Abstract
Objective
Although nursing home (NH) residents make up a large and growing proportion of Americans with diabetes mellitus, little is known about how glucose-lowering medications are used in this population. We sought to examine glucose-lowering medication use in Veterans Affairs (VA) NH residents with diabetes between 2005–2011.
Research Design and Methods
Retrospective cohort study, utilizing linked laboratory, pharmacy, administrative and NH Minimum Dataset (MDS) 2.0 databases in 123 VA NHs. A total of 9,431 long-stay (>90 days) VA NH residents over age 65 followed for 52,313 person-quarters. We identified receipt of glucose lowering medications including insulin, metformin, sulfonylureas, thiazolidinediones and others (alpha-glucosidase inhibitors, meglitinides, glucagon like peptide-1 analogs, dipeptidyl peptidase-4 inhibitors and amylin analogues) per quarter.
Results
The rates of sulfonylurea use in long-stay NH residents dropped dramatically from 24% in 2005 to 12% in 2011 (p<0.001), driven in large part by the dramatic decrease in glyburide use (10% to 2%, p<0.001). There was sharp drop in thiazolidinedione use in 2007 (4% to <1%, p<0.001). Metformin use was stable, ranging between 7% to 9% (p=0.24). Insulin use increased slightly from 30% to 32% (p<0.001). Use of other classes of glucose-lowering medications was stable (p=0.22) and low, remaining below 1.3%.
Conclusions and Relevance
Between 2005 and 2011, there were dramatic declines in use of sulfonylureas and thiazolidinediones in VA NH residents, suggesting that prescribing practices can be quickly changed in this setting.
Keywords: Nursing Home, diabetes, glucose-lowering, insulin, metformin
INTRODUCTION
Frail nursing home (NH) residents make up a large, growing and understudied segment of the diabetes population in the US.1 The most recent National Nursing Home Survey suggests that one in four nursing home residents aged 65 and older have a diagnosis of diabetes.2 Further, projections estimate that between 2005–2050, the prevalence of diabetes will skyrocket 449% among those older than 75 years.3,4 However, surprisingly little is known about current diabetes care practices in NHs,5,6 due in part to the fact that few national pharmacoepidemiologic data resources exist for NHs.
To improve prescribing practices in NH residents with diabetes, data are needed on recent prescribing practices as well as how prescribing patterns have evolved over time. Recent care practices provide baseline data and a benchmark for any future improvement interventions. Examining prescribing patterns over time provide insights into how prescribing patterns will evolve into the future and how we can shape these trends to promote high-quality care.
The last decade has been an exciting, dynamic time for glycemic control care practices. Initially, data suggested that near-normal glycemic control may lead to improved outcomes, leading many guidelines to recommend tighter glycemic control.7 Then, thiazolidinediones were found to increase cardiovascular risks, leading to a “black box” warning in 2007.8–10 In 2008, the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study showed increased all-cause mortality for patients randomized to more intensive glycemic control,11 diminishing enthusiasm for tight glycemic control, especially for older adults.12 Guidelines and quality indicators have serially incorporated these and other new study results, leading to a shifting landscape of diabetes care practices.2,13–15
Thus, we sought to leverage the national pharmacoepidemiologic data available for Veterans Affairs (VA) NHs to describe glycemic medication prescribing practices between 2005 – 2011. The objective of this study is to conduct exploratory research that will provide data on recent prescribing practices that will inform future efforts to improve glucose lowering medication prescribing in NHs.
METHODS
Study Population
We examined long stay patients age 65 or older with diabetes who were admitted to VA NHs (known as Community Living Centers or VA CLCs) between January 1st, 2005 and September 30th, 2011. We defined long stay CLC residents as veterans staying in a CLC for 90+ days (n=40,025), identified through the National Patient Care Database extended care files which provides admission and discharge dates. Using the American Diabetes Association (ADA) criteria for diagnosing diabetes mellitus,15 we used administrative data to identify long-stay CLC residents with diabetes if they had a Hemoglobin A1c (HbA1c) ≥ 6.5% using the VA Laboratory Results (LAR) file, or if they had HbA1c<6.5% but were on glucose reducing medications at the time of the test. This resulted in our final analytic cohort of 9,431 residents.
