Abstract
Objective
To assess the labial and lingual alveolar bone thickness in adults with maxillary central incisors of different inclination by cone-beam computed tomography (CBCT).
Methods
Ninety maxillary central incisors from 45 patients were divided into three groups based on the maxillary central incisors to palatal plane angle; lingual-inclined, normal, and labial-inclined. Reformatted CBCT images were used to measure the labial and lingual alveolar bone thickness (ABT) at intervals corresponding to every 1/10 of the root length. The sum of labial ABT and lingual ABT at the level of the root apex was used to calculate the total ABT (TABT). The number of teeth exhibiting alveolar fenestration and dehiscence in each group was also tallied. One-way analysis of variance and Tukey's honestly significant difference test were applied for statistical analysis.
Results
The labial ABT and TABT values at the root apex in the lingual-inclined group were significantly lower than in the other groups (p < 0.05). Lingual and labial ABT values were very low at the cervical level in the lingual-inclined and normal groups. There was a higher prevalence of alveolar fenestration in the lingual-inclined group.
Conclusions
Lingual-inclined maxillary central incisors have less bone support at the level of the root apex and a greater frequency of alveolar bone defects than normal maxillary central incisors. The bone plate at the marginal level is also very thin.
Keywords: Maxillary central incisors, Inclination, Alveolar bone thickness, Cone-beam computed tomography
INTRODUCTION
The dense cortical plates at the apical region of the incisors are regarded as orthodontic walls during orthodontic tooth repositioning, and efficient orthodontic tooth movement can only be ensured with adequate alveolar bone support.1 Upright positioning of the teeth in the center of the alveolus contributes to stable occlusion and better periodontal condition. As the number of adult orthodontic patients increases, orthodontists must pay closer attention to periodontal problems that could be aggravated during treatment. A thorough evaluation of the alveolar bone thickness (ABT) of the maxillary incisors to detect the limits of tooth movement helps orthodontists to secure proper torque control and provide safe treatment that can protect patients from iatrogenic bone loss and maintain healthy periodontal condition. Appropriate tooth torque is necessary to achieve better occlusion, facial esthetics, and stability. It is clinically important to correct and control the torque of maxillary anterior teeth.
Cephalometric radiographs are mid-sagittal projections. Thus, the bone width may be overestimated.1,2 Three-dimensional analysis of specific regions by cone-beam computed tomography (CBCT) may be a better method of assessing bone support. Compared with traditional radiographs, CBCT provides sensitive high-definition true-to-scale three-dimensional images without distortions or superimposition of structures. The high accuracy of CBCT has been reported.3,4,5,6 Considering these advantages, CBCT is the preferred technique for precise evaluation of alveolar bone dimensions.
Previous studies have reported CBCT evaluation of bone morphology in certain malocclusions, volume changes of alveolar bone before and after orthodontic retraction, etc.7,8 Thus, the aim of this study was to apply CBCT for the assessment of ABT of maxillary incisors with different labial-lingual inclinations.
MATERIALS AND METHODS
This study was developed according to established precepts of China Medical University Ethics Committee and included 45 patients (90 maxillary central incisors) aged 18 to 30 years with no prior orthodontic treatment who presented for maxillary CBCT at the Department of Oral Radiology and Orthodontics, School of Stomatology, China Medical University for general examination before orthodontic or other oral treatment and were recruited by questionnaire. Informed consent was obtained from all the included patients.
The exclusion criteria were missing or decayed teeth, prosthetic crowns, crowding more than 3 mm or spacing more than 1 mm in the maxillary anterior alveolar segment, noticeable periodontal disease, diagnosed systemic disease, and craniofacial dysmorphology.
