Abstract
The significant rise and projected trends in the incidence of type 2 diabetes argue for a concerted effort on prevention. The strongest currently available evidence for diabetes prevention involves people at high risk for type 2 diabetes (i.e., those with prediabetes). Randomized, controlled trials and translation studies have demonstrated that type 2 diabetes can be prevented or delayed through a structured lifestyle intervention that can be delivered cost-effectively in a variety of settings. For the first time in the United States, a coordinated, focused effort is underway to bring this effective and cost-conscious lifestyle intervention to communities across the country to ultimately reduce the incidence of type 2 diabetes.
Introduction
Diabetes affects almost 26 million Americans (1). Currently one in nine U.S. adults has diabetes and the Centers for Disease Control and Prevention (CDC) estimates that as many as one in three could be affected by 2050 if current trends continue (2). As many as 79 million people in the U.S. have prediabetes (1), representing more than one third of adult Americans and half of all adults aged 65 years and older. Those with prediabetes are 10 to 15 times more likely to develop type 2 diabetes and are at higher risk for cardiovascular disease than those without prediabetes (3). Addressing type 2 diabetes requires action directed toward those who have prediabetes.
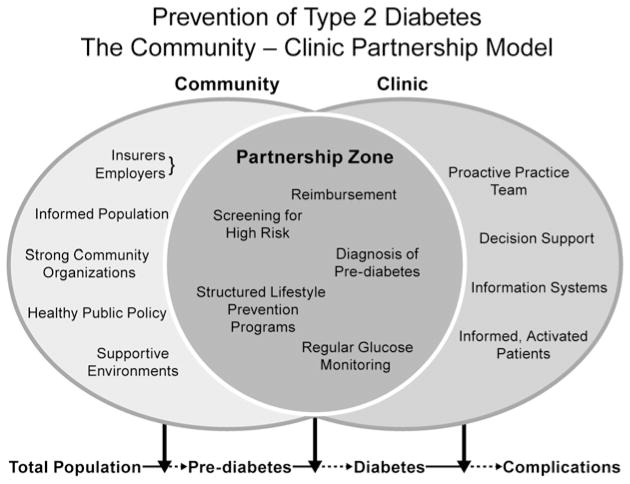
Preventing type 2 diabetes is a public health challenge that necessitates complementary and shared public health and clinical approaches that achieve more in combination than each can accomplish individually. The clinical sector must be involved in: assessing patient risk for type 2 diabetes; discussing risk status with patients and their support network; recommending that high-risk patients participate in effective, community-based structured lifestyle programs; providing medical nutrition therapy (MNT); and, where necessary, prescribing medications for those at risk for and diagnosed with type 2 diabetes. The public health sector has a significant role in: monitoring diabetes risk, mobilizing partnerships to reduce new cases of diabetes, linking people to proven diabetes prevention services, assuring quality of prevention programs, and developing policies that support individual risk reduction and community change that encourage healthy behaviors. Figure 1 shows this concept of public health and clinical approaches within the community and clinic to illustrate how they can work synergistically for prevention of type 2 diabetes. Interventions undertaken by any sector should be based on evidence from a variety of study designs so that prevention can move from proof-of-concept to improvement in population-level health outcomes.
Figure 1.
Prevention of type 2 diabetes: the community-clinic model. Elements in the clinical component are adapted from the Chronic Care Model, MacColl Institute for Healthcare Innovation. The elements listed in the figure are not intended to be all-inclusive but to provide information on the types of elements contributed by each sector and shared across sectors. Provided by Centers for Disease Control and Prevention, Division of Diabetes Translation.
Research on Lifestyle Interventions to Prevent/Delay Type 2 Diabetes
The Diabetes Prevention Program (DPP) is the largest efficacy trial providing evidence that type 2 diabetes can be prevented or delayed in those at high risk (4). This research study, led by the National Institutes of Health, is a landmark trial. It showed that persons with impaired glucose tolerance who lost 5% to 7% of their body weight and got 150 minutes of moderate physical activity per week through a lifestyle change program reduced their chances of developing type 2 diabetes by 58%. Since completion of the original 3-year DPP study, most of the participants have been followed for more than a decade in the Diabetes Prevention Program Outcomes Study (DDPOS) (5). When outcome study results were reported in 2009, the incidences of type 2 diabetes in the former metformin and placebo groups equaled those in the former lifestyle group, but the cumulative incidence of type 2 diabetes remained lowest in the lifestyle group. Thus, prevention or delay of type 2 diabetes with lifestyle intervention can persist for at least 10 years. Although it is uncertain why the incidences of type 2 diabetes in the metformin and placebo groups fell during the DPPOS, it is important to note that after the DPP study period, all participants were offered the lifestyle intervention because it would have been unethical to withhold it from the metformin and placebo groups.