Measures: Non-insulin Medications
Our primary study question was to determine the rates of use of glucose lowering medications over time in long-term CLC patients with diabetes. We examined the medication use in each of the 27 quarters between January 1st, 2005 and September 30th, 2011.
For non-insulin glucose lowering medications, we utilized the Pharmacy Benefits Management (PBM) database which contains information on medications dispensed to patients in the VA system.16 For each medication, the PBM database included start date, amount dispensed, drug name, and instructions for use, allowing us to estimate the end date for each medication. Non-insulin medications were divided into four categories: (1) Metformin; (2) Sulfonylureas; (3) thiazolidinediones or TZDs; (4) Other medications (i.e., alpha-glucosidase inhibitor, meglitinides, glucagon-like peptide-1 analogs, dipeptidyl peptidase-4 inhibitors, amylin analogs). Sulfonylureas were further divided into 2a) Glipizide and 2b) Glyburide. A medication was considered as used in a quarter if it was used at any day during that quarter. The full list of medications can be found in the Appendix.
Measures: Insulin
We categorized pharmacy dispensed insulin into basal or long-acting insulin (i.e. glargine or NPH) and bolus or short-acting insulin (i.e. Regular or Aspart).
We were unable to rely solely on the PBM database for insulin since it does not contain information on ward stock medications. Ward stock medications such as insulin could be given to patients without a specific pharmacy dispensing action tied to an individual patient. Thus, if insulin was recorded in the PBM database, it was dispensed by pharmacy for a specific resident; however, if insulin was not recorded in the PBM database, it may still have been dispensed to that resident as a ward stock medication.
Thus, we estimated the rates of insulin use by combining 1) rates of dispensed insulin from PBM data and 2) estimated rates of ward stock insulin use using multiple imputation with additional information including data from the Minimum Dataset (MDS) 2.0. The MDS is collected on all VA NH residents through quarterly surveys usually filled out by a nurse trained as an MDS data abstractor.17 One MDS data element asks, “Record the number of days injections of any type received in the past 7 days.” VA NH residents who had no reported injection use were categorized as not having used insulin.
To estimate the rates of ward stock insulin use, we used multiple imputation prediction models using age, comorbidities, use of glucose lowering medications (other than insulin) and VA station number to estimate the likelihood of insulin use. 18,19 Specifically, we developed our models using NH residents with pharmacy dispensed insulin as insulin users and NH residents with MDS data reporting no injections as insulin non-users. Then we applied this model to NH residents who had a report of recent injection but no pharmacy record of insulin, allowing us to estimate the likelihood of insulin use for these NH residents. Then we repeated the process with bootstrap datasets to obtain estimates of uncertainty of our predictions. Compared to alternative methods, multiple imputation appears to produce less biased prevalence estimates and standard errors.19
To explore the validity of our methodology to estimate insulin use, we examined the rates of injections in NH residents with diabetes and without diabetes. We found that the injection use rate was much higher among residents with diabetes (54% vs 18%, p<0.001), suggesting that MDS injection data included insulin use. The discrimination of our insulin use prediction model was excellent with a c-statistic of 0.81.
Measures: Comorbidities and Function
Presence of comorbid conditions including history of hypoglycemia was determined using ICD9 codes from the outpatient and inpatient visits up to one year prior to admission to CLC. Activities of Daily Living (ADL) score and weight loss data were obtained from the MDS 2.0 data. Weight loss was determined using the question, “Weight loss: 5% or more in last 30 days or 10% or more in last 180 days.” The MDS-ADL score was calculated using 7 activities (bed mobility, transfer, locomotion, dressing, eating, toilet use and personal hygiene) assessed on a five level scale (independent, supervision, limited assistance, extensive assistance and total dependence). The MDS-ADL score in each assessment is between 0 and 28 (higher scores indicating greater ADL limitations)20 and has been successfully used in previous studies.21
Statistical Analysis
We used descriptive statistics to describe basic characteristics of patients in our sample. The prevalence of use of glucose lowering medications over time was examined graphically by plotting the rates of use in each of the 27 quarters in our study period. Using linear regression, we determined the best fit line through the data. We tested whether the slope of each line differed from zero to determine whether rates of medications were stable, increasing or decreasing during our study period.