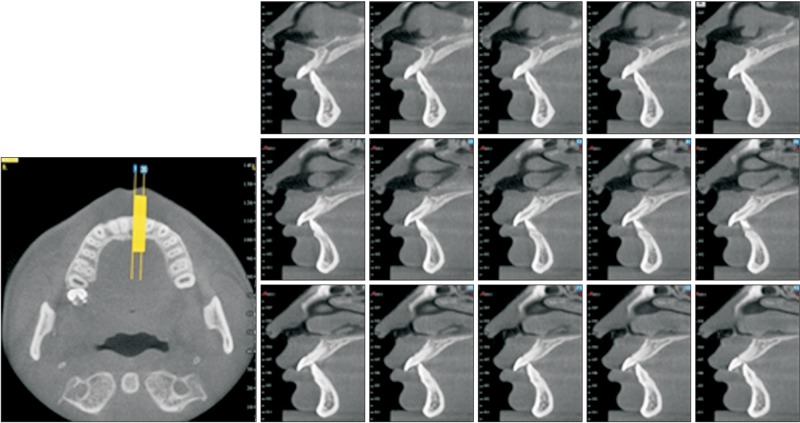
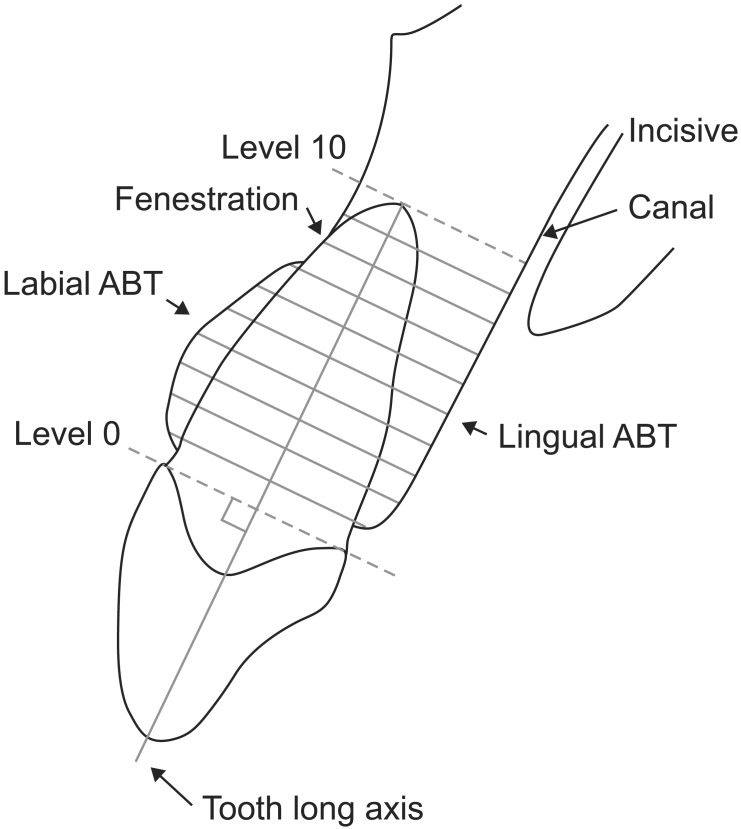
Three-dimensional CBCT images (NewTom TG; QR s.r.l., Verona, Italy) with a voxel size of 0.3 mm were acquired with an exposure time of 20 s at 0.75A, 110 kV, with axial slice thickness 0.3 mm. Reconstruction of the data was performed with NNT software (QR s.r.l.) to create three-dimensional projections of the images with maximum intensity for making linear measurements. The slices were generated from the assumed point of greatest labio-lingual distance (Figure 1). Any site showing no cortical bone around the root in at least three sequential slices was defined as an alveolar defect. When the alveolar defect was more than 2 mm from the cementoenamel junction (CEJ), it was defined as dehiscence. A fenestration was identified as an opening through the alveolar bone exposing parts of the root surface but not involving the alveolar crest (Figure 2).9
Figure 1. Three-dimensional reconstructions of cross-sectional and sagittal slices.
Figure 2. Determination of measurement levels.
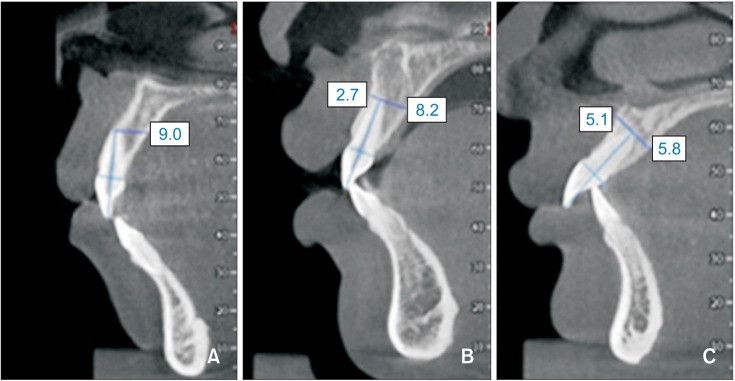
The root length of each tooth was defined as the distance from the CEJ to the apex and was divided into 10 intervals of equal length in selected sagittal slices (level 0 represented the CEJ junction and level 10 represented the root apex) (Figure 3). The labial and lingual thicknesses of the alveolar bone perpendicular to the tooth axis were measured linearly at each level (Figure 2).
