; HSBP, home systolic blood pressure; HDBP, home diastolic blood pressure.
Figure 3. Scatterplot of changes in between clinic and home blood pressures in all studies.
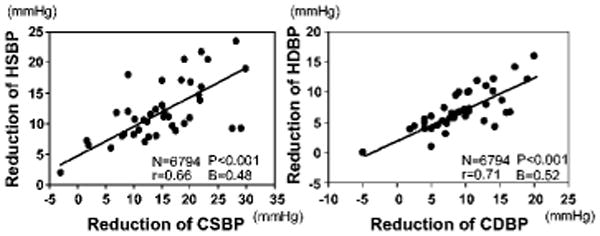
Data were collected from 30 articles (6794 subjects). Regression line, correlation coefficients (r), and regression coefficients (B) were analyzed weighted for number of enrolled subjects. CSBP indicates clinic systolic blood pressure; CDBP, clinic diastolic blood pressure; HSBP, home systolic blood pressure; HDBP, home diastolic blood pressure.
Figure 4. Relationship between baseline blood pressure levels and the reduction.
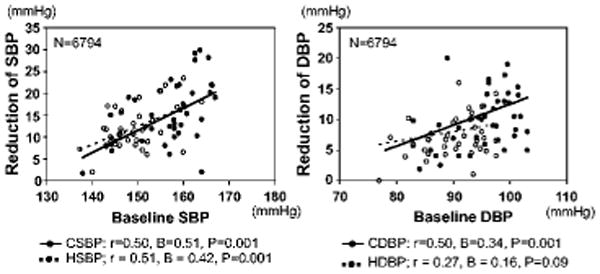
Data were collected from 30 articles (6794 subjects). Regression line, correlation coefficients (r), and regression coefficients (B) were analyzed weighted for number of enrolled subjects. CSBP indicates clinic systolic blood pressure; CDBP, clinic diastolic blood pressure; HSBP, home systolic blood pressure; HDBP, home diastolic blood pressure.
In the 7 articles in which 24-hr average BPs were available (N=1246),18, 20, 22, 25, 26, 32, 39 the changes in clinic, home, and 24-hr ambulatory BPs were -15.2 ± 0.07 / -10.2 ± 0.10 mmHg, -12.6 ± 0.06 / -8.2 ± 0.07 mmHg, -11.9 ± 0.04 / -8.5 ± 0.02 mmHg, respectively, and the differences between home and 24-hr ambulatory systolic BP was significant (1.2 mmHg, 95%CI 0.8-1.5 mmHg, P<0.001). Home systolic BP decreased 6% more than the 24-hr average systolic BP. The reductions of home diastolic BP and 24-hr diastolic BP (8.2 and 8.5 mmHg) were similar, although the difference was statistically significant (0.4 mmHg, 95%CI 0.2 to 0.7 mmHg, P<0.001).
In the 5 articles in which both daytime BP and nighttime BP were separately available (N=801) (excluding 2 articles in which only 24-hr average BP data was available),22, 25, 26, 32, 39 the treatment-induced changes are shown in Figure 5. Thus home systolic BP decreased 15% more than daytime ambulatory systolic BP, and 30% more than nighttime ambulatory systolic BP. The differences in home and daytime BP reductions were 1.6 mmHg (95%CI 1.1 to 2.2 mmHg, P<0.001) for systolic and 0.2 mmHg (95%CI -0.4 to 0.8 mmHg, P=0.55) for diastolic, and that in home and nighttime BP reductions were 3.8 mmHg (95%CI 3.3 to 4.4 mmHg, P<0.001) for systolic and 1.2 mmHg (95%CI 0.6 to 1.8 mmHg, P<0.001) for diastolic. Additionally, the treatment induced BP changes corrected for the level of BPs by using the Oldham's correction were 10.3 % for clinic systolic BP, 10.9 % for clinic diastolic BP, 10.1 % for home systolic BP, 10.4 % for home diastolic BP, 8.5 % for daytime systolic BP, 9.0 % for daytime diastolic BP, 8.1 % for nighttime systolic BP, and 9.0 % for nighttime diastolic BP.
Figure 5. Changes in home and daytime and nighttime blood pressures.