All the analyses were done using SAS software, version 9.4 (SAS institute, Cary, North Carolina) and STATA, version 13.1 (College Station, TX). The Committee on Human Research at the University of California, San Francisco and the Research and Development Committee of the San Francisco VA Medical Center reviewed and approved this study.
RESULTS
Characteristics of Study Cohort
Our study population consisted of 9,431 long term residents in VA CLCs with diabetes mellitus, followed for 52,313 person-quarters. Baseline characteristics for study subjects are presented in Table 1. Mean age of patients was 78 years with 67% over the age of 75 and they were mostly male (98%). Sixty seven percent of them were hospitalized in the six months prior to entering the CLC. Most patients were diagnosed with hypertension (87%) and coronary artery disease (54%). Twenty-six percent of patients had a diagnosis of hypoglycemia. Across the study period, 62% of our patients needed assistance for transferring and 32% needed assistance for eating.
Table 1.
Selected Characteristics of Study Cohort
| Patient Characteristics | Total number of patients (N= 9431) |
|---|---|
| Age (SD) | 78 ± 7 |
| 65 – 74 | 33 |
| 75 – 84 | 48 |
| ≥85 | 19 |
| Male gender | 98% |
| Hospitalization in past 180 days | 67% |
| Diagnoses | |
| Hypertension | 87% |
| Coronary Artery Disease | 54% |
| End Stage Renal Disease | 6% |
| Cerebrovascular disease | 39% |
| Dementia | 24% |
| Hypoglvcemia | 26% |
| ≥5% Weight Loss in 30 days or ≥10% weight loss in 180 days | 17% |
| MDS-ADL score (SD)* | 13 ± 9 |
| Needs assistance for transferring | 62% |
| Needs assistance for locomotion | 44% |
| Needs assistance for eating | 32% |
| Needs assistance for dressing | 78% |
| Needs assistance for toilet use | 72% |
| Use of Injectable Medications | 54% |
| Use of oral glucose lowering medication | 23% |
| Use of insulin | 31% |
| Hemoglobin A1c | |
| <7 | 60% |
| 7–7.9 | 24% |
| 8–8.9 | 10% |
| >=9 | 6% |
MDS ADL score is obtained by summing 7 activities (bed mobility, transfer, locomotion, dressing, eating, toilet use and personal hygiene) assessed on a five level scale (0 points for independent, 1 point for supervision, 2 points for limited assistance, 3 points for extensive assistance and 4 points for total dependence).
Across the study period 23% used oral glucose lowering medications and 31% used insulin. Sixty percent of nursing home residents with diabetes had HbA1c <7%. The 32% of patients who needed assistance eating were similar to our overall cohort, with 63% with a HbA1c <7% (compared to 60% in the overall cohort) and 28% receiving insulin (compared to 31% in the overall cohort).
Rates of Use of Non-Insulin Glucose Lowering Medications
Figure 1 shows the use of non-insulin glucose lowering medications by pharmacologic class over the study period in VA nursing home residents. In the first quarter of 2005, 24% of patients with diabetes were prescribed sulfonylureas, 9% were prescribed Metformin, 4% were prescribed thiazolidinediones and a small percentage (<1%) was prescribed other glucose lowering oral medications. Between first quarter of 2005 and third quarter of 2011, the proportion of patients prescribed sulfonylureas decreased dramatically from 24% to 12% (p<0.001). Over the same time period, the use of metformin did not change significantly (p=0.25). There was a sharp statistically significant decrease in the proportion of patients prescribed thiazolidinediones in 2007 (p<0.001). The use of other glucose-lowering medications were stable (p=0.22) and low, remaining below 1.3%.
Figure 1.
Use of Non-Insulin Glucose Lowering Medications for VA Nursing Home Residents, 2005–2011
Rates of Sulfonylurea Use
Glipizide and Glyburide represented the vast majority of sulfonylureas used in VA nursing home residents. (Figure 2) While both glipizide and glyburide use declined, glyburide use declined dramatically, falling from 10% in 2005 to 2% in 2011. In contrast, glipizide use decreased more modestly, from 14% in 2005 to 10% in 2011.
Figure 2.