Figure 3. Schematic illustration of labial and lingual bone thickness measurements. Level 0, cementoenamel junction; level 10, root apex area. ABT, Alveolar bone thickness.
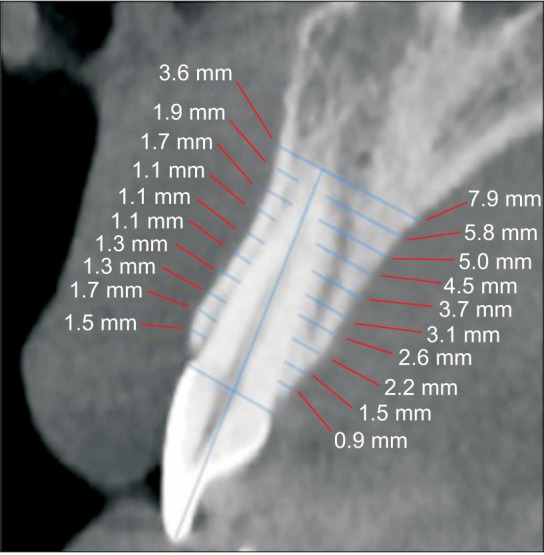
A total of 90 teeth were evaluated. The angle between the axis of the maxillary central incisors and the palatal plane (U1-PP) was determined, and the tomographs were divided into three groups of 30 teeth on the basis of U1-PP angle.10 The lingual-inclined group (U1-PP ≤ 110.1°) comprised 7 men and 8 women, mean age 22.3 ± 4.3 years; the normal group (110.1° < U1-PP ≤ 121.5°) comprised 6 men and 9 women, mean age 21.6 ± 4.5 years; and the labial-inclined group (U1-PP > 121.5°) comprised 7 men and 8 women, mean age 22.4 ± 4.2 years (Figure 4 and 5).
Figure 4. Measuring the angle between the axis of the maxillary central incisors and the palatal plane (U1-PP) in the median sagittal view.
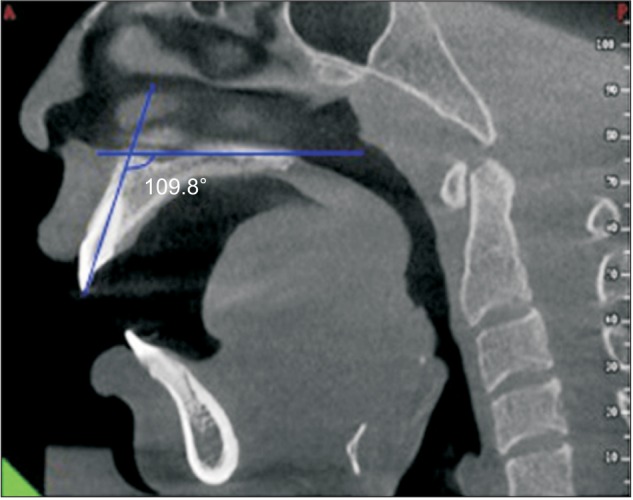
Figure 5. Representative images of three groups classified by different incisor inclination. A, Lingual-inclined group; B, normal group; C, labial-inclined group. The unit of the numberal data in the figure is millimeters.
The prevalence of fenestration and dehiscence in each group was also evaluated by careful observation of each image set.
Statistical analysis
All measurements were repeated after 2 weeks by the same investigator. Statistical calculations were performed with Statistical Package for the Social Sciences (SPSS) version 13.0 (SPSS Inc., Chicago, IL, USA). The data were found to be normally distributed with homogeneity of variance among groups by Shapiro-Wilks normality test and Levene's variance homogeneity test. Statistical comparisons of alveolar thickness in the different inclination groups were conducted by one-way analysis of variance (ANOVA) and Tukey's honestly significant difference (HSD) test. The level of probability for statistical significance was set at p = 0.05. Chi-square test was used for the evaluation of the prevalence of fenestrations and dehiscence. Intraclass correlation coefficients were used to determine intrarater agreement for the measurements. The intraclass correlation coefficients were between 0.881 and 0.992. Intraclass correlation coefficients of 0.75 or above are usually considered to be good, above 0.9 is excellent.
