Abstract
BACKGROUND
Abnormal separation of right coronary artery (RCA) from the left coronary system is an extremely rare variation among coronary artery anomalies. The compressions on the anomalous route of this artery may lead to arrhythmia, chest pain, or left ventricular dysfunction or may enhance formation of atherosclerotic plaques.
CASE REPORT
Here, we have reported a patient presented with heart failure who had an anomalous atherosclerotic RCA originating from left anterior descending artery. Interestingly, neither the anomalous origin nor the atherosclerosis was the cause of the patient’s problems and she suffered from a hypertensive cardiomyopathy.
CONCLUSION
This reminds that encountering an anomaly should not solely be interpreted as the cause of cardiac disease.
Keywords: Coronary Angiography, Left Ventricular Dysfunction, Coronary Vessel Anomaly
Introduction
Approximately, 1.3% of coronary angiograms show the presence of coronary artery anomalies (CAA).1 Separation of the right coronary artery (RCA) from the left coronary system is an extremely rare variation. Presence of these anomalies mostly raises concerns about their mechanical compression in their abnormal route to their target tissues. This compression may lead to myocardial ischemia which manifests as arrhythmia, chest pain, or left ventricular (LV) dysfunction. This anomalous route would cause perturbation of blood flow within the artery, enhancing the formation of atheromatous plaques within these vessels. The atherosclerosis process in turn causes arrhythmia, chest pain, or LV dysfunction as well. Here, we have reported an anomalous atherosclerotic RCA originating from left anterior descending artery (LAD), while none of the two pathologies were the cause of the patients’ symptoms.
Case Report
A 65-year-old lady referred to our hospital with a complaint of dyspnea. She was not a smoker and her past medical history consisted of hypertension and hyperlipidemia. On admission, physical examinations revealed an elevated jugular vein pressure accompanied by pulmonary rales up to two-thirds from the base of the lung. The patient was tachypnic (respiratory rate = 28) and blood pressure was 180/100 with a normal oral temperature (36.9 °C). Her electrocardiogram showed slight T-wave inversions in the leads V2 through V6 as well as leads I and aVL. Occasional ventricular premature complexes were also present (Figure 1). The cardiac troponin level was normal. Echocardiogram of the patient showed a LV ejection fraction (LVEF) of 23% without regional wall motion abnormalities with dilated LV and atrium. Presence of moderate amounts of mitral regurgitation and moderate concentric LV hypertrophy was also noticeable.
Figure 1.
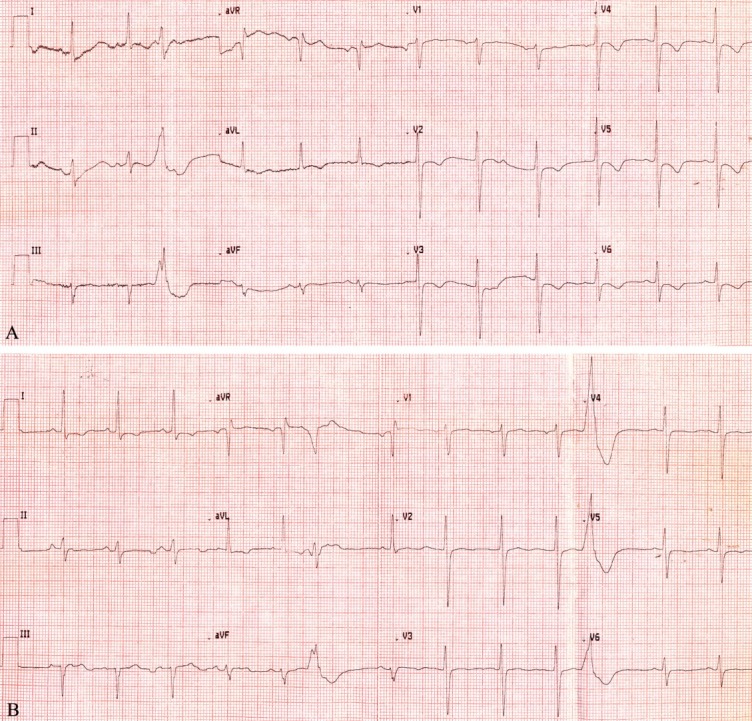
The electrocardiogram on admission showed slight T-wave inversion in the leads V2 through V6 as well as leads I and aVL with frequent ventricular premature complexes