Use of sulfonylurea medications for VA Nursing home residents, 2005–2011
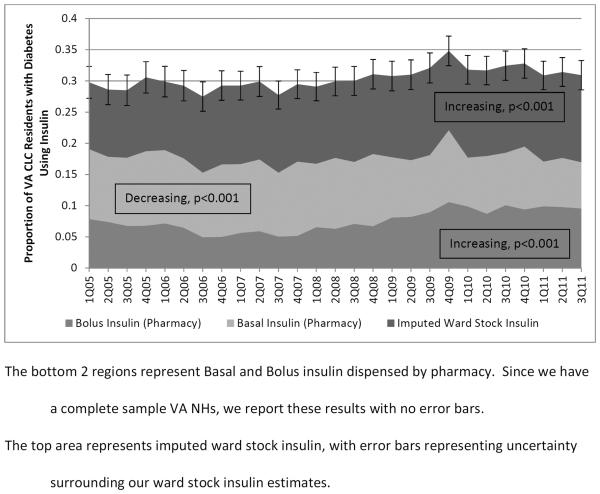
Rates of Insulin Use
The rates of dispensed basal insulin decreased from 11% in 2005 to 8% in 2011 (p<0.001). (Figure 3) In contrast, the rates of dispensed bolus insulin increased from 7% in 2005 to 10% in 2011 (p<0.001). The combined rate of all dispensed insulin did not change from 2005 to 2011 (p=0.50) and ranged from 15% to 22%. The rates of imputed insulin increased during our study period (p<0.001) and the rates of total insulin use (basal, bolus and imputed) increased slightly during our study period, from a minimum of 27% in 2006 to a maximum of 35% in 2009 (p<0.001).
Figure 3.
Rates of Insulin Use in VA nursing home residents, 2005–2011
We also examined the trends of MDS-reported injections among residents with and without diabetes. We found that while injection rates increased slightly among residents without diabetes (17% in 2005 vs 18% in 2011, p=0.04), injection rates increased more among residents with diabetes (51% in 2005 vs 56% in 2011, p<0.001), consistent with increasing insulin use.
DISCUSSION
In a national sample of VA nursing home residents between 2005 and 2011, we found evidence of substantial changes in the rates of use of different glucose lowering medications. As expected, thiazolidinedione use decreased dramatically in 2007, coinciding with the FDA black box warning regarding cardiovascular adverse events. Sulfonylurea use declined steady by almost half, driven mostly by declines in the use of glyburide. Further, we found evidence for modest increase in insulin use.
Our study on prescribing trends of glucose lowering medications adds to the previous published studies which have focused on younger, ambulatory patients. Specifically, Desai and colleagues focused on younger patients (mean age 58) using a national pharmacy benefits manager (2006 – 2008) and found decreasing rates of sulfonylurea and thiazolidinedione initiation with increasing rates of metformin initiation.22 Our study on older, NH residents also found decreasing rates of sulfonylurea and thiazolidinedione use. However, we found that metformin use in VA NH's was stable between 2005 – 2011. This may be due to the fact that the VA NH population is older with a high prevalence of renal insufficiency, limiting the proportion of patients who can receive metformin safely.
Although glyburide was added to the Beers list as a potentially inappropriate medication in 2012,23 the evidence of increased hypoglycemia risk with glyburide has been mounting since 1996.24,25 In 2006, a consensus statement from the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) noted that “longer acting agents (e.g. glyburide) are more likely to cause hypoglycemia than glipizide.”26 In 2009, an updated consensus statement from the ADA and EASD stated that glipizide is “preferable” over glyburide due to the “substantially” lower risk of hypoglycemia.27 Between 2007 and 2009, the national VA Pharmacy service released a series of bulletins, advising providers to avoid glyburide in older patients, especially in older patients with renal insufficiency.27,28 Our study shows that all of these efforts were successful in dramatically reducing the rates of glyburide use in VA nursing homes. Future studies should examine whether non-VA nursing homes experienced similar declines in sulfonylurea and glyburide use.