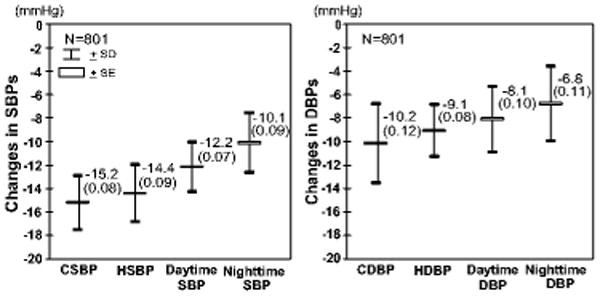
Data were collected from 5 articles (801 subjects), and analyzed using a random effects model except for the difference between home DBP and daytime DBP. Data are shown as mean (standard error). CSBP indicates clinic systolic blood pressure; CDBP, clinic diastolic blood pressure; HSBP, home systolic blood pressure; HDBP, home diastolic blood pressure. The difference between home BP and daytime BP are P<0.001 for systolic and P=0.59 for diastolic, and the difference between home BP and nighttime BP are both P<0.001
In the 10 articles in which antihypertensive drugs were taken in the morning (N=1809),12-15, 18, 20, 23, 25, 30, 41 the changes in clinic, morning and evening BP were -13.0 ± 0.04 / -11.2 ± 0.04 mmHg, -10.8 ± 0.08 / -6.1 ± 0.09 mmHg, -11.7 ± 0.06 / -7.4 ± 0.06 mmHg. The evening BP was reduced marginally more than morning BP [the difference: 1.1 mmHg (95%CI 0.9 to 1.2 mmHg, P<0.001) for systolic and 1.5 mmHg (95%CI 1.3 to 1.6 mmHg, P<0.001) for diastolic]. In the 4 articles in which antihypertensive drugs were taken in the evening (N=399),12, 37, 38, 40 the changes in clinic, morning, and evening BP were -8.2 ± 0.07 / -5.0 ± 0.10 mmHg, -12.5 ± 0.17 / -7.5 ± 0.20 mmHg, -5.6 ± 0.12 / -3.8 ± 0.15 mmHg. The morning BP reduced more than evening BP [the difference: 6.8 mmHg (95%CI 6.57 to 6.95 mmHg, P<0.001) for systolic and 3.6 mmHg (95%CI 3.4 to 3.9 mmHg, P<0.001) for diastolic].
In 6 articles 12,16,17, 25,35,41, the effects of calcium channel blockers (taken in the morning) on the reduction of CBP and HBP were 17.5 ± 0.10 / 12.4 ± 0.13 mmHg and 14.1 ± 0.07 / 9.1 ± 0.08 mmHg, and the differences between clinic and home BP were 3.3 mmHg (95%CI 3.1 to 3.5 mmHg, P<0.001) for systolic and 3.0 mmHg (95%CI 2.8 to 3.3 mmHg). The BP reductions corrected for the level of BPs by using the Oldham's correction were 11.4 % for clinic systolic BP, 13.5 % for clinic diastolic BP, 9.5 % for home systolic BP, and 10.2 % for home diastolic BP. In 5 articles,13, 14, 18, 21, 22 the effects of angiotensin converting enzyme inhibitors on the reduction of clinic BP and home BP were 15.1 ± 0.07 / 10.9 ± 0.08 mmHg and 11.9 ± 0.15 / 6.8 ± 0.14 mmHg, and the difference between clinic and home BP were 3.2 mmHg (95%CI 3.0 to 3.4 mmHg) for systolic and 4.3 mmHg (95%CI 3.7 to 4.9 mmHg) for diastolic. The BP reductions corrected for the level of BPs by using the Oldham's correction were 9.9 % for clinic systolic BP, 11.4 % for clinic diastolic BP, 8.4 % for home systolic BP, and 7.6 % for home diastolic BP. In 7 articles,18, 20, 22, 24, 33, 41 the effect of angiotensin II receptor blockers on reduction of CBP and HBP were 17.6 ± 0.07 / 10.5 ± 0.11 mmHg and 9.9 ± 0.23 / 6.5 ± 0.14 mmHg, and the difference between clinic and home BP were 8.0 mmHg (95%CI 7.8 to 8.2 mmHg) for systolic and 3.2 mmHg (95%CI 2.7 to 3.8 mmHg) for diastolic. The BP reductions corrected for the level of BPs by using the Oldham's correction were 14.3 % for clinic systolic BP, 11.2 % for clinic diastolic BP, 6.9 % for home systolic BP, and 7.3 % for home diastolic BP. In 2 articles in which there were placebo or control subjects,14, 40 the changes in clinic and home BP were -4.5 ± 0.89 / -4.8 ± 0.17 mmHg and -2.1 ± 0.32 / -1.9 ± 0.37 mmHg, respectively (the difference; both P<0.001).