RESULTS
The results of the labial and lingual ABT measurements of the maxillary central incisors are listed in Tables 1, 2, and 3. Statistically significant differences of ABT among the groups were found only at the root apex (level 10). At this level, the labial ABT (p < 0.01) and TABT (p < 0.05) values in the lingual-inclined group were significantly lower than those of the other groups. The labial ABT values around the maxillary central incisors in the lingual-inclined group were also lower than in the other groups from levels 1 to 9, but these differences were not significant, and there were no differences in lingual ABT values among the groups.
Table 1. Comparison of mean labial alveolar bone thickness values at ten root levels by analysis of variance (ANOVA).
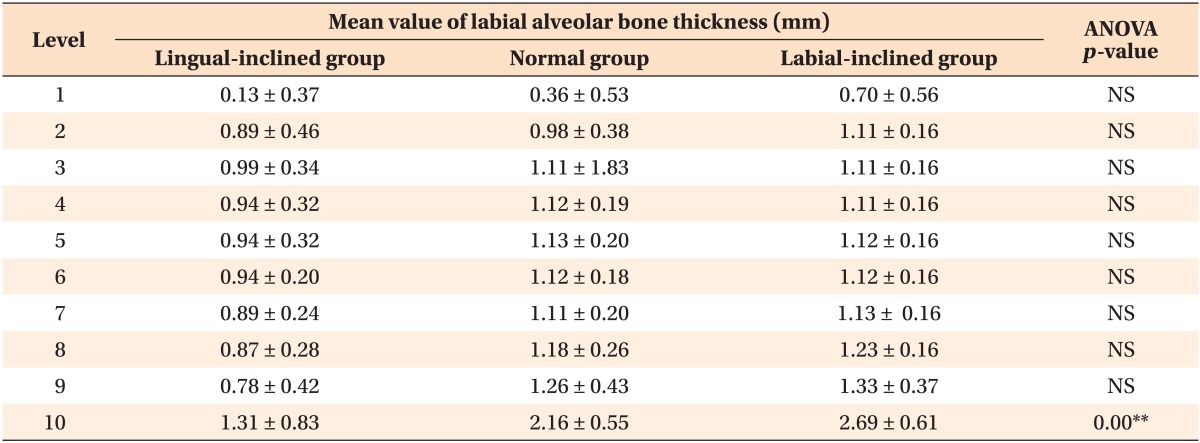
Values are presented as mean ± standard deviation.
**p < 0.01.
NS indicates no statistical significance among the three groups.
Table 2. Comparison of mean lingual alveolar bone thickness values at ten root levels using analysis of variance (ANOVA).
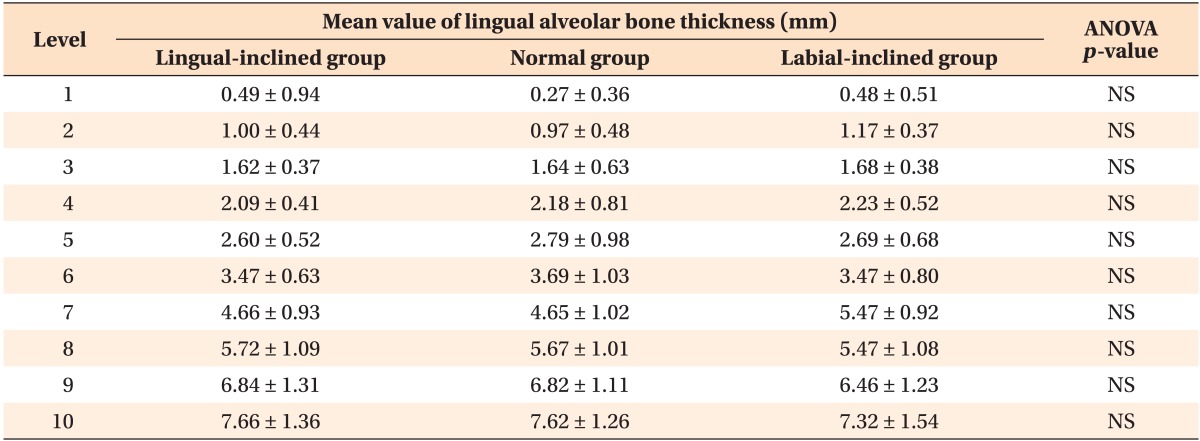
Values are presented as mean ± standard deviation.
NS indicates no statistical significance among the three groups.