While glyburide use dropped dramatically, glipizide use also declined, leading to a steep decline in overall sulfonylurea use. This may be due to an increasing recognition of the potential harms of sulfonylureas. Along with the well-known risks of hypoglycemia and weight gain, sulfonylureas have been implicated in an increase in cardiovascular mortality. This was first noted in the University Group Diabetes Study in 1976,29 but has since been observed in several observational studies.30–32 In 2013, these concerns ultimately led the American Association of Clinical Endocrinology to issue the controversial recommendation that newer agents such as GLP-1 Analogs, DPP-4 Inhibitors rather than sulfonylureas are preferred in most situations.33,34 Thus, the steep drop in sulfonylurea use that we observed may reflect a growing recognition by NH providers that sulfonylureas may be associated with substantial risks.
Driven mostly by the decline in sulfonylurea use, we observed a trend of lower rates of glucose lowering medication use during our study period. Although rates of insulin use increased slightly, it is more than offset by the decreases in sulfonylureas and thiazolidinediones. One possible explanation is that patients may have been on higher doses of insulin. For example, many patients who were on thiazolidinediones and insulin in 2006 may be on higher doses of just insulin in 2010. A second possible explanation is that Hemoglobin A1c tests may have been ordered more widely near the end of our study period, resulting in the identification of many VA NH residents with mild diabetes. This would lead to decreasing average disease severity in our cohort over time, resulting in the less medication use that we observed. If confirmed, this finding could represent an unintended consequence of quality indicators, where clinicians diagnose generously to increase the rates of their patients with excellent control.35
Few studies have examined the rates of insulin use. Li and colleagues utilized the Behavioral Risk Factor Surveillance System survey to show that between 2001 and 2007, the insulin use rates were stable between 20.2% and 22.5% in patients with type 2 diabetes (age >40).36 Using the National Health Interview Survey, the Centers for Disease Control and Prevention reports that 29% of the US adults over age 18 with diabetes used insulin in 2005 with 31% were using insulin by 2011.37 Our study adds to the evidence base by focusing on older NH residents as well as differentiating basal and bolus insulin use. We found that while basal insulin use declined, this decrease was offset by an increase in bolus insulin use. Further, the rates and trends of insulin use in NH residents with diabetes in our study were similar to younger, ambulatory patients with diabetes. Specifically, we found that the rates of insulin use in NH residents (30 – 32%, 2005 – 2011) were similar in both magnitude and trend compared to non-NH residents (29 – 31%, 2005 – 2011).
Our results should be interpreted in light of the strengths and limitations of our study. Strengths of our study include a national sample in the largest vertically integrated health system in the US. Limitations include our nearly all male population; since most NH residents are female, it is unclear whether our results would differ for predominantly female NH populations. Second, we did not have complete data on insulin use. Future research should focus on insulin use rates in NH populations to confirm our findings.
In summary, we examined the rates of use of glucose lowering medications in all VA NH's nationally between 2005 and 2011. We found that while rates of use of sulfonylureas (especially glyburide) and thiazolidinediones dropped substantially, rates of insulin use increased slightly.
ACKNOWLEDGEMENTS
Funding sources:
This work was supported with resources and the use of facilities at the San Francisco VA Medical center.
SJL's effort was supported by the Beeson Career Development program from the NIA (K23AG040779) and the American Federation of Aging Research.
MAS's effort was supported by NHLBI (R01HL111032).
Appendix.
List of Glucose Lowering Medications
| Medication Type | Medications Included in Class |
|---|---|
| Metformin | Metformin |
| Sulfonylureas | Glimepiride, Glyburide, Chlorpropamide, Glipizide, Tolazamide, Tolbutamide |
| TZD | Pioglitazone, Rosiglitazone |
| Others | Miglitol, Acarbose, Nateglinide, Repaglinide, Exenatide, Liraglutide, Sitagliptin, Linagliptin, Saxagliptin, Pramlintide |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author contributions:
SJL conceived the study and drafted the manuscript.
IS analyzed the data and provided critical revisions.
CB and KM helped obtain data and provided critical revisions.
MAS supervised the study and provided critical revisions.
Data access and Responsibility Statement:
SJL, IS and MAS had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Authors have no conflicts of interests to disclose.