The DPP provided invaluable information, but it included elements that can be economically challenging to maintain when attempting to achieve the same results in the broader prediabetes population. The DPP was resource-intensive. For example, the lifestyle intervention included one-on-one “core” sessions delivered by highly credentialed research staff. These sessions were followed by twice-monthly in-person “maintenance” sessions and telephone contact between sessions. In addition, participants were given several lifestyle modification tools, including access to exercise facilities and meal replacements at no cost to the participants. The cost to deliver the DPP lifestyle intervention in the first year was $1,399 per participant. Therefore, a major focus of subsequent research for type 2 diabetes prevention has been how to best use limited resources to deliver the lifestyle intervention, while ensuring that weight loss is sufficient to decrease the future incidence of type 2 diabetes significantly.
Several published research studies conducted in real-world settings have implemented modified versions of the lifestyle intervention used in the DPP research study. Ali and associates (6) conducted a systematic review and meta-analysis of 28 US -based investigations that adapted the DPP lifestyle intervention in real-world settings at lower cost. Because the DPP study established that weight loss was the single most important factor in reducing the incidence of type 2 diabetes, Ali and associates examined the weight loss achieved in these translation studies. They also evaluated program characteristics that influenced weight loss, including number of core sessions and type of intervention staff.
The studies in the analysis included four randomized, controlled trials; two cluster-randomized, controlled trials; 20 single-group pre-post studies; and two nonrandomized, controlled studies. The studies took place in diverse settings, including community centers, recreation centers, faith-based organizations, health care facilities, and via electronic media (four studies). A total of 3,797 participants were enrolled in interventions, and 2,916 participants who had complete follow-up data were included in the analysis. Loss to follow-up of study participants during the evaluation period ranged from 0% to 49%. The typical study participant was a non-Hispanic white female who was 55.1 years old and had a body mass index of 34.
Mean weight change across all studies was −3.99% at 12-month follow-up evaluation. Change in weight was similar regardless of whether the intervention was delivered by medical and allied health professionals or lay community personnel. The number of core sessions attended was strongly correlated with the number of core sessions offered. Every core session attended was associated with additional weight change of −0.26%. Qualitative information from studies included in the analysis indicated that attrition was not related to program length but rather to the effectiveness of behavioral modification techniques and participants’ perceptions of how likely they were to develop type 2 diabetes.
Further research in diabetes prevention is required. Among the topics that need to be addressed are: the underlying pathology of obesity, what interventions are effective for those at lower risk to prevent prediabetes, and what policies and changes to a community environment are effective for improving the health of the entire population. While these and other questions are tackled, it is important to implement currently known information in diabetes prevention to decrease the current and future diabetes burden.
The National Diabetes Prevention Program
Moving diabetes prevention from randomized, controlled trials to translation studies and on to implementation in communities is a daunting task. A concerted focus on building the infrastructure for and delivery of the adapted DPP lifestyle change program had not been undertaken in the U.S. until Congress authorized the CDC to establish and lead the National Diabetes Prevention Program (National DPP). The National DPP represents an approach to increase low-cost interventions based on the DPP in communities across America. Its foundation is a results-driven partnership that includes community-based organizations, health insurers, employers, health care systems, academia, and government agencies. The strategic approach to the National DPP has four core elements (Fig. 2). The following description of the core elements includes examples of progress in each but should not be interpreted as comprehensive because the National DPP continues to evolve and expand. Further information and developments related to the National DPP are available at www.cdc.gov/diabetes/prevention.
Figure 2.