Table 3. Comparison of alveolar bone thickness (ABT) and total ABT at the root apex by analysis of variance (ANOVA) and Tukey's honestly significant difference (HSD) test.
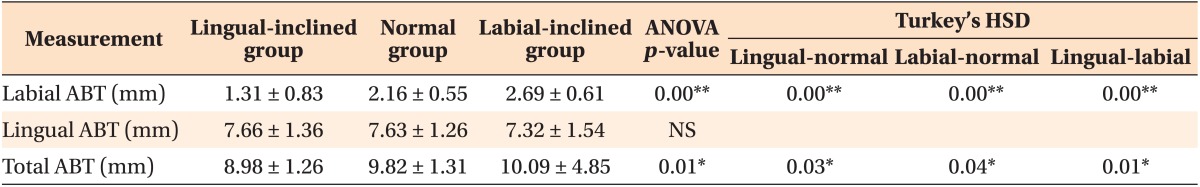
Values are presented as mean ± standard deviation.
**p < 0.01; *p < 0.05.
NS indicates no statistical significance among the three groups.
The ABT measurements of both the labial and lingual aspects of level 1 in the lingual-inclined and normal groups revealed that the bone at this level was very thin. Lingual ABT gradually increased from the CEJ to the apex. The labial ABT measured at the cervical segment in the normal group increased from the CEJ, remained constant in the middle third of the root, and then showed a continuous increase in the apical third.
Fenestrations were observed on the labial bone surface of the root in seven central incisors (Figure 6) in the lingual-inclined group, one central incisor in the normal group, and none in the labial-inclined group (Table 4). One central incisor in the normal group exhibited dehiscence at the marginal bone plate (Figure 7).
Figure 6. Fenestration on labial root surface (arrow).
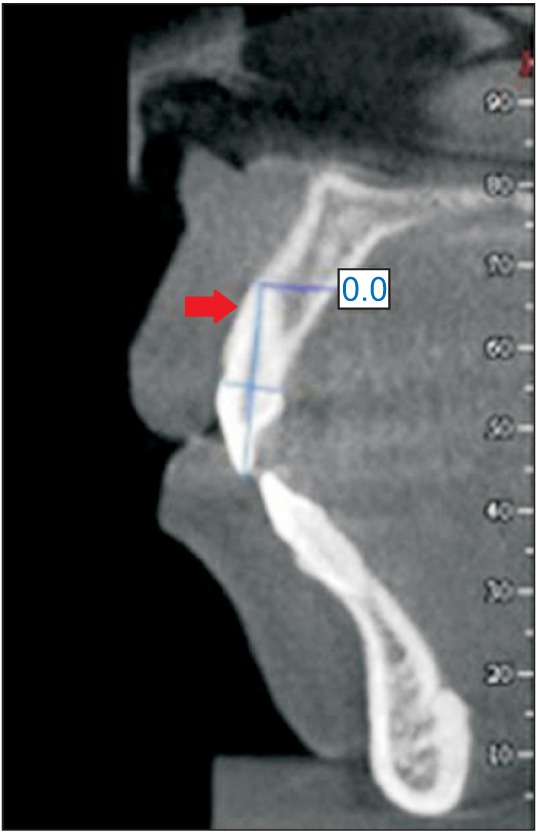
Table 4. Comparison of the frequency of fenestrations between the lingual-inclined group and normal group using chi-square test (n=30).
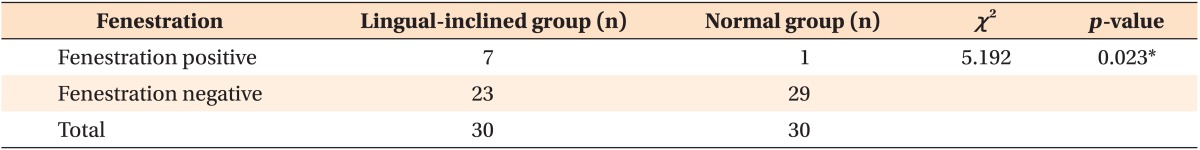
*p < 0.05.
Figure 7. Dehiscence on the root surface (arrow).