Previous Presentations:
This work has not been previously presented
REFERENCES
- 1.Zhang X, Decker FH, Luo H, et al. Trends in the prevalence and comorbidities of diabetes mellitus in nursing home residents in the United States: 1995–2004. Journal of the American Geriatrics Society. 2010;58:724–30. doi: 10.1111/j.1532-5415.2010.02786.x. [DOI] [PubMed] [Google Scholar]
- 2.Resnick HE, Heineman J, Stone R, Shorr RI. Diabetes in U.S. nursing homes, 2004. Diabetes care. 2008;31:287–8. doi: 10.2337/dc07-1425. [DOI] [PubMed] [Google Scholar]
- 3.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Population health metrics. 2010;8:29. doi: 10.1186/1478-7954-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang ES, Laiteerapong N, Liu JY, John PM, Moffet HH, Karter AJ. Rates of complications and mortality in older patients with diabetes mellitus: the diabetes and aging study. JAMA internal medicine. 2014;174:251–8. doi: 10.1001/jamainternmed.2013.12956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zarowitz BJ, Tangalos EG, Hollenack K, O'Shea T. The application of evidence-based principles of care in older persons (issue 3): management of diabetes mellitus. Journal of the American Medical Directors Association. 2006;7:234–40. doi: 10.1016/j.jamda.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Feldman SM, Rosen R, DeStasio J. Status of diabetes management in the nursing home setting in 2008: a retrospective chart review and epidemiology study of diabetic nursing home residents and nursing home initiatives in diabetes management. Journal of the American Medical Directors Association. 2009;10:354–60. doi: 10.1016/j.jamda.2009.02.010. [DOI] [PubMed] [Google Scholar]
- 7.American Diabetes A Standards of medical care in diabetes--2007. Diabetes care. 2007;30(Suppl 1):S4–S41. doi: 10.2337/dc07-S004. [DOI] [PubMed] [Google Scholar]
- 8.Woodcock J, Sharfstein JM, Hamburg M. Regulatory action on rosiglitazone by the U.S. Food and Drug Administration. The New England journal of medicine. 2010;363:1489–91. doi: 10.1056/NEJMp1010788. [DOI] [PubMed] [Google Scholar]
- 9.Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. The New England journal of medicine. 2007;356:2457–71. doi: 10.1056/NEJMoa072761. [DOI] [PubMed] [Google Scholar]
- 10.Tanne JH. FDA places “black box” warning on antidiabetes drugs. Bmj. 2007;334:1237. doi: 10.1136/bmj.39244.394456.DB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Action to Control Cardiovascular Risk in Diabetes Study G. Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. The New England journal of medicine. 2008;358:2545–59. doi: 10.1056/NEJMoa0802743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee SJ, Eng C. Goals of glycemic control in frail older patients with diabetes. JAMA. 2011;305:1350–1. doi: 10.1001/jama.2011.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetes care. 2012;35:1364–79. doi: 10.2337/dc12-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes care. 2012;35:2650–64. doi: 10.2337/dc12-1801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.American Diabetes A Standards of medical care in diabetes--2014. Diabetes care. 2014;37(Suppl 1):S14–80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 16.Smith MW, Joseph GJ. Pharmacy data in the VA health care system. Medical care research and review : MCRR. 2003;60:92S–123S. doi: 10.1177/1077558703256726. [DOI] [PubMed] [Google Scholar]
- 17.Dellefield ME. The work of the RN Minimum Data Set coordinator in its organizational context. Research in gerontological nursing. 2008;1:42–51. doi: 10.3928/19404921-20080101-04. [DOI] [PubMed] [Google Scholar]
- 18.Schafer JL. Multiple imputation: a primer. Statistical methods in medical research. 1999;8:3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- 19.White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Statistics in medicine. 2011;30:377–99. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 20.Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. The journals of gerontology Series A, Biological sciences and medical sciences. 1999;54:M546–53. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- 21.Kurella Tamura M, Covinsky KE, Chertow GM, Yaffe K, Landefeld CS, McCulloch CE. Functional status of elderly adults before and after initiation of dialysis. The New England journal of medicine. 