Discussion
The main findings of the present meta-analyses are as follows: (1) the changes produced by antihypertensive drug treatments in home BP were 20% smaller than those of clinic BP, and the changes in clinic BP were linearly related to those of home BP; (2) the difference in the BP reduction between clinic and home BP were attributable to the difference in the baseline BP levels; (3) the changes in home SBP were intermediate between the changes of clinic and ambulatory SBPs (including 24-hr SBP, daytime SBP, and nighttime SBP); and (4) the differing effects on clinic and home BP were similar for calcium channel blockers, angiotensin converting enzyme inhibitors, and angiotensin II receptor blockers, and also for placebo or control groups.
The changes in clinic and home BP (systolic / diastolic) produced by antihypertensive drug treatments were -15.2 / -10.3 mmHg and -12.2 / -8.0 mmHg, respectively, and these reductions of BP were smaller than the values shown in the Verberk's previous meta-analysis11. The changes in home and clinic BPs were linearly related to each other in the present meta-analysis, such that the effect on home BP was typically about 80% of the effect on clinic BP. Mancia and Parati4 reported that the reductions of clinic BP and 24-hr BP with antihypertensive treatments were -24.9 / -14.5 mmHg and -14.6 / -9.2 mmHg, respectively, and that the effect on 24-hr ambulatory BP was about 60% of the effect on clinic BP. Taken together, these results indicate that the reduction of home BP is about 20 % smaller, and that of 24-hr BP 40% smaller than the reduction of clinic BP produced by antihypertensive drugs.
The greater reductions of clinic BP than home BP with antihypertensive treatment were attributable to the difference in BP levels at baseline (usually clinic BP > home BP). This indicated that the lower the baseline BP levels are, the smaller the difference in the BP reduction between clinic BP and home BP will be.
In our meta-analysis of 7 studies which included 24-hr BP data as well as home BP,18, 20, 22, 25, 26, 32, 39 the reduction of 24-hr systolic BP was indeed less than the reduction of home SBP by 6%. When we analyzed the data in 5 studies in which both daytime and nighttime SBP were available, 22, 25, 26, 32, 39 the reductions of 24-hr systolic BP, daytime systolic BP and nighttime systolic BP were about 15%, 15% and 30% smaller than that of home systolic BP. In the meta-analysis of Mancia and Parati,4 it was also reported that nighttime BP was reduced less than daytime BP by antihypertensive drugs taken in the morning. Our meta-analysis indicated that the reduction of daytime BP was smaller than that of home BP. The difficulties in reducing nighttime BP might derive from morning dosing of antihypertensive drugs. To obtain nighttime BP control, Kario et al.44 previously reported that nighttime dosing of doxazosin, an alpha-adrenergic blocker, is effective. Additionally, Hermida et al.45-47 have reported that angiotensin II receptor blockers taken at bedtime reduced nighttime BP significantly more than when taken in the morning.
It is not clear why home BP exhibits a smaller reduction than clinic BP and a greater reduction than 24-hr BP following antihypertensive drug treatment. The baseline levels of clinic BP were higher than home BP, and there might be a regression-to-the-mean effect. The regression line of baseline BP levels and the BP reduction were similar between clinic BP and home BP. Even in placebo or control groups, the reductions of clinic BP were larger than home BP. Additionally, there might be a white coat effect (transient BP elevation in the physician's office) which is generally recognized to be reduced by both active and placebo treatment.48 Another factor affecting the differences in the reductions of clinic and home BP seems to be the timing of the administration of antihypertensive medications. Antihypertensive drugs taken in the evening reduced morning BP greater than clinic BP.
In some trials the BP decline was larger at home than in the office; in other trials this difference was negligible, and in some the office BP decline was 3 times larger. These differences in the reductions of CBP and HBP might be explained by inaccuracy of CBP measurements, because some studies did not describe the technique of CBP measurements (i.e. the BP devices and number of measurements). Therefore, we analyzed the reductions of CBP and HBP after excluding data sets in which the methods of clinic BP measurement were not clearly described; however, the reductions of CBP and HBP were similar to the results of the whole data set.