DISCUSSION
A thorough assessment of the ABT of the maxillary incisors can help orthodontists improve outcomes and make right treatment decisions. Labial-lingual movement of the anterior teeth to improve the sagittal relationship of the maxillary and mandibular arches is mandatory to achieve a more harmonious profile. However, excessive tooth movement can cause iatrogenic sequelae including root resorption, gingival recession, and alveolar bone loss. Apart from esthetics, periodontal health and the alveolar bone boundaries are important factors in orthodontic treatment. According to our research, there is a significant association between labial-lingual inclination and labial bone thickness at the root apex. This result is similar to the study by Zhou et al.11
The finding that lingual-inclined maxillary incisors have thinner supporting bone, especially in the root apex region, suggests that patients with lingual-inclined incisors should be carefully managed. In patients who have maxillary protrusion with compensatory lingual-inclined incisors, orthodontists should be cautious in determining whether to treat via conventional orthodontics alone or by a combined orthodontic program. If compensatory orthodontics are chosen for patients with slight skeletal discrepancy, orthodontists must make an effort to control the torque of the maxillary anterior teeth and to achieve root-control movement. Appropriate tooth torque is important for achieving better occlusion, facial esthetics, and stability. If torque cannot be controlled as expected, there will be many problems. Andrews demonstrated that when tooth torque deviated by more than 2 degrees from normal values, it had an adverse influence on the occlusion relationship.12 Studies have also shown that greater lingual crown torque will result in a less satisfactory profile and smile arch.13 Excessive lingual crown torque will also result in diminished bone volume, which increases the risk of periodontal damage. Ten Hoeve and Mulie2 noted that when the root apex approximated the dense cortical plate, additional force resulted in labial root absorption and perforation. Dehiscence and fenestrations in the cortical plate have been reported when transverse tooth movement is performed.14,15,16 According to our study, lingual-inclined incisors had a greater prevalence of fenestrations, and the fenestrations were predominant on the labial root surfaces. This corresponds with previous studies.17,18 Once fenestrations occur, the cortical plate is penetrated, and complete repair of the perforation site may not happen unless the teeth are relapsed.19,20,21 Thus, for patients with lingual-inclined incisors, a comprehensive evaluation of the periodontal bone support should be performed, preexisting fenestrations should be identified, and the patient should be informed of the increased risk of new or aggravated periodontal damage. The finding that there is a real risk of overestimating fenestration and dehiscence on CBCT imaging has no conflict with our study.22,23 Instead, it reminds us that even if the situation is not so bad, we must remain cautious.
Our measurements showed that labial-inclined incisors had thicker bone at the labial aspect of the root apex region. For patients who have maxillary dentoalveolar protrusion with flaring anterior teeth, the larger volume of bony support allows retraction of the anterior teeth with some tipping. Some authors hold that tooth movement during the retraction process is not pure translation but rather a combined movement with some tipping.24 Retraction results in upright incisors in the basal bone and ensures long-term stability.25 Thus, compared with lingual-inclined incisors, the movement of labial-inclined incisors is relatively easy and safe.
Our CBCT measurements revealed that the marginal alveolar plate was thin. Some studies have shown that orthodontic treatment can lead to marginal alveolar bone loss and gingival recession.26,27 Other researchers have proposed that alveolar bone loss was more evident at the marginal region because the movement was mostly controlled tipping and the retraction forces applied to the incisors were concentrated at the alveolar crest, leading to greater accumulation of pressure in the marginal region.24 Use of light force and long term activations to allow time for alveolar bone to remodel may help to reduce gingival recession and marginal bone loss.
CBCT facilitates alveolar bone measurement with good to excellent accuracy.28 Traditional radiographic images such as cephalograms, panoramic views, and periapical radiographs are less accurate for evaluating bony architecture.29 Fuhrmann30 found that there is a general overestimation of the labial-lingual bone width on lateral cephalograms when compared with physical measurements of the actual specimens, and Wehrbein et al.15,31 concluded that iatrogenic bony damage was substantially more pronounced than radiographic and macroscopic evaluations revealed. Because we cannot see the damage, it does not mean it is not there, and it should be beneficial to evaluate the bone volume of the maxillary anterior teeth by CBCT to detect preexisting bone defects before orthodontic treatment.
As we were dealing with very small dimensions, it was impossible to accurately detect thickness changes of less than 0.2 mm. To reduce measurement error, all the data were repeatedly measured and intraclass correlation coefficients were controlled at good to excellent. Further study enlarging the sample scale is required to enhance the statistical power and determine the differences more efficiently.
CONCLUSION
1. Patients with lingual-inclined incisors have lower ABT values at the root apex of the maxillary central incisor than patients with normal and labial-inclined incisors, and they appear to be more vulnerable to bone defects.