2009;361:1539–47. doi: 10.1056/NEJMoa0904655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Desai NR, Shrank WH, Fischer MA, et al. Patterns of medication initiation in newly diagnosed diabetes mellitus: quality and cost implications. The American journal of medicine. 2012;125:302, e1–7. doi: 10.1016/j.amjmed.2011.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American Geriatrics Society Beers Criteria Update Expert P American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. Journal of the American Geriatrics Society. 2012;60:616–31. doi: 10.1111/j.1532-5415.2012.03923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Staa T, Abenhaim L, Monette J. Rates of hypoglycemia in users of sulfonylureas. Journal of clinical epidemiology. 1997;50:735–41. doi: 10.1016/s0895-4356(97)00024-3. [DOI] [PubMed] [Google Scholar]
- 25.Shorr RI, Ray WA, Daugherty JR, Griffin MR. Individual sulfonylureas and serious hypoglycemia in older people. Journal of the American Geriatrics Society. 1996;44:751–5. doi: 10.1111/j.1532-5415.1996.tb03729.x. [DOI] [PubMed] [Google Scholar]
- 26.Nathan DM, Buse JB, Davidson MB, et al. Management of hyperglycemia in type 2 diabetes: A consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes care. 2006;29:1963–72. doi: 10.2337/dc06-9912. [DOI] [PubMed] [Google Scholar]
- 27.Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes care. 2009;32:193–203. doi: 10.2337/dc08-9025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aspinall SL, Zhao X, Good CB, et al. Intervention to decrease glyburide use in elderly patients with renal insufficiency. The American journal of geriatric pharmacotherapy. 2011;9:58–68. doi: 10.1016/j.amjopharm.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 29.Miller M, Knatterud GL, Hawkins BS, Newberry WB., Jr A study of the effects of hypoglycemia agents on vascular complications in patients with adult-onset diabetes. VI. Supplementary report on nonfatal events in patients treated with tolbutamide. Diabetes. 1976;25:1129–53. doi: 10.2337/diab.25.12.1129. [DOI] [PubMed] [Google Scholar]
- 30.Garratt KN, Brady PA, Hassinger NL, Grill DE, Terzic A, Holmes DR., Jr Sulfonylurea drugs increase early mortality in patients with diabetes mellitus after direct angioplasty for acute myocardial infarction. Journal of the American College of Cardiology. 1999;33:119–24. doi: 10.1016/s0735-1097(98)00557-9. [DOI] [PubMed] [Google Scholar]
- 31.Simpson SH, Majumdar SR, Tsuyuki RT, Eurich DT, Johnson JA. Dose-response relation between sulfonylurea drugs and mortality in type 2 diabetes mellitus: a population-based cohort study. CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne. 2006;174:169–74. doi: 10.1503/cmaj.050748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schramm TK, Gislason GH, Vaag A, et al. Mortality and cardiovascular risk associated with different insulin secretagogues compared with metformin in type 2 diabetes, with or without a previous myocardial infarction: a nationwide study. European heart journal. 2011;32:1900–8. doi: 10.1093/eurheartj/ehr077. [DOI] [PubMed] [Google Scholar]
- 33.Garber AJ, Abrahamson MJ, Barzilay JI, et al. American Association of Clinical Endocrinologists' comprehensive diabetes management algorithm 2013 consensus statement--executive summary. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2013;19:536–57. doi: 10.4158/EP13176.CS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gionfriddo MR, McCoy RG, Lipska KJ. The 2013 American Association of Clinical Endocrinologists' diabetes mellitus management recommendations: improvements needed. JAMA internal medicine. 2014;174:179–80. doi: 10.1001/jamainternmed.2013.12971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hayward RA, Kent DM. 6 EZ steps to improving your performance: (or how to make P4P pay 4U!) JAMA. 2008;300:255–6. doi: 10.1001/jama.2008.69. [DOI] [PubMed] [Google Scholar]
- 36.Li C, Ford ES, Zhao G, Tsai J, Balluz LS, Giles WH. Trends of insulin use among US adults with type 2 diabetes: the Behavioral Risk Factor Surveillance System, 1995–2007. Journal of diabetes and its complications. 2012;26:17–22. doi: 10.1016/j.jdiacomp.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 37.Prevention CfDCa . Age-Adjusted Percentage of Adults with Diabetes Using Diabetes Medication, by Type of Medication, United States, 1997–2011. 2011. [Google Scholar]