Since there was no past medical history of heart failure, we proceed with coronary angiography to exclude ischemic causes as the basis of her disease. Cannulation of the left main coronary artery (LMCA) displayed normal courses of the LMCA, left circumflex (LCX), and LAD. An anomalous RCA as a separate large branch arose from the proximal area of LAD. The abnormally originated RCA had three significant stenoses in the proximal and distal portions (Figure 2A-C). Attempts to cannulate the RCA with the right Judkins catheter were unsuccessful. Aortography did not show the presence of another origin for a supplementary RCA from another site (Figure 2D). This was concluded to be a benign anomaly with an atherosclerotic disease. As the amount of LVEF impairment was not concordant with the epicardial coronary abnormalities, the patient was considered as a case of dilated cardiomyopathy and the patient was given long-term medical therapy for her heart failure as well as her atherosclerotic disease. At follow-up, it was observed that the patient had an asymptomatic clinical status.
Figure 2.
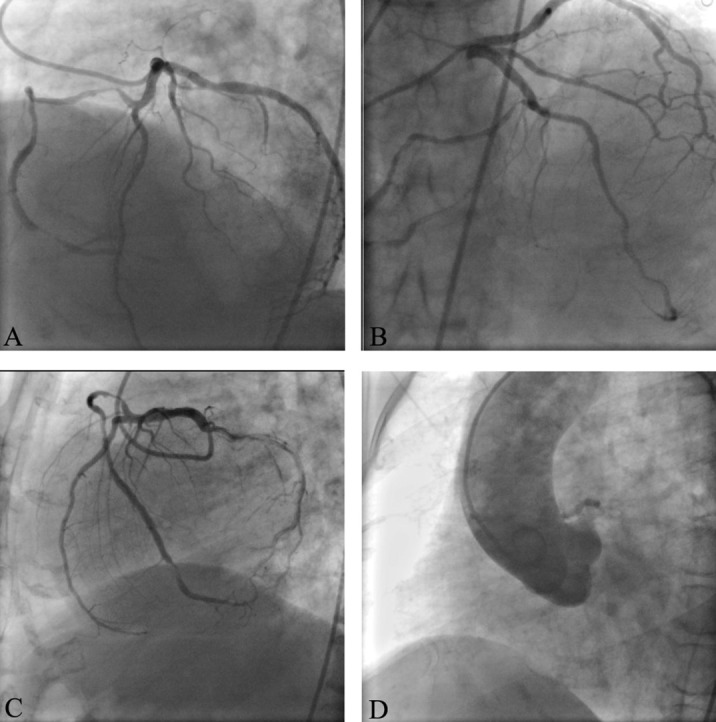
The coronary angiogram showed normal left main coronary artery, left circumflex, and left anterior descending artery (LAD); An anomalous right coronary artery (RCA) as a separate large branch arose from the proximal side of LAD; The abnormally originated RCA had three significant stenoses in the proximal and distal portions visible in the: (A) Left anterior oblique view with cranial angulation, (B) right anterior oblique view with cranial angulation, (C) Left lateral view, and (D) Aortography did not show the presence of an origin of a supplementary RCA from another site
Discussion
Disorders in the development of coronary arteries during the 3rd week of fetal development may eventually lead to CAAs. These disorders are discovered in 0.6-5.6% of diagnostic coronary angiograms, and in approximately 1% of routine autopsy examinations.1 The most common CAA is the presence of separate ostias for the LAD and LCX, seen in 0.41% of angiograms, followed by separation of the LCX from the RCA with a prevalence of 0.37%.2 An anomalous RCA originating from the left coronary (left sinus of Valsalva, the posterior sinus of Valsalva, the ascending aorta, the pulmonary artery, the LV, the LMCA, the LCX, or the LAD) system can be found in 0.1-0.9% of patients.3 Origination of RCA from the LAD is extremely rare and in most of them, anomalous RCA stems from the proximal or mid-segment of the LAD.4-7
The separation of RCA from the LAD is usually a benign disorder which does not lead to coronary mal-perfusion.8,9
The abnormal origin and course of these vessels may make them more prone to atherosclerosis which may lead to premature atherosclerotic stenosis within these vessels.10 Most patients with this pathology suffer from an exertional angina. However, other there would be other manifestations such as lethargy, hoarseness, and epigastric pain.4-6 Here, we have reported a case that summons the anomalous origin of RCA from LAD and atherosclerotic changes in that vessel. The absence of chest pain in this patient may be related to partial immobility of patient secondary to her heart failure. Furthermore; this absence of chest pain can be contributed to the well-developed collaterals from LCX supplied the distal portion of RCA as well.