Supplementary Material
Perspectives.
The reduction of home BP produced by antihypertensive drug treatment is about 80% of the magnitude of the reduction of clinic BP.
Acknowledgments
We thank Yukiko Ishikawa, MD, and Lim Zhen Lin, RDCS, for helping the preparation of this article.
Source of Funding: Supported in part by grants from NHLBI (R24 HL76857 and PO1- HL 47540)
Disclosure: The first author is supported in part by a grant from Mitsubishi Pharma Research Foundation
References
- 1.Staessen JA, Wang JG, Thijs L. Cardiovascular protection and blood pressure reduction: a meta-analysis. The Lancet. 2001;358:1305–1315. doi: 10.1016/S0140-6736(01)06411-X. [DOI] [PubMed] [Google Scholar]
- 2.Clement DL, De Buyzere ML, De Bacquer DA, de Leeuw PW, Duprez DA, Fagard RH, Gheeraert PJ, Missault LH, Braun JJ, Six RO, Van Der Niepen P, O'Brien E the Office versus Ambulatory Pressure Study I. Prognostic Value of Ambulatory Blood-Pressure Recordings in Patients with Treated Hypertension. N Engl J Med. 2003;348:2407–2415. doi: 10.1056/NEJMoa022273. [DOI] [PubMed] [Google Scholar]
- 3.Staessen JA, Thijs L, Fagard R, O'Brien ET, Clement D, de Leeuw PW, Mancia G, Nachev C, Palatini P, Parati G, Tuomilehto J, Webster J for the Systolic Hypertension in Europe Trial I. Predicting Cardiovascular Risk Using Conventional vs Ambulatory Blood Pressure in Older Patients With Systolic Hypertension. JAMA. 1999;282:539–546. doi: 10.1001/jama.282.6.539. [DOI] [PubMed] [Google Scholar]
- 4.Mancia G, Parati G. Office compared with ambulatory blood pressure in assessing response to antihypertensive treatment: a meta-analysis. J Hypertens. 2004;22:435–445. doi: 10.1097/00004872-200403000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, Jones DW, Kurtz T, Sheps SG, Roccella EJ. Recommendations for Blood Pressure Measurement in Humans and Experimental Animals: Part 1: Blood Pressure Measurement in Humans: A Statement for Professionals From the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005;45:142–161. doi: 10.1161/01.HYP.0000150859.47929.8e. [DOI] [PubMed] [Google Scholar]
- 6.O'Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G, Mengden T, Myers M, Padfield P, Palatini P, Parati G, Pickering T, Redon J, Staessen J, Stergiou G, Verdecchia P. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–848. doi: 10.1097/00004872-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Imai Y, Otsuka K, Kawano Y, Shimada K, Hayashi H, Tochikubo O, Miyakawa M, Fukiyama K. Japanese society of hypertension (JSH) guidelines for self-monitoring of blood pressure at home. Hypertens Res. 2003;26:771–782. doi: 10.1291/hypres.26.771. [DOI] [PubMed] [Google Scholar]
- 8.Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, Nishiyama A, Aihara A, Sekino M, Kikuya M, Ito S, Satoh H, Hisamichi S. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens. 1998;16:971–975. doi: 10.1097/00004872-199816070-00010. [DOI] [PubMed] [Google Scholar]
- 9.Bobrie G, Chatellier G, Genes N, Clerson P, Vaur L, Vaisse B, Menard J, Mallion JM. Cardiovascular Prognosis of “Masked Hypertension” Detected by Blood Pressure Self-measurement in Elderly Treated Hypertensive Patients. JAMA. 2004;291:1342–1349. doi: 10.1001/jama.291.11.1342. [DOI] [PubMed] [Google Scholar]
- 10.Pickering TG, Shimbo D, Haas D. Ambulatory Blood-Pressure Monitoring. N Engl J Med. 2006;354:2368–2374. doi: 10.1056/NEJMra060433. [DOI] [PubMed] [Google Scholar]
- 11.Verberk WJ, Kroon AA, Kessels AGH, de Leeuw PW. Home Blood Pressure Measurement: A Systematic Review. J Am Coll Cardiol. 2005;46:743–751. doi: 10.1016/j.jacc.2005.05.058. [DOI] [PubMed] [Google Scholar]