2. Fenestrations were more prevalent on the labial alveolar bone of lingual-inclined incisors. A thorough and comprehensive evaluation of periodontal bone support should be performed and preexisting bone defects should be detected prior to orthodontic treatment.
3. The bone plate at the marginal level was very thin. This reminds us that in order to reduce gingival recession and marginal bone loss, we should exert light forces and pay close attention to periodontal health.
ACKNOWLEDGEMENTS
Thank you for the support from the Department of Radiology, School of Stomatology, China Medical University.
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.Handelman CS. The anterior alveolus: its importance in limiting orthodontic treatment and its influence on the occurrence of iatrogenic sequelae. Angle Orthod. 1996;66:95–109. discussion 109-10. doi: 10.1043/0003-3219(1996)066<0095:TAAIII>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Ten Hoeve A, Mulie RM. The effect of antero-postero incisor repositioning on the palatal cortex as studied with laminagraphy. J Clin Orthod. 1976;10:804–822. [PubMed] [Google Scholar]
- 3.Zamora N, Llamas JM, Cibrián R, Gandia JL, Paredes V. Cephalometric measurements from 3D reconstructed images compared with conventional 2D images. Angle Orthod. 2011;81:856–864. doi: 10.2319/121210-717.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leuzinger M, Dudic A, Giannopoulou C, Kiliaridis S. Root-contact evaluation by panoramic radiography and cone-beam computed tomography of super-high resolution. Am J Orthod Dentofacial Orthop. 2010;137:389–392. doi: 10.1016/j.ajodo.2009.10.027. [DOI] [PubMed] [Google Scholar]
- 5.de Oliveira AE, Cevidanes LH, Phillips C, Motta A, Burke B, Tyndall D. Observer reliability of three-dimensional cephalometric landmark identification on cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:256–265. doi: 10.1016/j.tripleo.2008.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ganguly R, Ruprecht A, Vincent S, Hellstein J, Timmons S, Qian F. Accuracy of linear measurement in the Galileos cone beam computed tomography under simulated clinical conditions. Dentomaxillofac Radiol. 2011;40:299–305. doi: 10.1259/dmfr/72117593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nahm KY, Kang JH, Moon SC, Choi YS, Kook YA, Kim SH, et al. Alveolar bone loss around incisors in Class I bidentoalveolar protrusion patients: a retrospective three-dimensional cone beam CT study. Dentomaxillofac Radiol. 2012;41:481–488. doi: 10.1259/dmfr/30845402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sarikaya S, Haydar B, Ciğer S, Ariyürek M. Changes in alveolar bone thickness due to retraction of anterior teeth. Am J Orthod Dentofacial Orthop. 2002;122:15–26. doi: 10.1067/mod.2002.119804. [DOI] [PubMed] [Google Scholar]
- 9.Persson RE, Hollender LG, Laurell L, Persson GR. Horizontal alveolar bone loss and vertical bone defects in an adult patient population. J Periodontol. 1998;69:348–356. doi: 10.1902/jop.1998.69.3.348. [DOI] [PubMed] [Google Scholar]
- 10.Lin JX, Xu TM. Contemporary orthodontics. Peking, China: Peking University Medical Press; 2011. p. 607. [Google Scholar]
- 11.Zhou Z, Chen W, Shen M, Sun C, Li J, Chen N. Cone beam computed tomographic analyses of alveolar bone anatomy at the maxillary anterior region in Chinese adults. J Biomed Res. 2014;28:498–505. doi: 10.7555/JBR.27.20130002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andrews LF. Comments on straight-wire appliances. Am J Orthod Dentofacial Orthop. 1990;98:25A–27A. doi: 10.1016/S0889-5406(06)80002-8. [DOI] [PubMed] [Google Scholar]
- 13.Cao L, Zhang K, Bai D, Jing Y, Tian Y, Guo Y. Effect of maxillary incisor labiolingual inclination and anteroposterior position on smiling profile esthetics. Angle Orthod. 2011;81:121–129. doi: 10.2319/033110-181.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Remmelink HJ, van der. Effects of anteroposterior incisor repositioning on the root and cortical plate: a follow-up study. J Clin Orthod. 1984;18:42–49. [PubMed] [Google Scholar]