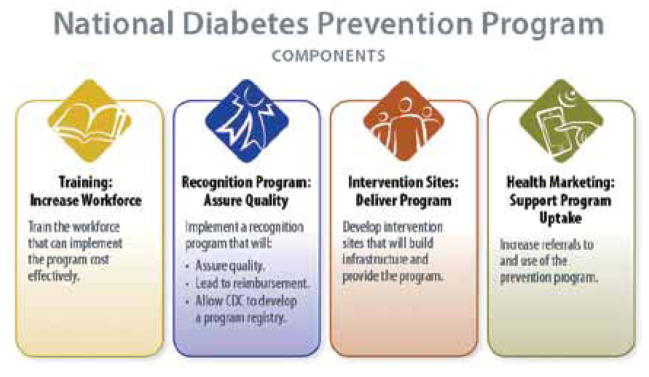
Summary of the four core elements of the National Diabetes Prevention Program. Provided by the Centers for Disease Control and Prevention, Division of Diabetes Translation.
Training
A trained workforce is required to deliver the lifestyle change program cost effectively, and the number of people with prediabetes requires that the workforce continue to expand to meet the demand. As demonstrated in the meta-analysis by Ali and associates (6), health professionals and lay community workers can effectively deliver the lifestyle change program. In response to this training need, the CDC established the Diabetes Training and Technical Assistance Center (DTTAC) at Emory University (see DTTAC article in this issue). Other organizations conduct training and should be assessed to ascertain that their level of training allows an organization’s lifestyle change program to meet CDC recognition program standards (below). In addition to training, DTTAC also provides a learning community for trainers.
Recognition Program
The CDC Diabetes Prevention Recognition Program (DPRP) is a key component of the National DPP. The objectives of the DPRP are to: 1) assure the quality, consistency, and broad dissemination of the lifestyle change program for people at high risk for type 2 diabetes; 2) develop and maintain a registry of organizations that are recognized for their ability to deliver an effective lifestyle change program; and 3) provide technical assistance to organizations that have applied for recognition to help them deliver an effective lifestyle change program and achieve and maintain recognition. The DPRP standards are used to assure consistent quality, which can help individuals at risk in deciding to participate, health care professionals considering whether to refer a patient, or an insurance provider considering whether to pay for the program. The CDC is responsible for the DPRP, and there is no cost to apply for recognition. More information about the DPRP and applications for recognition are available at www.cdc.gov/diabetes/prevention/recognition.
Lifestyle Change Program Sites and Payment Model
The most prominent core element of the National DPP is delivery of the lifestyle change program. The program is offered at many locations, including community-based organizations, worksites, and health care facilities. Several of these sites recently completed the application process for program recognition. A critical component to ongoing delivery of the lifestyle change program is payment. The nation’s largest health insurer – UnitedHealth Group (UHG) – and largest lifestyle program provider – the National YMCA (Y) – were the first organizations to formally partner with the CDC in the National DPP. The Y and UHG represent a new model for sustainable delivery of the lifestyle change program: a community-based organization (Y) receives payment on a pay-for-performance basis from a third-party health insurer (UHG). The CDC is working to bring more partners into the National DPP, including more organizations to deliver the lifestyle change program and other insurers to cover the cost of participation.
Health Marketing
Even the best lifestyle change programs will not succeed without adequate participation. National DPP partners are working on strategies to increase referrals to and participation in lifestyle change programs. Various participant engagement strategies are being evaluated, as are methods to increase health care professionals’ understanding and support of the lifestyle change program.
Summary
Altering the alarming increase in new cases of type 2 diabetes requires coordinated, focused action that implements the best evidence cost-effectively. The National DPP provides the opportunity to do that. Although many questions about diabetes prevention remain, there is no reason to delay concerted implementation of known information. Registered dietitians are integral to success and can be involved as the experts in nutrition and provision of medical nutrition therapy, participating with and supporting the variety of health workers that must be part of the delivery of lifestyle change programs, and helping people understand their risk status and connect to effective lifestyle change programs.
Footnotes
The findings and conclusions in this report are those of the author and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Centers for Disease Control and Prevention. National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States, 2011. Atlanta, GA: United States Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 2.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr. 2010;8:29–40. doi: 10.1186/1478-7954-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gerstein HC, Santaguida P, Raina P, et al. Annual incidence and relative risk of diabetes in people with various categories of dysglycemia: a systematic overview and meta-analysis of prospective studies. Diabetes Res Clin Pract. 2007;78:305–312. doi: 10.1016/j.diabres.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 4.Knowler WC, Barrett-Connor E, Flowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Diabetes Prevention Program Research Group. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374:1677–1686. doi: 10.1016/S0140-6736(09)61457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ali MK, Echouffo-Tcheugui J, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health Affairs. 2012;31:67–75. doi: 10.1377/hlthaff.2011.1009. [DOI] [PubMed] [Google Scholar]