- 12.Mengden T, Binswanger B, Spuhler T, Weisser B, Vetter W. The use of self-measured blood pressure determinations in assessing dynamics of drug compliance in a study with amlodipine once a day, morning versus evening. J Hypertens. 1993;11:1403–1411. doi: 10.1097/00004872-199312000-00013. [DOI] [PubMed] [Google Scholar]
- 13.Chatellier G, Dutrey-Dupagne C, Vaur L, Zannad F, Genes N, Elkik F, Menard J. Home self blood pressure measurement in general practice. The SMART study. Self-measurement for the Assessment of the Response to Trandolapril. Am J Hypertens. 1996;9:644–652. doi: 10.1016/0895-7061(96)00018-0. [DOI] [PubMed] [Google Scholar]
- 14.Vaur L, Dubroca II, Dutrey-Dupagne C, Genes N, Chatellier G, Bouvier-d'Yvoire M, Elkik F, Menard J. Superiority of home blood pressure measurements over office measurements for testing antihypertensive drugs. Blood Press Monit. 1998;3:107–114. [PubMed] [Google Scholar]
- 15.Bailey B, Carney SL, Gillies AA, Smith AJ. Antihypertensive drug treatment: a comparison of usual care with self blood pressure measurement. J Hum Hypertens. 1999;13:147–150. doi: 10.1038/sj.jhh.1000758. [DOI] [PubMed] [Google Scholar]
- 16.Fernandez-Gonzalez R, Gomez-Pajuelo C, Gabriel R, de La Figuera M, Moreno E of The Verapamil-Frequency R. Effect of verapamil on home self-measurement of blood pressure and heart rate by hypertensive patients. Verapamil-Frequency Research Group. Blood Press Monit. 2000;5:23–30. doi: 10.1097/00126097-200002000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Leeman MJ, Lins RL, Sternon JE, Huberlant BC, Fassotte CE. Effect of antihypertensive treatment on office and self-measured blood pressure: the Autodil study. J Hum Hypertens. 2000;14:525–529. doi: 10.1038/sj.jhh.1001068. [DOI] [PubMed] [Google Scholar]
- 18.Ragot S, Genes N, Vaur L, Herpin D. Comparison of three blood pressure measurement methods for the evaluation of two antihypertensive drugs: feasibility, agreement, and reproducibility of blood pressure response. Am J Hypertens. 2000;13:632–639. doi: 10.1016/s0895-7061(99)00258-7. [DOI] [PubMed] [Google Scholar]
- 19.Broege PA, James GD, Pickering TG. Management of hypertension in the elderly using home blood pressures. Blood Press Monit. 2001;6:139–144. doi: 10.1097/00126097-200106000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Mancia G, Korlipara K, van Rossum P, Villa G, Silvert B. An ambulatory blood pressure monitoring study of the comparative antihypertensive efficacy of two angiotensin II receptor antagonists, irbesartan and valsartan. Blood Press Monit. 2002;7:135–142. doi: 10.1097/00126097-200204000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Ragot S, Ezzaher A, Meunier A, Poterre M, Bourkaib R, Herpin D. Comparison of trough effect of telmisartan vs perindopril using self blood pressure measurement: EVERESTE study. J Hum Hypertens. 2002;16:865–873. doi: 10.1038/sj.jhh.1001494. [DOI] [PubMed] [Google Scholar]
- 22.Stergiou GS, Efstathiou SP, Skeva II, Baibas NM, Kalkana CB, Mountokalakis TD. Assessment of drug effects on blood pressure and pulse pressure using clinic, home and ambulatory measurements. J Hum Hypertens. 2002;16:729–735. doi: 10.1038/sj.jhh.1001477. [DOI] [PubMed] [Google Scholar]
- 23.Suzuki H, Nakamoto H, Okada H, Sugahara S, Kanno Y. Self-measured systolic blood pressure in the morning is a strong indicator of decline of renal function in hypertensive patients with non-diabetic chronic renal insufficiency. Clin Exp Hypertens. 2002;24:249–260. doi: 10.1081/ceh-120004229. [DOI] [PubMed] [Google Scholar]