- 15.Wehrbein H, Bauer W, Diedrich P. Mandibular incisors, alveolar bone, and symphysis after orthodontic treatment. A retrospective study. Am J Orthod Dentofacial Orthop. 1996;110:239–246. doi: 10.1016/s0889-5406(96)80006-0. [DOI] [PubMed] [Google Scholar]
- 16.Vardimon AD, Graber TM, Voss LR, Lenke J. Determinants controlling iatrogenic external root resorption and repair during and after palatal expansion. Angle Orthod. 1991;61:113–122. discussion 123-4. doi: 10.1043/0003-3219(1991)061<0113:DCIERR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Larato DC. Alveolar plate fenestrations and dehiscences of the human skull. Oral Surg Oral Med Oral Pathol. 1970;29:816–819. doi: 10.1016/0030-4220(70)90429-9. [DOI] [PubMed] [Google Scholar]
- 18.Larato DC. Alveolar plate defects in children's skulls. J Periodontol. 1972;43:502. doi: 10.1902/jop.1972.43.8.502. [DOI] [PubMed] [Google Scholar]
- 19.Wainwright WM. Faciolingual tooth movement: its influence on the root and cortical plate. Am J Orthod. 1973;64:278–302. doi: 10.1016/0002-9416(73)90021-3. [DOI] [PubMed] [Google Scholar]
- 20.Wingard CE, Bowers GM. The effects of facial bone from facial tipping of incisors in monkeys. J Periodontol. 1976;47:450–454. doi: 10.1902/jop.1976.47.8.450. [DOI] [PubMed] [Google Scholar]
- 21.Karring T, Nyman S, Thilander B, Magnusson I. Bone regeneration in orthodontically produced alveolar bone dehiscences. J Periodontal Res. 1982;17:309–315. doi: 10.1111/j.1600-0765.1982.tb01158.x. [DOI] [PubMed] [Google Scholar]
- 22.Patcas R, Müller L, Ullrich O, Peltomäki T. Accuracy of cone-beam computed tomography at different resolutions assessed on the bony covering of the mandibular anterior teeth. Am J Orthod Dentofacial Orthop. 2012;141:41–50. doi: 10.1016/j.ajodo.2011.06.034. [DOI] [PubMed] [Google Scholar]
- 23.Leung CC, Palomo L, Griffith R, Hans MG. Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofacial Orthop. 2010;137(4 Suppl):S109–S119. doi: 10.1016/j.ajodo.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 24.Vardimon AD, Oren E, Ben-Bassat Y. Cortical bone remodeling/tooth movement ratio during maxillary incisor retraction with tip versus torque movements. Am J Orthod Dentofacial Orthop. 1998;114:520–529. doi: 10.1016/s0889-5406(98)70172-6. [DOI] [PubMed] [Google Scholar]
- 25.Barrer HG, Buchin ID, Fogel MS, Swain BF, Ackerman JL. Borderline extraction cases: Panel discussion, part 5. J Clin Orthod. 1971;5:609–626. [Google Scholar]
- 26.Ogaard B. Marginal bone support and tooth lengths in 19-year-olds following orthodontic treatment. Eur J Orthod. 1988;10:180–186. doi: 10.1093/ejo/10.3.180. [DOI] [PubMed] [Google Scholar]
- 27.Zachrisson BU, Alnaes L. Periodontal condition in orthodontically treated and untreated individuals. II. Alveolar bone loss: radiographic findings. Angle Orthod. 1974;44:48–55. doi: 10.1043/0003-3219(1974)044<0048:PCIOTA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 28.Sun Z, Smith T, Kortam S, Kim DG, Tee BC, Fields H. Effect of bone thickness on alveolar bone-height measurements from cone-beam computed tomography images. Am J Orthod Dentofacial Orthop. 2011;139:e117–e127. doi: 10.1016/j.ajodo.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 29.Lupi JE, Handelman CS, Sadowsky C. Prevalence and severity of apical root resorption and alveolar bone loss in orthodontically treated adults. Am J Orthod Dentofacial Orthop. 1996;109:28–37. doi: 10.1016/s0889-5406(96)70160-9. [DOI] [PubMed] [Google Scholar]
- 30.Fuhrmann R. Three-dimensional interpretation of labiolingual bone width of the lower incisors. Part II. J Orofac Orthop. 1996;57:168–185. doi: 10.1007/BF02191880. [DOI] [PubMed] [Google Scholar]
- 31.Wehrbein H, Fuhrmann RA, Diedrich PR. Human histologic tissue response after long-term orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 1995;107:360–371. doi: 10.1016/s0889-5406(95)70088-9. [DOI] [PubMed] [Google Scholar]