In this patient, the amount of LV dysfunction could not be explained by a single inferior wall ischemia secondary to RCA disease state. So, none of the two pathologies led to her symptoms and she suffered from a third irrelevant disease, dilated cardiomyopathy, possibly due to longstanding hypertension. Hence, it is important to once encounter an anomaly, not solely interpret the concomitant cardiac problems as a consequence of that anomaly.
Acknowledgments
The authors would like to thank Dr. Nasrin Shokrpour at Center for Development of Clinical Research of Nemazee Hospital, Shiraz, Iran, for editorial assistance.
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Yamanaka O, Hobbs RE. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Cathet Cardiovasc Diagn. 1990;21(1):28–40. doi: 10.1002/ccd.1810210110. [DOI] [PubMed] [Google Scholar]
- 2.Engel HJ, Torres C, Page HL. Major variations in anatomical origin of the coronary arteries: angiographic observations in 4,250 patients without associated congenital heart disease. Cathet Cardiovasc Diagn. 1975;1(2):157–69. doi: 10.1002/ccd.1810010205. [DOI] [PubMed] [Google Scholar]
- 3.Wilkins CE, Betancourt B, Mathur VS, Massumi A, De Castro CM, Garcia E, et al. Coronary artery anomalies: a review of more than 10,000 patients from the Clayton Cardiovascular Laboratories. Tex Heart Inst J. 1988;15(3):166–73. [PMC free article] [PubMed] [Google Scholar]
- 4.Hughes MM. Anomalous origin of the right coronary artery from the left anterior descending coronary artery. Cathet Cardiovasc Diagn. 1997;42(3):308–9. doi: 10.1002/(sici)1097-0304(199711)42:3<308::aid-ccd19>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 5.Rath S, Battler A. Anomalous origin of the right coronary artery from the left anterior descending coronary artery. Cathet Cardiovasc Diagn. 1998;44(3):328–9. doi: 10.1002/(sici)1097-0304(199807)44:3<328::aid-ccd18>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 6.Khosravi Maharlooei M, Attar A, Goran A, Amuee S, Dehghan A, Monabati A. Hydatid Cyst of Ovary: A Case Report. Iran J Med Sci. 2009;34(1):76–9. [Google Scholar]
- 7.Jammula P, Gupta R, Uretsky BF. Images in cardiology: Anomalous origin of the right coronary artery from the left anterior descending artery. Heart. 2005;91(4):e30. doi: 10.1136/hrt.2004.054957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wann S, Schuchard G. Images in clinical medicine. Anomalous origin of the right coronary artery. N Engl J Med. 2006;355(9):e8. doi: 10.1056/NEJMicm050051. [DOI] [PubMed] [Google Scholar]
- 9.Kamran M, Bogal M. Anomalous right coronary artery originating from the left anterior descending artery. J Invasive Cardiol. 2006;18(8):E221–E222. [PubMed] [Google Scholar]
- 10.Taylor AJ, Rogan KM, Virmani R. Sudden cardiac death associated with isolated congenital coronary artery anomalies. J Am Coll Cardiol. 1992;20(3):640–7. doi: 10.1016/0735-1097(92)90019-j. [DOI] [PubMed] [Google Scholar]