- 24.Mengden T, Ewald S, Kaufmann S, vor dem Esche J, Uen S, Vetter H. Telemonitoring of blood pressure self measurement in the OLMETEL study. Blood Press Monit. 2004;9:321–325. doi: 10.1097/00126097-200412000-00010. [DOI] [PubMed] [Google Scholar]
- 25.Mion D, Ortega KC, Gomes MA, Kohlmann O, Oigman W, Nobre F. Amlodipine 2.5 mg once daily in older hypertensives: a Brazilian multi-centre study. Blood Press Monit. 2004;9:83–89. doi: 10.1097/00126097-200404000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Staessen JA, Den Hond E, Celis H, Fagard R, Keary L, Vandenhoven G, O'Brien ET. Antihypertensive treatment based on blood pressure measurement at home or in the physician's office: a randomized controlled trial. JAMA. 2004;291:955–964. doi: 10.1001/jama.291.8.955. [DOI] [PubMed] [Google Scholar]
- 27.Girerd X, Denolle T, Yau C, Fiquet B, Brunel P, Moulin B, Herpin D. Automated office and home phone-transmitted blood pressure recordings in uncontrolled hypertension treated with valsartan and hydrochlorothiazide. Blood Press Suppl. 2004;2:18–24. doi: 10.1080/08038020410004756. [DOI] [PubMed] [Google Scholar]
- 28.Halme L, Vesalainen R, Kaaja M, Kantola I. Self-Monitoring of Blood Pressure Promotes Achievement of Blood Pressure Target in Primary Health Care. Am J Hypertens. 2005;18:1415–1420. doi: 10.1016/j.amjhyper.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 29.Bobrie G, Delonca J, Moulin C, Giacomino A, Postel-Vinay N, Asmar R. A home blood pressure monitoring study comparing the antihypertensive efficacy of two angiotensin II receptor antagonist fixed combinations. Am J Hypertens. 2005;18:1482–1488. doi: 10.1016/j.amjhyper.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 30.Hashimoto J, Hirayama H, Hanasawa T, Watabe D, Asayama K, Metoki H, Kikuya M, Ohkubo T, Totsune K, Imai Y. Efficacy of combination antihypertensive therapy with low-dose indapamide: assessment by blood pressure self-monitoring at home. Clin Exp Hypertens. 2005;27:331–341. [PubMed] [Google Scholar]
- 31.Kamoi K, Ikarashi T. The bedtime administration of doxazosin controls morning hypertension and albuminuria in patients with type-2 diabetes: evaluation using home-based blood pressure measurements. Clin Exp Hypertens. 2005;27:369–376. [PubMed] [Google Scholar]
- 32.Niiranen TJ, Kantola IM, Vesalainen R, Johansson J, Ruuska MJ. A Comparison of Home Measurement and Ambulatory Monitoring of Blood Pressure in the Adjustment of Antihypertensive Treatment. Am J Hypertens. 2006;19:468–474. doi: 10.1016/j.amjhyper.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 33.Ewald S, vor dem Esche J, Uen S, Neikes F, Vetter H, Mengden T. Relationship between the frequency of blood pressure self-measurement and blood pressure reduction with antihypertensive therapy : results of the OLMETEL (OLMEsartan TELemonitoring blood pressure) study. Clin Drug Investig. 2006;26:439–446. doi: 10.2165/00044011-200626080-00002. [DOI] [PubMed] [Google Scholar]
- 34.Karotsis AK, Symeonidis A, Mastorantonakis SE, Stergiou GS. Additional antihypertensive effect of drugs in hypertensive subjects uncontrolled on diltiazem monotherapy: a randomized controlled trial using office and home blood pressure monitoring. Clin Exp Hypertens. 2006;28:655–662. doi: 10.1080/10641960600946429. [DOI] [PubMed] [Google Scholar]
- 35.Yamagishi T. Efficacy of azelnidipine on home blood pressure and pulse rate in patients with essential hypertension: comparison with amlodipine. Hypertens Res. 2006;29:767–773. doi: 10.1291/hypres.29.767. [DOI] [PubMed] [Google Scholar]
- 36.Yamagishi T. Beneficial effect of cilnidipine on morning hypertension and white-coat effect in patients with essential hypertension. Hypertens Res. 2006;29:339–344. doi: 10.1291/hypres.29.339. [DOI] [PubMed] [Google Scholar]
- 37.Ashizawa N, Seto S, Shibata Y, Yano K. Bedtime administration of cilnidipine controls morning hypertension. Int Heart J. 2007;48:597–603. doi: 10.1536/ihj.48.597. [DOI] [PubMed] [Google Scholar]
- 38.Ikeda T, Gomi T, Shibuya Y, Shinozaki S, Suzuki Y, Matsuda N. Add-On Effect of Bedtime Dosing of the alpha(1)-Adrenergic Receptor Antagonist Doxazosin on Morning Hypertension and Left Ventricular Hypertrophy in Patients Undergoing Long-Term Amlodipine Monotherapy. Hypertens Res. 2007;30:1097–1105. doi: 10.1291/hypres.30.1097. [DOI] [PubMed] [Google Scholar]
- 39.Verberk WJ, Kroon AA, Lenders JW, Kessels AG, van Montfrans GA, Smit AJ, van der Kuy PH, Nelemans PJ, Rennenberg RJ, Grobbee DE, Beltman FW, Joore MA, Brunenberg DE, Dirksen C, Thien T, de Leeuw PW. Self-measurement of blood pressure at home reduces the need for antihypertensive drugs: a randomized, controlled trial. Hypertension. 2007;50:1019–1025. doi: 10.1161/HYPERTENSIONAHA.107.094193. [DOI] [PubMed] [Google Scholar]
- 40.Eguchi K, Matsui Y, Shibasaki S, Ishikawa J, Hoshide S, Ishikawa S, Kabutoya T, Schwartz JE, Pickering TG, Shimada K, Kario K. Changes in self-monitored pulse pressure correlate with improvements in B-type natriuretic Peptide and urinary albumin in treated hypertensive patients. Am J Hypertens. 2007;20:1268–1275. doi: 10.1016/j.amjhyper.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 41.Nakamoto H, Nishida E, Ryuzaki M, Sone M, Suzuki H, Yoshimoto M, Itagaki K. Effect of telmisartan and amlodipine on home blood pressure by monitoring newly developed telemedicine system: monitoring test by using telemedicine. Telmisartan's effect on home blood pressure (teltelbosu) Clin Exp Hypertens. 2008;30:57–67. doi: 10.1080/10641960701815804. [DOI] [PubMed] [Google Scholar]
- 42.Snedecor GW, Cochran WG. Statistical Methods. Sixth. Iowa State University Press Ames; Iowa, USA: 1967. p. 190. [Google Scholar]
- 43.Gill JS, Beevers DG, Zezulka AV, Davies P. Relationship between initial blood pressure and its fall with treatment. The Lancet. 1985;325:567–569. doi: 10.1016/s0140-6736(85)91219-x. [DOI] [PubMed] [Google Scholar]
- 44.Kario K, Schwartz JE, Pickering TG. Changes of Nocturnal Blood Pressure Dipping Status in Hypertensives by Nighttime Dosing of {alpha}-Adrenergic Blocker, Doxazosin : Results from the HALT Study. Hypertension. 2000;35:787–794. doi: 10.1161/01.hyp.35.3.787. [DOI] [PubMed] [Google Scholar]
- 45.Hermida RC, Calvo C, Ayala DE, Lopez JE. Decrease in Urinary Albumin Excretion Associated With the Normalization of Nocturnal Blood Pressure in Hypertensive Subjects. Hypertension. 2005;46:960–968. doi: 10.1161/01.HYP.0000174616.36290.fa. [DOI] [PubMed] [Google Scholar]
- 46.Hermida RC, Calvo C, Ayala DE, Fernandez JR, Covelo M, Mojon A, Lopez JE. Treatment of non-dipper hypertension with bedtime administration of valsartan. J Hypertens. 2005;23:1913–1922. doi: 10.1097/01.hjh.0000182522.21569.c5. [DOI] [PubMed] [Google Scholar]
- 47.Hermida RC, Ayala DE, Fernandez JR, Calvo C. Comparison of the Efficacy of Morning Versus Evening Administration of Telmisartan in Essential Hypertension. Hypertension. 2007;50:715–722. doi: 10.1161/HYPERTENSIONAHA.107.094235. [DOI] [PubMed] [Google Scholar]
- 48.Fagard RH, Staessen JA, Thijs L, Gasowski J, Bulpitt CJ, Clement D, de Leeuw PW, Dobovisek J, Jaaskivi M, Leonetti G, O'Brien E, Palatini P, Parati G, Rodicio JL, Vanhanen H, Webster J. Response to Antihypertensive Therapy in Older Patients With Sustained and Nonsustained Systolic Hypertension. Circulation. 2000;102:1139–1144. doi: 10.1161/01.cir.102.10.1139. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


